Abstract
Increased sedentary behaviour (SB) is reportedly associated with mortality and morbidity in cardiovascular disease. However, its relation with physical function is not well understood in phase I cardiac rehabilitation (CR). This study aimed to investigate the rate of SB and the relation between SB and physical function among patients participating in phase I CR. This prospective multicentre cohort study enrolled patients participating in CR from October 2020 to July 2022. Patients with probable dementia and difficulty walking alone were excluded. We used sitting SB time as the index of SB and the Short Performance Physical Battery (SPPB) as the index of physical function at discharge. Patients were divided into the low SB group (< 480 min/day) or high SB group (≥ 480 min/day). We analysed and compared the two groups. The final analysis included 353 patients (mean age: 69.6 years, male: 75.6%), of whom 47.6% (168 of 353) were high SB patients. Total sitting SB time was higher in the high SB group versus the low SB group (733.6 ± 155.3 vs 246.4 ± 127.4 min/day, p < 0.001), and mean SPPB score was lower in the high SB group versus the low SB group (10.5 ± 2.4 vs 11.2 ± 1.6 points, p = 0.001). Multiple regression analysis identified SB as an explanatory variable for total SPPB score (p = 0.017). Patients with high SB had significantly lower SPPB scores than those with low SB. These findings underscore the importance of considering SB when improving physical function. Effective strategies to improve physical function can be developed that consider SB in phase I CR.
Similar content being viewed by others
Introduction
Patients with cardiovascular disease (CVD) such as heart failure (HF), ischaemic heart disease, and valvular disease typically report low levels of physical activity, which affect health-related quality of life (HRQOL) and increase the risk of disease progression and mortality1,2,3. The promotion of physical activity (exercise, sports, and increased activities of daily living) and exercise behaviour are effective in preventing or improving various diseases such as diabetes, obesity, some cancers, and high blood pressure4,5,6,7. Despite the regular promotion of physical activity, recent research in the USA and Europe has found increased health risks for death, obesity, diabetes, and CVD in people with sedentary behaviour (SB; i.e., any waking behaviour characterized by an energy expenditure of ≤ 1.5 metabolic equivalents while sitting, reclining, or lying down), and SB could be a potential target for improving cardiovascular health4,8. Moreover, it has been known for a long time that sitting SB time per day in the Japanese adult population is higher than that in foreign countries9. Thus, it is important not only to promote physical activity in the Japanese lifestyle but also to decrease sitting SB time to improve health.
Several previous reports have shown that in hospitalized patients, physical activity such as standing and/or walking decreased to 36% or less per day during their hospitalization, that they spent most of their time in bed or sitting, and that increased comorbidities were associated with a lower daily number of steps and lower upright time10,11,12,13. Patients with CVD were also reported to have greater amounts of objectively measured sedentary time compared to healthy controls14, and sedentarism was associated with personal and lifestyle characteristics and comorbidities14,15. Another report also suggested high levels of SB (9.7 ± 2.0 h/day) among patients with CVD at 28 days after discharge16.
The Short Physical Performance Battery (SPPB) is a series of tests used together to measure the functional performance of the lower extremities17,18,19. The test consists of three major components, each of which are scored independently: a set of 3 static balance tests, measurement of gait speed, and the five time sit-to-stand test17,18,19. The SPPB is now frequently being used as a screening tool for sarcopenia in elderly patients with CVD17,18,19. As the SPPB does not require special procedures or skills in evaluation, physical function and sarcopenia can be easily evaluated even in elderly people with complications18,19. For these reasons, the SPPB was used to assess physical function and perform SB screening in the present study.
Previous studies have also shown that 63.8% of elderly patients with HF had low physical function as assessed by the SPPB at discharge18 and that the motor Functional Independence Measure score of activities of daily living in these patients was an independent predictor of re-hospitalization within 90 days20. Another recent report found that the prevalence of hospital-associated disability was 7.43% among 238,160 patients with acute HF eligible for cardiac rehabilitation (CR), and only 44% patients received phase I CR (pre discharge) in the total cohort21. Comprehensive CR is composed of exercise and education programs that improve exercise capacity, HRQOL, and prognoses related to rates of mortality and readmission1,2,3, and such programs that included patient education reduced mortality by 73% compared to exercise-only programs1. In addition, SB is a potentially important target and may predict gains in cardiac knowledge received from a patient education program in phase II CR (post discharge)14,16. Thus, assessment of SB may also be necessary for phase II CR, especially for patients with high SB so that they can better understand and consider the contents of the education they receive during phase II CR.
However, there are few reports on the rate of SB and the relation between SB and the SPPB in patients with CVD participating in phase I CR (pre discharge). We hypothesized that patients with high SB would have poorer physical function as indicated by the SPPB score than patients with low SB. The present study aimed to investigate the rate of SB and the relation between SB and SPPB as an indicator of physical function and to consider further practical interventions for phase I CR.
Methods
Study design
This prospective multicentre cohort study included patients from four affiliated small-to-medium-scale hospitals with 200–580 beds, all of which conduct CR. Inclusion criteria comprised patients who were admitted to the affiliated hospitals from October 2020 to July 2022, participated in phase I CR, were hospitalized for more than five days, and had not been hospitalized for a medical procedure such as coronary angiography and percutaneous coronary intervention without CR. Excluded were patients with probable dementia (based on diagnosis or Mini-Mental State Examination score < 24), difficulty walking alone, disagreement with informed consent, hospital death, and data deficits.
Phase I CR
Comprehensive CR was based on the Japanese Circulation Society guidelines for rehabilitation in patients with CVD1. Phase I CR started within three days after admission and cardiac surgery1,22,23. The patients in phase I CR performed exercise based on frequency, intensity, type, and time as follows: frequency: exercise frequency was encouraged for 5 to 7 days during each week of CR; intensity: exercise intensity was encouraged within a Borg scale range of 11 to 13 or just below the patient’s anaerobic metabolism threshold; type: exercise types included stretching, aerobic exercise, and resistance training; and time: stretching exercises for the upper and lower body were performed for 10 to 20 min, and during aerobic exercise, patients performed warm-up, aerobics, and cool-down exercises for < 25 min, followed by 10 to 20 min of resistance training each day23.
Patients were lectured on diseases, lifestyle choices, nutrition, medicines they were taking, and exercise as offered by a doctor, nurse, registered dietitian, pharmacist, and physical or occupational therapists, respectively. Training on these exercises was adjusted according to each patient’s condition.
Patient characteristics
Patient characteristics such as age, sex, body mass index (BMI), employment, living together, smoking, marriage, main diagnosis, left ventricular ejection fraction, comorbidities, Charlson Comorbidity Index24, levels of serum haemoglobin and creatinine, and medications at the time of admission were collected from the medical records.
Sitting SB time
The Workforce Sitting Questionnaire25, whose reliability and validity are already confirmed in Japan26, was used as the basis for the questionnaire survey performed in this study to assess sitting SB time. This questionnaire contains six items related to sitting SB time over 1 week that reflect various life scenarios of driving, transportation, work, television viewing, personal computer/smartphone use, and other leisure time activity. Because the patients are hospitalized, driving and transportation times equal zero minutes. Patients were asked to answer each item for workdays and non-workdays over a 7-day (1-week) period. After a researcher gathered up all of the questionnaires, total sitting SB time as it related to the six life scenarios over the 7-day period were calculated. Following that, total sitting SB time in minutes/day was calculated by the researcher as total sitting SB time in minutes/7 days27,28. Thus, we considered sitting SB time for the entire day to indicate SB. Then, on the basis of a previous study, we divided the patients into two groups according to a cutoff value for SB of 480 min/day (low SB group: < 480 min/day, high SB group: ≥ 480 min/day)29.
SPPB for physical function
We used the SPPB as an index of physical function to evaluate standing balance, 4-m walking time, and standing/sitting times × 5. The SPPB is scored from 0 points (unable to complete a task) to 4 points (highest level of performance). The sum of the three test scores, which range from 0 to 12 points, was determined according to previously reported methods18,30. Patient characteristics were collected by one of the researchers from the medical record on the patient’s admission, and each patient’s SB and SPPB were assessed at discharge by one or two CR staff members.
Statistical analysis
All analyses were conducted on patients with no missing data for any of the variables. We first calculated the proportion of patients in the high SB group to all patients. We then compared the low SB and high SB groups using an unpaired t-test for continuous variables and Pearson’s Chi-squared test for categorical variables. A multiple linear regression analysis was conducted for the total SPPB score as the dependent variable. According to previous studies, we selected independent variables related to SB or SPPB such as age, sex, BMI, employment, smoking, marriage, main diagnosis, comorbidities, and variables that were statistically significant between the two groups31,32. Univariable and multivariable models were constructed. R studio (R version 4.0.2) was the analysis software33 used, and significance was regard as a p level < 0.05.
Ethical approval
This study was approved by the institutional review board for ethics at the Graduate School of Health Sciences, Kobe University (Approval no. 951-1), and each affiliated hospital received approval from its local ethics committee.
Informed consent
Informed consent was obtained from each patient.
Results
Patient selection
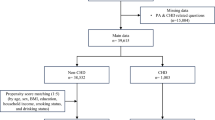
Figure 1 shows the flow chart of patients in the study. Among 7164 patients with cardiac disease admitted to the affiliated hospitals during the study period, 2354 patients met the inclusion criteria, including being hospitalized for more than five days and undergoing CR. After further excluding patients, 353 patients (mean age: 69.6, male; 75.6%) were finally included in the present study.
Rate of SB and comparison between the high and low SB groups
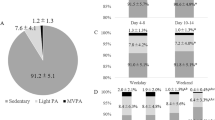
Clinical characteristics between the high SB group and low SB group can be compared in Table 1, which shows that the high SB group comprised 47.6% (168 of 353) the patients. There were significant differences in employment, smoking, main diagnosis, HF as a comorbidity, ARB as a medication, and SB between the two groups. Total sitting SB time in the high SB group was higher than that in the low SB group (733.6 ± 155.3 vs 246.4 ± 127.4 min/day, t = − 32.03, p < 0.001; Table 1, Fig. 2). Further, the mean SPPB score in the high SB group was lower than that in the low SB group (10.5 ± 2.4 vs 11.2 ± 1.6 points, t = 3.26, p = 0.001; Table 1, Fig. 2).
Multiple linear regression analysis for total SPPB score
Table 2 shows the results of multiple linear regression analysis for the total SPPB score. The factors significantly associated with total SPPB score included all variables except for valvular disease as a main diagnosis, diabetes and renal dysfunction as comorbidities, and ARB as a medication in the univariate model. Moreover, in the multivariable model, the factors significantly associated with total SPPB score included age, sex, HF as a main diagnosis, marriage, and SB. The adjusted R2 value was 0.3962, and the F-statistic was 16.4 for the 15 variables in this analysis model.
Discussion
The present study presented novel findings. First, the high SB group comprised 47.6% of the patients, indicating that about half of patients with CVD tended to spend long hours in SB. Second, characteristics of the patients such as smoking, HF as a main diagnosis and as a comorbidity, but not employment or medications, were observed among the patients with CVD who had higher levels of SB. Third, patients in the high SB group participating in phase I CR had significantly lower SPPB scores than patients in the low SB group. Finally, multiple regression analysis revealed that the SB remained an explanatory variable for total SPPB score. These findings suggest that high SB is present in about half of patients even in phase I CR, and hence, new strategies should be developed to stimulate patients with CVD to encourage more movement and less sitting.
To our knowledge, this is the first report on the effects of SB in the present study population, although some studies have investigated the causes or frequency of SB and/or physical activity in hospitalized patients4,10,11,12,13. The rate of SB was high at 47.6% and is relatively close to that of a previous study (sitting out of bed, 43%)12, even though the assessment methods were different between the two studies. Previous studies have pointed out that elderly patients tend to have more sitting SB time and spend more time in bed10,11. Therefore, particular attention should be paid to elderly patients with high SB.
In terms of our study hypothesis, patients with CVD showed high SB compared to those with low SB, which may support the occurrence of adverse outcomes4,14. Previous studies also suggested that the pattern of accumulation of sedentary time is important and linked it to acute detrimental effects on vascular function, blood pressure and lipids, which may contribute to the risk for cardiovascular events and mortality15,16,34,35. There were significant differences in the characteristics of our study patients for employment, smoking, main diagnosis, HF as a comorbidity, and ARB as a medication between the two groups. It is interesting to note that these factors largely align with predictors of high SB levels in the general population and of disease4,14,15,16,27,28,34,35. The present findings suggested that these factors may impact high SB levels in patients with CVD.
The total sitting SB time in the high SB group was 733.6 min/day, which converts to approximately 12.2 h/day. A previous study reported that an objectively measured sitting SB time ≥ 9.5 h/day was associated with increased risk of all-cause mortality36. As well, another study also suggested that patients with CVD and pre-CR sedentary time of 10.4 h/day are at risk for the detrimental health effects of SB, making these individuals highly vulnerable to recurrent cardiovascular events and premature death14. Moreover, CR reduced SB in these patients by 0.4 h/day14. As there are differences in the measurement methods, term, and subjects between previous studies and the present study, it is difficult to compare them directly. SB primarily occurred during leisure time, when the patients were not participating in phase I CR, suggesting that leisure time sedentary activities during hospitalization should be specifically targeted to achieve the largest reduction in total sedentary time.
The mean total SPPB score was lower in the high SB group than that in the low SB group in the present study. It is important that early mobilization to reduce SB, early screening for sarcopenia, and aerobic exercise and resistance training during hospitalization be carried out during phase I CR. In a previous study, multivariate analysis showed pre-hospital walking level to be a strong influencing factor of low physical function as assessed by SPPB at hospital discharge37. The exclusion criteria of the present study included patients with ‘difficulty walking alone’, so this factor did not effect the results of our study.
A score on the SPPB of < 7 points was associated with a larger risk of the combined endpoints of hospitalization and mortality for any cause (odds ratio = 3.6, 95% confidence interval; 1.0–12.9, p < 0.05) in patients with acute HF38,39. In addition, another previous study revealed that the SPPB has a ceiling effect40, which may have affected the results of the present analysis. In addition, our exclusion of patients who could not walk alone, indicating that they probably had severe physical function pre-hospitalization, might have excluded patients with low levels of independence. This fact likely affected the results of the present analysis.
A previous study in post-acute cardiac patients suggested that an improvement in the total SPPB score of > 1 was identified as the minimum clinically important difference (MCID)41. As we did not examine improvement in the pre-post SPPB total score, we could not investigate MCID in phase I CR. However, the very important clinical finding was that the high SB group had significantly lower physical function. Therefore, given that patients with high SB will likely become physically disabled in the future, it may be necessary for staff in charge of phase I CR to intervene in patients with SB during hospitalization to improve their activities of daily living.
The multiple linear regression analysis identified the factors significantly associated with total SPPB score to be age, smoking, marriage, HF, valvular disease as the main diagnosis, and SB. In addition, the adjusted R2 value was 0.3962 in this analysis model, indicating that the independent variable explains about 40% of the middle-level variation in the dependent variable.
HF is the final common pathway of several etiologies such as ischaemic and valvular heart disease42. Thus, the high SB group might include patients who were on a pathway of advanced cardiac disease and were likely to reduce physical function, even if they showed independence at this admission. As indicated by the multiple regression analysis, even after adjustment for other factors, high SB can predict impairment as indicated by the SPPB score. As mentioned above, although hospital-associated disability occurs infrequently among hospitalized patients with acute HF, only 44% of patients were accepted into phase I CR21. The main barrier may be the lack of referral of patients to rehabilitation, which means that rehabilitation and its importance have not yet penetrated deeply into the mindset of clinicians. However, we could not investigate that the reason for this in the present study.
A hospitalized patient with high SB may be experiencing a decline in physical function as indicated by the SPPB. Therefore, it is important to address these behavioural changes in phase I CR by focusing not only on increasing physical function but also in reducing high SB.
Study limitations
There are several limitations in the present study. First, this study included several cardiac diseases in the main diagnosis and comorbidities that require different treatments. Second, assessment of SB was by questionnaire and lacks objective measurements such as from an accelerometer. Third, domain-specific SB was not analysed in the present study and thus could not be investigated in detail. Because patients in phase I CR are, by definition, hospitalized, we could not investigate work or leisure time activities during hospitalization. Fourth, many patients were hospitalized for short-term procedures such as ablation or coronary angiography and were excluded from the final analysis, which may have led to the potential inclusion of selection bias in the present study. Fifth, the mechanism behind SB and other specific risk factors including, among others, cardiopulmonary function, hypertension, dyslipidemia, insulin resistance, obesity, reduced muscle strength and muscle activity, decreased vascular endothelial function, cognitive function, and neck and shoulder pain, were not investigated43,44. Nevertheless, the performance in both groups as indicated by the SPPB scores was close to optimal. Any one of these factors may have been a cause of the decline in physical function in the patients with high SB, as indicated by the lower SPPB score in this group. Finally, we could not investigate the relation between SB and prognosis such as rate of re-admission and mortality. Further studies are required to examine interventions to improve SB and SPPB. Despite these limitations, this multicentre clinical cohort study showed the effects of SB on physical function in phase I CR.
Conclusions
The relation between SB and SPPB as an index of physical function of patients with CVD in phase I CR was investigated. Patients in the high SB group had significantly lower SPPB scores than patients in the low SB group (Fig. 3). After adjustment for other associated factors in the multiple regression analysis, SB remained a factor associated with the total SPPB score. Our findings underscore the importance of addressing SB in patients with CVD even if they are undergoing phase I CR.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Makita, S. et al. JCS/JACR 2021 guideline on rehabilitation in patients with cardiovascular disease. Circ. J. 87(1), 155–235 (2022).
Izawa, K. P. et al. Usefulness of step counts to predict mortality in Japanese patients with heart failure. Am. J. Cardiol. 111(12), 1767–1771 (2013).
Izawa, K. P. et al. Long-term exercise maintenance, physical activity, and health-related quality of life after cardiac rehabilitation. Am. J. Phys. Med. Rehabil. 83(12), 884–892 (2004).
Biswas, A. et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Intern. Med. 162(2), 123–132 (2015).
Kurita, S. et al. Patterns of objectively assessed sedentary time and physical activity among Japanese workers: A cross-sectional observational study. BMJ Open 9(2), e021690 (2019).
Dogra, S. et al. Sedentary time in older men and women: An international consensus statement and research priorities. Br. J. Sports Med. 51(21), 1526–1532 (2017).
Kanejima, Y., Kitamura, M. & Izawa, K. P. Self-monitoring to increase physical activity in patients with cardiovascular disease: A systematic review and meta-analysis. Aging Clin. Exp. Res. 31(2), 163–173 (2019).
Bakker, E. A. et al. Dose-response association between moderate to vigorous physical activity and incident morbidity and mortality for individuals with a different cardiovascular health status: A cohort study among 142,493 adults from the Netherlands. PLoS Med. 18(12), e1003845 (2021).
Bauman, A. et al. The descriptive epidemiology of sitting: A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am. J. Prev. Med. 41(2), 228–235 (2011).
Callen, B. L., Mahoney, J. E., Grieves, C. B., Wells, T. J. & Enloe, M. Frequency of hallway ambulation by hospitalized older adults on medical units of an academic hospital. Geriatr. Nurs. 25(4), 212–217 (2004).
Pedersen, M. M. et al. Twenty-four-hour mobility during acute hospitalization in older medical patients. J. Gerontol. A. 68(3), 331–337 (2013).
Cattanach, N., Sheedy, R., Gill, S. & Hughes, A. Physical activity levels and patients’ expectations of physical activity during acute general medical admission. Intern. Med. J. 44(5), 501–504 (2014).
Meesters, J., Conijn, D., Vermeulen, H. M. & Vliet, V. T. Physical activity during hospitalization: Activities and preferences of adults versus older adults. Physiother. Theory Pract. 35(10), 975–985 (2019).
Bakker, E. A. et al. Sedentary behaviour in cardiovascular disease patients: Risk group identification and the impact of cardiac rehabilitation. Int. J. Cardiol. 326, 194–201 (2021).
Bellettiere, J. et al. Sedentary behavior and cardiovascular disease in older women: The objective physical activity and cardiovascular health (OPACH) study. Circulation 139(8), 1036–1046 (2019).
Duran, A. T., Ewing Garber, C., Cornelius, T., Schwartz, J. E. & Diaz, K. M. Patterns of sedentary behavior in the first month after acute coronary syndrome. J. Am. Heart Assoc. 8(15), e011585 (2019).
Chen, L. K. et al. Asian working group for sarcopenia: 2019 Consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 21(3), 300–307 (2020).
Kubo, I. et al. Relationship between physical function at discharge and hospital meal intake in elderly patients with heart failure. Heart Vessels 37(10), 1740–1748 (2022).
Saitoh, M. et al. Impact of chronic kidney disease and anemia on physical function in patients with chronic heart failure. Cardiorenal. Med. 4(2), 73–81 (2014).
Kitamura, M. et al. Relationship between activities of daily living and readmission within 90 days in hospitalized elderly patients with heart failure. Biomed. Res. Int. 2017, 7420738 (2017).
Ogawa, M. et al. Hospital-associated disability and hospitalization costs for acute heart failure stratified by body mass index- insight from the JROAD/JROAD-DPC database. Int. J. Cardiol. 367, 38–44 (2022).
Zwisler, A. D. et al. Cardiac rehabilitation section, European association of cardiovascular prevention and rehabilitation; committee on education and accreditation, european association of cardiovascular prevention and rehabilitation. Can level of education, accreditation and use of databases in cardiac rehabilitation be improved? Results from the European cardiac rehabilitation inventory survey. Eur. J. Prev. Cardiol. 19(2), 143–150 (2012).
Kanejima, Y. et al. Health literacy is associated with activities of daily living of patients participating in cardiac rehabilitation: A multicenter clinical study. Int. J. Environ. Res. Public Health 19(24), 16550 (2022).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 40(5), 373–383 (1987).
Chau, J. Y., van der Ploeg, H. P., Dunn, S., Kurko, J. & Bauman, A. E. A tool for measuring workers’ sitting time by domain: The workforce sitting questionnaire. Br. J. Sports Med. 45(15), 1216–1222 (2011).
Ishii, K. et al. Validity and reliability of Japanese-language self-reported measures for assessing adults domain-specific sedentary time. J. Epidemiol. 28(3), 149–155 (2018).
Izawa, K. P. & Oka, K. Sedentary behavior and health-related quality of life among Japanese living overseas. Gerontol. Geriatr. Med. 4, 2333721418808117 (2018).
Izawa, K. P. & Oka, K. Gender-related differences in sedentary behavior of Japanese living overseas in Malaysia. Rev. Recent Clin. Trials 15(3), 214–218 (2020).
Bennie, J. A. et al. The descriptive epidemiology of total physical activity, muscle-strengthening exercises and sedentary behaviour among Australian adults: Results from the National Nutrition and Physical Activity Survey. BMC Public Health 16, 73 (2016).
Puthoff, M. L. Outcome measures in cardiopulmonary physical therapy: Short physical performance battery. Cardiopulm Phys. Ther. J. 19(1), 17–22 (2008).
O’Donoghue, G. et al. A systematic review of correlates of sedentary behaviour in adults aged 18–65 years: A socio-ecological approach. BMC Public Health 16, 163 (2016).
Rhodes, R. E., Mark, R. S. & Temmel, C. P. Adult sedentary behavior: A systematic review. Am. J. Prev. Med. 42(3), e3–e28 (2012).
R Core Team. R: A Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, 2020). https://www.R-project.org/. Accessed 22 July 2022.
Diaz, K. M. et al. Patterns of sedentary behavior and mortality in US middle-aged and older adults: A national cohort study. Ann. Intern. Med. 167(7), 465–475 (2017).
Carter, S., Hartman, Y., Holder, S., Thijssen, D. H. & Hopkins, N. D. Sedentary behavior and cardiovascular disease risk: Mediating mechanisms. Exerc. Sport Sci. Rev. 45(2), 80–86 (2017).
Ekelund, U. et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ 366, l4570 (2019).
Kubo, I. et al. Worsening renal function during hospitalization in elderly patients with heart failure: An independent factor of activities of daily living decline. Heart Vessels 36, 76–84 (2020).
Llopis García, G. et al. Physical frailty and its impact on long-term outcomes in older patients with acute heart failure after discharge from an emergency department. Emergencias 31(6), 413–416 (2019).
Fuentes-Abolafio, I. J. et al. Physical functional performance and prognosis in patients with heart failure: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 20(1), 512 (2020).
Bergland, A. & Strand, B. H. Norwegian reference values for the short physical performance battery (SPPB): The Tromsø Study. BMC Geriatr. 19(1), 216 (2019).
Rinaldo, L. et al. Functional capacity assessment and minimal clinically important difference in post-acute cardiac patients: The role of short physical performance battery. Eur. J. Prev. Cardiol. 29(7), 1008–1014 (2022).
Johnson, M. J. Management of end stage cardiac failure. Postgrad. Med. J. 83(980), 395–401 (2007).
Hamilton, M. T., Hamilton, D. G. & Zderic, T. W. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes 56(11), 2655–2667 (2007).
Dunstan, D. W., Dogra, S., Carter, S. E. & Owen, N. Sit less and move more for cardiovascular health: Emerging insights and opportunities. Nat. Rev. Cardiol. 18(9), 637–648 (2021).
Acknowledgements
The present study benefitted from the support of Yuichi Matsuda, Ryohei Yoshikawa, Yuta Muranaka, Mitsuyo Okada, Toshimi Doi, Shinichi Shimada, Masashi Kanai, Masato Ogawa, Ryo Yoshihara, Natsumi Ikezawa, Ayami Osumi, and Ayano Makihara.
Funding
This work was supported by JSPS KAKENHI Grant Number JP22K11392.
Author information
Authors and Affiliations
Contributions
K.P.I.: Conceptualization, Methodology, Validation, Formal analysis, Writing—Original Draft; Y.K.: Conceptualization, Methodology, Validation, Formal analysis, Writing—Review & Editing, Visualization; M.K., K.I., A.O., I.K.: Conceptualization, Investigation, Writing—Review & Editing; K.N.: Resources, Writing—Review & Editing, Supervision; K.O., H.N., H.T., D.M., I.S.: Resources, Writing—Review & Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Izawa, K.P., Kanejima, Y., Kitamura, M. et al. Relation of sedentary behaviour to physical function in phase I cardiac rehabilitation. Sci Rep 13, 9387 (2023). https://doi.org/10.1038/s41598-023-36593-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36593-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.