Abstract
Radiotherapy should have low toxicity in the entrance channel (normal tissue) and be very effective in cell killing in the target region (tumour). In this regard, ions heavier than protons have both physical and radiobiological advantages over conventional X-rays. Carbon ions represent an excellent combination of physical and biological advantages. There are a dozen carbon-ion clinical centres in Europe and Asia, and more under construction or at the planning stage, including the first in the USA. Clinical results from Japan and Germany are promising, but a heated debate on the cost-effectiveness is ongoing in the clinical community, owing to the larger footprint and greater expense of heavy ion facilities compared with proton therapy centres. We review here the physical basis and the clinical data with carbon ions and the use of different ions, such as helium and oxygen. Research towards smaller and cheaper machines with more effective beam delivery is necessary to make particle therapy affordable. The potential of heavy ions has not been fully exploited in clinics and, rather than there being a single ‘silver bullet’, different particles and their combination can provide a breakthrough in radiotherapy treatments in specific cases.
Key points
-
Charged particle therapy is the most advanced radiotherapy technique.
-
Most of the patients are treated with protons, but heavy ions present additional biological advantages.
-
Carbon-ion therapy is ongoing in 12 centres worldwide and clinical results are promising, whereas new ions (like 4He and 16O) will be used in the future.
-
Heavy ion therapy is much more expensive than X-ray therapy and level 1 evidence of superiority is missing.
-
Radiobiology suggests that heavy ions can be exquisitely effective against hypoxic tumours and improve the effects of immunotherapy.
-
Rather than a ‘silver bullet’, different particles and their combination can provide optimal results in specific cases.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Wilson, R. R. Radiological use of fast protons. Radiology 47, 487–491 (1946).
Tobias, C. A. Failla Memorial lecture. The future of heavy-ion science in biology and medicine. Radiat. Res. 103, 1–33 (1985).
Durante, M. & Loeffler, J. S. Charged particles in radiation oncology. Nat. Rev. Clin. Oncol. 7, 37–43 (2010).
Castro, J. R. Results of heavy ion radiotherapy. Radiat. Environ. Biophys. 34, 45–48 (1995).
Colliez, F., Gallez, B. & Jordan, B. F. Assessing tumor oxygenation for predicting outcome in radiation oncology: a review of studies correlating tumor hypoxic status and outcome in the preclinical and clinical settings. Front. Oncol. 7, 10 (2017).
Blakely, E. A., Ngo, F., Curtis, S. & Tobias, C. A. Heavy-ion radiobiology: cellular studies. Adv. Radiat. Biol. 11, 295–389 (1984).
Tinganelli, W. & Durante, M. Carbon ion radiobiology. Cancers 12, 3022 (2020).
Tsujii, H. et al. Carbon-Ion Radiotherapy (Springer, 2014).
Kraft, G. Tumor therapy with heavy charged particles. Prog. Part. Nucl. Phys. 45, 473–544 (2000).
Thariat, J., Hannoun-Levi, J.-M., Sun Myint, A., Vuong, T. & Gérard, J.-P. Past, present, and future of radiotherapy for the benefit of patients. Nat. Rev. Clin. Oncol. 10, 52–60 (2012).
Lo, S. S. et al. Stereotactic body radiation therapy: a novel treatment modality. Nat. Rev. Clin. Oncol. 7, 44–54 (2010).
Pan, H. Y., Jiang, J., Shih, Y.-C. T. & Smith, B. D. Adoption of radiation technology among privately insured nonelderly patients with cancer in the United States, 2008 to 2014: a claims-based analysis. J. Am. Coll. Radiol. 14, 1027–1033.e2 (2017).
Waddle, M. R. et al. Photon and proton radiation therapy utilization in a population of more than 100 million commercially insured patients. Int. J. Radiat. Oncol. 99, 1078–1082 (2017).
Lievens, Y., Borras, J. M. & Grau, C. Provision and use of radiotherapy in Europe. Mol. Oncol. 14, 1461–1469 (2020).
Particle Therapy Co-Operative Group (PTCOG). Particle therapy facilities in clinical operation. PTCOG https://www.ptcog.ch/ (2021).
Malouff, T. D. et al. Carbon ion therapy: a modern review of an emerging technology. Front. Oncol. 10, 82 (2020).
Beltran, C., Amos, R. A. & Rong, Y. We are ready for clinical implementation of carbon ion radiotherapy in the United States. J. Appl. Clin. Med. Phys. 21, 6–9 (2020).
Pompos, A., Durante, M. & Choy, H. Heavy ions in cancer therapy. JAMA Oncol. 2, 1539–1540 (2016).
Bortfeld, T. R. & Loeffler, J. S. Three ways to make proton therapy affordable. Nature 549, 451–453 (2017).
Jäkel, O., Smith, A. R. & Orton, C. G. The more important heavy charged particle radiotherapy of the future is more likely to be with heavy ions rather than protons. Med. Phys. 40, 090601 (2013).
Durante, M. & Debus, J. Heavy charged particles: does improved precision and higher biological effectiveness translate to better outcome in patients? Semin. Radiat. Oncol. 28, 160–167 (2018).
Rackwitz, T. & Debus, J. Clinical applications of proton and carbon ion therapy. Semin. Oncol. 46, 226–232 (2019).
Tessonnier, T. et al. Helium ions at the heidelberg ion beam therapy center: Comparisons between FLUKA Monte Carlo code predictions and dosimetric measurements. Phys. Med. Biol. 62, 6784–6803 (2017).
Kurz, C., Mairani, A. & Parodi, K. First experimental-based characterization of oxygen ion beam depth dose distributions at the Heidelberg Ion-Beam Therapy Center. Phys. Med. Biol. 57, 5017–5034 (2012).
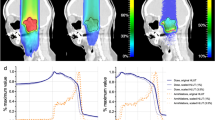
Kopp, B. et al. Development and validation of single field multi-ion particle therapy treatments. Int. J. Radiat. Oncol. 106, 194–205 (2020).
Inaniwa, T. et al. Application of lung substitute material as ripple filter for multi-ion therapy with helium-, carbon-, oxygen-, and neon-ion beams. Phys. Med. Biol. 66, 055002 (2021).
Dokic, I. et al. Next generation multi-scale biophysical characterization of high precision cancer particle radiotherapy using clinical proton, helium-, carbon- and oxygen ion beams. Oncotarget 7, 56676–56689 (2016).
Inaniwa, T. et al. Experimental validation of stochastic microdosimetric kinetic model for multi-ion therapy treatment planning with helium-, carbon-, oxygen-, and neon-ion beams. Phys. Med. Biol. 65, 045005 (2020).
Sokol, O., Krämer, M., Hild, S., Durante, M. & Scifoni, E. Kill painting of hypoxic tumors with multiple ion beams. Phys. Med. Biol. 64, 045008 (2019).
Durante, M. & Paganetti, H. Nuclear physics in particle therapy: a review. Rep. Prog. Phys. 79, 096702 (2016).
Newhauser, W. D. & Zhang, R. The physics of proton therapy. Phys. Med. Biol. 60, R155 (2015).
Schardt, D., Elsässer, T. & Schulz-Ertner, D. Heavy-ion tumor therapy: physical and radiobiological benefits. Rev. Mod. Phys. 82, 383–425 (2010).
Bichsel, H. Stochastics of energy loss and biological effects of heavy ions in radiation therapy. Adv. Quantum Chem. 65, 1–38 (2013).
Kamakura, S., Sakamoto, N., Ogawa, H., Tsuchida, H. & Inokuti, M. Mean excitation energies for the stopping power of atoms and molecules evaluated from oscillator-strength spectra. J. Appl. Phys. 100, 064905 (2006).
Bär, E., Andreo, P., Lalonde, A., Royle, G. & Bouchard, H. Optimized I-values for use with the Bragg additivity rule and their impact on proton stopping power and range uncertainty. Phys. Med. Biol. 63, 165007 (2018).
Besemer, A., Paganetti, H. & Bednarz, B. The clinical impact of uncertainties in the mean excitation energy of human tissues during proton therapy. Phys. Med. Biol. 58, 887–902 (2013).
De Smet, V., Labarbe, R., Vander Stappen, F., Macq, B. & Sterpin, E. Reassessment of stopping power ratio uncertainties caused by mean excitation energies using a water-based formalism. Med. Phys. 45, 3361–3370 (2018).
Embriaco, A., Bellinzona, E. V., Fontana, A. & Rotondi, A. On Molière and Fermi–Eyges scattering theories in hadrontherapy. Phys. Med. Biol. 62, 6290–6303 (2017).
Ebrahimi Loushab, M., Mowlavi, A. A., Hadizadeh, M. H., Izadi, R. & Jia, S. B. Impact of various beam parameters on lateral scattering in proton and carbon-ion therapy. J. Biomed. Phys. Eng. 5, 169–176 (2015).
Zeitlin, C. & La Tessa, C. The role of nuclear fragmentation in particle therapy and space radiation protection. Front. Oncol. 6, 65 (2016).
Lomax, A. J. Myths and realities of range uncertainty. Br. J. Radiol. 93, 20190582 (2020).
Paganetti, H. Range uncertainties in proton therapy and the role of Monte Carlo simulations. Phys. Med. Biol. 57, R99–R117 (2012).
Durante, M. & Flanz, J. Charged particle beams to cure cancer: strengths and challenges. Semin. Oncol. 46, 219–225 (2019).
Knopf, A.-C. & Lomax, A. In vivo proton range verification: a review. Phys. Med. Biol. 58, R131–R160 (2013).
Parodi, K. Vision 20/20: positron emission tomography in radiation therapy planning, delivery, and monitoring. Med. Phys. 42, 7153–7168 (2015).
Pönisch, F., Parodi, K., Hasch, B. G. & Enghardt, W. The modelling of positron emitter production and PET imaging during carbon ion therapy. Phys. Med. Biol. 49, 5217–5232 (2004).
Bauer, J. et al. Implementation and initial clinical experience of offline PET/CT-based verification of scanned carbon ion treatment. Radiother. Oncol. 107, 218–226 (2013).
Augusto, R. S. et al. An overview of recent developments in FLUKA PET tools. Phys. Med. 54, 189–199 (2018).
Durante, M. & Parodi, K. Radioactive beams in particle therapy: past, present, and future. Front. Phys. 8, 00326 (2020).
Durante, M., Golubev, A., Park, W.-Y. & Trautmann, C. Applied nuclear physics at the new high-energy particle accelerator facilities. Phys. Rep. 800, 1–37 (2019).
Chacon, A. et al. Experimental investigation of the characteristics of radioactive beams for heavy ion therapy. Med. Phys. 47, 3123–3132 (2020).
Augusto, R. S. et al. New developments of 11C post-accelerated beams for hadron therapy and imaging. Nucl. Instrum. Methods Phys. Res. B 376, 374–378 (2016).
Chao, A. W. & Chou, W. Reviews of Accelerator Science and Technology. Volume 2: Medical Applications of Accelerators (World Scientific, 2009).
Farr, J. B., Flanz, J. B., Gerbershagen, A. & Moyers, M. F. New horizons in particle therapy systems. Med. Phys. 45, e953–e983 (2018).
Alonso, J. R. & Antaya, T. A. Superconductivity in medicine. Rev. Accel. Sci. Technol. 05, 227–263 (2012).
Jongen, Y. et al. Compact superconducting cyclotron C400 for hadron therapy. Nucl. Instrum. Methods Phys. Res. A 624, 47–53 (2010).
Syresin, E. M. et al. Superconducting synchrotron project for hadron therapy. Phys. Part. Nucl. Lett. 9, 202–212 (2012).
Noda, K. et al. Recent progress and future plans of heavy-ion cancer radiotherapy with HIMAC. Nucl. Instrum. Methods Phys. Res. B 406, 374–378 (2017).
Zlobin, A. V. & Schoerling, D. in Nb3Sn Accelerator Magnets. Designs, Technologies and Performance (eds. Schoerling, D. & Zlobin, A.) 3–22 (Springer, 2019).
Wan, W. et al. Alternating-gradient canted cosine theta superconducting magnets for future compact proton gantries. Phys. Rev. Spec. Top. Accel. Beams 18, 103501 (2015).
Baird, Y. T. E. & Li, Q. Optimized magnetic design of superconducting magnets for heavy ion rotating gantries. IEEE Trans. Appl. Supercond. 30, 1–8 (2020).
Caporaso, G. J., Chen, Y.-J. & Sampayan, S. E. The dielectric wall accelerator. Rev. Accel. Sci. Technol. 02, 253–263 (2009).
Ma, W. J. et al. Laser acceleration of highly energetic carbon ions using a double-layer target composed of slightly underdense plasma and ultrathin foil. Phys. Rev. Lett. 122, 014803 (2019).
Higginson, A. et al. Near-100 MeV protons via a laser-driven transparency-enhanced hybrid acceleration scheme. Nat. Commun. 9, 724 (2018).
Ahmed, H. et al. High energy implementation of coil-target scheme for guided re-acceleration of laser-driven protons. Sci. Rep. 11, 699 (2021).
Wang, K. D. et al. Achromatic beamline design for a laser-driven proton therapy accelerator. Phys. Rev. Accel. Beams 23, 111302 (2020).
Karsch, L. et al. Towards ion beam therapy based on laser plasma accelerators. Acta Oncol. 56, 1359–1366 (2017).
Linz, U. & Alonso, J. Laser-driven ion accelerators for tumor therapy revisited. Phys. Rev. Accel. Beams 19, 124802 (2016).
Noda, K. Progress of radiotherapy technology with HIMAC. J. Phys. Conf. Ser. 1154, 012019 (2019).
Kubiak, T. Particle therapy of moving targets — the strategies for tumour motion monitoring and moving targets irradiation. Br. J. Radiol. 89, 20150275 (2016).
Bert, C. & Durante, M. Motion in radiotherapy: particle therapy. Phys. Med. Biol. 56, R113–R144 (2011).
Riboldi, M., Orecchia, P. R. & Baroni, P. G. Real-time tumour tracking in particle therapy: technological developments and future perspectives. Lancet Oncol. 13, e383–e391 (2012).
Czerska, K. et al. Clinical practice vs. state-of-the-art research and future visions: Report on the 4D treatment planning workshop for particle therapy–Edition 2018 and 2019. Phys. Med. 82, 54–63 (2021).
Graeff, C., Lüchtenborg, R., Eley, J. G., Durante, M. & Bert, C. A 4D-optimization concept for scanned ion beam therapy. Radiother. Oncol. 109, 419–424 (2013).
Iwata, Y. et al. Design of a superconducting rotating gantry for heavy-ion therapy. Phys. Rev. Spec. Top. Accel. Beams 15, 044701 (2012).
Rahim, S. et al. Upright radiation therapy — a historical reflection and opportunities for future applications. Front. Oncol. 10, 213 (2020).
Yang, J., Chu, D., Dong, L. & Court, L. E. Advantages of simulating thoracic cancer patients in an upright position. Pract. Radiat. Oncol. 4, e53–e58 (2014).
Zhang, X. et al. Development of an isocentric rotating chair positioner to treat patients of head and neck cancer at upright seated position with multiple nonplanar fields in a fixed carbon-ion beamline. Med. Phys. 47, 2450–2460 (2020).
Sheng, Y. et al. Performance of a 6D treatment chair for patient positioning in an upright posture for fixed ion beam lines. Front. Oncol. 10, 213 (2020).
Cornforth, M. N. Occam’s broom and the dirty DSB: cytogenetic perspectives on cellular response to changes in track structure and ionization density. Int. J. Radiat. Biol. 97, 1099–1108 (2020).
Stannard, C. et al. Malignant salivary gland tumours: can fast neutron therapy results point the way to carbon ion therapy? Radiother. Oncol. 109, 262–268 (2013).
Parker, C. et al. Targeted alpha therapy, an emerging class of cancer agents. JAMA Oncol. 4, 1765–1772 (2018).
Durante, M., Orecchia, R. & Loeffler, J. S. Charged-particle therapy in cancer: clinical uses and future perspectives. Nat. Rev. Clin. Oncol. 14, 483–495 (2017).
Blakely, E. A. The 20th Gray lecture 2019: health and heavy ions. Br. J. Radiol. 93, 20200172 (2020).
Fowler, J. F. 21 years of biologically effective dose. Br. J. Radiol. 83, 554–568 (2010).
Friedrich, T., Scholz, U., Elsässer, T., Durante, M. & Scholz, M. Systematic analysis of RBE and related quantities using a database of cell survival experiments with ion beam irradiation. J. Radiat. Res. 54, 494–514 (2013).
Wang, J. Z., Huang, Z., Lo, S. S., Yuh, W. T. C. & Mayr, N. A. A generalized linear-quadratic model for radiosurgery, stereotactic body radiation therapy, and high-dose rate brachytherapy. Sci. Transl. Med. 2, 39ra48 (2010).
Takahashi, Y. et al. Heavy ion irradiation inhibits in vitro angiogenesis even at sublethal dose. Cancer Res. 63, 4253–4257 (2003).
Liu, Y. et al. Effects of carbon-ion beam irradiation on the angiogenic response in lung adenocarcinoma A549 cells. Cell Biol. Int. 38, 1304–1310 (2014).
Konings, K., Vandevoorde, C., Baselet, B., Baatout, S. & Moreels, M. Combination therapy with charged particles and molecular targeting: a promising avenue to overcome radioresistance. Front. Oncol. 10, 128 (2020).
Durante, M., Brenner, D. J. & Formenti, S. C. Does heavy ion therapy work through the immune system? Int. J. Radiat. Oncol. Biol. Phys. 96, 934–936 (2016).
Wulf, H. et al. Heavy-ion effects on mammalian cells: inactivation measurements with different cell lines. Radiat. Res. 104, 122–134 (1985).
ICRU Report 93: Prescribing, Recording, and Reporting Light Ion Beam Therapy. J. ICRU 16 (2016).
Inaniwa, T. et al. Treatment planning for a scanned carbon beam with a modified microdosimetric kinetic model. Phys. Med. Biol. 55, 6721–6737 (2010).
Grün, R. et al. Impact of enhancements in the local effect model (LEM) on the predicted RBE-weighted target dose distribution in carbon ion therapy. Phys. Med. Biol. 57, 7261–7274 (2012).
Tommasino, F. & Durante, M. Proton radiobiology. Cancers 7, 353–381 (2015).
Paganetti, H. Relative biological effectiveness (RBE) values for proton beam therapy. Variations as a function of biological endpoint, dose, and linear energy transfer. Phys. Med. Biol. 59, R419–R472 (2014).
Mutter, R. W. et al. Incorporation of biologic response variance modeling into the clinic: limiting risk of brachial plexopathy and other late effects of breast cancer proton beam therapy. Pract. Radiat. Oncol. 10, e71–e81 (2020).
Zhang, L., Wang, W., Hu, J., Lu, J. & Kong, L. RBE-weighted dose conversions for patients with recurrent nasopharyngeal carcinoma receiving carbon-ion radiotherapy from the local effect model to the microdosimetric kinetic model. Radiat. Oncol. 15, 277 (2020).
Wang, W. et al. RBE-weighted dose conversions for carbon ionradiotherapy between microdosimetric kinetic model and local effect model for the targets and organs at risk in prostate carcinoma. Radiother. Oncol. 144, 30–36 (2020).
Molinelli, S. et al. Dose prescription in carbon ion radiotherapy: How to compare two different RBE-weighted dose calculation systems. Radiother. Oncol. 120, 307–312 (2016).
Fossati, P., Matsufuji, N., Kamada, T. & Karger, C. P. Radiobiological issues in prospective carbon ion therapy trials. Med. Phys. 45, e1096–e1110 (2018).
Friedrich, T., Scholz, U., Durante, M. & Scholz, M. RBE of ion beams in hypofractionated radiotherapy (SBRT). Phys. Med. 30, 588–591 (2014).
Yoshida, Y. et al. Evaluation of therapeutic gain for fractionated carbon-ion radiotherapy using the tumor growth delay and crypt survival assays. Radiother. Oncol. 117, 351–357 (2015).
Chapman, J. D. Can the two mechanisms of tumor cell killing by radiation be exploited for therapeutic gain? J. Radiat. Res. 55, 2–9 (2014).
Laine, A. M. et al. The role of hypofractionated radiation therapy with photons, protons, and heavy ions for treating extracranial lesions. Front. Oncol. 5, 302 (2016).
Barker, H. E., Paget, J. T. E., Khan, A. A. & Harrington, K. J. The tumour microenvironment after radiotherapy: mechanisms of resistance and recurrence. Nat. Rev. Cancer 15, 409–425 (2015).
Strigari, L., Benassi, M., Sarnelli, A., Polico, R. & D’Andrea, M. A modified hypoxia-based TCP model to investigate the clinical outcome of stereotactic hypofractionated regimes for early stage non-small-cell lung cancer (NSCLC). Med. Phys. 39, 4502–4514 (2012).
Toma-Dasu, I., Sandström, H., Barsoum, P. & Dasu, A. To fractionate or not to fractionate? That is the question for the radiosurgery of hypoxic tumors. J. Neurosurg. 121, 110–115 (2014).
McKeown, S. R. Defining normoxia, physoxia and hypoxia in tumours — implications for treatment response. Br. J. Radiol. 87, 20130676 (2014).
Furusawa, Y. et al. Inactivation of aerobic and hypoxic cells from three different cell lines by accelerated (3)He-, (12)C- and (20)Ne-ion beams. Radiat. Res. 154, 485–496 (2000).
Tinganelli, W. et al. Kill-painting of hypoxic tumours in charged particle therapy. Sci. Rep. 5, 17016 (2015).
Grassberger, C., Ellsworth, S. G., Wilks, M. Q., Keane, F. K. & Loeffler, J. S. Assessing the interactions between radiotherapy and antitumour immunity. Nat. Rev. Clin. Oncol. 16, 729–745 (2019).
Durante, M. et al. X-rays vs. carbon-ion tumor therapy: cytogenetic damage in lymphocytes. Int. J. Radiat. Oncol. Biol. Phys. 47, 793–798 (2000).
Durante, M. & Formenti, S. Harnessing radiation to improve immunotherapy: better with particles? Br. J. Radiol. 93, 20190224 (2020).
Davuluri, R. et al. Lymphocyte nadir and esophageal cancer survival outcomes after chemoradiation therapy. Int. J. Radiat. Oncol. 99, 128–135 (2017).
Mohan, R. et al. Proton therapy reduces the likelihood of high-grade radiation-induced lymphopenia in glioblastoma patients: phase II randomized study of protons vs photons. Neuro. Oncol. 23, 284–294 (2021).
Kim, N. et al. Proton beam therapy reduces the risk of severe radiation-induced lymphopenia during chemoradiotherapy for locally advanced non-small cell lung cancer: a comparative analysis of proton versus photon therapy. Radiother. Oncol. 156, 166–173 (2021).
Takahashi, Y. et al. Carbon ion irradiation enhances the antitumor efficacy of dual immune checkpoint blockade therapy both for local and distant sites in murine osteosarcoma. Oncotarget 10, 633–646 (2019).
Helm, A. et al. Reduction of lung metastases in a mouse osteosarcoma model treated with carbon ions and immune checkpoint inhibitors. Int. J. Radiat. Oncol. 109, 594–602 (2021).
Marcus, D. et al. Charged particle and conventional radiotherapy: current implications as partner for immunotherapy. Cancers 13, 1468 (2021).
Friedrich, T., Henthorn, N. & Durante, M. Modeling radioimmune response — current status and perspectives. Front. Oncol. 11, 647272 (2021).
Wang, Z. et al. Charged particle radiation therapy for uveal melanoma: a systematic review and meta-analysis. Int. J. Radiat. Oncol. 86, 18–26 (2013).
Mishra, K. K. et al. Long-term results of the UCSF-LBNL randomized trial: charged particle with helium ion versus iodine-125 plaque therapy for choroidal and ciliary body melanoma. Int. J. Radiat. Oncol. Biol. Phys. 92, 376–383 (2015).
Kamada, T. et al. Carbon ion radiotherapy in Japan: an assessment of 20 years of clinical experience. Lancet Oncol. 16, e93–e100 (2015).
Shinoto, M. et al. Carbon ion radiation therapy with concurrent gemcitabine for patients with locally advanced pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys. 95, 498–504 (2016).
Kawashiro, S. et al. Multi-institutional study of carbon-ion radiotherapy for locally advanced pancreatic cancer: Japan Carbon-ion Radiation Oncology Study Group (J-CROS) study 1403 pancreas. Int. J. Radiat. Oncol. 101, 1212–1221 (2018).
Nevala-Plagemann, C., Hidalgo, M. & Garrido-Laguna, I. From state-of-the-art treatments to novel therapies for advanced-stage pancreatic cancer. Nat. Rev. Clin. Oncol. 17, 108–123 (2020).
Yamasaki, A., Yanai, K. & Onishi, H. Hypoxia and pancreatic ductal adenocarcinoma. Cancer Lett. 484, 9–15 (2020).
Ho, W. J., Jaffee, E. M. & Zheng, L. The tumour microenvironment in pancreatic cancer — clinical challenges and opportunities. Nat. Rev. Clin. Oncol. 17, 527–540 (2020).
Huart, C., Chen, J., Le Calvé, B., Michiels, C. & Wéra, A.-C. Could protons and carbon ions be the silver bullets against pancreatic cancer? Int. J. Mol. Sci. 21, 4767 (2020).
Liermann, J. et al. Carbon ion radiotherapy in pancreatic cancer: a review of clinical data. Radiother. Oncol. 147, 145–150 (2020).
Dreher, C., Habermehl, D., Jäkel, O. & Combs, S. E. Effective radiotherapeutic treatment intensification in patients with pancreatic cancer: higher doses alone, higher RBE or both? Radiat. Oncol. 12, 203 (2017).
Shinoto, M. et al. Carbon-ion radiotherapy for locally recurrent rectal cancer: Japan Carbon-ion Radiation Oncology Study Group (J-CROS) study 1404 rectum. Radiother. Oncol. 132, 236–240 (2019).
Cai, X. et al. The role of carbon ion radiotherapy for unresectable locally recurrent rectal cancer: a single institutional experience. Radiat. Oncol. 15, 209 (2020).
Habermehl, D. et al. Reirradiation using carbon ions in patients with locally recurrent rectal cancer at HIT: first results. Ann. Surg. Oncol. 22, 2068–2074 (2015).
Guren, M. G. et al. Reirradiation of locally recurrent rectal cancer: a systematic review. Radiother. Oncol. 113, 151–157 (2014).
Venkatesulu, B. P., Giridhar, P., Malouf, T. D., Trifletti, D. M. & Krishnan, S. A systematic review of the role of carbon ion radiation therapy in recurrent rectal cancer. Acta Oncol. 59, 1218–1223 (2020).
Imada, H. et al. Comparison of efficacy and toxicity of short-course carbon ion radiotherapy for hepatocellular carcinoma depending on their proximity to the porta hepatis. Radiother. Oncol. 96, 231–235 (2010).
Qi, W.-X., Fu, S., Zhang, Q. & Guo, X.-M. Charged particle therapy versus photon therapy for patients with hepatocellular carcinoma: a systematic review and meta-analysis. Radiother. Oncol. 114, 289–295 (2015).
Habermehl, D. et al. Hypofractionated carbon ion therapy delivered with scanned ion beams for patients with hepatocellular carcinoma–feasibility and clinical response. Radiat. Oncol. 8, 59 (2013).
Shibuya, K. et al. A feasibility study of high-dose hypofractionated carbon ion radiation therapy using four fractions for localized hepatocellular carcinoma measuring 3 cm or larger. Radiother. Oncol. 132, 230–235 (2019).
Chauvel, P. Osteosarcomas and adult soft tissue sarcomas: is there a place for high LET radiation therapy? Ann. Oncol. 3, S107–S110 (1992).
Strander, H., Turesson, I. & Cavallin-ståhl, E. A systematic overview of radiation therapy effects in soft tissue sarcomas. Acta Oncol. 42, 516–531 (2003).
Weber, D. C. et al. Profile of European proton and carbon ion therapy centers assessed by the EORTC facility questionnaire. Radiother. Oncol. 124, 185–189 (2017).
Matsunobu, A. et al. Impact of carbon ion radiotherapy for unresectable osteosarcoma of the trunk. Cancer 118, 4555–4563 (2012).
Kamada, T. et al. Efficacy and safety of carbon ion radiotherapy in bone and soft tissue sarcomas. J. Clin. Oncol. 20, 4466–4471 (2002).
Cuccia, F. et al. Outcome and toxicity of carbon ion radiotherapy for axial bone and soft tissue sarcomas. Anticancer Res. 40, 2853–2859 (2020).
Seidensaal, K. et al. The role of combined ion-beam radiotherapy (CIBRT) with protons and carbon ions in a multimodal treatment strategy of inoperable osteosarcoma. Radiother. Oncol. 159, 8–16 (2021).
Uhl, M. et al. Highly effective treatment of skull base chordoma with carbon ion irradiation using a raster scan technique in 155 patients: first long-term results. Cancer 120, 3410–3417 (2014).
Mattke, M. et al. High control rates of proton- and carbon-ion-beam treatment with intensity-modulated active raster scanning in 101 patients with skull base chondrosarcoma at the Heidelberg Ion Beam Therapy Center. Cancer 124, 2036–2044 (2018).
Nikoghosyan, A. V. et al. Randomised trial of proton vs. carbon ion radiation therapy in patients with low and intermediate grade chondrosarcoma of the skull base, clinical phase III study. BMC Cancer 10, 606 (2010).
Cramer, J. D., Burtness, B., Le, Q. T. & Ferris, R. L. The changing therapeutic landscape of head and neck cancer. Nat. Rev. Clin. Oncol. 16, 669–683 (2019).
Akbaba, S. et al. Bimodal radiotherapy with active raster-scanning carbon ion radiotherapy and intensity-modulated radiotherapy in high-risk nasopharyngeal carcinoma results in excellent local control. Cancers 11, 379 (2019).
Shirai, K. et al. Prospective observational study of carbon-ion radiotherapy for non-squamous cell carcinoma of the head and neck. Cancer Sci. 108, 2039–2044 (2017).
Högerle, B. A. et al. Primary adenoid cystic carcinoma of the trachea: clinical outcome of 38 patients after interdisciplinary treatment in a single institution. Radiat. Oncol. 14, 117 (2019).
Kong, L. et al. Phase I/II trial evaluating carbon ion radiotherapy for salvaging treatment of locally recurrent nasopharyngeal carcinoma. J. Cancer 7, 774–783 (2016).
Baumann, B. C. et al. Comparative effectiveness of proton vs photon therapy as part of concurrent chemoradiotherapy for locally advanced cancer. JAMA Oncol. 6, 237–246 (2020).
Li, X. et al. Toxicity profiles and survival outcomes among patients with nonmetastatic nasopharyngeal carcinoma treated with intensity-modulated proton therapy vs intensity-modulated radiation therapy. JAMA Netw. Open 4, e2113205 (2021).
Gondi, V., Yock, T. I. & Mehta, M. P. Proton therapy for paediatric CNS tumours — improving treatment-related outcomes. Nat. Rev. Neurol. 12, 334–345 (2016).
Newhauser, W. D. & Durante, M. Assessing the risk of second malignancies after modern radiotherapy. Nat. Rev. Cancer 11, 438–448 (2011).
Rieber, J. G. et al. Treatment tolerance of particle therapy in pediatric patients. Acta Oncol. 54, 1049–1055 (2015).
Mohamad, O. et al. Risk of subsequent primary cancers after carbon ion radiotherapy, photon radiotherapy, or surgery for localised prostate cancer: a propensity score-weighted, retrospective, cohort study. Lancet Oncol. 20, 674–685 (2019).
Ohno, T. & Okamoto, M. Carbon ion radiotherapy as a treatment modality for paediatric cancers. Lancet Child Adolesc. Health 3, 371–372 (2019).
Knäusl, B., Fuchs, H., Dieckmann, K. & Georg, D. Can particle beam therapy be improved using helium ions? – A planning study focusing on pediatric patients. Acta Oncol. 55, 751–759 (2016).
Horst, F. et al. Physical characterization of 3He ion beams for radiotherapy and comparison with 4He. Phys. Med. Biol. 66, 095009 (2021).
Tommasino, F., Scifoni, E. & Durante, M. New ions for therapy. Int. J. Part. Ther. 2, 428–438 (2015).
Scifoni, E. et al. Including oxygen enhancement ratio in ion beam treatment planning: model implementation and experimental verification. Phys. Med. Biol. 58, 3871–3895 (2013).
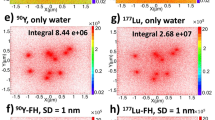
Sokol, O. et al. Oxygen beams for therapy: advanced biological treatment planning and experimental verification. Phys. Med. Biol. 62, 7798–7813 (2017).
Hagiwara, Y. et al. Influence of dose-averaged linear energy transfer on tumour control after carbon-ion radiation therapy for pancreatic cancer. Clin. Transl. Radiat. Oncol. 21, 19–24 (2020).
Matsumoto, S. et al. Unresectable chondrosarcomas treated with carbon ion radiotherapy: relationship between dose-averaged linear energy transfer and local recurrence. Anticancer Res. 40, 6429–6435 (2020).
Bassler, N. et al. LET-painting increases tumour control probability in hypoxic tumours. Acta Oncol. 53, 25–32 (2014).
Bassler, N., Jäkel, O., Søndergaard, C. S. & Petersen, J. B. Dose- and LET-painting with particle therapy. Acta Oncol. 49, 1170–1176 (2010).
Ebner, D. K., Frank, S. J., Inaniwa, T., Yamada, S. & Shirai, T. The emerging potential of multi-ion radiotherapy. Front. Oncol. 11, 624786 (2021).
Inaniwa, T., Kanematsu, N., Noda, K. & Kamada, T. Treatment planning of intensity modulated composite particle therapy with dose and linear energy transfer optimization. Phys. Med. Biol. 62, 5180–5197 (2017).
Horsman, M. R. et al. Imaging hypoxia to improve radiotherapy outcome. Nat. Rev. Clin. Oncol. 9, 674–687 (2012).
Mazal, A. et al. FLASH and minibeams in radiation therapy: the effect of microstructures on time and space and their potential application to protontherapy. Br. J. Radiol. 93, 20190807 (2020).
Favaudon, V. et al. Ultrahigh dose-rate FLASH irradiation increases the differential response between normal and tumor tissue in mice. Sci. Transl. Med. 6, 245ra93 (2014).
Vozenin, M. C. et al. The advantage of FLASH radiotherapy confirmed in mini-pig and cat-cancer patients. Clin. Cancer Res. 25, 35–42 (2019).
Montay-Gruel, P. et al. Hypofractionated FLASH-RT as an effective treatment against glioblastoma that reduces neurocognitive side effects in mice. Clin. Cancer Res. 27, 775–784 (2021).
Di Martino, F. et al. FLASH radiotherapy with electrons: issues related to the production, monitoring, and dosimetric characterization of the beam. Front. Phys. 8, 570697 (2020).
Jolly, S., Owen, H., Schippers, M. & Welsch, C. Technical challenges for FLASH proton therapy. Phys. Med. 78, 71–82 (2020).
Zakaria, A. M. et al. Ultra-high dose-rate, pulsed (FLASH) radiotherapy with carbon ions: generation of early, transient, highly oxygenated conditions in the tumor environment. Radiat. Res. 194, 587–593 (2020).
Vozenin, M.-C., Montay-Gruel, P., Limoli, C. & Germond, J.-F. All irradiations that are ultra-high dose rate may not be FLASH: the critical importance of beam parameter characterization and in vivo validation of the FLASH effect. Radiat. Res. 194, 571–572 (2020).
Rothwell, B. C. et al. Determining the parameter space for effective oxygen depletion for FLASH radiation therapy. Phys. Med. Biol. 66, 055020 (2021).
Chaudhary, P. et al. Radiobiology experiments with ultra-high dose rate laser-driven protons: methodology and state-of-the-art. Front. Phys. 9, 624963 (2021).
Bourhis, J. et al. Treatment of a first patient with FLASH-radiotherapy. Radiother. Oncol. 139, 18–22 (2019).
Pratx, G. & Kapp, D. S. A computational model of radiolytic oxygen depletion during FLASH irradiation and its effect on the oxygen enhancement ratio. Phys. Med. Biol. 64, 185005 (2019).
Labarbe, R., Hotoiu, L., Barbier, J. & Favaudon, V. A physicochemical model of reaction kinetics supports peroxyl radical recombination as the main determinant of the FLASH effect. Radiother. Oncol. 153, 303–310 (2020).
Jansen, J. et al. Does FLASH deplete oxygen? Experimental evaluation for photons, protons, and carbon ions. Med. Phys. 48, 3982–3990 (2021).
Boscolo, D., Scifoni, E., Durante, M., Krämer, M. & Fuss, M. C. May oxygen depletion explain the FLASH effect? A chemical track structure analysis. Radiother. Oncol. 162, 68–75 (2021).
Weber, U., Scifoni, E. & Durante, M. FLASH radiotherapy with carbon ion beams. Med. Phys. https://doi.org/10.1002/mp.15135 (2021).
Schültke, E. et al. Microbeam radiation therapy — grid therapy and beyond: a clinical perspective. Br. J. Radiol. 90, 20170073 (2017).
Lamirault, C. et al. Short and long-term evaluation of the impact of proton minibeam radiation therapy on motor, emotional and cognitive functions. Sci. Rep. 10, 13511 (2020).
Billena, C. & Khan, A. J. A current review of spatial fractionation: back to the future. Int. J. Radiat. Oncol. 104, 177–187 (2019).
Dilmanian, F. A. et al. Interlaced x-ray microplanar beams: a radiosurgery approach with clinical potential. Proc. Natl Acad. Sci. USA 103, 9709–9714 (2006).
Dilmanian, F. A. et al. Interleaved carbon minibeams: an experimental radiosurgery method with clinical potential. Int. J. Radiat. Oncol. Biol. Phys. 84, 514–519 (2012).
González, W. & Prezado, Y. Spatial fractionation of the dose in heavy ions therapy: an optimization study. Med. Phys. 45, 2620–2627 (2018).
Prezado, Y. et al. A potential renewed use of very heavy ions for therapy: neon minibeam radiation therapy. Cancers 12, 1356 (2021).
Kirkby, K. J. et al. Heavy charged particle beam therapy and related new radiotherapy technologies: the clinical potential, physics and technical developments required to deliver benefit for patients with cancer. Br. J. Radiol. 93, 20200247 (2020).
Kramer, M. et al. Helium ions for radiotherapy? Physical and biological verifications of a novel treatment modality. Med. Phys. 43, 1995–2004 (2016).
Acknowledgements
The authors thank Uli Weber, Emanuele Scifoni, Olga Sokol, Daria Boscolo, Burkhard Jakob, Anastasiia Quarz, Koji Noda and Elena Benedetto for their precious assistance in the preparation of the figures. The research activities at GSI and Heidelberg Ion Beam Therapy Center (HIT) are partly supported by the EU Horizon 2020 research and innovation programme under grant agreement no. 101008548 (HITRIplus). Projects on innovative beam delivery at GSI are supported by ERC advanced grant 2020 number 883425 (BARB).
Review criteria
The authors searched PubMed and Scopus using the keywords ‘heavy ions’, ‘carbon ions’, ‘clinical trials’ and ‘comparative’, and selected the period from 2016, considering our previous reviews on the topic21,83. We also searched the ClinicalTrials.gov website with the keywords ‘heavy ions’, ‘carbon ions’, ‘comparative’, ‘randomized’ and ‘phase III’. The website www.ptcog.ch was used for the latest statistics on particle therapy.
Author information
Authors and Affiliations
Contributions
M.D. produced the first draft. J.D. and J.S.L. worked on the biological and clinical sections. All authors edited and modified the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.D. has no conflict of interest. J.S.L. is co-chair of the medical advisory board at Mevion. J.D. received grants from several companies and attended advisory board meetings of Merck KGaA (Darmstadt).
Additional information
Peer review information
Nature Reviews Physics thanks Hywel Owen, Eleanor Blakely and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
42254_2021_368_MOESM1_ESM.mp4
Supplementary video 1 | Track structure in biology. A heavy ion track (uranium 750 MeV/n), simulated with the Monte Carlo code TRAX, is overlaid to a live cell imaging movie of U2OS osteosarcoma cells labeled with NBS1-GFP protein. NBS1 (Nijmegen breakage syndrome) is a gene involved in DNA double strand break (DSB) repair. While in the simulation every dot correspond to a ionization event, in the movie the accumulation of the fluorescent protein (time lapse 0-15 min) correspond to the protein recruitment to sites of DNA DSBs, clearly along the track- However, high-energy electrons (δ-rays) are also produced by high-energy heavy ions, and they can hit neighboring cells, as shown in the bottom nucleus, where sporadic DSBs are evident. Movie from the GSI collection, distributed with permission.
42254_2021_368_MOESM2_ESM.mp4
Supplementary video 2 | Differences in the DNA lesion distribution between X-rays and heavy ions. The live cell imaging movies show human osteosarcoma U2OS cells irradiated labelled with (A) 53BP1-GFP or (B) NBS1-GFP and exposed to (A) X-rays or (B) heavy ions (two separate iron ions 1 GeV/n). Both 53BP1 and NBS1 are involved in DNA DSB repair. The movie shows the fast recruitment of the repair proteins to the DNA DSB sites that are uniformly distributed in the nucleus after X-rays (A), but mostly distributed along the tracks for heavy ions (B). Movie from the GSI collection, distributed with permission.
42254_2021_368_MOESM3_ESM.mp4
Supplementary video 3 | The principle of pencil beam scanning in particle therapy. The therapy is divided in thin slices, and every slice is scanned with a small pencil beam using magnetic deflection in the XY plane. Changing the energy, the beam is moved to the next slice on the Z-axis, and scanned again. Movie produced by GSI press office, distributed with permission.
Glossary
- Hypoxia
-
Reduced oxygen supply in a tissue compared with the normal level (normoxia or physioxia). Tumours are typically hypoxic.
- Linear energy transfer
-
Energy loss of charged particles per unit track length (see Eq. 1).
- Entrance channel
-
The normal tissue volume traversed by the therapeutic beam before reaching the target region (tumour).
- Spread-out Bragg peak
-
The monoenergetic beam Bragg peak is too narrow to cover a tumour volume. It must, therefore, be enlarged to provide a uniform biological dose to the target volume.
- Track structure
-
The complete set of ionizations and excitation events caused by a charged particle traversing a medium. Energy is deposited either directly by the traversing ion or by the high-energy electrons emitted by target atom ionization (δ-rays — see Supplementary Video 1).
- Conformal radiotherapy
-
A delivery system that shapes the radiation beams to match the shape of the tumour.
- Straggling
-
Variation in the range of a particle beam caused by the stochastic nature of the energy loss process.
- Dose halo
-
Energy deposited due to scattering in the volume immediately surrounding the target.
- Treatment planning
-
The calculation of the optimal beam directions, energies and intensities to achieve the highest possible dose to the tumour while sparing organs at risk and reducing unnecessary dose to the normal tissue.
- Hypofractionation
-
Reduction of the number of fractions and increase of the dose per fraction compared with the conventional radiotherapy scheme (2 Gy per fraction in 20–30 fractions, one fraction per day).
- Gyroradius
-
Radius of the circular motion of a charged particle in the presence of a uniform magnetic field.
- Rigidity
-
Impact of the magnetic field on the trajectory of a charged particle (Eq. 5).
- Passive modulation systems
-
Systems to produce spread-out Bragg peak from a monoenergetic beam using passive scatterers with different techniques, such as a rotating wheel of different techniques or a scatterer with a collimator and a patient-specific compensator.
- Targeted radioimmunotherapy
-
Cancer therapy that uses a targeting construct (e.g. antibody, peptides or nanoparticles), attached to a radionuclide, to deliver a systemic cytotoxic dose of radiation to malignant tissue.
- Reoxygenation
-
Hypoxic sub-volumes in cancers are radioresistant. During the interval between fractions, the blood can reach the hypoxic niches that survived the previous fraction, making them radiosensitive.
- Second cancers
-
Malignant neoplasias induced by the treatment to a primary tumour.
Rights and permissions
About this article
Cite this article
Durante, M., Debus, J. & Loeffler, J.S. Physics and biomedical challenges of cancer therapy with accelerated heavy ions. Nat Rev Phys 3, 777–790 (2021). https://doi.org/10.1038/s42254-021-00368-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42254-021-00368-5
This article is cited by
-
Innovative approaches to enhance high-LETd tumor targeting in carbon ion radiotherapy
Health and Technology (2024)
-
Quasi-real-time range monitoring by in-beam PET: a case for 15O
Scientific Reports (2023)
-
High-LET charged particles: radiobiology and application for new approaches in radiotherapy
Strahlentherapie und Onkologie (2023)
-
Carbon ion radiotherapy combined with immunotherapy: synergistic anti-tumor efficacy and preliminary investigation of ferroptosis
Cancer Immunology, Immunotherapy (2023)
-
Ways to unravel the clinical potential of carbon ions for head and neck cancer reirradiation: dosimetric comparison and local failure pattern analysis as part of the prospective randomized CARE trial
Radiation Oncology (2022)