Abstract
Mother-to-child transmission of SARS-CoV-2 has been reported since the onset of the COVID-19 pandemic. We conducted a study to summarize evidence on the risk of mother-to-child transmission in the first 30 days after birth in high-income countries and to evaluate the association between preventive measures and the risk of infection for the neonate. A systematic review and meta-analysis were undertaken following PRISMA guidelines. The National Library of Medicine, Web of Science, and Excerpta Medica databases were screened on February 26, 2022. All prospective observational studies addressing the frequency of infection in infants born to mothers SARS-CoV-2 positive were included. Twenty-six studies were included, reporting data of 2653 mothers with SARS-CoV-2 and 2677 neonates. The proportion meta-analysis pointed out an overall estimate of SARS-CoV-2 infection among infants of 2.3% (95% CI: 1.4–3.2%). Data from studies with (1.4%, 95% CI: 0.8–2) and without (1.3%, 95% CI: 0.0–2.7%) rooming-in provided similar risk of infection. Adopting at least two prevention measures during rooming-in resulted in a rate of mother-to-child infection of 1.0% (95%CI: 0.3–1.7%). The results of this study show a low rate of perinatal infection, support the rooming-in and confirm the effectiveness of preventive measures in reducing the risk of mother-to-child viral transmission.
Similar content being viewed by others
Introduction
Since its outbreak in March 2020, the COVID-19 pandemic has significantly impacted perinatal care. The main concern pointed out the possible transmission of the infection from a mother who tested positive for COVID-19 to her infant during the perinatal and early postnatal period1,2. This concern, justified by an initial lack of knowledge of the virulence and effects of this novel virus, led to the disruption of some practices recognized as crucial for maternal bonding and breastfeeding initiation, such as skin-to-skin and rooming-in3. This disruption in breastfeeding initiation, coupled with an initial concern about the viral transmission via breast milk or dyad proximity, has significantly impacted breastfeeding rates during the hospital stay and after discharge. As a result, increased reliance on breast milk substitutes occurred4,5. However, many authors have demonstrated the safety of breastfeeding even during maternal COVID-19 infection, and nowadays, these concerns and the choice of formulated milk seem unjustified 6. Furthermore, breastfeeding provides the optimum nutrition for the neonate and protects the infant against infection, even in the case of SARS-CoV-26,7. Indeed, it has now been demonstrated that breast milk does not contain complete viral particles with the ability to replicate but instead contains antibodies with a neutralizing capacity in the case of a mother infected with the virus8,9. However, the duration and extent of this effect are still debated10. Due to the heterogeneity of studies to reduce the possibility of mother-to-child transmission, many scientific societies and hospitals have recommended that SARS-CoV-2 positive mothers adopt practices of distancing themselves from their babies and use personal protective equipment, such as masks and gloves during rooming-in or breastfeeding11,12. However, the effectiveness of these preventive measures in reducing mother-to-child transmission is still under study11. Within this complex context, gaining further insight into the rate of mother-to-child transmission of infection after birth, including the implementation of preventive measures such as wearing a mask and physical distancing in potentially decreasing the risk of infection, is critical to refine and adapting perinatal practices to the COVID-19 era. We conducted a systematic review to evaluate the infection transmission rate in the perinatal or early postnatal period in neonates born to mothers who tested positive for COVID-19 in high-income countries.
Methods
To conduct this study, the 2020 edition of the Preferred Reporting Items for Systematic reviews and Meta-Analyses statement was followed12. The systematic review has been registered in the Research Registry (identifying number reviewregistry1640).
Literature search strategy
The literature search was performed in the National Library of Medicine via PubMed, directly interfaced with MEDLINE, the National Library of Medicine’s database of citations from biomedical journals. We also performed literature search via Web of Science (WOS) and Excerpta Medica (Embase) databases on February 26, 2022.The following string was adopted: (newborns or neonates or infants) AND (SARS-CoV-2 OR COVID-19) AND (transmission OR infection OR horizontal) AND (mothers OR breastmilk OR breastfeeding OR human milk OR dyads OR rooming-in OR hygiene OR formula). The secondary references of all included articles were screened looking for additional reports. Three pairs of reviewers conducted the literature search in blind. At the end of the literature search, controversies were solved consulting a senior researcher.
Eligibility criteria
Eligible were all prospective observational studies published in English addressing the frequency of infants born to mothers with a SARS-CoV-2 infection. The following inclusion criteria were considered: (1) SARS-CoV-2 infection in mothers had to be ascertained by a nasopharyngeal swab through a molecular test in the week preceding the delivery or on the day of delivery; (2) SARS-CoV-2 infection in infants had to be ascertained by a nasopharyngeal swab through a molecular test during the first 30 days after birth; (3) Studies had to be conducted in high-income countries as defined by World Bank classification. Studies including < 10 infected mothers were excluded. Date restriction was not applied.
Data extraction and quality assessment
From each eligible study, the following information was extracted: first author’ name, year of publication, year of the subject’s enrolment, country, number of mothers with SARS-CoV-2 infection, number of infants with and without SARS-CoV-2 infection, clinical presentation (especially need of oxygen supplementation and/or ventilatory support) of infected mothers and infants, gestational age at delivery. Information on possible preventive measures included avoidance of rooming-in, distancing the neonate from the mother, breastfeeding avoidance, breastmilk pasteurization, the use of facial mask for the mother, hands hygiene and the use of gloves by mothers, respectively. The Newcastle–Ottawa Scale for assessing the quality of non-randomized studies in meta-analyses was used to assess the quality of the studies. Data extraction and quality assessment were independently performed by pairs of investigators. Controversies were solved by consensus. If controversies stood, a senior researcher was involved.
Data synthesis and analysis
Data synthesis was performed through a proportion meta-analysis. The main outcome measure was the estimate of infected infants born to mothers with SARS-CoV-2 infection. Random-effects models were used. Pooled data were given with 95% confidence interval values (95% CI) and showed by forest plots. The I2-index was used to evaluate the heterogeneity and values > 50% were considered as significant. For the possible occurrence of a significant heterogeneity, subgroup meta-analyses focused on the use of rooming- in, on the adoption of at least two preventive measures and the year of subject’s enrollment were also planned. Publication bias was assessed through the use of Egger’s test. OpenMeta® software (Rockville, Maryland, USA) was used for the analyses.
A sensitivity analysis, excluding studies with extreme results, has also been performed to understand their influence on the main pooled analysis.
Statement of ethics
An ethics statement is not applicable because this study is based exclusively on published literature.
Results
Literature search results
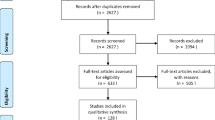
The literature search process is shown in Fig. 1.
Flow diagram of the literature search process; From Page et al.12. For more information, visit: http://www.prisma-statement.org/.
Among 1536 articles retained after duplication removal, we finally included 26 prospective studies13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38. Most studies (N = 21) were conducted during 2020, one in 2021 and four between 2020 and 2021 (Table 1).
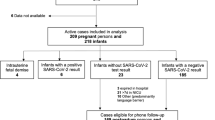
The studies were carried out in Italy (N = 8), in the USA (N = 6), in Spain (N = 3), in Poland (N = 2), in Israel (N = 2), in France (N = 1), in the United Arab Emirates (N = 1) and in Saudi Arabia (N = 1). One further study was an international multicenter study. The studies included 2653 mothers infected by SARS-CoV-2: only 4.7% (N = 126) of them needed oxygen or ventilatory support. A total of 2677 neonates were tested for SARS-CoV-2 and 100 resulted positive. Only five (5%) neonates needed oxygen supplementation and/or ventilatory support. All studies included infants born through vaginal and cesarean sections. In 14 studies the mother-infant dyad was enabled to stay together after birth 24 h a day13,14,18,19,21,23,24,25,26,27,29,31,32,36, in 6 it was not allowed17,20,28,30,33,33 and in the remaining 6 studies15,16,22,35,37,38, there was no information about it. In 12 studies two or more preventive measures were undertaken14,17,19,21,23,26,27,29,30,31,33,34, in 10 only one or no one13,15,16,18,20,22,24,25,28,36 and in the remaining 4 studies there was no information about preventive measures32,35,37,38. Considering only the studies in which rooming in practice was performed, at least two preventive measures were adopted in 8 of these studies14,19,21,23,26,27,29,31, one or no preventive measures were adopted in 5 studies13,18,24,25,36 and in one study it was not specified 32. The quality assessment evaluation is provided in the supplementary online table. We hereby provide a short summary of the NOS grading: Eight studies were considered as “high-quality” with a score ≥ 7, whereas twelve studies were considered “medium-quality”, having a score comprised between 4 and 615,18,20,24,25,34,35,36.
Proportion meta-analysis
The proportion meta-analysis pointed out an overall estimate of SARS-CoV-2 infection among infants born to infected mothers of 2.3% (95% CI: 1.4–3.2%), (Fig. 2). The I2-test was 62.4%, demonstrating a moderate heterogeneity. The sensitivity analysis performed excluding three studies with extreme results (pooled prevalence > 10%)19,22,34, showed a slight reduction of the overall pooled prevalence (1.4%, 95% CI: 0.9–1.8, I2-test 0%, Fig. 3) without a significant statistical difference compared to the main meta-analysis, taking into account the overlap of 95% confidence interval values among the two analyses.
The sub-analysis investigating the relationship between rooming-in practice and the proportion of infected neonates showed similar data pooling from studies with (1.4%, 95% CI: 0.8–2%, I2-test 10.5%, Fig. 4) and without (1.3%, 95% CI: 0.0–2.7%, I2-test 0%, Fig. 5) rooming-in. The proportion meta-analysis pooling data from studies applying at least two preventive measures showed an infection estimate of 1.0% (95% CI: 0.4–1.7%, I2-test 0%), whereas data from studies with either one or no preventive measure provided an estimate of 3.2% (95% CI: 1.2–5.2%, I2-test 82%). Moreover, analyzing only data from studies with rooming-in, if at least two preventive measures were adopted, the infection rate was 1.0% (95%CI: 0.3–1.7%, I2-test 0%), while in the group with rooming-in and only one or no preventive measures the infection rate was 1.9% (95 CI: 0.8–3.0%, I2-test 31%). Finally, the sub-analysis including studies performed exclusively in 2020 showed similar results to that including studies performed also during 2021 (2.2%, 95% CI: 1.2–3.2%, I2-test 65.8%, vs 3.1 95% CI: 0.7–5.4, I2-test 35.8%, respectively). The latter data are shown in the supplementary online figures.
Discussion
The objective of this systematic review and meta-analysis was to evaluate the proportion of infants born to mothers with COVID-19 who tested positive for SARS-CoV-2 during the first 30 days after birth. According to present findings, SARS-CoV-2 infection among neonates born to infected mothers was found to be 2.3%, indicating that mother-to-child transmission in the neonatal period appears to be relatively low and consistent with previously published data. The sensitivity analysis reported a mother-to-child transmission rate that, although slightly reduced, did not statistically differ from that found in the main meta-analysis, confirming the applicability of this study’s results. Moreover, the statistical heterogeneity was reduced (I2-test = 0%), confirming that, although the three studies with extreme results represented the source of the statistical heterogeneity in the main meta-analysis, they did not significantly influence the results of the pooled analysis.
The present meta-analysis collected data only from high-income countries with similar infant mortality and morbidity rates and a similar healthcare delivery system too. Despite the restriction in the inclusion criteria of the studies, the mother-to-child transmission rate of SARS-CoV-2 infection in the first month of life appears to overlap with that described in papers that included also low- and middle-income countries. Indeed, in the review by Gupta et al., the composite percentage of positive infants born to SARS-CoV-2 positive mothers appears to be between 1 and 4%39. Accordingly, Allotey et al. conducted a systematic review and meta-analysis including 472 studies (cohort studies, case series and case reports, respectively), independently of the prospective or retrospective data collection and countries’ income, and reported that the overall percentage of SARS-CoV-2 positivity in babies born to mothers with COVID- 19 was less than 2%40. Therefore our results indicate a similar infection rate when considering studies performed exclusively in 2020 vs studies performed exclusively in 2021, suggesting that the infection rate remains relatively low even in the presence of more transmissible variants of SARS-CoV-2, identified through 202141. Indeed, since the first pandemic wave, there have been numerous variants of SARS-CoV-2, each with its own characteristics of virulence and contagiousness. In a further step, it will be worth understanding how the emergence of highly contagious variants (such as Omicron variants that appeared in 2021) may also have affected the percentage of infants who tested positive after birth. Among the neonates who tested positive for SARS-CoV-2 in the present study, only 5% needed oxygen supplementation and/or ventilatory support. This result is in line with several other studies which have reported a favourable outcome after delivery in most SARS-CoV-2 positive neonates42,43,44. As described in the systematic review by Garcia et al.44, symptoms of COVID-19 in the neonatal period appear to be mild, with a low mortality rate, mainly associated with the occurrence of comorbidities. Raschetti et al. reported that 55.7% of COVID-19 positive newborns were symptomatic, which is much higher than the percentage found by Garcia et el. and Liguoro et al., ranging between 11 and 20% 42,43,44. Differences in available studies could be due to the difficulty of discriminating whether a more severe clinical course is the result of an induced delivery or caesarean section imposed by the severe clinical condition of the mother, associated to neonatal complications connected to preterm delivery, mode of delivery and critical maternal conditions at the time of delivery, rather than to a real direct effect of the virus on the infants' organism39,45. In fact, our data support that the balance between the potential risk of postnatal transmission of the virus by the mother is decisively outweighed by the well-known benefits of skin-to-skin contact, rooming-in practice and above all, breastfeeding6. In fact, since the first wave of the pandemic, several international institutions, including the WHO, have issued guidelines that did not recommend the precautionary separation of the infected mother from her child46,47. These international policies had significant relevance in protecting the bonding of the dyad and the beneficial effects of breastfeeding even at a time when the lack of knowledge had led some government institutions in some individual countries to promote mother-baby separation 48. Given the rapidly changing recommendations on perinatal practices, particularly at the beginning of the pandemic and the incomplete consistency of perinatal policies with recommendations or best practices11, we conducted a sub-analysis to investigate whether the rooming-in practice was associated with an increased positivity rate of SARS-CoV-2 percentage in neonates born to mothers with COVID-19 infection. The results of the present study indicate that neonates who roomed in and those who were separated from their mother showed a similar rate of SARS-CoV-2 positivity, confirming the safety of the rooming-in practice whose major role in promoting maternal and infant bonding and breastfeeding is widely acknowledged49. On the contrary, Kollikonda et al.50 conducted a systematic review including 8 studies published before November 2020 and reported that 19.4% of roomed-in infants tested positive as compared to 1.67% of the isolated ones. The authors hypothesized that the high positivity rate associated with the practice of rooming-in could be partially due to inconsistent use of protective devices such as masks in addition to the implementation of inadequate air isolation measures. Moreover, considering that the practice of skin-to-skin contact with SARS-CoV-2 positive mothers was not associated with an increased positivity rate, a further speculation is related to the prolonged proximity to a SARS-CoV-2 positive mother that occurs during rooming-in rather than during the Kangaroo mother care. Indications of the WHO foresee that the mother should follow some preventive measures to reduce the probability of a transmitted infection. These measures mainly concern using face masks, gloves, recommendations on the distance to keep with the neonate, even if in the same room, and hand hygiene and washing46. The effectiveness of these measures in preventing an infection has been clearly demonstrated and has been widely recommended by almost all supranational institutions and local governments51. Concerning some particular situations, such as hospitalization after birth, the indications on which measures to adopt are less defined, and hospital policies often have determined their implementation in the first part of the pandemic52. Further, a sub-analysis showed that the use of two or more preventive measures correlated with a trend towards a reduction in the percentage of infants who tested positive during hospitalization (1% with two or more measures vs 3.2% with either one or no measures). Similarly, during rooming-in, adopting at least two preventive measures resulted in a rate of mother-to-child infection of 1% vs 1.9% if one or no preventive measures were taken. This observation further underlines the efficacy of implementing protective measures in terms of social and hospital life to limit the spread of the infection51. New variants of SARS-CoV-2 are still causing concern due to their very high contagiousness. At the same time, several governments have declared the end of the health emergency, removing some very effective preventive measures in the community, including the use of face masks and social distancing. While in maternity wards more and more women arrive at delivery positive for the virus, little is known about the effects of these highly contagious variants on neonates39. Our review presents at least some limitations. Firstly, nine studies could not be retrieved and therefore assessed for eligibility. We included even studies in which neonates were defined as infected or not considering the result of a single nasopharyngeal swab, although we were aware that, following the WHO indications, a single positive nasopharyngeal swab, especially in the early postnatal period, is not synonymous with certain infections53, and the timing of the neonate’s infection was not considered. Moreover, the results cannot be extended to low- and middle-income countries. Finally, it was not possible to accurately assess the risk of infection associated to the newer SARS-CoV-2 variants. On the other hand, we believe that there are also important strengths, since we included only prospective studies thus limiting the heterogeneity of the included reports. Moreover, we analysed the possible role of rooming-in and preventive hygiene measures in high-resource countries. In conclusion, the results of this meta-analysis confirm the low rate of SARS-CoV-2 perinatal infection in high-income countries. Moreover, based on the present findings, there is no reason to prevent infant-mother proximity, rooming-in and breastfeeding even in the event of a re-emerging new pandemic wave. In any case, preventive measures of viral transmission are crucial in containing the infection of the neonates looking forward towards a further reduction of adverse health outcomes in this peculiar fragile group, in the absence of data on the adverse effects of the infection on neurodevelopment and later stages of life.
Data availability
All data generated or analyzed during this study are included in this article and its supplementary material files. Further enquiries can be directed to the corresponding author.
References
Wesołowska, A., Orczyk-Pawiłowicz, M., Bzikowska-Jura, A., Gawrońska, M. & Walczak, B. Protecting breastfeeding during the COVID-19 pandemic: A scoping review of perinatal care recommendations in the context of maternal and child well-being. IJERPH 19, 3347 (2022).
Twanow, J.-D.E., McCabe, C. & Ream, M. A. The COVID-19 pandemic and pregnancy: Impact on mothers and newborns. Semin. Pediatr. Neurol. 42, 100977 (2022).
Spatz, D. L. et al. Promoting and protecting human milk and breastfeeding in a COVID-19 world. Front. Pediatr. 8, 633700 (2021).
Ching, C. et al. Old tricks, new opportunities: How companies violate the international code of marketing of breast-milk substitutes and undermine maternal and child health during the COVID-19 pandemic. IJERPH 18, 2381 (2021).
Tomori, C., Gribble, K., Palmquist, A. E. L., Ververs, M. & Gross, M. S. When separation is not the answer: Breastfeeding mothers and infants affected by COVID-19. Maternal Child Nutr. 16, 4 (2020).
Van Goudoever, J. B. et al. Updating clinical practices to promote and protect human milk and breastfeeding in a COVID-19 Era. Front. Pediatr. 2022, 10 (2022).
Vizzari, G. et al. Human milk, more than simple nourishment. Children 8, 863 (2021).
Pullen, K. M. et al. Selective functional antibody transfer into the breastmilk after SARS-CoV-2 infection. Cell Rep. 37, 109959 (2021).
Milani, G. P., Porro, A., Agostoni, C. & Giannì, M. L. Breastfeeding during a pandemic. Ann. Nutr. Metab. 78, 17–25 (2022).
Bäuerl, C. et al. SARS-CoV-2 RNA and antibody detection in breast milk from a prospective multicentre study in Spain. Arch. Dis. Child Fetal Neonatal Ed. 107, 216–221 (2022).
Merewood, A. et al. Breastfeeding supportive practices in European hospitals during the COVID-19 pandemic. J. Maternal-Fetal Neonatal Med. https://doi.org/10.1080/14767058.2021.1986482 (2021).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ https://doi.org/10.1136/bmj.n71 (2021).
Szczygiol, P. et al. COVID-19 in pregnancy, management and outcomes among pregnant women and neonates—results from tertiary care center in Wroclaw. Ginekol. Pol. https://doi.org/10.5603/GP.a2021.0201 (2022).
Verma, S. et al. Outcomes of maternal-newborn dyads after maternal SARS-CoV-2. Pediatrics 146, e2020005637 (2020).
Zhang, P. et al. Maternal, neonatal and placental characteristics of SARS-CoV-2 positive mothers. J. Maternal-Fetal. Neonatal Med. https://doi.org/10.1080/14767058.2021.1892637 (2021).
Alouini, S. et al. Maternal-fetal implications of SARS CoV-2 infection during pregnancy, viral, serological analyses of placenta and cord blood. IJERPH 19, 2105 (2022).
AlQurashi, M. et al. Clinical Characteristics of newborn infants delivered to pregnant women with laboratory-confirmed COVID-19: A single-center experience from Saudi Arabia. Cureus https://doi.org/10.7759/cureus.18573 (2021).
Angelidou, A. et al. Association of maternal perinatal SARS-CoV-2 infection with neonatal outcomes during the COVID-19 pandemic in Massachusetts. JAMA Netw. Open 4, 4 (2021).
Biasucci, G. et al. Safe perinatal management of neonates born to SARS-CoV-2 positive mothers at the epicenter of the Italian epidemic. Front. Pediatr. 8, 256 (2020).
Blasco-Santana, L. et al. Maternal and perinatal outcomes and placental pathologic examination of 29 SARS-CoV-2 infected patients in the third trimester of gestation. J. Obstetr. Gynaecol. Res. 47, 2131–2139 (2021).
Buonsenso, D. et al. Short- and mid-term multidisciplinary outcomes of newborns exposed to SARS-CoV-2 in utero or during the perinatal period: Preliminary findings. Eur. J. Pediatr. https://doi.org/10.1007/s00431-021-04319-1 (2022).
Villar, J. et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection the intercovid multinational cohort study. JAMA Pediatr. 175, 817–826 (2021).
Ibrahim, C. et al. Management of infants born to mothers with SARS-CoV2 infection: A prospective observational study. BMJ Paediatr. Open 4, 824 (2020).
Januszewski, M. et al. COVID-19 in pregnancy-perinatal outcomes and vertical transmission preventative strategies, when considering more transmissible SARS-CoV-2 variants. J. Clin. Med. 10, 3724 (2021).
Jimenez, I. et al. Umbilical cord clamping and skin-to-skin contact in deliveries from women positive for SARS-CoV-2: A prospective observational study. BJOG-An Int. J. Obstetr. Gynaecol. 128, 908–915 (2021).
Kunjumon, B. et al. Breast milk and breastfeeding of infants born to SARS-CoV-2 positive mothers: A prospective observational cohort study. Am. J. Perinatol. 38, 1209–1216 (2021).
Ronchi, A. et al. Evaluation of rooming-in practice for neonates born to mothers with severe acute respiratory syndrome coronavirus 2 infection in Italy. JAMA Pediatr. 175, 260–266 (2021).
Rottenstreich, A. et al. Vaginal delivery in SARS-CoV-2-infected pregnant women in Israel: A multicenter prospective analysis. Arch. Gynecol. Obstet. 303, 1401–1405 (2021).
Salvatore, C. et al. Neonatal management and outcomes during the COVID-19 pandemic: An observation cohort study. Lancet Child Adolescent Health 4, 721–727 (2020).
Shlomai, N. et al. Neonatal SARS-CoV-2 infections in breastfeeding mothers. Pediatrics 147, 5 (2021).
Solis-Garcia, G. et al. Epidemiology, management and risk of SARS-CoV-2 transmission in a cohort of newborns born to mothers diagnosed with COVID-19 infection. Anal. Pediatr. 94, 173–178 (2021).
Capozza, M. et al. Perinatal transmission and outcome of neonates born to SARS-CoV-2-positive mothers: The experience of 2 highly endemic italian regions. Neonatology https://doi.org/10.1159/000518060 (2021).
Conti, M. et al. Consequences of early separation of maternal-newborn dyad in neonates born to SARS-CoV-2 positive mothers: An observational study. Int. J. Environ. Res. Public Health 18, 5899 (2021).
Conti, M. et al. Immune response of neonates born to mothers infected with SARS-CoV-2. JAMA Netw. Open 4, 11 (2021).
Edlow, A. et al. Assessment of maternal and neonatal SARS-CoV-2 viral load, transplacental antibody transfer, and placental pathology in pregnancies during the COVID-19 pandemic. JAMA Netw. Open 3, 12 (2020).
Falsaperla, R. et al. Neonates born to COVID-19 mother and risk in management within 4 weeks of life: A single-center experience, systematic review, and meta-analysis. Am. J. Perinatol. 38, 1010–1022 (2021).
Fenizia, C. et al. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat. Commun. 11, 5128 (2020).
Garcia-Ruiz, I. et al. Congenital infection of SARS-CoV-2 in live-born neonates: A population-based descriptive study. Clin. Microbiol. Infect. 27, 1521 (2021).
Gupta, P. et al. An observational study for appraisal of clinical outcome and risk of mother-to-child SARS-CoV-2 transmission in neonates provided the benefits of mothers’ own milk. Eur. J. Pediatr. 181, 513–527 (2022).
Allotey, J. et al. SARS-CoV-2 positivity in offspring and timing of mother-to-child transmission: Living systematic review and meta-analysis. BMJ 2022, e067696. https://doi.org/10.1136/bmj-2021-067696 (2022).
Duong, B. V. et al. Is the SARS CoV-2 omicron variant deadlier and more transmissible than delta variant?. Int. J. Environ. Res. Public Health 19, 4586 (2022).
Raschetti, R. et al. Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nature Commun. 11, 1 (2020).
Liguoro, I. et al. SARS-COV-2 infection in children and newborns: A systematic review. Eur. J. Pediatr. 179, 1029–1046 (2020).
García, H., Allende-López, A., Morales-Ruíz, P., Miranda-Novales, G. & Villasis-Keever, M. Á. COVID-19 in neonates with positive RT–PCR test. Systematic review. Arch. Med. Res. 53, 252–262 (2022).
Allotey, J. et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ-Br. Med. J. 370, 3320 (2020).
WHO—Interim guidance. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance, 13 March 2020. World Health Organization. https://apps.who.int/iris/handle/10665/331446. License: CC BY-NC-SA 3.0 IGO (2020)
Davanzo, R. et al. Breastfeeding and coronavirus disease-2019: Ad interim indications of the Italian Society of Neonatology endorsed by the Union of European Neonatal & Perinatal Societies. Matern. Child Nutr. 16, 3 (2020).
Spatz, D. L. et al. Promoting and protecting human milk and breastfeeding in a COVID-19 world. Front. Pediatr. 8, 256 (2020).
Leone, T. A. & Abreu, W. J. The term newborn. Clin. Perinatol. 48, 431–445 (2021).
Kollikonda, S. et al. Transmission of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) through infant feeding and early care practices: A systematic review. J. Neonatal. Perinatal. Med. https://doi.org/10.3233/NPM-210775 (2021).
da Silva, S. J. R. et al. Two years into the COVID-19 pandemic: Lessons learned. ACS Infect. Dis. 8, 1758–1814 (2022).
Turner, S., McGann, B. & Brockway, M. ’Merilee’. A review of the disruption of breastfeeding supports in response to the COVID-19 pandemic in five Western countries and applications for clinical practice. Int. Breastfeed J. 17, 38 (2022).
World Health Organization. Definition and categorization of the timing of mother-to-child transmission of SARS-CoV-2: Scientific brief, 8 February 2021. https://apps.who.int/iris/handle/10665/339422. License: CC BY-NC-SA 3.0 IGO (2021).
Author information
Authors and Affiliations
Contributions
M.L.G. and G.P.M. conceptualized and designed the study. D.M., G.V., and M.T. collected the data. G.T. performed the statistical analyses. A.C. assessed the quality of the studies. D.M., M.L.G., G.P.M., G.V. writing original draft preparation. L.P., C.A., P.M., F.M. writing review and editing. All authors gave a significant contribution to data interpretation in their field of expertise. All authors reviewed the manuscript and approved it as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Morniroli, D., Vizzari, G., Tosi, M. et al. Mother-to-child transmission of SARS-CoV-2 infection in high-income countries: a systematic review and meta-analysis of prospective observational studies. Sci Rep 13, 8813 (2023). https://doi.org/10.1038/s41598-023-36097-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36097-1
This article is cited by
-
Impact of COVID-19 pandemic on cord blood banking and transplantation
Cell and Tissue Banking (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.