Abstract
Cancer is a leading cause of death, accounting for almost 10 million deaths annually worldwide. Personalised therapies harnessing genetic and clinical information may improve survival outcomes and reduce the side effects of treatments. The aim of this study is to appraise published evidence on clinicopathological factors and genetic mutations (single nucleotide polymorphisms [SNPs]) associated with prognosis across 11 cancer types: lung, colorectal, breast, prostate, melanoma, renal, glioma, bladder, leukaemia, endometrial, ovarian. A systematic literature search of PubMed/MEDLINE and Europe PMC was conducted from database inception to July 1, 2021. 2497 publications from PubMed/MEDLINE and 288 preprints from Europe PMC were included. Subsequent reference and citation search was conducted and a further 39 articles added. 2824 articles were reviewed by title/abstract and 247 articles were selected for systematic review. Majority of the articles were retrospective cohort studies focusing on one cancer type, 8 articles were on pan-cancer level and 6 articles were reviews. Studies analysing clinicopathological factors included 908,567 patients and identified 238 factors, including age, gender, stage, grade, size, site, subtype, invasion, lymph nodes. Genetic studies included 210,802 patients and identified 440 gene mutations associated with cancer survival, including genes TP53, BRCA1, BRCA2, BRAF, KRAS, BIRC5. We generated a comprehensive knowledge base of biomarkers that can be used to tailor treatment according to patients’ unique genetic and clinical characteristics. Our pan-cancer investigation uncovers the biomarker landscape and their combined influence that may help guide health practitioners and researchers across the continuum of cancer care from drug development to long-term survivorship.
Similar content being viewed by others
Introduction
Cancer is a leading cause of death, accounting for about 19 million new cases and almost 10 million deaths annually worldwide1. Increasing burden of cancer incidence and mortality has become one of the key public health targets globally, leading to a surge of research focusing on understanding, prevention and treatment of cancer disease.
Traditionally, initial patient treatment and prognosis are defined by cancer type and stage at diagnosis, using widely accepted cancer staging systems such as Tumour-Node-Metastasis (TNM) classification2. However, cancer staging alone does not accurately predict survival in patients with cancer; it has been shown that there are other clinicopathological factors and molecular markers that can improve prognostic estimation, such as certain genetic mutations and comorbidities3,4. More precise prognosis could help understand the reasons of disease progression, decide on most appropriate treatment plan, and improve survival of patients with cancer.
In an era of precision medicine, knowledge of patient characteristics and biomarkers that are associated with prognosis and survival is key for further scientific advances and meaningful improvements of cancer patient outcomes5. Nowadays, the majority of oncology clinical trials include biomarkers, compared to only 15% in 20006. Clinical trial strategies have become more complex over time, examining multiple biomarkers per trial and exploring pan-cancer biomarkers. Yet, there is a lack of evidence base of the benefits of the use of biomarkers on patient survival7. Further understanding of the impact of genetic and clinicopathological factors on patient’s survival is needed to advance the field of precision cancer medicine. With sufficient evidence of the impact an individual patient’s characteristics have on cancer prognosis and survival, treatments and interventions can be focused on those patients who will benefit, sparing the side effects, treatment time and expense for those who will not.
The objective of this review is to summarise published evidence on biomarkers (clinicopathological factors and genetic mutations [SNPs]) that are associated with cancer survival in 11 major cancer types: lung, colorectal, breast, prostate, melanoma, renal, glioma, bladder, leukaemia, endometrial, ovarian. These 11 cancer types include most common cancers worldwide8 and are consistent with the cancer data available to the research community in one of the most widely known genomic data resources provided by Genomics England9. We provide two comprehensive lists of validated clinicopathological factors and genes that are important in cancer prognosis and will be valuable resources for cancer researchers, health practitioners and patients.
Results
The literature search identified a total of 2785 articles. 39 additional articles were identified through other sources such as reference and citation review. After title and abstract screening and removal of articles with insufficient data, 247 articles were included in the systematic review. PRISMA flow diagram is provided in Fig. 1. Full details of title and abstract screening are provided in Supplementary Data 1. Full list of references of studies included in this systematic review is provided in Supplementary References. Most of the studies were retrospective cohort studies focusing on one cancer type, 8 articles included more than one cancer type (pan-cancer studies) and 6 articles were reviews (including 2 articles that included both a review and their original data analysis). Details on selection criteria are provided in Supplementary Note 2. The number of papers excluded and reasons for exclusion are provided in Fig. 1.
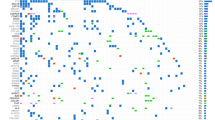
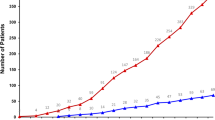
Studies were categorised into three groups based on their primary focus: (1) clinical (studies conducted on hospital or similar data and primarily focusing on clinicopathological factors)—115 studies; (2) genetic (studies conducted on genetic data with the primary focus on SNPs)—119; (3) clinical and genetic (studies considering both clinicopathological factors and SNPs)—13 studies. Studies were also categorised by cancer type (Table 1) and publication year (Supplementary Table 1). An upward trend of articles published in this topic was observed with about half of articles published in the last 5 years. More than half of all publications were related to three most common cancers: lung, colorectal and breast. The lowest number of articles was observed for bladder and glioma cancers.
The most frequently reported prognostic factors are summarised in Tables 2 and 3. Full lists of clinicopathological factors and genes recorded during the systematic review (including those recorded only in one study) are provided in Supplementary Data 2 and 3. Tables with extracted data by study are provided in Supplementary Data 4 and 5. 246 individual studies were included in the clinicopathological factor analysis representing 908,567 patients. 144 individual studies were included in the genetic mutation analysis representing 210,802 patients. The total number of individual studies is higher than the number of articles included in the systematic review due to three reasons. Firstly, studies that analysed both clinicopathological and genetic factors were included in both analyses. Secondly, pan-cancer studies which reported results by cancer type were split into multiple individual studies. Thirdly, review articles were split into multiple studies.
Prognostic clinicopathological factors
Table 2 presents the results of clinicopathological factors associated with survival that were reported significant in at least three multivariable studies (51 factors). Supplementary Data 2 provides a full list of prognostic clinicopathological factors, including more information on effect direction. The two prognostic factors that were found significant in the majority of the studies were patient’s age (135 studies) and pathological stage (133 studies). Both age and stage were unanimously found as risk factors in all cancer types; older patients and cancers with later stage were associated with reduced survival. Similarly, histological grade was frequently found as significant prognostic factor (83 studies) with higher grade leading to shorter survival. Grade was not relevant as a prognostic factor in melanoma and leukaemia.
Demographic factors
In addition to age, five other demographic prognostic factors were identified: gender (72 studies), race/ethnicity (18 studies), education level (9 studies), marital status (8 studies), and deprivation/socioeconomic status (5 studies). Male patients had shorter survival in breast, lung, renal, glioma, melanoma, leukaemia and bladder cancers, while colorectal cancer studies showed conflicting results. The prognostic direction of race/ethnicity depended on cancer type and population of the data sample. Higher education level, married status and higher socioeconomic status were associated with improved survival.
Tumour-related factors
Although pathological stage and histological grade were most frequently reported tumour-related factors, 12 other tumour-related factors were often reported, including size of tumour or metastatic nodules (52 studies), tumour site (48 studies), lymph node status (41 studies), invasion (37 studies), cancer subtype (36 studies), metastasis in general (22 studies) or metastasis to specific organs such as bone metastasis (4 studies) and liver metastasis (8 studies), number of metastatic sites (15 studies) and number of involved lymph nodes (13 studies). It was noted that some of these tumour-related factors are the constituents of tumour staging or grading (e.g., tumour size or lymph node status). All these factors were identified as risk factors for survival (presence or higher number/size of analysed factors led to shorter survival) with an exception of cancer subtype and tumour site, which had a prognostic direction dependent on cancer type. Two cancer type-specific factors were identified frequently as prognostic factors for cancer survival: thickness (Breslow depth) was important in melanoma (13 studies) and Gleason score was important in prostate cancer (4 studies).
Lifestyle and family history factors
Two lifestyle characteristics were frequently found as prognostic factors for cancer survival: smoking (16 studies), and weight/BMI (11 studies). Smoking was an important risk factor for shorter survival in lung, colorectal, prostate and bladder cancers. Higher weight/BMI was an important risk factor for shorter survival in breast, lung, ovarian, prostate and bladder cancers. However, the opposite effect of higher weight/BMI was recorded in renal and colorectal cancers. Family history was identified as an important risk factor for shorter survival in 8 studies on breast, colorectal and bladder cancers.
Treatment-related factors
Some studies included treatment strategies in their prognostic models and majority found that surgery (22 studies), chemotherapy (28 studies) and radiotherapy (12 studies) help improve survival for patients with cancer. Operative extent (3 studies), residual disease after surgery (7 studies), whether cancer recurred (4 studies) and whether there was any treatment performed (4 studies) were also important prognostic factors for survival. Two well-known patient performance status assessment systems were frequently found as significant prognostic factors for survival: ECOG10 (14 studies) and KPS11 (11 studies).
Factors related to other conditions
Presence or higher number of comorbidities in patients with cancer were found as important prognostic factors for reduced survival (10 studies). Some studies included comorbidities as a binary variable (whether a patient has any comorbidities or not), while others used composite comorbidity scores or grading systems (e.g., mild, moderate, severe comorbidities). In addition, individual comorbidities such as diabetes (8 studies) and chronic obstructive pulmonary disease (COPD; 5 studies) were found as significant prognostic factors for shorter survival in multiple cancer types. Bowel obstruction was an important factor leading to shorter survival in colorectal cancer (11 studies). Ulceration was an important factor for shorter survival in colorectal and melanoma cancers (11 studies). Anaemia was found significant in leukaemia and prostate cancer (3 studies). Low patient’s cognitive status was associated with shorter survival in prostate, colorectal and pan-cancer studies (4 studies).
Clinical biomarkers
Several clinical biomarkers were identified as important prognostic factors for cancer survival. In colorectal and lung cancers, higher CEA serum level was associated with shorter survival (22 studies). ER (estrogen receptor) (12 studies) and PR (progesterone receptor) (9 studies) status were important prognostic factors in breast and endometrial cancers (ER status was also important in colorectal cancer). ER and PR positive patients were found to survive longer in all studies. Higher white blood cell count was an important risk factor in leukaemia and endometrial cancer leading to shorter survival (10 studies). Elevated serum lactate dehydrogenase (LDH) level was associated with shorter survival in lung, leukaemia, prostate cancers and on pan-cancer level (9 studies). Decreased haemoglobin was associated with reduced survival in lung, renal, prostate and leukaemia cancers (7 studies). High alkaline phosphatase (ALP) level was associated with shorter survival in breast, colorectal, lung, prostate cancers and on pan-cancer level (6 studies). Albumin level, platelet count and lymphocyte count were also associated with survival, but the effect direction differed by cancer type. In colorectal cancer studies, higher CA19-9 (carbohydrate antigen 19-9) (4 studies) and CA125 (carbohydrate antigen-125) (1 study) levels were associated with shorter survival. CA125 was also found as a significant risk factor for survival in lung cancer and pan-cancer studies (2 studies). Although CA125 is used as a marker for treatment response in ovarian cancers in clinical practice, only one study in our review showed significant association between CA125 and ovarian cancer (pan-cancer study which included ovarian and endometrial cancers). All 15 studies which focused on ovarian cancer either did not test or did not find CA125 to be significantly associated with overall survival.
Prognostic gene mutations
Table 3 presents the results of genes associated with survival that were recorded as significant in at least three multivariable studies (14 genes). TP53 gene mutation was one of the most frequently reported prognostic risk factors for cancer survival (11 studies). TP53 gene encodes a tumour suppressor protein that plays an important role in cell cycle arrest, apoptosis, senescence, DNA repair and changes in metabolism and is widely known to be associated with cancer disease12. The review found that TP53 was an important prognostic risk factor in colorectal, lung, renal, endometrial, leukaemia cancers and on pan-cancer level. In breast cancer, the effect direction depended on cancer sub-type. Two studies found that TP53 mutations were associated with worse outcome in patients with ER positive status, but not in patients with ER negative status. PTEN gene is another tumour suppressor gene, for which mutations have been observed in many cancers13. Mutations in PTEN gene were associated with shorter survival in colorectal cancer, but longer survival in endometrial cancer (4 studies).
Two DNA repair genes, BRCA1 and BRCA2 were among the most frequently reported genes to be associated with survival (6 and 11 studies respectively). BRCA1 and BRCA2 genes encode proteins that help maintain genomic stability and act as tumour suppressors. BRCA mutations in the germline have become a hallmark for hereditary breast and ovarian cancers14. In this systematic review it was found that the effect direction of mutations in BRCA1 and BRCA2 genes varies by cancer type. Mutations in BRCA1 gene were associated with shorter survival in breast cancer, but longer survival in ovarian and endometrial cancers. Mutations in BRCA2 gene were associated with shorter survival in breast, colorectal and bladder cancers, but longer survival in ovarian, endometrial and lung cancers. ERCC2 was another gene related to DNA repair (nucleotide excision repair pathway), that was associated with cancer survival (5 studies). ERCC2 mutations were associated with shorter survival in colorectal and lung cancer, but were found to prolong survival in bladder cancer.
Mutations in oncogenes BRAF, KRAS and NRAS were frequently observed as prognostic factors for shorter survival (7, 6 and 4 studies respectively). RAS family oncogenes KRAS and NRAS have long been known to be associated with cancer15, and along with BRAF oncogene were frequently found in colorectal cancer16,17. In this review, all three oncogenes were associated with shorter survival in colorectal cancer. BRAF and NRAS gene mutations were also associated with shorter survival in melanomas. NRAS gene was found to be a protective prognostic factor in one study on leukaemia.
BIRC5, an immune-related gene, is a member of the inhibitor of apoptosis gene family, which encode negative regulatory proteins that prevent cell death and promote cell proliferation. It was shown to be highly expressed and lead to poor prognosis in most cancers previously18. In this review, BIRC5 gene mutations have been associated with shorter survival in glioma, lung, ovarian, melanoma and endometrial cancers (5 studies).
CDH1 gene is most commonly known to predispose diffuse gastric and lobular breast cancers19. It encodes cadherin protein and loss of function in this gene contributes to cancer progression by increased proliferation, invasion and metastasis. In this review, CDH1 gene was identified as significant prognostic factor for overall survival in colorectal cancer with some studies reporting risk while others protective effect (4 studies).
ASXL1 gene is known to be frequently mutated in all types of malignant myeloid diseases including chronic myelomonocytic leukaemia and acute myeloid leukaemia. ASXL1 mutations are most frequent in chronic myelomonocytic leukaemia (about 45%).20 This review found ASXL1 mutations to have a prognostic effect on survival in leukaemia. Three studies reported ASXL1 mutations to be associated with shorter overall survival in chronic myelomonocytic and acute myeloid leukaemias.
ECD, IL4R and WDR82 are protein coding genes, not commonly known to be associated with cancer risk or prognosis. However, multiple studies in this review identified mutations in these genes as prognostic factors for cancer survival. ECD mutations were found to be associated with shorter survival in renal, ovarian and pan-cancer studies (3 studies). IL4R mutations were found to be associated with shorter survival in colorectal and prostate cancers (3 studies). WDR82 mutations were found to be associated with shorter survival in renal, lung and melanoma cancers (3 studies).
Discussion
We extracted and summarised data on clinicopathological and genetic factors associated with survival from 247 articles across eleven cancer types. The findings indicate that prognostic factors for cancer survival have been investigated previously, however usually focusing on one cancer type and/or one data type. This summary of previously published literature shows that there is more diversity in research conducted on genetic prognostic factors related to cancer survival when compared to clinicopathological factors. Even though a large number of genetic mutations were identified to be associated with cancer survival (440 genes), only 40 of these were found significant in more than one multivariable study, and only 14 in three or more studies. In contrast, there were fewer clinicopathological prognostic factors identified overall (238 factors), but 79 of these were found significant in more than one multivariable study, and 51 were found significant in three or more studies. This is not surprising due to the differences between clinicopathological and genetic data that is collected from patients with cancer. The clinical, pathological and demographic information collected about the patient and the tumour are usually limited to tens or hundreds of data points, while the size of genetic data is substantially bigger, making genetic mutation analysis on whole-genome level difficult and time consuming. Therefore, most genetic studies focus on one biological pathway or group of genes associated with cancer leading to less overlap across genetic studies.
Our findings were in line with a previously published systematic review on clinicopathological prognostic factors in patients with incurable cancer21, which found comorbidities, gender, tumour site, tumour bulk, metastasis and performance status to be associated with survival. In addition, our review identified patient’s age and stage as the most frequently reported factors associated with survival. Considering the review cited above focused on patients with incurable cancer, they all would have had cancer with advanced stage; hence stage was not reported among prognostic factors. Age was among the most frequently tested prognostic factors in the aforementioned review, but results on the effect direction of age were inconsistent across studies some showing better survival for younger and some for older patients. In our review, older age was found to be consistently associated with reduced survival.
Despite the emergence of personalised cancer treatments in the recent years, there is still a gap between prognostic biomarker discoveries and their clinical use. Healthcare providers do not feel adequately informed about the evidence of the biomarker association to patient outcomes22. This review provides a unique view of clinicopathological and genetic prognostic factors across different cancer types and large patient base. The findings confirm that factors such as age, tumour stage, size and grade, tumour spread to other organs can be used to predict cancer survival. A lot of these factors are well known and widely used in clinical practice for prognosis and treatment of cancer. However, this overview draws attention to other, less commonly used, factors, which might help produce more precise prognosis and survival estimates in the future. Biomarkers such as CEA serum level, haemoglobin level, albumin level, white blood cell count, serum lactate dehydrogenase level, platelet count, alkaline phosphatase, lymphocyte count, CA19-9 level and CA125 level were found to be significantly associated with overall survival and could be collected and used as objective markers in future work on cancer prognosis. This overview demonstrates the prognostic ability of SNP mutations in well-known genes such as TP53, BRCA1, BRCA2, BRAF, KRAS and less commonly known genes such as ECD, IL4R and WDR82.
The information presented in this systematic review contributes to the understanding of cancer disease and could be used by researchers to further test and build the knowledge base about prognostic factors for cancer survival. This information could be used to develop complex prognostic models, which in turn could help predict cancer prognosis more accurately. Most importantly, this information could be used in the design of biomarker-driven oncology clinical trials23,24, which might lead into discoveries of new cancer treatments.
This systematic review summarises clinicopathological and genetic prognostic factors related to cancer survival at a large scale and on pan-cancer level. The results presented in this review are based on a high number of studies with large patient samples (average sample size in clinicopathological studies was 3,693 patients, and 1,464 patients in genetic studies). In addition to summarising widely known prognostic factors for cancer survival, our review draws attention to a number of less known factors, which haven’t been commonly used for cancer prognosis in research and clinical practice. Conducted on pan-cancer level, our review allows for comparison across different cancers and detects prognostic biomarkers that are important across multiple cancer types.
We acknowledge several limitations. This review was completed on a large scale and therefore provides summarised aggregate information about prognostic factors associated with cancer survival. For in depth understanding of factor effect sizes, a more specialised review should be completed, including a meta-analysis. Due to the large scale of this review, only the factors that were found significant in at least one study were included. However, information about insignificant factors could be useful for certain use cases and could be collected in a review of a smaller scale (e.g., in a review focusing on one cancer type). Due to the lack of detail and inconsistent reporting of insignificant results in included studies, only significant results were summarised in this review. Distinction between significance in multivariable and univariable analyses provides information on which factors remain significantly associated with cancer survival after inclusion of other important prognostic factors.
Single nucleotide polymorphisms were the focus of the genetics part of this review, however a similar summary could be conducted for other types of genetic variation such as copy number variation, which would help build even better understanding about the genes and their functions’ prognostic association with cancer survival. We combined the findings about genetic prognostic variables from both germline and somatic mutations, however it should be noted that these mutations could bear different meaning for cancer prognosis and treatment possibilities. Targeted cancer therapies due to the finding of known predictive biomarkers and genetic factors were not in scope of this review, but they have been increasingly used in practice in recent years and are known to significantly affect survival outcomes. Further studies could be performed with a focus on treatment-related prognostic effects on cancer survival.
We focused on individual prognostic factors associated with survival, because interaction effects were rarely reported in the literature. Exploring prognostic effects of different factor interactions (including cross-sectional interactions between clinicopathological and genetic factors) could be the focus of future research. The findings show that there is more research completed for more common cancer types such as lung, breast or colorectal cancers, however the evidence base for less common cancers like glioma or bladder cancer is slim. More research should be done on less common cancers in order to improve the knowledge, prognosis prediction and availability of personalised treatments for these cancers. The amount of healthcare data being collected is increasing exponentially, which has led to the rise of application of machine learning and similar computational methods in healthcare. However, this review shows that the majority of research conducted on prognostic factors related to cancer survival are based on traditional regression methods, such as Cox proportional hazards regression. Only 6 out of 247 articles used a machine learning approach (e.g., random forest or neural networks). The use of machine learning methods in the future might help assess larger amounts of data and develop insights on a larger scale.
This systematic review of 247 studies found 440 genes, including TP53, BRCA1, BRCA2, BRAF, KRAS, BIRC5, and 238 clinicopathological factors, including patient’s age and gender, tumour stage, histological grade, size, site, subtype, invasion and lymph node status, that are important prognostic factors for cancer survival. A summary of this scale helps improve understanding of prognostic factors across different cancer types and shows the gaps in research such as prognostic effects of interactions and less common cancer types. It also serves as a knowledge base for biomarker-driven oncology trials and further research work on cancer prognostic models, which both could lead to improvements in patient care and outcomes.
Methods
Information sources and search
This systematic review was conducted and reported according to The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines25. A literature search was conducted using PubMed/MEDLINE and Europe PMC from database inception up until 1st July 2021. The search strategy contained inclusion and exclusion criteria described in free text words as well as database-specific terms (MeSH terms in PubMed/MEDLINE and keywords in Europe PMC). No limit for publication dates was applied. Full details of search inclusion and exclusion criteria as well as reproducible search terms for both databases are provided in Supplementary Note 1. All published literature found in PubMed/MEDLINE database were included in the review with an addition of de-duplicated preprints from Europe PMC database to capture most recent studies in this topic. The references and citations of key studies were reviewed, and additional articles were added to the review.
Study selection
Search criteria and study selection criteria were reviewed together and agreed by both authors. Any disagreements between reviewers were resolved through discussion. Titles and abstracts were reviewed first, and full text was retrieved for those studies where decision could not be made based on the abstract. Eligibility and exclusion criteria used in the screening of titles and abstracts are provided in Supplementary Note 2. Remaining articles were reviewed in full text and excluded from the final review if an article was a review and did not provide sufficient data about prognostic factors (sample size, factor significance, effect direction and/or univariable/multivariable method) and/or an article did not report significant associations with survival on individual factor level.
Data extraction
Full text and supplementary materials of selected studies were reviewed to extract the data. Effects of prognostic factors and genetic mutations were synthesised by vote counting and summarising the direction of the effect26. The direction of the effect was determined by analysing reported effect sizes. It was noted whether a reported effect (e.g., hazard ratio) showed association to reduced survival (risk factor) or improved survival (protective factor). Direction of reported effects associated with patient survival was extracted if they reached significance of p-value <0.05. The effects from univariable and multivariable analyses were summarised separately. When either univariable or multivariable results were reported in a study, they were extracted and counted towards their respective category. When a factor was significant in both multivariable and univariable analyses in a single study, multivariable analysis took priority for the result extraction. When a factor was found significant in univariable analysis, but not in multivariable analysis (or it was not tested in multivariable analysis), only univariable result was extracted. In rare cases, where it was not clear whether reported results are from univariable or multivariable analysis, the results were not extracted. For each individual factor, the effect direction was recorded including notes on conflicting results. If there were conflicting results, the notes were taken focusing on differences across cancer types. A factor was included in the summary if at least one study recorded its effect direction.
The main end point for data collection was overall survival of patients with cancer. If overall survival was not reported, effects related to cancer specific, disease free, progression free, event free or time specific survival were collected. Review articles were included in the synthesis if they provided sample size and significance of prognostic effects reported in the reviewed studies. If there was an overlap between studies included in review articles and studies selected during our literature search, we included those studies as individual articles and excluded them from review article results to avoid double counting.
Two summary tables were prepared as a result of data synthesis: one for clinicopathological factors and one for genetic mutations. Some studies contributed to only one of the summary tables, while other studies were included in both. For example, some genetic studies included clinicopathological variables in the regression models for adjustment purposes. If such studies presented effects of these adjustment variables and their significance, this information was recorded in the summary of clinicopathological factors. Same rule was applied in the reverse situation (where clinicopathological studies used genetic factors for adjustment purposes), however it was rare.
Pan-cancer studies were summarised in two different ways. If a study presented results for all included cancer types overall, results were considered as one study and they were categorised as pan-cancer rather than individual cancer types. On the other hand, if a study reported results separately for cancer types, these were reported as separate studies (sample size was split accordingly). Similarly, studies included in the review articles were reported as separate studies.
Genetic studies were summarised on gene level, however specific SNP IDs were also collected if they were mentioned in the article. Both germline and somatic mutations were included in this review. Some studies did not explicitly report whether they analysed germline or somatic DNA data, while other studies analysed both types. Therefore, results in this review are summarised for germline and somatic mutations together. Clinicopathological factor summary includes all factors that were reported in reviewed articles except factors related to treatments and therapies specific to cancer type (e.g., specific drug treatment). Results about general treatments such as chemotherapy, radiotherapy, surgery are included in the results. Very few studies recorded interaction effects associated with cancer survival. These interaction variables were often specific to the study and its data sample, and did not appear in any other studies, therefore they were not included in the results. On rare occasions, where multiple studies were published using the same data sample, the results were included as multiple studies only if prognostic factors being tested were different.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All the data collected and analysed in this study are provided in supplementary materials.
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Brierley J. D. et al. TNM Classification of Malignant Tumours. 8th ed. Hoboken, NJ: Wiley-Blackwell; 2017.
Alexander, M. et al. Lung cancer prognostic index: A risk score to predict overall survival after the diagnosis of non-small-cell lung cancer. Br. J. Cancer 117, 744–751 (2017).
Dienstmann, R. et al. Prediction of overall survival in stage II and III colon cancer beyond TNM system: A retrospective, pooled biomarker study. Ann. Oncol. 28, 1023–1031 (2017).
Vargas, A. J. & Harris, C. C. Biomarker development in the precision medicine era: Lung cancer as a case study. Nat. Rev. Cancer 16, 525–537 (2016).
Vadas A., Bilodeau T. J. & Oza C. Special report: The evolution of biomarker use in clinical trials for cancer treatments. J. Precis. Med. https://www.thejournalofprecisionmedicine.com/the-journal-of-precision-medicine/special-report-the-evolution-of-biomarker-use-in-clinical-trials-for-cancer-treatments/. Accessed on 2022-04-11.
Davis, C. et al. Availability of evidence of benefits on overall survival and quality of life of cancer drugs approved by European Medicines Agency: retrospective cohort study of drug approvals 2009-13. BMJ 2017 359, j4530 (2017).
World Health Organisation cancer statistics. https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed on 2022-01-21.
HM Government. Genome UK: the future of healthcare. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/920378/Genome_UK_-_the_future_of_healthcare.pdf. Accessed on 2022-01-21.
C. G. Zubrod, et al. Appraisal of methods for the study of chemotherapy of cancer in man: comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. J. Chron. Dis. (1960), pp. 7-35.
Karnofsky, D. A. & Burchenal, J. H. (1949) The Clinical Evaluation of Chemotherapeutic Agents in Cancer. In: MacLeod, C. M., Ed., Evaluation of Chemotherapeutic Agents, Columbia University Press, New York, 196-196.
Olivier, M., Hollstein, M. & Hainaut, P. TP53 mutations in human cancers: origins, consequences, and clinical use. Cold Spring Harb. Perspect. Biol. 2, a001008 (2010).
Milella, M. et al. PTEN: multiple functions in human malignant tumors. Front Oncol. 5, 24 (2015).
Venkitaraman, A. R. Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell 108, 171–182 (2002).
Bos, J. L. ras oncogenes in human cancer: Areview [published correction appears in Cancer Res 1990 Feb 15;50(4):1352]. Cancer Res. 49, 4682–4689 (1989).
Yokota, T. et al. BRAF mutation is a powerful prognostic factor in advanced and recurrent colorectal cancer. Br. J. Cancer 104, 856–862 (2011).
Vaughn, C. P., Zobell, S. D., Furtado, L. V., Baker, C. L. & Samowitz, W. S. Frequency of KRAS, BRAF, and NRAS mutations in colorectal cancer. Genes Chromosomes Cancer 50, 307–312 (2011).
Xu, L., Yu, W., Xiao, H. & Lin, K. BIRC5 is a prognostic biomarker associated with tumor immune cell infiltration. Sci. Rep. 11, 390 (2021).
Benusiglio, P. R. et al. CDH1 germline mutations and the hereditary diffuse gastric and lobular breast cancer syndrome: A multicentre study. J. Med Genet 50, 486–489 (2013).
Gelsi-Boyer, V. et al. Mutations in ASXL1 are associated with poor prognosis across the spectrum of malignant myeloid diseases. J. Hematol. Oncol. 5, 12 (2012).
Hauser, C. A., Stockler, M. R. & Tattersall, M. H. Prognostic factors in patients with recently diagnosed incurable cancer: a systematic review. Support Care Cancer 14, 999–1011 (2006).
Selleck, M. J., Senthil, M. & Wall, N. R. Making meaningful clinical use of biomarkers. Biomark. Insights 12, 1177271917715236 (2017).
Hu C. & Dignam J. J. Biomarker-driven oncology clinical trials: Key design elements, types, features, and practical considerations. JCO Precis. Oncol. 2019;3:PO.19.00086. https://doi.org/10.1200/PO.19.00086.
Antoniou, M. et al. Biomarker-guided trials: Challenges in practice. Contemp. Clin. Trials Commun. 16, 100493 (2019).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021 18, e1003583, https://doi.org/10.1371/journal.pmed.1003583 (2021).
McKenzie J. E. & Brennan S. E. Synthesizing and presenting findings using other methods. In: Higgins J. P. T., Thomas J., Chandler J., et al, eds. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane. https://doi.org/10.1002/9781119536604.ch12 (2019).
Acknowledgements
A.G.L. is supported by funding from the Wellcome Trust (204841/Z/16/Z), National Institute for Health Research (NIHR) University College London Hospitals Biomedical Research Centre (BRC714/HI/RW/101440), NIHR Great Ormond Street Hospital Biomedical Research Centre (19RX02) and the Academy of Medical Sciences (SBF006\1084). The funders have no role in the writing of the manuscript or the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
J.G. and A.G.L. conceived and designed the study. J.G. undertook literature search, literature review and data extraction. A.G.L. supervised the research and methodological decisions. J.G. and A.G.L. analysed the data and interpreted the results. J.G. wrote the initial manuscript draft. A.G.L. revised the manuscript draft. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gammall, J., Lai, A.G. Pan-cancer prognostic genetic mutations and clinicopathological factors associated with survival outcomes: a systematic review. npj Precis. Onc. 6, 27 (2022). https://doi.org/10.1038/s41698-022-00269-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41698-022-00269-5
This article is cited by
-
CD74 as a prognostic and M1 macrophage infiltration marker in a comprehensive pan-cancer analysis
Scientific Reports (2024)
-
Identification of ZBTB9 as a potential therapeutic target against dysregulation of tumor cells proliferation and a novel biomarker in Liver Hepatocellular Carcinoma
Journal of Translational Medicine (2022)