Abstract
Health promotion interventions offer great potential in advocating a healthy lifestyle and the prevention of diseases. Some barriers to communicating health promotion to people of certain cultural groups might be overcome via the internet- and mobile-based interventions (IMI). This systematic review and meta-analysis aims to explore the effectiveness of culturally adapted IMI for health promotion interventions among culturally diverse populations. We systematically searched on Cochrane Central Register of Controlled Trials (CENTRAL), EbscoHost/MEDLINE, Ovid/Embase, EbscoHost/PsychINFO, and Web of Science databases in October 2020. Out of 9438 records, 13 randomized controlled trials (RCT) investigating culturally adapted health promotion IMI addressing healthy eating, physical activity, alcohol consumption, sexual health behavior, and smoking cessation included. From the included studies 10,747 participants were eligible. Culturally adapted IMI proved to be non-superior over active control conditions in short- (g = 0.10, [95% CI −0.19 to 0.40]) and long-term (g = 0.20, [95% CI −0.11 to 0.51]) in promoting health behavior. However, culturally adapted IMI for physical activity (k = 3, N = 296) compared to active controls yielded a beneficial effect in long-term (g = 0.48, [95%CI 0.25 to 0.71]). Adapting health promotion IMI to the cultural context of different cultural populations seems not yet to be recommendable given the substantial adaption efforts necessary and the mostly non-significant findings. However, these findings need to be seen as preliminary given the limited number of included trials with varying methodological rigor and the partly substantial between-trial heterogeneity pointing in the direction of potentially useful culturally adapted IMI which now need to be disentangled from the less promising approaches.
PROSPERO registration number: 42020152939
Similar content being viewed by others
Introduction
Health promotion interventions are an effective way of disease prevention and improving overall health1,2. Well-established approaches focus amongst others on healthy eating, exercising, avoiding excessive use of alcohol, quitting smoking, and sexual health behaviors, such as condom use3,4. Promoting these health behaviors on a large scale by using health promotion interventions might be a promising mean for reducing the burden of disease5,6,7. However, these intervention offers do not always reach or fit populations equally between and within countries8.
The reach of these interventions could be expanded globally via the internet9 using the Internet- and mobile-based interventions (IMI)10,11,12,13,14. IMI offers time and place flexibility, potential cost-effectiveness, and scalability without necessarily losing effectiveness15. Thereby, IMI could reach a diverse group of people including minorities and people of a cultural background that is not yet well covered by the established health care systems16,17,18,19. However, IMI also come with some substantial limitations, most prominently risk of low adherence and uptake20,21. In order to tackle these issues, population-related factors such as the needs and expectations of the users should be taken into account15. Tailoring the intervention content and delivery method to the target group’s culture can thus be a means for increasing engagement and effectiveness22.
Researchers in the field of health promotion are encouraged by WHO to approach their practice and research considering diverse human experience and intersectionality of various factors, including culture, gender, immigration status, and ethnicity, which may be related to lower physical and mental health23,24,25. In order to offer an acceptable and relevant health service to people of a certain cultural background, health promotion interventions could be developed from scratch with cultural sensitivity or a less resource-consuming way can, for example, be tailoring an already existing intervention for specific cultural groups26. This process is defined as cultural adaptation27. Cultural adaptation could be adopted on surface structure modifications (pairing materials and messages to apparent features of the target population such as language) or deep structure modifications (concerning intersecting effects of social, cultural, and historical variables on the target behavior)28,29. Culturally adapted face-to-face interventions are shown to be effective in smoking cessation30,31, health education, and healthy eating32. Moreover, IMI developed for ethnic minorities and underserved populations are also shown to be accepted and effective in the promotion of various health behaviors such as physical activity33 and healthy eating16.
Previous reviews included IMI for ethnic minority and historically underserved populations in developed countries22,34,35,36. However, none of them specifically examined culturally adapted IMI for health promotion. The number of studies exploring the development and dissemination of culturally adapted health promotion IMI is increasing and thus a systematic review and meta-analysis seems timely. Hence, this review aims to systematically identify culturally adapted IMI on health promotion and explore their effectiveness among populations that is different from the original intervention’s target group.
Results
All the predefined characteristics of included articles are presented in Table 1.
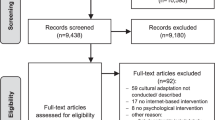
Study selection
We identified a total of 20,012 records. After screening titles and abstracts and full-texts, 13 studies were included in the quantitative analyses. The main characteristics of the studies are outlined in Table 1. During the full-text screening, 38 studies were excluded due to lack of cultural adaptation, 29 studies were concerning culturally sensitive interventions, 13 studies did not report relevant outcome data, eight studies were no original articles, four studies were not RCTs, five were excluded due to other reasons (i.e. novel interventions, study protocols, non-English full-text) and one due to a differing health promotion topic.
Study characteristics
The 13 RCTs included in this review comprise a total of N = 10,747 randomized participants, mostly adult populations (N = 9710). Trials were conducted between 2012 and 202037,38,39,40,41,42,43,44,45,46,47,48,49. The mean age of the participants varied from 14 to 57 (see Table 1). Primary studies focused on smokers (k = 3, N = 2546), individuals diagnosed with Type 2 diabetes (k = 2, N = 171), and HIV + individuals (k = 1, N = 433).
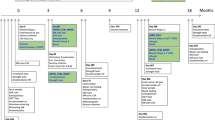
Four studies dealt with smoking cessation37,39,41,49, two with both healthy eating and physical activity38,42, three with physical activity only45,46,47, two with healthy eating only40,43, one with sexual health behavior44, and one with alcohol consumption48.
Four studies provided follow-up data on short-term effectiveness (one to five months follow-up)39,41,42,46, three studies on long-term effectiveness (six to 12-months follow-up)40,45,47, six studies provided follow-up data on both assessment points.
Seven studies were conducted in the USA38,39,43,44,45,47,48, two in China37,42, two in Brazil40,41, one in Hong Kong46, and one in Australia49.
The cultural adaptation was based on a theory or a guideline in three studies38,39,40. Eight studies based their cultural adaptation on a formative research/pilot study or expert review37,41,42,44,45,47,48,49. Two studies did not provide information regarding the basis of cultural adaptation43,46. In terms of alterations of the intervention content, four studies incorporated both surface and deep structure changes38,40,43,45, while nine studies used surface structure changes only28. Details of the culturally adapted and original interventions are presented in Table 2.
Risk of bias of in included studies
The risk of bias assessment of the included studies is presented in Figs. 1, 2. The interrater reliability suggested substantial agreement between the raters, κ = 0.79. Five studies were assessed to have a low risk of bias, five studies had some risk of bias and three studies were rated to have a high risk of bias. Four studies were assessed to have some risk of bias due to deviations from the intended intervention40,43,46,48, three studies were assessed to have some risk of bias in the measurement of the outcome domain41,44,46. Two studies37,38 were assessed to have some risk of bias due to missing outcome data, one study43 had a high risk of bias in this domain. One study was assessed to have some risk of bias arising from the randomization process40. This study had an unequal number of clusters, which resulted in significant baseline differences in primary outcomes.
Effectiveness
Nine studies that provided data to calculate standardized mean difference effect sizes were pooled. Individual data points are presented in Supplementary Table 1. Four studies concerning smoking cessation did only provide dichotomous outcomes. We conducted separate meta-analyses for the different areas of health promotion (physical activity, smoking cessation), in the case of at least three studies reported on the same outcome. Since we included only nine studies in the analysis, we refrained from exploring the publication bias via a funnel plot50. Following, we report on pooled effectiveness across health promotion domains.
The meta-analysis of six studies38,43,44,45,47,48 examining any long-term health promotion interventions revealed that culturally adapted IMI of health promotion were not superior to active control conditions in the long-term. In addition, four studies38,43,44,48 that provided short-term follow-up data were not superior to active control conditions in improving health behavior outcomes. Due to substantial heterogeneity, the results are reported descriptively, see Figs. 3, 4.
Comparisons with passive control groups could not be pooled given the low number of studies (k = 4), see Fig. 5. One study39 reported only Odds ratios ([OR], 1.13; 95% CI 0.18 to 7.04).
Due to a small number of studies (k = 9), we did not perform the predefined subgroup and sensitivity analyses.
Effectiveness of culturally adapted IMI of physical activity
Five studies reported physical activity outcomes, four of which provided data via accelerometers/pedometers38,45,47 and one via a self-reported questionnaire46. Pooling the three studies with active control conditions resulted in a small significant long-term effect favoring culturally adapted IMI (N = 296; g = 0.48; 95% CI 0.25 to 0.71; I2 = 41%; fixed effect), see Fig. 6.
Effectiveness of culturally adapted IMI of smoking cessation
Three RCTs (N = 8,112) reported smoking cessation outcomes measuring short-term abstinence at the end of the intervention versus active controls. The meta-analysis findings of these studies were not significant (Odds Ratio [OR], 1.75; 95% CI 0.51 to 6.05, I2 = 56%), see Fig. 7. The number of included studies was small (k = 3) and the effect size was mainly based on one large-scale study with N = 8000 participants37.
Effectiveness of culturally adapted IMI of healthy eating, sexual health behavior, and alcohol consumption
Fewer than three studies reported on sexual health behavior44, alcohol consumption48, and healthy eating40,43. Only one generic outcome, health-related quality of life, was reported in one trial42. These studies were not eligible for pooling due to the number of trials in the respective outcome but reported in Figs. 3–5.
Discussion
To our knowledge, this is the first systematic review and meta-analysis that assessed the effectiveness of culturally adapted IMI on health promotion among populations which the intervention was originally not developed for. Our results suggested that culturally adapted IMI are not more effective in promoting health behaviors than active conditions in short- (g = 0.10) and long-term (g = 0.20), respectively. When regarding health promotion topics separately, health promotion of physical activity resulted in a small to moderate effect favoring culturally adapted IMI over active control conditions in the long-term (g = 0.48). This is in line with a previous umbrella review of health promotion IMI for minority and historically underserved populations, which, however, not exclusively included culturally adapted IMI22. Similarly, another meta-analysis of IMI concerning physical activity did highlight the superiority of IMI over a control group or no-treatment condition, without a specific focus on culturally adapted interventions14. No other significant effect was revealed for the other addressed health promotion topics.
Subgroup analyses aiming to detangle the substantial between trial heterogeneity were not feasible. Heterogeneity among the included studies was moderate to substantial, I2 ranged from 0.36 to 0.66. Prior research points to differential effects on culturally adapted health promotion interventions in terms of different populations (age and ethnicity51), different intervention features (professional vs. non-professional provider)32, intervention duration and follow-up times in culturally adapted face-to-face interventions52, interventions focusing on general population groups53, different methodological decisions (RCT methodology use, different control groups, e.g. tailored website, no-treatment controls53) and cultural adaptation contents (inclusion of social support and/or family members51, integrating cultural beliefs and values54). There might be further possible explanations for between-study heterogeneity, and future research needs to provide a better understanding of the impact such factors have on the effectiveness of culturally adapted IMI for health promotion. The present findings are inconsistent with previous meta-analyses on IMI in several ways. Among western populations, these meta-analyses yielded positive effects favoring IMI compared to a waitlist and/or active controls (e.g. other internet-based or face-to-face interventions): for smoking cessation and abstinence outcome10,55, which is maintained at 12-month follow-up56 and higher effects achieved with the use of tailored messages10,13; healthy eating57,58,59 and weight loss60; sexual health behavior promotion61 and regarding HIV prevention and condom use62. Another meta-analysis found significant positive effects of tailored (based on personal relevance) web-based interventions on health behaviors compared to non-tailored web-based interventions53 and a different meta-analysis of SMS-based interventions on various health behavior outcomes suggested that targeted and tailored (based on demographic and psychosocial factors) SMS yielded larger effect sizes, especially for physical activity interventions (g = .51), which yielded a similar effect size to our results (g = 0.48)10. Most surprisingly in this context is our null-finding regarding the effectiveness of culturally adapted IMI compared to waitlist control conditions, which are known to provide a rather upper benchmark of the benefit of interventions63, usually associated with significantly larger between-group effect sizes in IMI for health promotion as well10,13,64. Although some of the meta-analyses mentioned above concern tailored intervention contents, none of the above-mentioned meta-analyses were specifically examining culturally adapted IMI. Therefore, our results cannot be easily compared with prior meta-analyses. However, if culturally adapted IMI for health promotion are not effective at all, even when compared to waitlist controls, we might need to challenge the idea of providing culturally adapted IMI to populations for which the intervention was originally not developed for at large and examine whether IMI developed with cultural sensitivity are effective in the same target groups. Hence, explanations for this surprisingly limited effectiveness seem warranted.
One possible explanation of our results might be related to the quality of cultural adaptation of the interventions. The cultural adaptation processes were rarely well defined in the included studies. Therefore, it was not clear whether aspects of cultural adaptation were appropriate. In addition, the high dropout among included studies could be an indicator of cultural adaptation not working as intended by the researcher. Moreover, only three studies based their cultural adaptation process on a theory, which might contribute to its quality. A tested theory of cultural adaptation of IMI is missing. However, there are guidelines developed for culturally adapting face-to-face interventions28,65 and researchers could implement these guidelines when adapting an IMI66. A recent taxonomy of cultural adaptation of IMI for mental disorders serves as a basis for future cultural adaptations of IMI67. Adopting a theoretical basis in intervention development is suggested to result in higher effects, as was shown in a meta-analysis14. However, this could not be shown in our results: only one out of the three IMI that utilized a theory of cultural adaptation resulted in an improvement in physical activity outcome38. In the future, culturally adapted intervention studies should consider supporting cultural adaption with an established theory and report the adaptation process in more detail to lead prospective cultural adaptations and replications. In the process of cultural adaptation, some of the included studies sought expert reviews, focus group feedback, and conducted a pilot study, and at least altered one aspect of the intervention. However, the majority of the changes were regarded as taking place only at the surface structure28, which might be one reason for the limited impact of culturally adapted IMI shown in the present review. Surface structure changes aim at improving feasibility while deep structure changes target program’s effect for the participants28. Implementing deep structure changes involves core cultural values of a certain population, such as beliefs towards a health issue, or performing a behavior as a member of gender identity. A meta-analysis of face-to-face culturally adapted health interventions showed that incorporating family members and religious values, which are considered as deep structure changes, in the intervention was related to improvements31. Future research should consider exploring surface versus deep structure alterations on the effectiveness of IMI e.g. in the framework of dismantling and additive clinical trial designs aiming at detangling active components and mechanisms of change of the respective interventions68,69,70,71.
Moreover, culturally adapting interventions is not free from criticism. It should be taken into account that the majority of the interventions developed in the fields of psychology and behavioral medicine are for a rather homogeneous group (white, educated, middle to high socioeconomic status) but not representative for the majority19,72. In the cultural adaptation process, the same intervention is often altered to cater to the needs of a different group of people that are non-white, occasionally less educated, and/or bilingual. This process could be seen as a form of assimilation for the target group because even the topic of the intervention might also be representative of western, white, educated humans1. Therefore, in order to avoid these issues, the first step of cultural adaption might include approaching the problem and defining it with the cultural sensitivity of its target group73. In addition, people of a certain cultural background are not homogenous within themselves, each member’s experience is affected by intersecting factors74. Therefore, it might be more complicated than often expressed to adapt an intervention for a cultural group75. One possible solution might be to invest in adapting interventions to cultural specifics of the users, e.g. based on user needs assessments76 or community leaders’ input77. Another solution, especially for migrant/immigrant populations could be developing interventions based on the target groups’ acculturation levels, i.e. a process on a spectrum of either orientation to the host culture or maintaining the native culture1,76. It seems also worthwhile to pay attention to intersecting factors that might influence a member of a cultural group, namely gender and literacy. However, we first need to establish whether to culturally adapt health promotion IMI at all. The present findings at least suggest—except for physical activity IMI—a non-favorable cost-benefit ratio, a result that still is in need of stronger evidence.
Another topic of relevance to our findings is the reach, uptake, and intervention adherence of culturally adapted IMI. Even if such IMI would be effective, they still need to be used in order to exploit their full potential. Although internet technologies are widely used globally78, there are still barriers to utilizing these technologies, which cause inequalities in accessing the internet and mobile technologies and comprehending health information16,79,80. Moreover, pure mobile-based interventions are seemingly less effective than internet-based or combined interventions81,82,83, which might also affect for instance minority populations, where they are more likely to use a smartphone to access the internet than non-minority populations where multiple device (e.g. tablets, desktops) ownership is common84. To increase adherence, multimodal content and guidance (direct contact with the provider)85 might be useful via diminishing issues of health literacy, motivational and volitional aspects, and the digital divide71,86,87. These aspects might be particularly important in people of certain cultural backgrounds living in a high-income country, people living in low-income countries, and/or vulnerable populations, such as immigrants, given the limited representation of many of these populations in the health research, and high rates of drop-out86,88,89,90,91.
This review has some limitations. First, we included interventions concerning only five prominent areas of health promotion thus results might not be generalizable to other health promotion domains. Second, the definition of cultural adaptation varies, and our operationalization of culturally adapted interventions resulted in the exclusion of studies that investigated IMI that were developed newly in a culturally sensitive way. Comparison of culturally adapted vs. culturally sensitive interventions is an interesting further research topic. Moreover, comparing culturally adapted versus culturally sensitive IMI might present insights into whether it is worthwhile to develop a novel IMI for a group or adapt an already existing one. Third, we were able to pool data from only 13 studies, which further limit the generalizability of our results. Due to this limited evidence base, analyses were restricted to the main research questions while subgroup analyses were not feasible yet. Future updates might allow for exploring the between-study heterogeneity highlighted in the present review, while the findings reported here could guide researchers in what to examine next. In this context, we suggest adding generic outcomes such as health-related quality of life, daily functioning, or self-efficacy to domain/disease-specific outcomes to allow for cross-trial cross health promotion domain comparisons in the future. Fourth, although the studies included in this meta-analysis were culturally adapted, the adaptation process was rarely well defined. Fifth, only three out of 13 studies used a theory to adapt the intervention. And last, none of the studies were comparing culturally adapted IMI to non-adapted IMI. This creates a difficulty to draw any firm conclusions about the differential effectiveness of culturally adapted interventions. Despite these limitations, this meta-analysis had some strengths. To our knowledge, this is the first meta-analysis concerning culturally adapted health promotion IMI. Moreover, this a-prior registered systematic review included mostly scientifically sound RCTs from a broad sample and health behavior topics. A summary of recommendations for future research is represented in Box 1.
Conclusion
Based on the present findings, culturally adapted IMI might not be superior compared to control conditions in the short- and long-term, except for physical activity. Although they might exhibit a more attractive health offer to their target group, their usefulness is questionable or at least need further examination. Thereby, it might be worthwhile to take into consideration intersecting aspects of experiences of people of certain cultural groups regarding health behaviors to assure acceptability and effectiveness when designing interventions and contribute to diminishing health inequalities.
Methods
Protocol and registration
This systematic review and meta-analysis has been registered at PROSPERO (Registration number: CRD 42020152939) and follows the format of the PRISMA guideline92. Review protocol93 described the aim, methodology, and data analysis plan in advance. Changes to study protocol are listed in the supplementary notes.
Eligibility criteria
Studies were included if they (1) were RCTs, (2) had no treatment, treatment as usual (TAU), placebo, waitlist, or active control conditions, (3) were delivered via the internet, (4) were culturally adapted for a population that differed from the original intervention’s target group, (5) examined a health promotion intervention on healthy eating, physical activity, alcohol consumption, sexual health behavior and/or smoking cessation (6) reported one of the respective health promotion-specific outcomes: body mass index (BMI), time spent exercising, change in condom use, level of smoking, level of alcohol consumption, or one of the following generic outcomes: health-related quality of life and self-efficacy.
Information sources and study selection
The initial search was conducted in the following databases on 26. August 2019: Cochrane Central Register of Controlled Trials (CENTRAL), EbscoHost/MEDLINE, Ovid/Embase, EbscoHost/PsychINFO, and Web of Science. A combination of keywords (including MeSH terms) indicating culturally adapted IMI for health promotion has been used. The search terms are published in this review’s protocol93 and cover comprehensively both the topic of the present review as well as one of a parallel systematic review on culturally adapted IMI for mental health conditions94,67. There were no restrictions on the publication date. A search update was conducted on 15 October 2020.
All search results were merged into Covidence95 and duplicates were automatically removed. Two reviewers screened titles and abstracts of the identified articles against the inclusion criteria and selected potentially relevant articles for the full-text screening. Full-text screening has been performed by two reviewers independently, disagreements have been solved by consensus or a third reviewer where needed. The study selection is illustrated in the PRISMA flow diagram (see Fig. 8).
Data extraction
Data extraction was conducted by two independent reviewers and then extracted data was then checked by a third reviewer. The following data were extracted from the included studies: publication details, study participants (demographics and cultural background, baseline characteristics), study design, study setting, characteristics of the original and culturally adapted intervention, health behavior-specific and generic outcome measures, information regarding cultural adaptation (content, utilization of theoretical or evidence-based components). Behavioral outcomes are defined as: physical activity measured via physical activity minutes per week with accelerometers or self-report questionnaires; healthy eating measured via BMI; alcohol consumption assessed via the level of alcohol consumption; smoking cessation assessed via the level of smoking or the abstinence percentage; sexual health behavior assessed with condom use. Generic outcomes were defined as health-related quality of life and self-efficacy, assessed by means of validated self-report questionnaires. Control conditions were categorized into active (placebo, other health promotion interventions & TAU) and passive controls (waitlist & No treatment). When related information could not be extracted, corresponding authors of the articles were contacted to obtain information. The extracted data was tabulated.
Risk of bias
Two independent reviewers performed quality assessments with Cochrane Collaboration’s Risk of Bias Tool 2.096. The RoB tool 2.0 has five domains including bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in the measurement of the outcome, bias in the selection of the reported result. A third reviewer solved disagreements following a discussion between the reviewers. The Kappa statistic was used to calculate interrater reliability97.
Meta-analysis
For each study, a standardized mean difference (SMD) and 95% confidence intervals (CI) were calculated with mean scores of intervention and control groups. In order to decrease the bias of small samples, Hedges’ g was calculated98. Effect sizes were recoded when higher scores of an outcome assessment indicated worsening results (e.g. BMI and level of alcohol consumption). For continuous outcomes, Hedges’ g and 95% CIs were reported; for dichotomous outcomes, odds ratios and CIs were reported. Random effects model was chosen for analyses due to an expected diversity among IMI of health promotion, sample size, and duration of intervention among studies99. Data were pooled to calculate a standardized mean effect size for each outcome and a forest plot with 95% CIs, in the case of at least three studies reporting the respective outcome. Otherwise, results were presented descriptively. Sensitivity analysis was planned to assess the impact of studies with a high risk of bias. Analyses were performed in R package meta and metafor, and Review Manager 5100,101,102,103. Continuous effect sizes were categorized along with Cohen’s rule of thumb with 0.20 considered a small effect, 0.50 medium effect, and 0.80 large effects104. In order to assess publication bias, we planned to conduct funnel plots.
Statistical heterogeneity among studies was analyzed with the I2 statistics97,105. Statistical heterogeneity refers to the variability among effect sizes in a meta-analysis106. However, the veracity of measures of heterogeneity is arguable; therefore, their interpretation should be made with caution97. Statistical heterogeneity was calculated with the I2 test for each outcome domain. Heterogeneity I2 ≥ 60% was regarded as substantial heterogeneity, in which case no pooled effect sizes are reported. Subgroup analyses were planned to explore possible sources of heterogeneity on population, duration of the intervention, delivery of the intervention, and presence of guidance.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data supporting the findings of this study are available within the respective articles cited in this review and from the corresponding author on reasonable request.
Code availability
Meta-analyses were conducted using the R Studio packages Meta100 and Metafor103, and Review Manager101,102. The code is publicly available in the following github repository: https://github.com/MathiasHarrer/Doing-Meta-Analysis-in-R.
References
Liu, J. J. et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: Mixed-methods evidence synthesis. Health Technology Assessment https://doi.org/10.3310/hta16440 (2012).
Cerf, M. E. Healthy lifestyles and noncommunicable diseases: nutrition, the life‐course, and health promotion. Lifestyle Med. 2, 1–12 (2021).
Preston, S. H., Stokes, A., Mehta, N. K. & Cao, B. Projecting the effect of changes in smoking and obesity on future life expectancy in the United States. Demography 51, 27–49 (2014).
World Health Organization. Sexual Health and its Linkages to Reproductive Health: an Operational Approach 1–12 (World Health Organization, 2017).
Di Cesare, M. et al. Inequalities in non-communicable diseases and effective responses. Lancet 381, 585–597 (2013).
World Health Organization. Global Status Report On Noncommunicable Diseases 2014 (World Health Organization, 2014).
World Health Organization. 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases (World Health Organization, 2013).
Friel, S. & Marmot, M. G. Action on the Social determinants of health and health inequities goes global. Annu. Rev. Public Health. https://doi.org/10.1146/annurev-publhealth-031210-101220 (2011).
Muñoz, R. F. Using evidence-based Internet interventions to reduce health disparities worldwide. J. Med. Internet Res. 12, 1–10 (2010).
Head, K. J., Noar, S. M., Iannarino, N. T. & Grant Harrington, N. Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Soc. Sci. Med. 97, 41–48 (2013).
Fiedler, J., Eckert, T., Wunsch, K. & Woll, A. Key facets to build up eHealth and mHealth interventions to enhance physical activity, sedentary behavior and nutrition in healthy subjects—an umbrella review. BMC Public Health 20, 1–21 (2020).
Müller, A. M. et al. Physical activity, sedentary behavior, and diet-related ehealth and mhealth research: Bibliometric analysis. J. Med. Internet Res. 20, e122 (2018).
Do, H. P. et al. Which eHealth interventions are most effective for smoking cessation? A systematic review. Patient Prefer. Adherence 12, 2065–2084 (2018).
Webb, T. L., Joseph, J., Yardley, L. & Michie, S. Using the Internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J. Med. Internet Res. 12, 1–18 (2010).
Muñoz, R. F. et al. Massive open online interventions: a novel model for delivering behavioral- health services worldwide. Clin. Psychol. Sci. 4, 194–205 (2016).
Vandelanotte, C. et al. Past, present, and future of ehealth and mhealth research to improve physical activity and dietary behaviors. J. Nutr. Educ. Behav. 48, 219–228.e1 (2016).
Jiang, X., Ming, W. K. & You, J. H. S. The cost-effectiveness of digital health interventions on the management of cardiovascular diseases: systematic review. J. Med. Internet Res. 21, 1–11 (2019).
Elbert, N. J. et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J. Med. Internet Res. 16, 1–23 (2014).
Henrich, J., Heine, S. J. & Norenzayan, A. Beyond WEIRD: towards a broad-based behavioral science. Behav. Brain Sci. 33, 111–135 (2010).
Lin, J., Faust, B., Ebert, D. D., Krämer, L. & Baumeister, H. A web-based acceptance-facilitating intervention for identifying patients’ acceptance, uptake, and adherence of internet- and mobile-based pain interventions: randomized controlled trial. J. Med. Internet Res. 20, e244 (2018).
Baumeister, H. et al. Impact of an acceptance facilitating intervention on diabetes patients’ acceptance of Internet-based interventions for depression: a randomized controlled trial. Diabetes Res. Clin. Pract. 105, 30–39 (2014).
Armaou, M., Araviaki, E. & Musikanski, L. eHealth and mHealth interventions for ethnic minority and historically underserved populations in developed countries: an umbrella review. Int. J. Community Well-Being 3, 193–221 (2020).
Clauss-Ehlers, C. S., Chiriboga, D. A., Hunter, S. J., Roysircar, G. & Tummala-Narra, P. APA multicultural guidelines executive summary: ecological approach to context, identity, and intersectionality. Am. Psychol. 74, 232–244 (2019).
Lewis, J. A., Williams, M. G., Peppers, E. J. & Gadson, C. A. Applying intersectionality to explore the relations between gendered racism and health among black women. J. Couns. Psychol. 64, 475–486 (2017).
World Health Organization. Promoting health in the SDGs. Report on 9th Global Conference on Health Promotion 1–37 (World Health Organization, 2016).
Barrera, M., Castro, F. G. & Steiker, L. K. H. A critical analysis of approaches to the development of preventive interventions for subcultural groups. Am. J. Community Psychol. 48, 439–454 (2011).
Bernal, G., Jiménez-Chafey, M. I., & Domenech Rodríguez, M. M. & Domenech Rodríguez Cultural adaptation of treatments: a resource for considering culture in evidence-based practice. Prof. Psychol. Res. Pract. 40, 361–368 (2009).
Resnicow, K., Soler, R., Braithwaite, R. L., Ahluwalia, J. S. & Butler, J. Cultural sensitivity in substance use prevention. J. Community Psychol. 28, 271–290 (2000).
Cardemil, E. Cultural adaptations to empirically supported treatments: a research agenda. Sci. Rev. Ment. Heal. Pract. 7, 8–21 (2010).
Liu, J. J. et al. Smoking cessation interventions for ethnic minority groups—a systematic review of adapted interventions. Prev. Med. (Balt.). 57, 765–775 (2013).
Nierkens, V. et al. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. a systematic review. PLoS ONE https://doi.org/10.1371/journal.pone.0073373 (2013).
Lambert, S. et al. The effect of culturally-adapted health education interventions among culturally and linguistically diverse (CALD) patients with a chronic illness: a meta-analysis and descriptive systematic review. Patient Educ. Couns. https://doi.org/10.1016/j.pec.2021.01.023 (2021).
Staffileno, B. A. B. A., Tangney, C. C. C. C. & Fogg, L. Favorable outcomes using an eHealth approach to promote physical activity and nutrition among young African American women. J. Cardiovasc. Nurs. 33, 62–71 (2018).
Anderson-Lewis, C., Darville, G., Mercado, R. E., Howell, S. & Di Maggio, S. mHealth technology use and implications in historically underserved and minority populations in the united states: Systematic literature review. JMIR mHealth uHealth 6, e128 (2018).
Montague, E. & Perchonok, J. Health and wellness technology use by historically underserved health consumers: Systematic review. J. Med. Internet Res. 14, e78 (2012).
Bennett, G. G. et al. Electronic health (eHealth) interventions for weight management among racial/ethnic minority adults: a systematic review. Obes. Rev. 15, 146–158 (2014).
Augustson, E. et al. Text to quit China: an mHealth smoking cessation. Trial Am. J. Health Promot. 31, 217–225 (2017).
Bender, M. S., Cooper, B. A., Park, L. G., Padash, S. & Arai, S. A feasible and efficacious mobile-phone based lifestyle intervention for Filipino Americans with type 2 diabetes: randomized controlled trial. JMIR Diabetes 2, e30 (2017).
Bowen, D. J., Henderson, P. N., Harvill, J. & Buchwald, D. Short-term effects of a smoking prevention website in American Indian youth. J. Med. Internet Res. 14, e81 (2012).
Brito Beck Da Silva, K. et al. Evaluation of the computer-based intervention program stayingfit Brazil to promote healthy eating habits: The results from a school cluster-randomized controlled trial. Int. J. Environ. Res. Public Health 16, 1–18 (2019).
Cruvinel, E., Richter, K. P., Colugnati, F. & Ronzani, T. M. An experimental feasibility study of a hybrid telephone counseling/text messaging intervention for post-discharge cessation support among hospitalized smokers in Brazil. Nicotine Tob. Res. 21, 1700–1705 (2019).
Duan, Y. P., Wienert, J., Hu, C., Si, G. Y. & Lippke, S. Web-based intervention for physical activity and fruit and vegetable intake among Chinese university students: a randomized controlled trial. J. Med. Internet Res. 19, 1–15 (2017).
Fortmann, A. L. et al. Dulce digital: An mHealth SMS based intervention improves glycemic control in hispanics with type 2 diabetes. Diabetes Care 40, 1349–1355 (2017).
Kurth, A. E. et al. Linguistic and cultural adaptation of a computer-based counseling program (CARE+ Spanish) to support HIV treatment adherence and risk reduction for people living with HIV/AIDS: a randomized controlled trial. J. Med. Internet Res. 18, e195 (2016).
Larsen, B. A. et al. Randomized trial of a physical activity intervention for Latino Men: Activo. Am. J. Prev. Med. 59, 219–227 (2020).
Lau, P. W. C., Pitkethly, A. J., Leung, B. W. C., Lau, E. Y. & Wang, J. J. The intervention effect of SMS delivery on chinese adolescent’s physical activity. Int. J. Environ. Res. Public Health 16, 1–12 (2019).
Marcus, B. H. et al. Pasos Hacia La Salud: a randomized controlled trial of an internet-delivered physical activity intervention for Latinas. Int. J. Behav. Nutr. Phys. Act. 13, 62 (2016).
Montag, A. C. et al. Preventing alcohol-exposed pregnancy among an american indian/alaska native population: effect of a screening, brief intervention, and referral to treatment intervention. Alcohol. Clin. Exp. Res. 39, 126–135 (2015).
Peiris, D. et al. A smartphone app to assist smoking cessation among aboriginal australians: findings from a pilot randomized controlled trial. JMIR mHealth uHealth 7, e12745 (2019).
Rothstein, H. R., Sutton, A. J. & Borenstein, M. Publication Bias in Meta-Analyses: Prevention, Assessment and Adjustments (John Wiley & Sons, 2005).
Rathod, S. et al. The current status of culturally adapted mental health interventions: a practice-focused review of meta-analyses. Neuropsychiatr. Dis. Treat. 14, 165–178 (2018).
Harper Shehadeh, M., Maercker, A., Heim, E., Chowdhary, N. & Albanese, E. Cultural adaptation of minimally guided interventions for common mental disorders: a systematic review and meta-analysis. JMIR Ment. Heal 3, e44 (2016).
Lustria, M. L. A. et al. A meta-analysis of web-delivered tailored health behavior change interventions. J. Health Commun. https://doi.org/10.1080/10810730.2013.768727 (2013).
Van Loon, A., Van Schaik, A., Dekker, J. & Beekman, A. Bridging the gap for ethnic minority adult outpatients with depression and anxiety disorders by culturally adapted treatments. J. Affect. Disord. 147, 9–16 (2013).
Whittaker, R. et al. Mobile phone text messaging and app‐based interventions for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD006611.pub5 (2019).
Myung, S.-K., McDonnell, D. D., Kazinets, G., Seo, H. G. & Moskowitz, J. M. Effects of web- and computer-based smoking cessation programs. Arch. Intern. Med. https://doi.org/10.1001/archinternmed.2009.109 (2009).
Joiner, K. L., Nam, S. & Whittemore, R. Lifestyle interventions based on the diabetes prevention program delivered via eHealth: a systematic review and meta-analysis. Prev. Med. (Balt.). 100, 194–207 (2017).
Rodriguez Rocha, N. P. & Kim, H. eHealth interventions for fruit and vegetable intake: a meta-analysis of effectiveness. Heal. Educ. Behav. 46, 947–959 (2019).
Kelly, J. T., Reidlinger, D. P., Hoffmann, T. C. & Campbell, K. L. Telehealth methods to deliver dietary interventions in adults with chronic disease: a systematic review and meta-analysis1,2. Am. J. Clin. Nutr. 104, 1693–1702 (2016).
Hutchesson, M. J. et al. eHealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis. Obes. Rev. 16, 376–392 (2015).
Bailey, J. V. et al. Interactive computer-based interventions for sexual health promotion. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.cd006483.pub2 (2010).
Noar, S. M., Black, H. G. & Pierce, L. B. Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. Aids 23, 107–115 (2009).
Cunningham, J. A., Kypri, K. & McCambridge, J. Exploratory randomized controlled trial evaluating the impact of a waiting list control design. BMC Med. Res. Methodol. 13, 150 (2013).
Graham, A. et al. Systematic review and meta-analysis of Internet interventions for smoking cessation among adults. Subst. Abuse Rehabil. 55. https://doi.org/10.2147/sar.s101660 (2016).
Bernal, G. & Sáez-Santiago, E. Culturally centered psychosocial interventions. J. Community Psychol. 34, 121–132 (2006).
Salamanca-Sanabria, A., Richards, D. & Timulak, L. Adapting an internet-delivered intervention for depression for a Colombian college student population: an illustration of an integrative empirical approach. Internet Inter. 15, 76–86 (2019).
Spanhel, K. et al. Cultural adaptation of internet- and mobile-based interventions for mental disorders: a systematic review. npj Digit. Med. https://doi.org/10.1038/s41746-021-00498-1 (2021).
Domhardt, M. et al. Therapeutic processes in digital interventions for anxiety: a systematic review and meta-analytic structural equation modeling of randomized controlled trials. Clin. Psychol. Rev. 90, 102084 (2021).
Domhardt, M., Cuijpers, P., Ebert, D. D. & Baumeister, H. More light? opportunities and pitfalls in digitalized psychotherapy process research. Front. Psychol. 12, 1–5 (2021).
Kazdin, A. E. Mediators and mechanisms of change in psychotherapy research. Annu. Rev. Clin. Psychol. 3, 1–27 (2007).
Domhardt, M. et al. Mediators and mechanisms of change in internet- and mobile-based interventions for depression: a systematic review. Clin. Psychol. Rev. 83, 101953 (2021).
Rad, M. S., Martingano, A. J. & Ginges, J. Toward a psychology of Homo sapiens: Making psychological science more representative of the human population. Proc. Natl Acad. Sci. USA 115, 11401–11405 (2018).
Gone, J. P. A community-based treatment for Native American historical trauma: prospects for evidence-based practice. J. Consult. Clin. Psychol. 77, 751–762 (2009).
Nagayama Hall, G. C., Yip, T. & Zárate, M. A. On becoming multicultural in a monocultural research world: a conceptual approach to studying ethnocultural diversity. Am. Psychol. 71, 40–51 (2016).
Bernal, G. & Adames, C. Cultural adaptations: conceptual, ethical, contextual, and methodological issues for working with ethnocultural and majority-world populations. Prev. Sci. 18, 681–688 (2017).
Castro, F. G., Barrera, M. & Holleran Steiker, L. K. Issues and challenges in the design of culturally adapted evidence-based interventions. Ssrn https://doi.org/10.1146/annurev-clinpsy-033109-132032 (2010).
Warne, D. & Wescott, S. Social determinants of American Indian Nutritional Health. Curr. Dev. Nutr. https://doi.org/10.1093/cdn/nzz054 (2019).
Abaza, H. & Marschollek, M. mHealth application areas and technology combinations. Methods Inf. Med. 56, e105–e122 (2017).
Hall, C. S., Fottrell, E., Wilkinson, S. & Byass, P. Assessing the impact of mHealth interventions in low- and middle-income countries—what has been shown to work? Glob. Health Action 7, 25606 (2014).
Kruse, C. et al. Barriers to the use of mobile health in improving health outcomes in developing countries: Systematic review. J. Med. Internet Res. 21, 1–13 (2019).
Weisel, K. K. et al. Standalone smartphone apps for mental health—a systematic review and meta-analysis. npj Digit. Med. 2, 1–10 (2019).
Bendig, E. et al. Internet-based interventions in chronic somatic disease. Dtsch. Arztebl. Int. 115, 659–665 (2018).
Ebert, D. D. et al. Internet- and mobile-based psychological interventions: applications, efficacy, and potential for improving mental health. Eur. Psychol. 23, 167–187 (2018).
Tsetsi, E. & Rains, S. A. Smartphone Internet access and use: extending the digital divide and usage gap. Mob. Media Commun. 5, 239–255 (2017).
Baumeister, H., Reichler, L., Munzinger, M. & Lin, J. The impact of guidance on Internet-based mental health interventions - A systematic review. Internet Inter. 1, 205–215 (2014).
Arsenijevic, J., Tummers, L. & Bosma, N. Adherence to electronic health tools among vulnerable groups: Systematic literature review and meta-analysis. J. Med. Internet Res. 22, e11613 (2020).
Aranda-Jan, C. B., Mohutsiwa-Dibe, N. & Loukanova, S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health 14, 1–15 (2014).
James, D. C., Harville, C., Sears, C., Efunbumi, O. & Bondoc, I. Participation of African Americans in e-Health and m-Health studies: a systematic review. Telemed. e-Health 23, 351–364 (2017).
Hwang, D. S. A., Lee, A., Song, J. M. & Han, H. R. Recruitment and retention strategies among racial and ethnic minorities in web-based intervention trials: retrospective qualitative analysis. J. Med. Internet Res. 23, e23959 (2021).
Callier, S. & Fullerton, S. M. Diversity and inclusion in unregulated mHealth research: addressing the risks. J. Law Med. Ethics 48, 115–121 (2020).
Druce, K. L., Dixon, W. G. & McBeth, J. Maximizing engagement in mobile health studies: lessons learned and future directions. Rheum. Dis. Clin. North Am. 45, 159–172 (2019).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 339, 332–336 (2009).
Balci, S., Spanhel, K., Sander, L. & Baumeister, H. Protocol for a systematic review and meta-analysis of culturally adapted internet- And mobile-based health promotion interventions. BMJ Open https://doi.org/10.1136/bmjopen-2020-037698 (2020).
Spanhel, K., Balci, S., Baumeister, H., Bengel, J. & Sander, L. B. Cultural adaptation of Internet- and mobile-based interventions for mental disorders: a systematic review protocol. Syst. Rev. 9, 207 (2020).
Babineau, J. Product Review: Covidence (Systematic Review Software). J. Can. Heal. Libr. Assoc./J. l’Association bibliothèques la St.é du Can. 35, 68 (2014).
Sterne, J. A. C. et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ https://doi.org/10.1136/bmj.l4898 (2019).
Higgins JPT et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. (The Cochrane Collaboration, 2011). Available at: www.handbook.cochrane.org.
Fritz, C. O., Morris, P. E. & Richler, J. J. Effect size estimates: current use, calculations, and interpretation. J. Exp. Psychol. Gen. 141, 2–18 (2012).
Tufanaru, C., Munn, Z., Stephenson, M. & Aromataris, E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int. J. Evid. Based Health. 13, 196–207 (2015).
Balduzzi, S., Rücker, G. & Schwarzer, G. How to perform a meta-analysis with R: a practical tutorial. Evid. Based Ment. Health 22, 153–160 (2019).
Harrer, M., Cuijpers, P. & Ebert, D. Doing meta-analysis in R. https://doi.org/10.5281/ZENODO.2551803 (2019).
The Nordic Cochrane Centre. Review Manager (RevMan) (The Cochrane Collaboration, 2014).
Viechtbauer, W. Conducting meta-analyses in R with the metafor. J. Stat. Softw. 36, 1–48 (2010).
Cohen, J. Statistical Power Analysis for the Behavioural Science 2nd edn. (Erlbaum Associate, 1988).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. https://doi.org/10.1002/sim.1186 (2002).
Card, N. A. Applied Meta-Analysis for Social Science Research. (Guilford, 2011).
Bender, M. S. & Clark, M. J. Cultural adaptation for ethnic diversity: a review of obesity interventions for preschool children. Calif. J. Health Promot 9, 40 (2011).
Barrera, M., Castro, F. G., Strycker, L. & Toobert, D. Cultural adaptations of behavioral health interventions: a progress report. J. Consult. Clin. Psychol. 81, 196–205 (2013).
Castro, Y. et al. Adaptation of a counseling intervention to address multiple cancer risk factors among overweight/obese latino smokers. Heal. Educ. Behav. 42, 65–72 (2015).
Philis-Tsimikas, A. et al. Improvement in diabetes care of underinsured patients enrolled in Project Dulce: A community-based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care 27, 110–115 (2004).
Acknowledgements
The authors wish to thank all contacted authors who provided the missing information. We would like to thank student assistants Fatma Cakir, Karamdeep Khinda, and Felicitas Feldhahn for their support in screening and data extraction. S.B. receives a scholarship granted by the Ministry of National Education in Turkey, K.S. is supported by the German Academic Scholarship Foundation. Open Access funding was provided by the University of Ulm. The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
S.B., K.S., L.S., and H.B. conceived the study design. S.B., K.S., and L.S. developed the search strategy, study selection, and extraction. S.B. wrote the draft of the manuscript. All authors read, provided feedback, and approved the final version. S.B. is the guarantor of the review.
Corresponding author
Ethics declarations
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Balci, S., Spanhel, K., Sander, L.B. et al. Culturally adapting internet- and mobile-based health promotion interventions might not be worth the effort: a systematic review and meta-analysis. npj Digit. Med. 5, 34 (2022). https://doi.org/10.1038/s41746-022-00569-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-022-00569-x
This article is cited by
-
Culturally adapted Turkish version of an internet-based mindfulness intervention for university students: a randomized controlled feasibility trial
BMC Digital Health (2024)
-
Needs for mobile and internet-based psychological intervention in patients with self-injury and suicide-related behaviors: a qualitative systematic review
BMC Psychiatry (2024)
-
Challenges in implementing cultural adaptations of digital health interventions
Communications Medicine (2024)
-
Safeguarding Users of Consumer Mental Health Apps in Research and Product Improvement Studies: an Interview Study
Neuroethics (2024)
-
A modern web-based health promotion program for patients in Greece with diabetes 2 and obesity: an interventional study
BMC Public Health (2023)