Abstract
Advancements in deep learning techniques carry the potential to make significant contributions to healthcare, particularly in fields that utilize medical imaging for diagnosis, prognosis, and treatment decisions. The current state-of-the-art deep learning models for radiology applications consider only pixel-value information without data informing clinical context. Yet in practice, pertinent and accurate non-imaging data based on the clinical history and laboratory data enable physicians to interpret imaging findings in the appropriate clinical context, leading to a higher diagnostic accuracy, informative clinical decision making, and improved patient outcomes. To achieve a similar goal using deep learning, medical imaging pixel-based models must also achieve the capability to process contextual data from electronic health records (EHR) in addition to pixel data. In this paper, we describe different data fusion techniques that can be applied to combine medical imaging with EHR, and systematically review medical data fusion literature published between 2012 and 2020. We conducted a systematic search on PubMed and Scopus for original research articles leveraging deep learning for fusion of multimodality data. In total, we screened 985 studies and extracted data from 17 papers. By means of this systematic review, we present current knowledge, summarize important results and provide implementation guidelines to serve as a reference for researchers interested in the application of multimodal fusion in medical imaging.
Similar content being viewed by others
Introduction
The practice of modern medicine relies heavily on synthesis of information and data from multiple sources; this includes imaging pixel data, structured laboratory data, unstructured narrative data, and in some cases, audio or observational data. This is particularly true in medical image interpretation where substantial clinical context is often essential to provide diagnostic decisions. For example, it has repeatedly been shown that a lack of access to clinical and laboratory data during image interpretation results in lower performance and decreased clinical utility for the referring provider1,2. In a survey of radiologists, the majority (87%) stated that clinical information had a significant impact on interpretation3. The importance of clinical context for accurate interpretation of imaging data is not limited to radiology; instead many other imaging-based medical specialties such as pathology, ophthalmology, and dermatology, also rely on clinical data to guide image interpretation in practice4,5,6. Pertinent and accurate information regarding the current symptoms and past medical history enables physicians to interpret imaging findings in the appropriate clinical context, leading to a more relevant differential diagnosis, a more useful report for the physicians, and optimal outcome for the patient.
In the current digital era, the volume of radiological imaging exams is growing. To meet this increased workload demand, an average radiologist may have to interpret an image every 3–4 s over an 8-h workday which contributes to fatigue, burnout, and increased error-rate7. Deep learning in healthcare is proliferating due to the potential for successful automated systems to either augment or offload cognitive work from busy physicians8,9,10. One class of deep learning, namely convolutional neural networks (CNN) has proven very effective for image recognition and classification tasks, and are therefore often applied to medical images. Early applications of CNNs for image analysis in medicine include diabetic retinopathy, skin cancer, and chest X-rays11,12,13,14,15,16,17,18. Yet, these models consider only the pixel data as a single modality for input and cannot contextualize other clinical information as would be done in medical practice, therefore may ultimately limit clinical translation.
As an example consider the “simple” task in radiology of identifying pneumonia on a chest radiograph, something that has been achieved by many investigators training deep learning models for automated detection and classification of pathologies on chest X-rays19,20. Yet without clinical context such as patient history, chief complaint, prior diagnoses, laboratory values, such applications may ultimately have limited impact on clinical practice. The imaging findings on chest X-rays consistent with pneumonia, despite having imaging features that can generally differentiate alternative diagnoses, are nonspecific and accurate diagnosis requires the context of clinical and laboratory data. In other words, the chest X-ray findings that suggest pneumonia would be accurate in one person with fever and an elevated white blood cell count but in another patient without those supporting clinical characteristics and laboratory values, similar imaging finding may instead represent other etiologies such as atelectasis, pulmonary edema, or even lung cancer. There are countless examples across different medical fields in which clinical context, typically in the form of structured and unstructured clinical data from the electronic health record (EHR), is critical for accurate and clinically relevant medical imaging interpretation. As with human physicians, automated detection and classification systems that can successfully utilize both medical imaging data together with clinical data from the EHR, such as patient demographics, previous diagnoses and laboratory values, may lead to better performing and more clinically relevant models.
Multimodal deep learning models that can ingest pixel data along with other data types (fusion) have been successful in applications outside of medicine, such as autonomous driving and video classification. As an example, a multimodal fusion detection system for autonomous vehicles, that combines visual features from cameras along with data from Light Detection and Ranging (LiDAR) sensors, is able to achieve significantly higher accuracy (3.7% improvement) than a single-modal CNN detection model21. Similarly, a multimodal social media video classification pipeline leveraging both visual and textual features increased the classification accuracy to 88.0%, well above single modality neural networks such as Google’s InceptionV3 which reached an accuracy of 76.4% on the same task22. The improvements in performance for these efforts not only echo the justification in medical applications, leveraging fusion strategies for medical imaging is also primarily motivated by the desire to integrate complementary contextual information and overcome the limitation of image-only models.
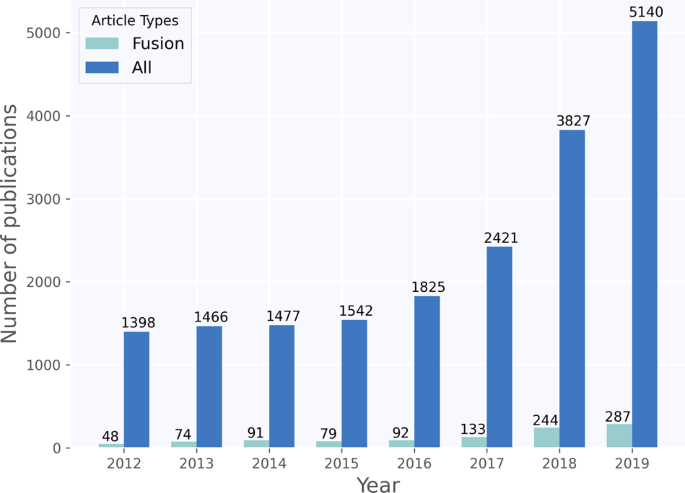
The recent medical imaging literature shows a similar trend where both EHR and pixel data are leveraged in a “fusion-paradigm” for solving complex tasks which cannot readily be tackled by a single modality (Fig. 1). The new fusion paradigm covers a wide range of methodologies and techniques with varying terms and model architectures that have not been studied systematically. The purpose of this review paper is to present a comprehensive analysis of deep learning models that leverage multiple modalities for medical imaging tasks, define and consolidate relevant terminology, and summarize the results from state-of-the-art models in relevant current literature. We hope this review can help inform future modeling frameworks and serve as a reference for researchers interested in the application of multimodal fusion in medical imaging.
Terminology and strategies in fusion
Data fusion refers to the process of joining data from multiple modalities with the aim of extracting complementary and more complete information for better performing machine learning models as opposed to using a single data modality.
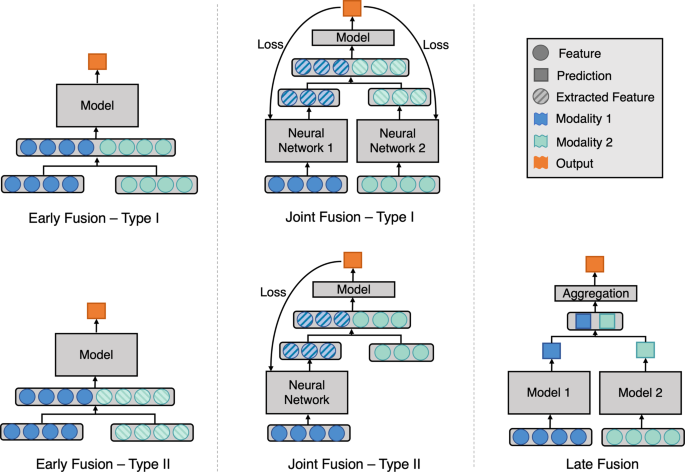
Figure 2 illustrates the three main different fusion strategies, namely early, joint, and late fusion. Here we define and describe each fusion strategy in detail:
Model architecture for different fusion strategies. Early fusion (left figure) concatenates original or extracted features at the input level. Joint fusion (middle figure) also joins features at the input level, but the loss is propagated back to the feature extracting model. Late fusion (right figure) aggregates predictions at the decision level.
Early fusion23, commonly known as feature level fusion, refers to the process of joining multiple input modalities into a single feature vector before feeding into one single machine learning model for training (Fig. 2 Early Fusion). Input modalities can be joined in many different ways, including concatenation, pooling or by applying a gated unit23,24. Fusing the original features represents early fusion type I, while fusing extracted features, either from manual extraction, imaging analysis software or learned representation from another neural network represents early fusion type II. We consider predicted probabilities to be extracted features, thus fusing features with predicted probabilities from different modalities is also early fusion type II.
Joint fusion (or intermediate fusion) is the process of joining learned feature representations from intermediate layers of neural networks with features from other modalities as input to a final model. The key difference, compared to early fusion, is that the loss is propagated back to the feature extracting neural networks during training, thus creating better feature representations for each training iteration (Fig. 2 Joint Fusion). Joint fusion is implemented with neural networks due to their ability to propagate loss from the prediction model to the feature extraction model(s). When feature representations are extracted from all modalities, we consider this joint fusion type I. However, not all input features require the feature extraction step to be defined as joint fusion (Fig. 2 Joint Fusion—Type II).
Late fusion23 refers to the process of leveraging predictions from multiple models to make a final decision, which is why it is often known as decision-level fusion (Fig. 2 Late Fusion). Typically, different modalities are used to train separate models and the final decision is made using an aggregation function to combine the predictions of multiple models. Some examples of aggregation functions include: averaging, majority voting, weighted voting or a meta-classifier based on the predictions from each model. The choice of the aggregation function is usually empirical, and it varies depending on the application and input modalities.
Results
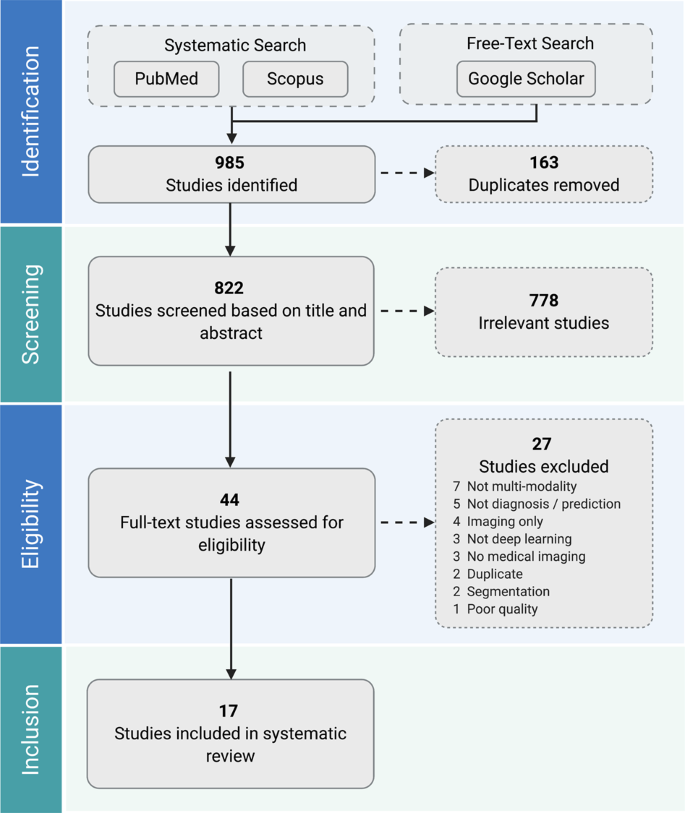
A total of 985 studies were identified through our systematic search. After removing duplicates and excluding studies based on title and abstract using our study selection criteria (see Methods), 44 studies remained for full-text screening. A total of 17 studies fulfilled our eligibility criteria and were included for systematic review and data extraction. The studies were in English except for a single paper in Chinese. Figure 3 presents a flowchart of the study screening and selection process and Table 1 displays the included studies and extracted data.
Early fusion
The majority of the studies that remained after our full-text screening (11/17) used early fusion to join the multimodal input. Thung et al.25 conducted image-image fusion of PET and MRI images using a joint fusion approach, but since they concatenated clinical and imaging features into one single feature vector before feeding into their neural network, we categorized their approach as early fusion. Six out of eleven early fusion studies extracted features from medical imaging using a CNN (Table 1). Four out of the six studies that applied neural networks for feature extraction simply concatenated the extracted imaging features with clinical features for their fusion strategy26,27,28,29. The remaining two studies by Liu et al.30 and Nie et al.31 applied dimensionality reduction techniques before concatenating the features. Five studies used software generated and/or manually extracted features from medical imaging before fusing with clinical data. Software-based feature extraction included radiomics features such as skewness and kurtosis32 or volume and thickness quantification of the regions of interest25,33. Manually extracted features included radiological assessments such as size, angle, and morphology of anatomical structures34. Out of these five studies, two applied feature selection strategies to reduce the feature dimension and improve predictive performance. The employed feature selection strategies included a rank-based method using Gini coefficients32, a filter-based method based on mutual information of the features35, and a genetic-algorithm based method35. Seven of the early fusion studies compared the performance of their fusion models against single modality models (Table 1). Six of these studies showed an improvement in performance when using fusion25,26,28,29,31,33, and the remaining one achieved the same performance but reduced standard deviation27, alluding to a model with better stability.
Joint fusion
Joint fusion was used in four out of the seventeen studies. Spasov et al.36, Yala et al.37, and Yoo et al.38 implemented CNNs to learn image features and fused these feature representations with clinical features before feeding them into a feed-forward neural network. Spasov et al. and Yala. et al. both used simple concatenation to fuse the learned imaging and clinical features. To cater to the differences between the dimensionality and dynamic range between the imaging and clinical features, Yoo et al. replicated and scaled their clinical features before fusion and they observed improvements in performances. Kawahara et al.39 also used CNNs as feature extractors for imaging modalities but experimented with a unique multimodal multi-task loss function that considers multiple combinations of the input modalities. The predicted probabilities of these multi-task outputs were aggregated for prediction, but we do not consider this late fusion since the probabilities were not from separate models. Kawahara et al., Yala et al. and Yoo et al. reported an improvement in performance using fusion compared to image-only models (Table 1). Yoo et al. further compared their joint fusion model to a late fusion model and achieved a 0.02 increase in Area Under Receiver Operating Characteristic Curve (AUROC).
Late fusion
Late fusion was used in three out of the seventeen included studies (Table 1). Each of the three late fusion papers applied a different type of aggregation strategy. Yoo et al.38 took the mean of the predicted probabilities from two single modality models as the final prediction. Reda et al.40 built another classifier using the single modality models’ prediction probabilities as inputs. Qiu et al.41 trained three independent imaging models that took as input a single MRI slice, each from a specific anatomical location. Max, mean and majority voting were applied to aggregate predictions from the three imaging models. The results from the three aggregation methods were combined again by majority voting before another round of late fusion with the clinical models. All late fusion models showed improvements in performances when compared to models that used only single modalities.
Discussion
The purpose of this review is to aggregate the collective knowledge of prior work applying multimodal deep learning fusion techniques that combine medical imaging with clinical data. We propose consistent terminology for multimodal fusion techniques and categorize prior work by fusion strategy. Overall, we found that multimodality fusion models generally led to increased accuracy (1.2–27.7%) and AUROC (0.02–0.16) over traditional single modality models for the same task. However, no single fusion strategy consistently led to optimal performance across all domains. Since our literature review shows that additional patient information and clinical context can result in better model performance, and fusion methods better replicate the human expert interpretation workflow, it is recommended to always experiment with fusion strategies when multimodal data is available.
The deep learning fusion models reviewed represent a spectrum of medical applications ranging from radiology31 to hematology29. For example, fusion strategies were often applied to the diagnosis and prediction of Alzheimer’s disease25,28,33,36,41. In clinical practice, neither imaging nor clinical data alone are sufficient for the diagnosis of Alzheimer’s disease. Leveraging deep learning fusion techniques consistently showed improvements in performance for Alzheimer’s disease diagnosis, while physicians struggle with accurate and reliable diagnostics even when multimodality is present, as proven by histopathological correlation42. This highlights the importance and utility of multimodal fusion techniques in clinical applications.
Fusion approaches in other less complex clinical applications also improved performance over single modality models, even those in which single modality models have been widely reported to achieve high performance, such as pixel-based models for automated skin cancer detection43. While the fusion approach varied widely, the consistent improvement in reported performance across a wide variety of clinical use cases suggests that model performance based on single-modal data may not represent state of the art for a given application when multimodal data are not considered.
The complexity of the non-imaging data in multimodal fusion work was limited, particularly in the context of available feature-rich and time-series data in the EHR. Instead, most studies focused primarily on basic demographic information such as age and gender25,27,39, a limited range of categorical clinical history such as hypertension or smoking status32,34 or disease-specific clinical features known to be strongly associated with the disease of interest such as APOE4 for Alzheimer’s25,28,33,36 or PSA blood test for prediction of prostate cancer40. While selecting features known to be associated with disease is meaningful, future work may further benefit from utilizing large volumes of feature-rich data, as seen in fields outside medicine such as autonomous driving44,45.
Implementation guidelines for fusion models
In most applications early fusion was used as the first attempt for multimodal learning, a straightforward approach that does not necessarily require training multiple models. However, when the input modalities are not in the same dimensions, which is typical when combining clinical data represented in 1D with imaging data in 2D or 3D, then high-level imaging features must be extracted as a 1D vector before fusing with the 1D clinical data. There were a variety of strategies used to accomplish this; including using manually extracted imaging features or software-generated features25,32,33,34,35. It is worth noting, that unless there is a compelling reason for using such an approach, outputs from linear layers of a CNN are usually effective feature representations of the original image28,29,31. This is because learned features representations often result in much better task-specific performance than can be obtained with manual or software extracted features46. Based on the reviewed papers, early fusion consistently improved performance over single modality models, and is supported by this review as an initial strategy to fuse multimodal data.
When using CNNs to extract features from imaging modalities, the same CNNs can also be used in joint fusion. However, joint fusion is implemented using neural networks which can be a limitation especially with smaller datasets better suited for traditional machine learning models. For example, if there are disproportionately few samples relative to the number of features in the dataset or if some of the input features are sparsely represented, early or late fusion is preferred because they can be implemented with traditional machine learning algorithms (e.g., Lasso and ElasticNet47) that are better suited for this type of data48. Nevertheless, joint and early fusion neural networks are both able to learn shared representations, making it easier for the model to learn correlations across modalities, thereby resulting in better performance49. Studies have also shown that fusing highly correlated features in earlier layers and less correlated features in deeper layers improve model performance50,51. In addition, we suspect that joint fusion models have the potential to outperform other fusion strategies, as the technique iteratively updates its feature representations to better complement each modality through simultaneous propagation of the loss to all feature extracting models. Yet to date, there is insufficient evidence to systematically assess this effect in fusion for medical imaging and is an important area for future exploration.
When signals from different modalities do not complement each other, that is to say input modalities separately inform the final prediction and do not have inherent interdependency, then trying a late fusion approach is preferred. This is chiefly because when feature vectors from multiple modalities are concatenated, such as in early and joint fusion, high-dimensional vectors are generated which can be difficult for machine learning models to learn without overfitting, unless a large number of input samples are available. This is the so-called “curse of dimensionality” in machine learning52,53. Late fusion mitigates this problem by utilizing multiple models that are each specialized on a single modality, thus limiting the input feature vector size for each model. For example, the quantitative result of a Mini Mental State Examination and the pixel data obtained from a brain MRI (e.g., Qiu et al.41) are largely independent data, and would therefore be suitable candidates for input into late fusion models.
Furthermore, in the common real-world scenario of missing or incomplete data, i.e. some patients have only clinical data available but no imaging data or vice-versa, late fusion retains the ability to make predictions. This is because late fusion employs separate models for separate modalities, and aggregation functions such as majority voting and averaging can be applied even when predictions from a modality is missing. When the different input modalities have very different numbers of features, predictions might be overly influenced by the most feature-rich modality (e.g., Reda et al.40). Late fusion is favorable in this scenario as it considers each modality separately. Yoo et al.38 also showed that repeating or scaling the modality that has fewer features before fusion achieved a boost in the model’s performance. Nonetheless, joint fusion can also be tuned to mitigate the difference in number of features, by setting feature producing linear layers of the feature extraction model to output a similar number of features as the other modalities. Our recommendations are summarized in Table 2.
Ideally, researchers want to first build and optimize single modality models to dually serve as baseline models and provide inputs to fusion models. Multiple fusion strategies can then be implemented to compare model performance and guide subsequent fusion experiments. Since better performance is consistently achieved with multimodal fusion techniques, routine best practice should include reporting of the systematic investigation of various fusion strategies in addition to deep learning architectures and hyperparameters.
Limitations
We devised our search string to only consider papers after 2012. This constitutes a limitation as we excluded earlier papers that applied fusion using traditional machine learning techniques or simple feed-forward neural networks. Publication bias is an important limitation since positive results can be disproportionately reported in the published literature, which may have the aggregate effect of overrepresenting the advantages of fusion techniques. Furthermore, using our study selection criteria, we only looked at fusion techniques applied to clinical prediction and diagnosis, but we recognize that fusion can be applied to other interesting medical tasks such as segmentation and registration.
As the included studies investigate different objectives, use different input modalities, report different performance metrics, and not all papers provide confidence bounds, we are not able to aggregate or statistically compare the performance gains in a meta-analysis. In addition, the reported metrics cannot always be considered valid, since some studies didn’t use an independent test-set for an unbiased performance estimate29,40. The limited number of studies per medical field and the heterogeneity of each study also makes it difficult to compare the studies qualitatively. A few studies implemented fusion in unconventional ways, which may introduce subjectivity when we classify each study into early, late, and joint fusion.
Future research
This systematic review found that multimodal fusion in medicine is a promising yet nascent field that complements the clinical practice of medical imaging interpretation across all disciplines. We have defined and summarized key terminology, techniques, and evaluated the state of the art for multimodal fusion in medical imaging, honing in on key insights and unexplored questions to guide task and modality-specific strategies. The field of multimodal fusion for deep learning in medical imaging is expanding and novel fusion methods are expected to be developed. Future work should focus on shared terminology and metrics, including direct evaluation of different multimodal fusion approaches when applicable. We found that multimodal fusion for automated medical imaging tasks broadly improves the performance over single modality models, and further work may discover additional insights to inform optimal approaches.
Methods
This systematic review was conducted based on the PRISMA guidelines54.
Search strategy
A systematic literature search was implemented in PubMed and Scopus under the supervision of a licensed librarian. The key search terms included a combination of the three major themes: ‘deep learning’, ‘multimodality fusion’, and ‘medical imaging’. Terms for segmentation, registration, and reconstruction were used as exclusion criteria in the search. The search encompassed papers published between 2012 and 2020. This range was considered appropriate due to the rise in popularity in applying CNN on medical images since the 2012 ImageNet challenge. The complete search string for both databases is provided in Supplementary Methods. For potentially eligible studies cited by articles already included in this review, additional targeted free-text searches were conducted on Google Scholar if they did not appear in Scopus or PubMed.
We included all research articles in all languages that applied deep learning models for clinical outcome prediction or diagnosis using a combination of medical imaging modalities and EHR data. Studies specific to deep learning were included rather than the broader field of machine learning because deep learning has consistently shown superior performance in image-related tasks. We selected only studies that fused medical imaging with EHR data since, unlike image-image fusion, this is an exciting new technique that effectively merges heterogeneous data types and adds complementary rather than overlapping information to inform prediction and diagnosis. We defined medical imaging modalities as any type of medical images used in clinical care. Studies that used deep learning only for feature extractions were also included for our review. We excluded any study that combined extracted imaging features with the original imaging modality, as we still considered this a single modality. Articles that fused multimodal data for segmentation, registration or reconstruction were also excluded due to our criteria for outcome prediction and diagnosis. Articles from electronic preprint archives such as ArXiv were excluded in order to ensure only papers that passed peer-review were included. Lastly, papers with poor quality that hindered our ability to meaningfully extract data were also excluded.
Study selection
The Covidence software (www.covidence.org) was used for screening and study selection. After removal of duplicates, studies were screened based on title and abstract, and then full-texts were obtained and assessed for inclusion. Study selection was performed by two independent researchers (S.-C.H. and A.P.), and disagreements were resolved through discussion. In cases where consensus could not be achieved a third researcher was consulted (I.B.).
Data extraction
For benchmarking the existing approaches we extracted the following data from each of the selected articles: (a) fusion strategy, (b) year of publication, (c) authors, (d) clinical domain, (e) target outcome, (f) fusion details, (g) imaging modality, (h) non-imaging modality, (i) number of samples, and (j) model performance (Table 1). We classified the specific fusion strategy based on the definitions in the section “Terminology and strategies in fusion”. The number of samples reported is the full data-size including training, validation and testing data. For classification tasks we extracted AUROC whenever this metric was reported, otherwise we extracted accuracy. When the article contained several experiments, metrics from the experiment with the best performing fusion model were extracted. These items were extracted to enable researchers to find and compare current fusion studies in their medical field or input modalities of interest.
Data availability
The authors declare that all data supporting the findings of this study are available within the paper and its Supplementary information files.
References
Leslie, A., Jones, A. J. & Goddard, P. R. The influence of clinical information on the reporting of CT by radiologists. Br. J. Radiol. 73, 1052–1055 (2000).
Cohen, M. D. Accuracy of information on imaging requisitions: does it matter? J. Am. Coll. Radiol. 4, 617–621 (2007).
Boonn, W. W. & Langlotz, C. P. Radiologist use of and perceived need for patient data access. J. Digit. Imaging 22, 357–362 (2009).
Comfere, N. I. et al. Provider-to-provider communication in dermatology and implications of missing clinical information in skin biopsy requisition forms: a systematic review. Int. J. Dermatol. 53, 549–557 (2014).
Comfere, N. I. et al. Dermatopathologists’ concerns and challenges with clinical information in the skin biopsy requisition form: a mixed-methods study: Clinical information in dermatopathology. J. Cutan. Pathol. 42, 333–345 (2015).
Jonas, J. B. et al. Glaucoma. The Lancet 390, 2183–2193 (2017).
McDonald, R. J. et al. The effects of changes in utilization and technological advancements of cross-sectional imaging on radiologist workload. Acad. Radiol. 22, 1191–1198 (2015).
Dean, N. C. et al. Impact of an electronic clinical decision support tool for emergency department patients with pneumonia. Ann. Emerg. Med. 66, 511–520 (2015).
Banerjee, I. et al. Development and Performance of the Pulmonary Embolism Result Forecast Model (PERFORM) for Computed Tomography Clinical Decision Support. JAMA Netw. Open 2, e198719 (2019).
Sandeep Kumar, E. & Jayadev, P. S. Deep Learning for Clinical Decision Support Systems: A Review from the Panorama of Smart Healthcare. In Deep Learning Techniques for Biomedical and Health Informatics. Studies in Big Data (eds. Dash, S. et al.) vol. 68, 79–99 (Springer, Cham, 2020).
Hinton, G. Deep learning—a technology with the potential to transform health care. JAMA 320, 1101 (2018).
Stead, W. W. Clinical implications and challenges of artificial intelligence and deep learning. JAMA 320, 1107 (2018).
Dunnmon, J. A. et al. Assessment of convolutional neural networks for automated classification of chest radiographs. Radiology 290, 537–544 (2019).
Irvin, J. et al. CheXpert: a large chest radiograph dataset with uncertainty labels and expert comparison. Proc. AAAI Conf. Artif. Intell. 33, 590–597 (2019).
Jaeger, S. et al. Two public chest X-ray datasets for computer-aided screening of pulmonary diseases. Quant. Imaging Med. Surg. 4, 475–477 (2014).
Johnson, A. E. W. et al. MIMIC-CXR, a de-identified publicly available database of chest radiographs with free-text reports. Sci. Data 6, 317 (2019).
Kallianos, K. et al. How far have we come? Artificial intelligence for chest radiograph interpretation. Clin. Radiol. 74, 338–345 (2019).
Gulshan, V. et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA 316, 2402 (2016).
Rajpurkar, P. et al. Deep learning for chest radiograph diagnosis: A retrospective comparison of the CheXNeXt algorithm to practicing radiologists. PLoS Med. 15, e1002686 (2018).
Majkowska, A. et al. Chest radiograph interpretation with deep learning models: assessment with radiologist-adjudicated reference standards and population-adjusted evaluation. Radiology 294, 421–431 (2020).
Person, M., Jensen, M., Smith, A. O. & Gutierrez, H. Multimodal fusion object detection system for autonomous vehicles. J. Dyn. Syst. Meas. Control 141, 071017 (2019).
Trzcinski, T. Multimodal social media video classification with deep neural networks. In Photonics Applications in Astronomy, Communications, Industry, and High-Energy Physics Experiments 2018 (eds. Romaniuk, R. S. & Linczuk, M.) (SPIE, 2018).
Ramachandram, D. & Taylor, G. W. Deep Multimodal Learning: A Survey on Recent Advances and Trends. IEEE Signal Process. Mag. 34, 96–108 (2017).
Kiela, D., Grave, E., Joulin, A. & Mikolov, T. Efficient large-scale multi-modal classification. In The Thirty-Second AAAI Conference on Artificial Intelligence (AAAI-18), (2018).
Thung, K.-H., Yap, P.-T. & Shen, D. Multi-stage Diagnosis of Alzheimer’s Disease with Incomplete Multimodal Data via Multi-task Deep Learning. In Deep Learning in Medical Image Analysis and Multimodal Learning for Clinical Decision Support (eds. Cardoso, M. J. et al.) vol. 10553, 160–168 (Springer International Publishing, 2017).
Kharazmi, P., Kalia, S., Lui, H., Wang, Z. J. & Lee, T. K. A feature fusion system for basal cell carcinoma detection through data-driven feature learning and patient profile. Skin Res. Technol. 24, 256–264 (2018).
Yap, J., Yolland, W. & Tschandl, P. Multimodal skin lesion classification using deep learning. Exp. Dermatol. 27, 1261–1267 (2018).
Li, H. & Fan, Y. Early Prediction Of Alzheimer’s Disease Dementia Based On Baseline Hippocampal MRI and 1-Year Follow-Up Cognitive Measures Using Deep Recurrent Neural Networks. In 2019 IEEE 16th International Symposium on Biomedical Imaging (ISBI 2019) 368–371 (IEEE, 2019).
Purwar, S., Tripathi, R. K., Ranjan, R. & Saxena, R. Detection of microcytic hypochromia using cbc and blood film features extracted from convolution neural network by different classifiers. Multimed. Tools Appl. 79, 4573–4595 (2020).
Liu, Mingqian, Lan, Jun, Chen, Xu, Yu, Guangjun & Yang, Xiujun Bone age assessment model based on multi-dimensional feature fusion using deep learning. Acad. J. Second Mil. Med. Univ. 39, 909–916 (2018).
Nie, D. et al. Multi-channel 3D deep feature learning for survival time prediction of brain tumor patients using multi-modal neuroimages. Sci. Rep. 9, 1103 (2019).
Hyun, S. H., Ahn, M. S., Koh, Y. W. & Lee, S. J. A machine-learning approach using PET-based radiomics to predict the histological subtypes of lung cancer. Clin. Nucl. Med. 44, 956–960 (2019).
Bhagwat, N., Viviano, J. D., Voineskos, A. N., Chakravarty, M. M. & Alzheimer’s Disease Neuroimaging Initiative. Modeling and prediction of clinical symptom trajectories in Alzheimer’s disease using longitudinal data. PLOS Comput. Biol. 14, e1006376 (2018).
Liu, J. et al. Prediction of rupture risk in anterior communicating artery aneurysms with a feed-forward artificial neural network. Eur. Radiol. 28, 3268–3275 (2018).
An, G. et al. Comparison of Machine-Learning Classification Models for Glaucoma Management. J. Healthc. Eng. 2018, 1–8 (2018).
Spasov, S. E., Passamonti, L., Duggento, A., Lio, P. & Toschi, N. A. Multi-modal Convolutional Neural Network Framework for the Prediction of Alzheimer’s Disease. In 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) 1271–1274 (IEEE, 2018).
Yala, A., Lehman, C., Schuster, T., Portnoi, T. & Barzilay, R. A deep learning mammography-based model for improved breast cancer risk prediction. Radiology 292, 60–66 (2019).
Yoo, Y. et al. Deep learning of brain lesion patterns and user-defined clinical and MRI features for predicting conversion to multiple sclerosis from clinically isolated syndrome. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 7, 250–259 (2019).
Kawahara, J., Daneshvar, S., Argenziano, G. & Hamarneh, G. Seven-point checklist and skin lesion classification using multitask multimodal neural nets. IEEE J. Biomed. Health Inform. 23, 538–546 (2019).
Reda, I. et al. Deep learning role in early diagnosis of prostate cancer. Technol. Cancer Res. Treat. 17, 153303461877553 (2018).
Qiu, S. et al. Fusion of deep learning models of MRI scans, Mini–Mental State Examination, and logical memory test enhances diagnosis of mild cognitive impairment. Alzheimers Dement. Diagn. Assess. Dis. Monit. 10, 737–749 (2018).
Beach, T. G., Monsell, S. E., Phillips, L. E. & Kukull, W. Accuracy of the Clinical Diagnosis of Alzheimer Disease at National Institute on Aging Alzheimer Disease Centers, 2005–2010. J. Neuropathol. Exp. Neurol. 71, 266–273 (2012).
Esteva, A. et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature 542, 115–118 (2017).
Hecker, S., Dai, D. & Van Gool, L. End-to-End Learning of Driving Models with Surround-View Cameras and Route Planners. In Computer Vision – ECCV 2018 (eds. Ferrari, V. et al.) vol. 11211, 449–468 (Springer International Publishing, 2018).
Jain, A., Singh, A., Koppula, H. S., Soh, S. & Saxena, A. Recurrent Neural Networks for driver activity anticipation via sensory-fusion architecture. In 2016 IEEE International Conference on Robotics and Automation (ICRA) 3118–3125 (IEEE, 2016).
Goodfellow, I., Bengio, Y. & Courville, C. Deep Learning (MIT Press, 2017).
Zou, H. & Hastie, T. Regularization and variable selection via the elastic net. J. R. Stat. Soc. Ser. B Stat. Methodol. 67, 301–320 (2005).
Subramanian, V., Do, M. N. & Syeda-Mahmood, T. Multimodal Fusion of Imaging and Genomics for Lung Cancer Recurrence Prediction. In 2020 IEEE 17th International Symposium on Biomedical Imaging (ISBI) 804–808 (IEEE, 2020).
Ngiam, J. et al. Multimodal Deep Learning. In Proceedings of the 28th International Conference on Machine Learning (ICML) 689–696 (2011).
Karpathy, A. et al. Large-Scale Video Classification with Convolutional Neural Networks. In 2014 IEEE Conference on Computer Vision and Pattern Recognition 1725–1732 (IEEE, 2014).
Neverova, N., Wolf, C., Taylor, G. & Nebout, F. ModDrop: adaptive multi-modal gesture recognition. IEEE Trans. Pattern Anal. Mach. Intell. 38, 1692–1706 (2016).
Bach, F. Breaking the curse of dimensionality with convex neural networks. J. Mach. Learn. Res. 18, 1–53 (2017).
Mwangi, B., Tian, T. S. & Soares, J. C. A review of feature reduction techniques in neuroimaging. Neuroinformatics 12, 229–244 (2014).
David, M., Alessandro, L., Jennifer, T. & Douglas, G. A. The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 6, e1000097 (2009).
Acknowledgements
The authors wish to thank John Alexander Borghi from Stanford Lane Medical Library for his help with creating the systematic search. The research reported in this publication was supported by the National Library of Medicine of the National Institutes of Health under Award Number R01LM012966. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
S.-C.H. and A.P. are co-first authors who contributed equally to this study. Concept and design: S.-C.H., A.P., M.P.L., and I.B. Study selection: S.-C.H. and A.P. Data extraction: S.-C.H., A.P., and S.S. Drafting of the manuscript: S.-C.H., A.P., I.B., and M.P.L. Critical revision of the manuscript for important intellectual content: S.-C.H., A.P., I.B., and M.P.L. Supervision: I.B. and M.P.L.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, SC., Pareek, A., Seyyedi, S. et al. Fusion of medical imaging and electronic health records using deep learning: a systematic review and implementation guidelines. npj Digit. Med. 3, 136 (2020). https://doi.org/10.1038/s41746-020-00341-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-020-00341-z
This article is cited by
-
Deep learning based joint fusion approach to exploit anatomical and functional brain information in autism spectrum disorders
Brain Informatics (2024)
-
AtPCa-Net: anatomical-aware prostate cancer detection network on multi-parametric MRI
Scientific Reports (2024)
-
Healthcare on the brink: navigating the challenges of an aging society in the United States
npj Aging (2024)
-
Empowering precision medicine: AI-driven schizophrenia diagnosis via EEG signals: A comprehensive review from 2002–2023
Applied Intelligence (2024)
-
Development of Medical Imaging Data Standardization for Imaging-Based Observational Research: OMOP Common Data Model Extension
Journal of Imaging Informatics in Medicine (2024)