Abstract
In chronic obesity, hepatocytes become insulin resistant and exert important effects on systemic metabolism. Here we show that in early onset obesity (4 weeks high-fat diet), hepatocytes secrete exosomes that enhance insulin sensitivity both in vitro and in vivo. These beneficial effects were due to exosomal microRNA miR-3075, which is enriched in these hepatocyte exosomes. FA2H is a direct target of miR-3075 and small interfering RNA depletion of FA2H in adipocytes, myocytes and primary hepatocytes leads to increased insulin sensitivity. In chronic obesity (16–18 weeks of a high-fat diet), hepatocyte exosomes promote a state of insulin resistance. These chronic obese hepatocyte exosomes do not directly cause impaired insulin signalling in vitro but do promote proinflammatory activation of macrophages. Taken together, these studies show that in early onset obesity, hepatocytes produce exosomes that express high levels of the insulin-sensitizing miR-3075. In chronic obesity, this compensatory effect is lost and hepatocyte-derived exosomes from chronic obese mice promote insulin resistance.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
The datasets generated in current study are available from the corresponding authors upon reasonable request. There are no restrictions on data availability. All mouse lines in this study are available from the Jackson Laboratory. The miRNA-seq data have been deposited in the NCBI Gene Expression Omnibus under accession number GSE164310. Source data are provided with this paper.
References
Kahn, S. E., Hull, R. L. & Utzschneider, K. M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444, 840–846 (2006).
Lee, Y. S., Wollam, J. & Olefsky, J. M. An integrated view of immunometabolism. Cell 172, 22–40 (2018).
Roden, M. & Shulman, G. I. The integrative biology of type 2 diabetes. Nature 576, 51–60 (2019).
Romeo, G. R., Lee, J. & Shoelson, S. E. Metabolic syndrome, insulin resistance, and roles of inflammation—mechanisms and therapeutic targets. Arter. Thromb. Vasc. Biol. 32, 1771–1776 (2012).
Mathieu, M., Martin-Jaular, L., Lavieu, G. & Thery, C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell-to-cell communication. Nat. Cell Biol. 21, 9–17 (2019).
Mori, M. A., Ludwig, R. G., Garcia-Martin, R., Brandao, B. B. & Kahn, C. R. Extracellular miRNAs: from biomarkers to mediators of physiology and disease. Cell Metab. https://doi.org/10.1016/j.cmet.2019.07.011 (2019).
Kalluri, R. & LeBleu, V. S. The biology, function, and biomedical applications of exosomes. Science https://doi.org/10.1126/science.aau6977 (2020).
Castano, C., Kalko, S., Novials, A. & Parrizas, M. Obesity-associated exosomal miRNAs modulate glucose and lipid metabolism in mice. Proc. Natl Acad. Sci. USA 115, 12158–12163 (2018).
Deng, Z. B. et al. Adipose tissue exosome-like vesicles mediate activation of macrophage-induced insulin resistance. Diabetes 58, 2498–2505 (2009).
Ferrante, S. C. et al. Adipocyte-derived exosomal miRNAs: a novel mechanism for obesity-related disease. Pediatr. Res 77, 447–454 (2015).
Flaherty, S. E. 3rd et al. A lipase-independent pathway of lipid release and immune modulation by adipocytes. Science 363, 989–993 (2019).
Ying, W. et al. Adipose tissue macrophage-derived exosomal miRNAs can modulate in vivo and in vitro insulin sensitivity. Cell 171, 372–384 (2017).
Ying, W. et al. MiR-690, an exosomal-derived miRNA from M2-polarized macrophages, improves insulin sensitivity in obese mice. Cell Metab. https://doi.org/10.1016/j.cmet.2020.12.019 (2021).
Crewe, C. et al. An endothelial-to-adipocyte extracellular vesicle axis governed by metabolic state. Cell 175, 695–708 e613 (2018).
Thomou, T. et al. Adipose-derived circulating miRNAs regulate gene expression in other tissues. Nature 542, 450–455 (2017).
Baek, D. et al. The impact of microRNAs on protein output. Nature 455, 64–71 (2008).
Bartel, D. P. MicroRNAs: target recognition and regulatory functions. Cell 136, 215–233 (2009).
Selbach, M. et al. Widespread changes in protein synthesis induced by microRNAs. Nature 455, 58–63 (2008).
Scheja, L. & Heeren, J. Metabolic interplay between white, beige, brown adipocytes and the liver. J. Hepatol. 64, 1176–1186 (2016).
Turner, N. et al. Distinct patterns of tissue-specific lipid accumulation during the induction of insulin resistance in mice by high-fat feeding. Diabetologia 56, 1638–1648 (2013).
Povero, D. et al. Lipid-induced hepatocyte-derived extracellular vesicles regulate hepatic stellate cell via microRNAs targeting PPAR-gamma. Cell Mol. Gastroenterol. Hepatol. 1, 646–663 e644 (2015).
Lee, Y. S. et al. Exosomes derived from palmitic acid-treated hepatocytes induce fibrotic activation of hepatic stellate cells. Sci. Rep. 7, 3710 (2017).
Chen, L., Chen, R., Kemper, S., Charrier, A. & Brigstock, D. R. Suppression of fibrogenic signaling in hepatic stellate cells by Twist1-dependent microRNA-214 expression: role of exosomes in horizontal transfer of Twist1. Am. J. Physiol. Gastrointest. Liver Physiol. 309, G491–G499 (2015).
Pescador, N. et al. Serum circulating microRNA profiling for identification of potential type 2 diabetes and obesity biomarkers. PLoS ONE 8, e77251 (2013).
Chen, L., Brenner, D. A. & Kisseleva, T. Combatting fibrosis: exosome-based therapies in the regression of liver fibrosis. Hepatol. Commun. 3, 180–192 (2019).
Shurtleff, M. J., Temoche-Diaz, M. M., Karfilis, K. V., Ri, S. & Schekman, R. Y-box protein 1 is required to sort microRNAs into exosomes in cells and in a cell-free reaction. eLife https://doi.org/10.7554/eLife.19276 (2016).
Shurtleff, M. J. et al. Broad role for YBX1 in defining the small noncoding RNA composition of exosomes. Proc. Natl Acad. Sci. USA 114, E8987–E8995 (2017).
Ran, F. A. et al. In vivo genome editing using Staphylococcus aureus Cas9. Nature 520, 186–U198 (2015).
Platt, R. J. et al. CRISPR-Cas9 knockin mice for genome editing and cancer modeling. Cell 159, 440–455 (2014).
Liu, P. S. et al. Alpha-ketoglutarate orchestrates macrophage activation through metabolic and epigenetic reprogramming. Nat. Immunol. 18, 985–994 (2017).
Ostrowski, M. et al. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nat. Cell Biol. 12, 19–30 (2010).
Song, L. et al. KIBRA controls exosome secretion via inhibiting the proteasomal degradation of Rab27a. Nat. Commun. 10, 1639 (2019).
Bobrie, A. et al. Rab27a supports exosome-dependent and -independent mechanisms that modify the tumor microenvironment and can promote tumor progression. Cancer Res. 72, 4920–4930 (2012).
Agarwal, V., Bell, G. W., Nam, J. W. & Bartel, D. P. Predicting effective microRNA target sites in mammalian mRNAs. eLife https://doi.org/10.7554/eLife.05005 (2015).
Zhao, Y. et al. Liver governs adipose remodelling via extracellular vesicles in response to lipid overload. Nat. Commun. 11, 719 (2020).
Alderson, N. L. et al. The human FA2H gene encodes a fatty acid 2-hydroxylase. J. Biol. Chem. 279, 48562–48568 (2004).
Eckhardt, M., Yaghootfam, A., Fewou, S. N., Zoller, I. & Gieselmann, V. A mammalian fatty acid hydroxylase responsible for the formation of alpha-hydroxylated galactosylceramide in myelin. Biochem. J. 388, 245–254 (2005).
Shang, M. et al. Macrophage-derived glutamine boosts satellite cells and muscle regeneration. Nature 587, 626–631 (2020).
Lignitto, L. et al. Nrf2 activation promotes lung cancer metastasis by inhibiting the degradation of Bach1. Cell 178, 316–329 (2019).
Yan, S. et al. IRF3 reduces adipose thermogenesis via ISG15-mediated reprogramming of glycolysis. J. Clin. Invest. https://doi.org/10.1172/JCI144888 (2021).
Seo, J. B. et al. Knockdown of Ant2 reduces adipocyte hypoxia and improves insulin resistance in obesity. Nat. Metab. 1, 86–97 (2019).
Li, P. et al. Hematopoietic-derived galectin-3 causes cellular and systemic insulin resistance. Cell 167, 973–984 e912 (2016).
Ying, W., Cheruku, P. S., Bazer, F. W., Safe, S. H. & Zhou, B. Investigation of macrophage polarization using bone marrow derived macrophages. J. Vis. Exp. https://doi.org/10.3791/50323 (2013).
Li, P. et al. LTB4 promotes insulin resistance in obese mice by acting on macrophages, hepatocytes and myocytes. Nat. Med. 21, 239–247 (2015).
Garcia, D. M. et al. Weak seed-pairing stability and high target-site abundance decrease the proficiency of lsy-6 and other microRNAs. Nat. Struct. Mol. Biol. 18, 1139–1146 (2011).
Acknowledgements
We thank the UCSD IGM Genomics Center for RNA-seq, the UCSD electron microscopy core for electron microscopic analysis, and the Vector Development Core Laboratory for lentivirus preparation. This study was funded by the US National Institute of Diabetes and Digestive and Kidney Diseases (grant nos. P30 DK063491, R00DK115998 and R01DK125560 to W.Y.) and the US National Institute of Diabetes and Digestive and Kidney Diseases (grant nos. P30 DK063491 and DK101395 to J.M.O.).
Author information
Authors and Affiliations
Contributions
W.Y. designed the studies, and Y.J. and Z.L. performed most of the experiments. F.C.G.D.R., K.A.M. and H.G. assisted with in vivo insulin stimulation assays, cell culture, qPCR analysis and western blot analysis. Z.J. and H.G. assisted with bone marrow cell isolation and differentiation. R.I., M.Y., W.F. and Z.J. assisted with tissue collection. G.B. assisted with hepatocyte isolation and glucose output assays. W.Y. and J.M.O. supervised the project. W.Y. and J.M.O. analysed and interpreted the data and cowrote the paper.
Corresponding authors
Ethics declarations
Competing interests
W.Y. and J.M.O. are coinventors on a provisional patent covering the use of miR-3075 as an insulin sensitizer. Outside this, the other authors declare no competing interests.
Additional information
Peer review information Nature Metabolism thanks Jan-Wilhelm Kornfeld, Anja Zeigerer and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Isabella Samuelson.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
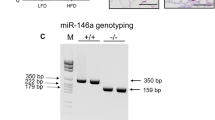
Extended Data Fig. 1 Hepatocyte exosomes from early stage obese mice improve cellular insulin sensitivity.
The marker characteristics (a) and production (b) of exosomes (Exos) derived from lean, 4wk or 16wk HFD WT hepatocytes. c, The appearance of red fluorescence in key metabolic tissues of 12wk HFD WT mice after tail vein injection with PKH26-labeled 4wk HFD hepatocyte Exos. 4wk HFD hepatocyte Exos without PKH26 labeling were injected to evaluate the level of autofluorescence. d, Effect of empty liposome treatment on metabolic phenotypes of 16wks HFD/obese WT mice. e, Effect of hepatocyte Exos treatment on body weight. f, the population and activation status of adipose tissue macrophages by flow cytometry analysis. Adipose tissue macrophages (ATM)=CD11b+F4/80+, M1 ATM=CD11c+CD206-, and M2 ATM=CD11c-CD206+. g, Effect of 4wk HFD Exos on proinflammatory cytokine abundance in epididymal fat of 18wk HFD mice by qPCR analysis. Effects of 4wk HFD Exos on glucose uptake of 3T3-L1 adipocytes (h), L6 myocytes (i), and glucose production of 12wk HFD/obese hepatocytes (j). k, The levels of insulin-stimulated AKT phosphorylation in 3T3-L1 adipocytes, L6 myocytes, and obese hepatocytes. e-k, empty liposomes were used in the control groups. All experiments were repeated at least twice with similar results. Data are presented as mean ± SEM. n=7 (b), n=6 (d), n=5-10 (e), n=5 (f, h), n=3 (g), n=6 (i), n=8 (j) per group. Two-sided Student’s t-test.
Extended Data Fig. 2 Effect of hepatocyte-specific YBX1 knockout on the ability of hepatocyte Exos to regulate metabolic responses.
a, Hepatocyte YBX1 levels in the hepatocyte-specific Cas9 transgenic mice after 4 weeks of injection of lentivirus harbouring gRNA-YBX1 vectors. Control mice were treated with a lentiviral empty vector. b, Expression of TSG101 and CD63 in Exos derived from both 4wk HFD WT and YBX1KO hepatocytes. c, Body weight of both WT and YBX1KO mice after 4 weeks HFD feeding. d, Effect of hepatocyte Exos on body weight of 18wks HFD/obese recipient mice. Empty liposomes were used in the control HFD WT mice. e, Effect of 4wk HFD WT Exos or YBX1KO Exos on cellular phosphorylated AKT levels. Control cells were treated with empty liposomes. All experiments were repeated at least twice with similar results. Data are presented as mean ± SEM. n=8 (c and d) per group.
Extended Data Fig. 3 Effect of hepatocyte-specific Rab27 knockout on metabolic phenotypes.
a, Hepatocyte Rab27 levels in the hepatocyte-specific Cas9 transgenic mice after 4 weeks of injection of lentivirus harboring gRNA Rab27 vectors. Control mice were treated with a lentiviral empty vector. b, Effect of 4wk HFD Rab27KO hepatocyte Exos on glucose production in 16wk HFD/obese primary hepatocytes. Empty liposomes were used in the control cells. c, Body weight of both WT and hepatocyte-specific Rab27KO mice after 4 weeks HFD feeding. d, Hepatic glucose production after Rab27 knockout. All experiments were repeated at least twice with similar results. Data are presented as mean ± SEM. n=4 (b), n=6 (c), n=8 (d) per group. Two-sided Student’s t-test.
Extended Data Fig. 4 Effect of miR-3075 on insulin sensitivity.
miR-3075 abundance in liver (a), skeletal muscle (SKL, b), and eWAT (c) of 18wk HFD WT recipient mice after treatment with 4wk HFD Exos. qPCR analysis of miR-3075 abundance (d), hepatic glucose production (e), and insulin-stimulated AKT phosphorylation (f) in lean, 4wk or 16wk HFD WT hepatocytes. g, Effect of the miR-3075 antagomir on AKT phosphorylation level in 4wk HFD hepatocytes. h, miR-3075 abundance in key metabolic tissues of lean WT mice, 3T3-L1 adipocytes, and L6 myocytes. i, Effect of 4wk HFD Exos, 4wk HFD YBX1KO Exos, or combination treatment with 4wk HFD YBX1KO plus miR-3075 mimic on cellular insulin responses. j, Glucose tolerance of NCD, 4wk HFD, and 16wk HFD WT mice. k, qPCR analysis of miR-3075 abundance within Exos derived from lean hepatocytes transfected with the miR-3075 mimic. l, Effect of miR-3075-enriched hepatocyte (miR-3075oe) Exos on 3T3-L1 adipocyte glucose uptake. m, The levels of phosphorylated AKT in metabolic tissues of 4wks HFD WT mice after treatment with the miR-3075 antagomir. Effects of miR-3075 antagomir on glucose tolerance (n) and insulin sensitivity (o) of lean WT mice. n=4 (a-c, h, k), n=6-8 (d), n=8 (e), n=6 (i), n=8 (j, l), n=5-6 (n and o) per group. All experiments were repeated at least twice with similar results. Data are presented as mean ± SEM. Two-sided Student’s t-test.
Extended Data Fig. 5 miR-3075 represses FA2H expression.
a, qPCR analysis of possible target genes of miR-3075. b, FA2H abundance after transfection with the miR-3075 mimic. c, The expression of miR-3075 in human HepG2 cells. d, Effect of miR-3075 overexpression on FA2H abundance in human HepG2 cells. e, Validation of FA2H knockdown in 3T3-L1 adipocytes, L6 myocytes, and obese hepatocytes. f, Effect of Fa2h knockdown on AKT phosphorylation in the cells without insulin stimulation. b and c, The control cells were transfected with a scramble miRNA mimic. e and f, non-targeting control siRNA was used in the control cells. All experiments were repeated at least twice with similar results. Data are presented as mean ± SEM. n=5-6 (a, c) per group. Two-sided Student’s t-test.
Extended Data Fig. 6 16wk HFD Exos treatment did not affect cellular insulin sensitivity.
a-c, Effect of 16wk HFD Exos on cellular insulin responses. Empty liposomes were used in the control groups. All experiments were repeated at least twice with similar results. Data are presented as mean ± SEM. n=5-6 (a), n=6 (b), n=4 (c) per group.
Extended Data Fig. 7 Effect of miR-434-3p on macrophage activation.
a, Gating strategy of flow cytometry analysis of adipose tissue macrophages. F4/80+CD11b+ ATMs were gated from viable CD45+ cells, and M1 (CD11c+CD206-) and M2 (CD11c-CD206+) cells were then gated from F4/80+CD11b+ ATMs. b, miR-434-3p abundance in epididymal fat of NCD recipient mice after treatment of 16wk HFD Exos for 5 weeks. c, qPCR analysis of miR-434-3p abundance in BMDMs after transfection with the miR-434-3p mimic. d, Effect of miR-434-3p overexpression on proinflammatory activation in naïve M0 BMDMs. e-g, Effect of miR-434-3p on glucose uptake in 3T3-L1 adipocytes and L6 myocytes and primary hepatocyte glucose production. c-g, A scramble miRNA mimic was used in control cells. All experiments were repeated at least twice with similar results. Data are presented as mean ± SEM. n=4 (a, e, g), n=5-6 (c), n=6-7 (d), n=12 (f) per group. Two-sided Student’s t-test.
Supplementary information
Supplementary Information
Supplementary Table 1: information on reagents and resources.
Source data
Source Data Fig. 1
Unprocessed western blots.
Source Data Fig. 3
Unprocessed western blots.
Source Data Fig. 4
Unprocessed western blots.
Source Data Fig. 5
Unprocessed western blots.
Source Data Fig. 6
Unprocessed western blots.
Source Data Extended Data Fig. 1
Unprocessed western blots.
Source Data Extended Data Fig. 2
Unprocessed western blots.
Source Data Extended Data Fig. 3
Unprocessed western blots.
Source Data Extended Data Fig. 4
Unprocessed western blots.
Source Data Extended Data Fig. 5
Unprocessed western blots.
Rights and permissions
About this article
Cite this article
Ji, Y., Luo, Z., Gao, H. et al. Hepatocyte-derived exosomes from early onset obese mice promote insulin sensitivity through miR-3075. Nat Metab 3, 1163–1174 (2021). https://doi.org/10.1038/s42255-021-00444-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42255-021-00444-1
This article is cited by
-
Adipose tissue macrophages secrete small extracellular vesicles that mediate rosiglitazone-induced insulin sensitization
Nature Metabolism (2024)
-
Liver-derived extracellular vesicles improve whole-body glycaemic control via inter-organ communication
Nature Metabolism (2024)
-
Sub-nanosized vanadate hybrid clusters maintain glucose homeostasis and restore treatment response in inflammatory disease in obese mice
Nano Research (2024)
-
Bone marrow mesenchymal stem cell-derived exosomal microRNA-382 promotes osteogenesis in osteoblast via regulation of SLIT2
Journal of Orthopaedic Surgery and Research (2023)
-
The link between gestational diabetes and cardiovascular diseases: potential role of extracellular vesicles
Cardiovascular Diabetology (2022)