Abstract
Mycotoxigenic fungi can infect and produce potent mycotoxins in foodstuffs prior to harvest, during harvest (field fungi), and in storage after harvest (storage fungi), which when ingested, can result in adverse health effects. This study was aimed at assessing the knowledge, attitudes, and practices adopted by the Ghanaian populace to help mitigate the occurrence of molds and mycotoxins in foods. A cross-sectional survey involving a structured questionnaire was conducted with 642 respondents from twelve regions of Ghana. Descriptive statistics and analyses of variance were calculated. Correct Classification Rate (CCR) was measured to assess the utility of a logistic regression model. The results of the study showed that the majority of 299 (46.6%) of the respondents were between the ages of 18–25. Age and educational level were related to knowledge about the occurrence of fungi and mycotoxins in foods (p < 0.05). More than half the respondents, 50% indicated that they knew of aflatoxins as a major mycotoxin present in food. Higher education directly influenced on the knowledge of mycotoxicosis and the management of stored food to present intoxication by fungal metabolites. 502 (32.9%) knew that consuming foods with toxins could cause stomach aches. The most commonly consumed food commodity despite the presence of visible growth of fungi was bread (35.3%). The average KAP score for knowledge showed that, out of 100%, there was adequate knowledge (63.8%) among the members of the Ghanaian populace. Favorable environmental conditions of high humidity (> 85% ERH) and temperature (> 28–32 °C) enhance the proliferation of fungi in most foods and the attendant production of mycotoxins such as aflatoxins, ochratoxins, and fumonisins are associated with several severe human and animal health conditions; mycotoxicosis was associated with high fever, pain, vomiting, suppression of immunity, cancer, etc. when these foods are consumed on regular basis for a prolonged length of time. Future examination of the food items used for the School Feeding Programme in Ghana will offer opportunities to examine the risks of feeding youth with fungal-contaminated food preparations from providers.
Similar content being viewed by others
Introduction
Fungal contamination of foodstuffs and agricultural produce is a prevailing global problem, particularly in developing countries. The prevailing hot and humid tropical environmental climate conditions support the growth of mycobiota both in the field and in storage1. Unfortunately, the growth of fungi causes not only spoilage but depreciates food quality and reduces food security. The ubiquitous nature of fungi and their airborne spores enable them to thrive over a wide range of habitats including deserts, hyper-saline environments such as the sea, on rocky surfaces, etc. with varying climatic conditions of low and high temperatures2.
The species of fungi causing mycotoxicosis are mainly in the genera of Aspergillus, Fusarium, and Penicillium, although others have also been implicated in causing mycotoxicosis in man when he ingests food contaminated by fungal toxins. Indeed, some mycotoxins cause diseases such as cancer (aflatoxins), and some damage vital organs such as the brain and nervous system, liver, and kidney to mention but a few3,4. Of great concern to public health is the effect of mycotoxins on the fragile immune systems of adults and children alike, although infants, by virtue of their smaller body weight and less acid stomach, are more susceptible to mycotoxins than adults5,6.
Indigenous farmers in Africa have devised the use of local plant parts to reduce fungal and insect infestation in stored staple foods7,8. However, fungal toxins continue to take a toll on the health of the populace. It is presumed that the lack of knowledge of the conditions which predispose food to fungal intoxication is not well understood by both the farmers and the populace although the phenomenon has been demonstrated by scientists in the pertinent literature9.
It is well known that aflatoxins are potent hepatotoxic, teratotoxic, mutagenic, and carcinogenic mycotoxins produced by members of the Aspergillus section Flavi namely A. flavus, A. parasiticus, A. nomius, A. pseudonomius, A. arachidicola, A. minisclerotigenes, A. ochraceoroseus, A. korhogoencis, A. pseudocaelatus, A. pseudotamarii, and A. bombycis10. Aflatoxins B1, B2, G1, and G2 can occur in foods such as groundnuts, tree nuts, maize, rice, figs, dried spices, crude vegetable oils, cocoa beans, cocoa powder, chocolate, cotton seeds, copra etc.11,12. Aflatoxins M1 and M2 are found in milk and milk products. Human hepatic cancer and acute fatal diseases eg. Hepatitis have occurred in association with the consumption of heavy contaminated foods in Asia, africa and else where13,14,
Ochratoxins are the main mycotoxin with nephrotoxic effects and have been associated with Balkan Endemic Nephropathy and tumour development in the urinary tract15,16,17. Ochratoxin A (OTA) is a toxic secondary metabolite produced by several species of Aspergillus and Penicillium genera. For example, OTA is produced by Aspergillus carbonarius, A. sclerotiorum, A. sulphureus, A. alliaceus, A. affinis, A. albertensis, A. welwitschive, A. cretensis, A. alutaceus (= A ochraceus) and A. niger and species belonging to the A. niger aggregation18,19 in tropical zones18,20,21,22. The European Food Safety Authority23 affirmed that OTA is nephrotoxic in all animal species tested and exerts immunotoxic, neurotoxic, and teratogenic effects at high dose levels. OTA has been detected in high contamination levels in maize, rye, coffee, cocoa powder, and chocolate, and other related foods in Africa24,25,26,27,28. Penicillium verrucosum and P. nordicum also grew well and produced OTA18.
Fumonisin is a group of fifteen (15) closely related mycotoxins produced by species of Fusarium i.e. F. proliferatum, F. globosum, F. nygum, F. subglutinans, F. verticillioides = (F. moniliforme) all included in the Gibberella fujikuroi species complex29. F. verticillioides is important in veterinary medicine as a cause of porcine pulmonary edema and equine leucoencephalomalacia and oesophageal cancer in humans. Several cogenes of fumonisins A1, A2, B2, B3 and B4 as well as P are known29. Studies have also shown that some strains of Aspergillus niger, A. welwitschiae as well as Alternaria alternata and Fusarium oxysporum also produce fumonisins. Fumonisins have been shown to occur in barley, wheat, sorghum, rice, millet and corn products29. The most common syndromes associated with fumonisins are leucoencephalomalacia in horses, pulmonary oedema and hydrothorax in pigs, and hepatotoxicity, carcinogenicity and oesophageal cancer in humans9,30.
Zearalenone, ZEA, previously known as F2-toxin in a resorcyclic acid lactone produced by Fusarium graminearum, F. colmorum, F. crookwellense, and F. equiseti31,32. Another mycotoxin of health importance is Vomitoxin which is also known as deoxynivalenol (DON) and is a type B trichothecene, an epoxy sesqueterpenoid. It occurs predominantly in grains, e.g. wheat, maize, barley, rye, oat, and less so in rice, sorghum and triticale33. It is a secondary metabolite of Fusarium culmorum and F. graminearum.
Patulin is isolated from several species belonging to the genera Aspergillus, Penicillium, Paecilomyces, and Byssochlamys. Among the Aspergillus species, the number of patulin producing species is limited to three of the Clavali group, namely, A. clavatus, A. giganteus, and A. longivestica34. Within the genus Penicillium, patulin-producing species are P. carneum, P. glavigeum, P. concentricum, P. coprobium, P. dipodomyicola, P. expansum, P. patulum, Psclerotigenum and P. valpinum35. In the case of Paecilomyces and Byssochlamys, B. nivea and B. saturanus produce patulin but B. fulva does not36,37. Currently, the list of mycotoxins levels in food is regulated in many countries including European Community and Africa are aflatoxins, ochratoxin A, zearalenone, fumonisins and trichothecene36.
Food safety is a vital gauge or criterion for enhanced food security. In sub–Saharan Africa where major food losses occur, health challenges and even human fatalities have arisen from eating contaminated key staple foods by fungal pathogens in the field (field fungi) and in storage (storage fungi)38,39,40.
The most effective way to prevent mycotoxin formation in stored staple food from the farm gate through the food value chain is to implement Good Agricultural Practices (GAP), Good Manufacturing Practices (GMP), and Hazard Analysis of the Produce at the Critical Control Point (HACCP) (13,022,000; 2005). Post-harvest practices (drying, sorting, removal of broken and mouldy ones, keeping perishable staples in well-ventilated storage houses etc.) could also help in reducing food quality losses not excepting preharvest practices such as crop rotation, row planting, etc.6,41.
In 2011, The Food and Agriculture Organisation, (FAO) funded a Continental Programme on Post-Harvest Losses (PHL) Reduction in Sub-Saharan Africa, including Ghana. The FAO42 PHL report covered staple food commodities (processed and unprocessed), e.g. maize, sorghum, millet, cowpea, rice, plantain, cassava, cocoyam, yam, fruits (mango, orange, pineapple, tangerine) oil palm, tomatoes, okra, groundnut, bambara groundnut, etc. poultry and poultry products, Livestock (cattle, sheep, goats, guinea fowls, fish (marine and artisanal etc.) and made recommendations to increase food security along the food value chain in Ghana. FAO made a recommendation for improving food safety and security.
Prior to the FAO42 PHL report, and thereafter there have been over 41 fungal species identified belonging to more than 20 genera recorded as field and storage contaminants of staple foods, spice and spice products, grains and grain products, pulse and beans in Ghana43. These fungal contaminants included species of the aforementioned mycotoxin-producing genera: Aspergillus, Alternaria, Curvularia, Candida, Fusarium, Monilia, Geotrichum, Mucor, Neurospora, Oidiodendron, Paecilomyces, Penicillium, Pullularia, Rhizoctonia, Rhizopus, Syncephalastrum, Torula, Trichothecium, Saccharomyces and Trichoderma44,45,46,47,48,49,50,51,52,53,54,55 etc. Aspergillus species (A. alutaceus = A. ochraceus, A. candidus, A. fumigatus, A. glaucus, A. niger, A. sulphureus, A. terreus, A. amstelodami, A. ustus, A. nidulans, A. tamarii, A. flavus) predominated over other species encountered followed by Penicillium (P. digitatum, P. expansum, P. verrocusum, P. oxalicum, P. frequentans, P. purpurogenum, P. urticae) Paecilomyces (P. puntonii, P. varioti); Rhizopus (R. oligosporus, R. oryzae, R. stolonifer); Fusarium (F. verticillioides = F. moniliforme, F. nivale, F. oxysporum), Alternaria alternata, Curvularia lunata, Geotrichum albidium, Neurospora sitophila, etc.56.
When potential mycotoxin-producing species are predisposed to conducive environmental conditions such as in the tropics, risk factors triggering mycotoxigenesis are induced into action, especially when farmers and the general population are not abreast with the risk factors because of the paucity of information.
The pertinent literature on mycotoxins found in Ghanaian staple foods, spices, cereals, peanuts, and processed grain and peanut products is replete with examples of mycotoxin contamination of foods. Table 1 summarizes mycotoxins detected in Ghana’s staple foods, food products, spices, and seasoning products. These findings underscore the view that there is a paucity of information on the application of techniques to curtail toxin formation in our foods. The prerequisites for extending the shelf life and quality of agricultural produce are not well understood by the populace and farm handlers of stored agricultural produce. To the best of our knowledge, there is hardly any published report on the knowledge, handling of stored foods, attitude to the consumption of mycotoxin-contaminated foods as well as the pre-and post-harvest handling of food to preclude proliferation and in vivo mycotoxin formation in stored agricultural produce in Ghana.
Methodology
Study design
This study was both qualitative and quantitative research. A prospective cross-sectional study design was used to collate information from food vendors and members of the Ghanaian populace and their basic knowledge, attitudes, and practices to mitigate infection of fungi in foods using a structured online questionnaire.
Study site
The study was carried out across the country. Ghana is on the Gulf of Guinea, West Africa, where it covers about 23,884,245 ha of land and water and is positioned between latitudes 4°N and 11°N and longitudes 4° W and 2°E. Sixteen (16) regions and 216 districts constitute the country and are well defined by five broadly characterized agro – ecological zones, namely, Coastal Savannah, Evergreen Deciduous Forest, Transitional, and Savannah (Fig. 1). The population of Ghana currently stands at 31,000,062 people according to the data of Ghana Statistical Service87.
Map of Ghana showing the sixteen regions where sampling of views was carried out to assess the information required.
Desk study
A desk study was carried out to collate available information (on the internet) in Ghana on the occurrence and detection of some principal mycotoxins found in food. This is presented in Table 1. This spans the period 1986–2022.
Key—Population of regions.
1 = 653,266 | 2 = 2479 | 3 = 4,780,380 | 4 = 1,208,699 |
5 = 868,479 | 6 = 2,633,154 | 7 = 3,093,000 | 8 = 2,310,983 |
9 = 742,664 | 10 = 711,435 | 11 = 2,118,252 | 12 = 2,201,863 |
13 = 658,903 | 14 = 1,046,545 | 15 = 564,536 | 16 = 5,455,692 |
Inclusion criteria
Members of the Ghanaian populace who have basic knowledge in food safety.
Exclusion criteria
Members of the Ghanaian populace who do not have basic knowledge in food safety.
Determination of sample size
We adopted the prescribed formula of Yamane (1967) where:
In this formula, “n” represents the sample size to be calculated, while “N” is the relevant population. The value of “e‟ (standard error) depends on the required confidence level set by the researcher. If the confidence level is 0.95 percent, then the “e‟ value would be 0.05. In this study, a 95% confidence level was adopted. Our check revealed that the population of Ghana is about 31,000,000 which also represents food consumers in Ghana. Therefore, for N = 31,000,000, e = 5%, therefore n = 385.10 which approximates to 385. This implies that the minimum recommended size (number) is 385 respondents. We exceeded this and recruited 642 respondents nationwide.
Data collection
An online questionnaire was designed for the national survey and divided into 4 sections: socio–demographic characteristics; basic knowledge of the respondent on fungal presence in foods; respondent practices on the control and management of fungi in foods; respondent in-depth knowledge and management of fungi in foods. In the socio–demographic section, respondents were asked to provide information on their age, sex, occupation, and residential region. The basic knowledge of respondents on the presence of fungi in food allowed respondents to portray their layman’s knowledge about the presence of fungi in foods. The respondent’s practice for the control and management of fungi in food gave a clue as to how they handled foods that have been contaminated with mycotoxins and how they manage the occurrence of fungi. On the question of attitude towards the knowledge and management of fungi in foods, we derived from the respondents their knowledge and management of fungi in food. After due consultation with respondents who were 18 years and above, the questionnaire was uploaded onto all social media platforms.
The online survey was conducted between April to June 2021. A reminder was sent to all potential respondents in July 2021. All returned responses were checked and verified to ensure proper completion. A total of 642 validated questionnaires were returned.
Fully completed survey forms
Fully completed surveys were deemed valid responses. English was the main language used to communicate in the interview and questionnaire, but where there was the need for a different language, help was provided by an interpreter. All our national COVID-19 protocols were strictly adhered to, i.e. ensuring the wearing of face masks, the use of sanitizers, washing of hands thoroughly, and socially distancing during the survey.
All methods were carried out in accordance with relevant guidelines and regulations.
Ethics approval and consent to participate
Ethical clearance and permission were sought from the University of Health and Allied Sciences (UHAS) ethical clearance committee with Protocol Identification Number: UHAS-REC A.946 20–21. We confirm that informed consent was obtained from all subjects.
Statistical analysis
Completeness and consistency of the data were checked and entered into Statistical Package for Social Sciences (IBM SPSS) data analysis software version 20 was employed to analyze the quantitative data obtained from the respondents. IBM SPSS was used to detect and remove inaccurate and incomplete data. Results were presented as descriptive statistics in tables, and graphs to facilitate interpretation. A threshold of significance was set at < 0.05 (p < 0.05).
The Chi-Square test of association was carried out to determine whether there was a significant association between categorical variables. The Mann–Whitney test was also used to test differences between two groups, while the Kruskal–Wallis test was used to test differences between more than two groups. The Conover-Iman pairwise comparison test was carried out on the categories within the variables.The statistical Hosmer–Lemeshow test, correct classification rate (CCR), and Area under the curve (AUC) were considered as the parameters for the goodness of fit test for the model. The Hosmer–Lemeshow test measured how poorly a model predicts an event of interest. Another useful measure to assess the utility of a logistic regression model is the correct classification rate (CCR). The area under the curve (AUC) is a measure of the ability of a classifier to distinguish between classes and is used as a summary of the ROC curve. Finally, Wilcoxon paired sample comparison test was used to test the familiarity of the respondents with yeasts and molds as well as mycotoxins likely to be found in the foods. Microsoft Excel version 2013 was used to plot the graphs.
Results
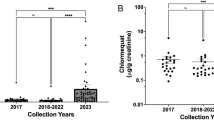
The results of the desk study on the incidence and detection of mycotoxins in foods in Ghana are summarized in Table 1. The products include staple foods, dehydrated and processed products, etc. Mycotoxins detected were aflatoxins, fumonisins, sterigmatocystin, tenuazonic acid, patulin, and penicillanic acid (Table 1). Fungal genera producing these toxins were predominantly in the genus Aspergillus, Penicillium, and Fusarium (Table 1).
Demographic data
The demographical data is summarized in Table 2. The majority of the respondents were between the ages of 18–25 years (46.6%); older people of 45 years and above formed the minority (1.9%). The respondents were predominated by males (52.3%) and by females (47.7%). The married constituted 69.3% and the remaining 30.7% were single. The majority of the respondents (80.4%) were either studying in tertiary education or had completed it, and only 3.0% had informal education. Interestingly, 44.5% of the total respondents have had a formal education; 52.5% were students and 3% were in informal education.
There was an inequitable return of questionnaires from the various regions. Most respondents resided in the Volta Region (24.8%) followed by Greater Accra (21.2%) and Eastern Region (10.0%) followed by Ashanti Region (9.8%). The remaining regions recorded less than 10% response with the least coming from North East (0.8%) and Western North (0.8%).
Knowledge of the types of mycotoxins in foods
Respondents indicated their knowledge of the mycotoxins likely to occur in Ghanaian foods. There were multiple responses and a summary of the results is shown in Table 3. The majority of the respondents selected aflatoxins 453/843 (55.7%) followed by ochratoxin 137/843 (16.3%) and fumonisins 136/843 (16.1%). Zearalenone 54/843 (6.4%) was less known to the respondents. The remaining mycotoxins (patulin, trichothecene, ergot alkaloids, vomitoxin (deoxynivalenol)) scored 01–0.6% (Table 3). Interestingly, 0.4% and 0.1% of the respondents believed that yeasts and bacteria, respectively, also produce mycotoxins. Finally, 5.7% had no idea about mycotoxins in foods (Table 3).
Identification of food commodities predisposed to infection by moulds and yeasts
Moulds and yeasts are ubiquitous and can be resident preferentially in any nutrient-rich substrate for their growth88. In this survey, respondents identified fruits, vegetables, and fish (12.7–16.9%) as the most susceptible to infection; cereals, meat, root, and tuber crops also experienced mouldiness (12.8–14.6%) while bread was mentioned by only 2.1% of the respondents (Table 4). Peanuts (groundnuts) and other nuts were also prone to contamination (10.7%). Interestingly, respondents found kenkey less susceptible (0.3%), contrary to the general view of the populace.
Multiple analysis of the response of respondents to the consumption of food despite identification of visible fungal growth
Table 5 summarises the results obtained from the survey using the questionnaire. Bread was the most consumed commodity (35.5%) despite visible signs of fungal contamination. This was followed by fish (9.9%), fruits (9.5%), meat (9.5%), and vegetables (9.0%). Only 0.2–0.3% of respondents ate infected root tubers and banku. Curiously, about 1.1% of the respondents avoided eating contaminated kenkey and 13.0% did not eat any of the listed foods found infected with fungi (Table 5).
The respondents from the regions adduced several reasons for attempting to eat food visibly infected with fungi as shown in Table 5. For example, 55.6% of the respondents consumed food visibly infected with fungi. Some respondents (15.5%) also ate food with visible fungal contamination because they believed nothing fatal happened to them after eating and a further 3.8% of respondents purchased such contaminated food because they were cheaper on the market (Table 6). A greater percentage (6.5%) did not find any change in taste after the contaminated food was cooked for eating.
Knowledge of the adverse health effects on humans who consume contaminated foods intoxicated with mycotoxins
Table 7 is a summary of the results obtained. About one-third (32.9%) of the respondents believe that consumption of mycotoxin-contaminated foods can cause stomach upsets and aching. On the other hand, 30.8% attributed the incidence of diarrhea after toxin intoxication to the ingestion of contaminated food. Still others (15.5%) indicated that immunosuppression can be attributed to mycotoxins, while some 11.7% indicated that toxins can cause fever. The remaining 9.0% had indicated that mycotoxins can be carcinogenic in their effect on humans and animals alike.
Knowledge and application of practices for the control and management of fungal contamination in stored foods
Although half of the respondents (50.7%) had seldom heard about fungi and their growth in foods, 34–38% either never heard about it and 5.3% had no clue about it (Table 8). Curiously, 77.9% of the respondents follow the traditionally prescribed storage conditions to preserve food. About 6.7–12.6% either discard visibly contaminated food or use only fresh food for cooking and consumption purposes (Table 8).
Statistical relatedness of data obtained from the survey
Tables 2, 3, 4, 5, 6, 7, 9, 10, 11, 12 and 13 summarize the rest of the statistical analysis of the data obtained from the questionnaire.
Results in Table 8 show that age was directly related to knowledge about the occurrence of fungi and mycotoxins in foods (p < 0.05); educational level also was positively related to knowledge about the occurrence of fungi and mycotoxins in foods (p < 0.05). All other demographic characteristics investigated (marital status, occupation, regional affiliation) were found to have no significant (p > 0.05) influence on the knowledge status of the respondents.
From Table 9, the same alphabet superscript assigned to categories denotes insignificant differences between groups. Different alphabets denote significant differences between groups.
Knowledge among age groups below 18 and 18–25 is significantly different from the age group 36–45.
Knowledge among those with secondary education is significantly different from those with basic, tertiary, and postgraduate education.
The Hosmer–Lemeshow test which is a statistical test for the logistic regression model is used frequently as a risk prediction model. Results showed that the model is a good fit (P-Value > 0.767). The CCR of 90.03% and the AUC of 66.60% also confirm that the model is a good fit ( Table 10).
With knowledge status as the dependent variable, the independent variables in the model were statistically insignificant except for the age group variable. Age groups above 45 years have increased odds of basic knowledge of fungi presence than the age group 36–45. Age groups 36–45 also have increased odds of basic knowledge of fungi presence than the age group 25–35. Age groups 25–35 also have increased odds of basic knowledge of fungi presence than the age group below 18 years. The age group 18–25 was used as the reference group.
In the Table 11, the average KAP score for knowledge indicated that, out of a total of 100%, there was adequate knowledge (63.8%) among the members of the Ghanaian populace. As to how familiar the respondents were with the terms mold and yeast, a mean score of 2.431 was obtained; how familiar the respondents were with the term mycotoxin recorded a mean score of 2.014 which is lower than the average mean of the knowledge of respondents. The results show that the familiarity of the respondents with the terms; molds, yeast, and mycotoxins were directly related to their knowledge about the occurrence of mycotoxins in foods (p < 0.05) (Table 12).
The Chi-square test of association was conducted to ascertain whether a statistical relationship existed between the practices for the control and management of fungi in food and their knowledge of the occurrence of fungi in foods. In terms of the practice of management and control of fungi in foods, respondents who did not consume food showing visible fungi growth constituted 56.4%; respondents who consumed food with visible fungi growth constituted with them was 36.0%. Results in Table 13 show that the consumption of food showing visible fungal growth is significantly (p < 0.05) related to the knowledge about the occurrence of fungi in foods. Respondents who inspected food for the presence of fungi on foods before consumption was 81.2%, while respondents who did not check for the presence of molds and fungi on foods before consumption constituted 18.8%. The results showed that it is not related to the knowledge of the occurrence of fungi in foods (p > 0.05).
Discussion
Mycotoxin contamination of foods and processed food products is a universal problem that denies the grains from crop harvest the full benefits for use in food security. No country is exempt from fungal intoxication in food. The results of the desktop study showed a whole array of foodstuffs contaminated by potent mycotoxins of health importance and belonging to the genera Aspergillus, Penicillium, and Fusarium (Table 1). Local research into the occurrence of mycotoxins in Ghana is encouraging but a lot more needs to be done particularly in the area of damage to human health and its long-term effects on longevity. The pertinent literature in West Africa is replete with studies on the incidence of mycotoxins in staple edible foods and spices. Mycotoxins detected include aflatoxins, fumonisins, ochratoxins, penicillinic acid, patulin, vomitoxin (deoxynivalenol), zearalenone, trichothecenes28,38,89,90,91,92,93,94,95,96. The same is true for East and Central Africa6,38,97,98,99,100. Extensive studies on mycotoxins in staples, edible foods, and spices have also been carried out in Southern Africa101 and Egypt102,103. What needs to be underscored, is the education of the population to identify conditions of storage that predispose stored foods to mycotoxin contamination and the need to avoid the use of mouldy foods for animal and human consumption.
Results from the current study show that the majority of the respondents in the study were between the youthful ages of 18–25 yrs and had adequate knowledge about the contamination of foods by fungi. This agrees with the findings of104 who found the knowledge of natural toxins in foods by students of ages between 21 and 25 yrs in tertiary institutions in Ghana. This trend could be attributed to the larger volume of information on the internet available to the computer-literate youth on their mobile phones, laptops, and other gadgets. Another source of information on food intoxication could come from occasional educative FM radio, TV programs, and videos that they could access from their phones out of curiosity.
Our present result contrasts the findings of97 in Kenya. They showed that respondents above 35yrs were more knowledgeable about fungi and natural mycotoxin contamination because of their field experience of more than 20yrs as farmers. Cultural influences may therefore determine the acquisition of the intuition to identify and deal with natural mycotoxin contamination in stored foods.
There was a preponderance of male over female respondents in this present study. Presumably, women carry out duties related to food processing and cooking in addition to other ancillary activities at home and so makes them relatively busy. Indeed, Jere et al.105 reported that in Malawi, women generally carry out food processing and cooking activities in addition to other household chores which keep them occupied for the best part of the day. Jere et al.105 carried out studies related to the exposure of school children to aflatoxins (from Aspergillus flavus) and fumonisins (Fusarium species) in Malawi and confirmed the detection of high concentrations of mycotoxins in food prepared by women in addition to their other household chores. The same was true in Tanzania106 and Nigeria107. They surmised that educational level plays a major role in the detection and corrective interventions in mycotoxicosis as earlier endorsed by108.
Our current study showed that in Ghana, female respondents were significantly (p < 0.05) less knowledgeable than their male counterparts (data not shown), while Matumba et al.6 stated that women played a significant role in the hawking, preparation, and utilization of foods in Malawi. In other instances in Tanzania, Magembe et al.97 found that female respondents showed greater and adequate awareness of mould infection than men. Presumably, both cultural and educational differences in Africa can influence the detection of fungi, natural mycotoxin contamination, and response to practical control of storage diseases of fungal origin by their ability to identify and infer their presence in foods. In this present study, the majority of our respondents have attained tertiary education and had adequate knowledge about the presence of fungi in food while the rest had either no education background or are semi-literates with a low level of formal education. Lesuuda et al.109 also reported that in Kenya, the majority of their respondents were primary school leavers, and their knowledge of mycotoxin contamination of staple food and dehydrated cereal grains was significantly low (p < 0.05).
The statistical analysis managed the inequitable return of questionnaires from the regions since data for the entire country was bulked to exceed the minimum number of respondents required for significance. The majority of the respondents were familiar with the terms mould and yeasts and mycotoxins, although the majority attributed ingestion of mycotoxins to stomach ache and diarrhea while about 9% attributed mycotoxins as the agent of cancer and 15% believed mycotoxins cause immune suppressions (Table 7). Curiously, 30.8% attributed mycotoxin ingestion to diarrhea (Table 7). Clearly, their ignorance can be traced to their low level of education as reported by97 in Tanzania. Azaman et al.110 investigated stakeholders’ knowledge, attitude, and practices (KAP) towards aflatoxin contamination in peanut–based products and concluded that knowledge influences awareness as well as attitudes and conservation and management behavior of farmers. The adequate KAP score of 63.08 + 13.21% (Table 11) obtained in this present study agrees with the conclusion of110.
It is well known worldwide that aflatoxins, especially aflatoxin B1, is the most toxic mycotoxin with severe debilitating effects on humans and animals alike12,111,112. The majority of the respondents in this study (55.7%) (Table 3) mentioned aflatoxins as the major mycotoxin they were aware of followed by ochratoxin (16.3%) and fumonisins (16.1%); the remaining mycotoxins were less known (0.1–6.4%); while 5.79% had no idea about mycotoxins in foods. Toma113 and Matumba et al.6 also found from their studies in Ethiopia and Tanzania respectively, that aflatoxins are the best well-known mycotoxins. Studies in Kenya by Lesuuda et al.109 agree with our findings that the majority of their respondents knew very little about other mycotoxins other than aflatoxins. The pertinent literature contains information on the association between inadequate knowledge about aflatoxin contamination with high rates of exposure to aflatoxins100,108,114,115.
Fungal spores are ubiquitous and can settle on any kind of food substrate rich enough to support their growth and proliferation provided there are conducive environmental and physical conditions. Naturally, some staple foods, cereals and grains, fruits and vegetables, etc. provide a miscellany of nutrients and some better substrates for fungal growth than others88.
Respondents in this paper identified foods consumed in spite of visible fungal growth (Table 5). Fruits contaminated with fungi are discarded when completely infected. However, in many instances, mangoes, oranges and guavas etc. are trimmed to remove infected portions and then eaten. Unfortunately, the presence of the fungus imparts some toxic metabolites, and mycotoxins associated with fruits are mostly patulin, aflatoxin, ochratoxin, fusarial toxins, and Alternaria toxins6. Cereals and legumes are often infected by mycotoxins such as aflatoxins and fumonisins. Interestingly, respondents (35.5%), named bread as the most consumed food even with visible fungi and the least (0.2–0.3%) root tubers and banku (made from fermented maize flour). Respondents also scored 1.1% for kenkey (another fermented maize product) which is a popular meal in Ghana. The fermented dough for the preparation of kenkey made from maize grains is first soaked in water for 2–3 days, after which the floating damaged and infected grains are removed by decanting from the surface of the water. This process is followed by blending the soaked grains in a disc attrition device corn miller, and the resulting dumpling is fermented for 2–3 days before using the dumpling to prepare kenkey. It is known that the clearing and fermentation stages reduce the risk of mycotoxin contamination. It is not surprising that only 1.1% of the respondents indicated that maize is consumed even if visibly mouldy. Indeed, there has been only one record of aflatoxin contamination of kenkey in Ghana60 but the infection of grains and cereals and legumes in storage in silos and home barns is well documented by many workers in Ghana7,44,58,59,64,70,71,72,73,84.
Respondents to our structured questionnaires were aware of the health problems associated with the consumption of food contaminated with fungal toxins and named ailments such as stomach ache, diarrhea, suppression of the immune system, cancer, etc. (Table 7). This finding is at variance with the report of Matumba et al.6 in Malawi where consumption of mouldy foods was attributed to malaria and high fever. Lack of adequate information and minimal educational background could be the cause of such ignorance. Furthermore, the problem is accentuated by some health professionals and agricultural extension officers knowing little or not having heard about the debilitating effect of continuous ingestion of foods laden with fungal contaminants in Ghana116,117. On the contrary, Llesanmi and Llesanmi118 reported that in Nigeria, health workers were abreast with the knowledge of infection of foods by mycotoxins produced by fungi and the health risks associated with it. However, the prescribed method of removing of mouldy grains from farm produce is not as strictly adhered to. Jolly et al.108 stated that although farmers in some African countries are aware of the detrimental consequences of eating contaminated foods, their origin, and remedial traditional practices, this has not been strictly adhered to in practical terms. It is obvious that public education is lacking in Ghana on the occurrence of aero-mycoflora in storage facilities and in the fresh before harvest and the subsequent formation of metabolites in foods for human consumption. Cutting-edge technological methods are available for precluding fungi in storage and during food processing. Emphasis should be on adapting and applying good storage management practices and changing the behavioral lassitude to protect oneself from ingesting mycotoxin-contaminated foods. Unfortunately, the mould contaminated cereals, legumes, fruits, vegetables, etc. have been used inadvertently for animal and human feed, especially for chickens, ruminants, and others119,120. This is subsequently passed on in the meat produced and is unintentionally ingested with the toxin.
Kortei et al.121 reported that in Ghana cereals (e.g. Sorghum) with visible mouldiness have been used to prepare local alcoholic beverages with impunity leading to the consumption of mycotoxins (aflatoxins, fumonisins, ochratoxins, penicillinic acid, etc.). This viewpoint is endorsed by the data in Tables 4, 7, 11 and 12 showing the paucity of relevant information to the public on the potential hazards of mycotoxicosis.
Essentially, a “School Feeding Programme” from UNESCO (Millenium Development Goals) (UNESCO, 2000) has been introduced in some African countries to keep children at school and improve their erudition through nourishment. The formulation of food and times of the day the pupils are fed vary from country to country. Food analysis of the raw materials and food served to the children indicated the intake of mycotoxins (aflatoxins, ochratoxins, fumonisin, zearalenone, vomitoxin (deoxynivalenol) etc.) are beyond permissive levels6,97,100,105,109.
The Government of Ghana has adopted the 2nd Millenium Development Goals of the United Nations, seeking to promote education in all countries through many interventions including the introduction of Nutrition and School Feeding Programmes, Ghana School Feeding Programme (GSFP) began in 2005122. The aim is to achieve food security by providing public primary school students with one hot meal per day, usually procured from the farm produce of local farmers. It is one of the strategies for achieving the Millenium Development Goal 2 (MDGs) on hunger, poverty and primary education123,124. The GSFP is an indicator of the Comprehensive Africa Agricultural Development Programme CAADP Pillar 3, which seeks to enhance food security and reduce hunger in line with the UN Sustainable Development Goals (MDGs) on hunger, poverty, and malnutrition (Schoolfeeding.gov.gh).
Granted, the food ingredients used come from buffer stocks and farmer supply. There is a need to screen the raw materials for the presence of mycotoxins owing to the fact that we might be feeding our future leaders with foods containing mycotoxins with the potential of having a debilitating effect on the health of the youth. The urgency of disseminating information on the potential danger and how to handle it in foods and feeds should be rigorously addressed125 in the near future by our scientific food storage and management experts.
Conclusion
In summary, there was adequate knowledge (63.8%) among the members of the Ghanaian populace regarding the knowledge and attitude of the occurrence of fungi and mycotoxins in foods as well as during storage. However, the respondents’ familiarity with the terms mold and yeasts (fungi) and the different types of mycotoxins was low. This undeniably calls for the intensification of education of the Ghanaian populace on yeasts and molds as well as mycotoxins in relation to their potential to cause grave harm to humans and animals as they occur in our foods.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon a reasonable request.
References
Walker, S., Jaime, R., Kagot, V. & Probst, C. Comparative effects of hermetic and traditional storage devices on maize grain: Mycotoxin development, insect infestation and grain quality. J. Stored Prod. Res. 77, 34–44 (2018).
Green, T. A., Schroeter, B. & Sancho, L. G. Plant Life in Antarctica 13. Funct. Plant Ecol. https://doi.org/10.1201/9781420007626-139 (2007).
Bbosa, G. S. et al. Review of the biological and health effects of aflatoxins on body organs and body systems. Aflatoxins Rec. Adv. Fut. Prospects 12, 239–265 (2013).
Fung, F. & Clark, R. F. Health effects of mycotoxins: A toxicological overview. J. Toxicol. Clin. Toxicol. 42, 217–234 (2004).
Adaku Chilaka, C. & Mally, A. Mycotoxin occurrence, exposure and health implications in infants and young children in Sub-Saharan Africa: A review. Foods 9, 1585 (2020).
Matumba, L. et al. Uncommon occurrence ratios of aflatoxin B 1, B 2, G 1, and G 2 in maize and groundnuts from Malawi. Mycotoxin Res. 31, 57–62 (2015).
Bediako, K. A. et al. Aflatoxin contamination of groundnut (Arachis hypogaea L.): Predisposing factors and management interventions. Food Control 98, 61–67 (2019).
Atanda, O., Ogunrinu, M. & Olorunfemi, F. A neutral red desiccated coconut agar for rapid detection of aflatoxigenic fungi and visual determination of aflatoxins. World Mycotoxin J. 4, 147–155 (2011).
Elkenany, R. & Awad, A. Types of mycotoxins and different approaches used for their detection in foodstuffs. Mansoura Vet. Med. J. 22, 25–32 (2021).
Norlia, M. et al. Aspergillus section Flavi and aflatoxins: Occurrence, detection, and identification in raw peanuts and peanut-based products along the supply chain. Front. Microbiol. 10, 2602 (2019).
Joint, F., Additives, W. E. C. F. & Organization, W. H. Evaluation of certain food additives and contaminants: forty-ninth report of the Joint FAO/WHO Expert Committee on Food Additives (World Health Organization, 1999).
Odamtten, G.T. Natural occurrence, economic impact and control of Aflatoxins in Africa. In: WHO Expert Committee Meeting on Aflatoxins and Health. Brazaville, Republic of Congo (2005).
Ostry, V., Malir, F., Toman, J. & Grosse, Y. Mycotoxins as human carcinogens—The IARC Monographs classification. Mycotoxin Res. 33, 65–73 (2017).
Organization, W. H. & Cancer, I. A. f. R. o. Some naturally occurring substances: food items and constituents, heterocyclic aromatic amines and mycotoxins. IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans 56 (1993).
Reddy, L. & Bhoola, K. Ochratoxins—Food contaminants: Impact on human health. Toxins 2, 771–779 (2010).
Pfohl-Leszkowicz, A. & Manderville, R. A. Ochratoxin A: An overview on toxicity and carcinogenicity in animals and humans. Mol. Nutr. Food Res. 51, 61–99 (2007).
Abouzied, M. et al. Ochratoxin A concentrations in food and feed from a region with Balkan Endemic Nephropathy. Food Addit. Contam. 19, 755–764 (2002).
Wang, Y. et al. Ochratoxin A producing fungi, biosynthetic pathway and regulatory mechanisms. Toxins 8, 83 (2016).
Ayoub, F., Reverberi, M., Ricelli, A., d’Onghia, A. M. & Yaseen, T. Early detection of Aspergillus carbonarius and A. niger on table grapes: A tool for quality improvement. Food Addit. Contam. 27, 1285–1293 (2010).
Abrunhosa, L., Paterson, R., Kozakiewicz, Z., Lima, N. & Venâncio, A. Mycotoxin production from fungi isolated from grapes. Lett. Appl. Microbiol. 32, 240–242 (2001).
Pitt, J., Basilico, J., Abarca, M. & Lopez, C. Mycotoxins and toxigenic fungi. Med. Mycol. 38, 41–46 (2000).
O’Callaghan, J., Caddick, M. & Dobson, A. A polyketide synthase gene required for ochratoxin A biosynthesis in Aspergillus ochraceus. Microbiology 149, 3485–3491 (2003).
EFS Authority. Opinion of the scientific panel on contaminants in the food chain [CONTAM] related to ochratoxin A in food. EFSA J. 4, 365 (2006).
Kumagai, S. et al. Aflatoxin and ochratoxin A contamination of retail foods and intake of these mycotoxins in Japan. Food Addit. Contam. 25, 1101–1106 (2008).
Brera, C. et al. Ochratoxin A in cocoa and chocolate products from the Italian market: Occurrence and exposure assessment. Food Control 22, 1663–1667 (2011).
Sánchez-Hervás, M., Gil, J., Bisbal, F., Ramón, D. & Martínez-Culebras, P. Mycobiota and mycotoxin producing fungi from cocoa beans. Int. J. Food Microbiol. 125, 336–340 (2008).
Mounjouenpou, P. et al. Filamentous fungi producing ochratoxin a during cocoa processing in Cameroon. Int. J. Food Microbiol. 121, 234–241 (2008).
Copetti, M. V., Iamanaka, B. T., Pitt, J. I. & Taniwaki, M. H. Fungi and mycotoxins in cocoa: From farm to chocolate. Int. J. Food Microbiol. 178, 13–20 (2014).
Altomare, C., Logrieco, A. F. & Gallo, A. Mycotoxins and mycotoxigenic fungi: Risk and management. A challenge for future global food safety and security (2021).
Smith, G. W. Fumonisins. In Veterinary Toxicology (ed. Smith, G. W.) 1003–1018 (Elsevier, 2018).
Ferrigo, D., Raiola, A. & Causin, R. Fusarium toxins in cereals: Occurrence, legislation, factors promoting the appearance and their management. Molecules 21, 627 (2016).
Frizzell, C. et al. Endocrine disrupting effects of zearalenone, alpha-and beta-zearalenol at the level of nuclear receptor binding and steroidogenesis. Toxicol. Lett. 206, 210–217 (2011).
Sobrova, P. et al. Deoxynivalenol and its toxicity. Interdiscip. Toxicol. 3, 94–99 (2010).
Varga, J., Due, M., Frisvad, J. C. & Samson, R. A. Taxonomic revision of Aspergillus section Clavati based on molecular, morphological and physiological data. Stud. Mycol. 73, iii–iii (2012).
Frisvad, J. C., Smedsgaard, J., Larsen, T. O. & Samson, R. A. Mycotoxins, drugs and other extrolites produced by species in Penicillium subgenus Penicillium. Stud. Mycol. 49, 201–241 (2004).
Puel, O., Galtier, P. & Oswald, I. P. Biosynthesis and toxicological effects of patulin. Toxins 2, 613–631 (2010).
Houbraken, J., Samson, R. A. & Frisvad, J. C. Byssochlamys: significance of heat resistance and mycotoxin production. In Advances in Food Mycology (eds Houbraken, J. et al.) 211–224 (Springer, 2006).
Mutegi, C. et al. Incidence of aflatoxin in peanuts (Arachis hypogaea Linnaeus) from markets in Western, Nyanza and Nairobi Provinces of Kenya and related market traits. J. Stored Prod. Res. 52, 118–127 (2013).
Gong, Y. et al. Postweaning exposure to aflatoxin results in impaired child growth: A longitudinal study in Benin, West Africa. Environ. Health perspect. 112, 1334–1338 (2004).
Lewis, L. et al. Aflatoxin contamination of commercial maize products during an outbreak of acute aflatoxicosis in eastern and central Kenya. Environ. Health Perspect. 113, 1763–1767 (2005).
Reddy, K., Nurdijati, S. & Salleh, B. An overview of plant-derived products on control of mycotoxigenic fungi and mycotoxins. Asian J. Plant Sci. 9, 126 (2010).
Tefera, T. Post-harvest losses in African maize in the face of increasing food shortage. Food secur. 4, 267–277 (2012).
Odamtten, G. T., Nartey, L., Wiafe-Kwagyan, M., Anyebuno, G. & Kyei-Baffour, V. Resident microbial load, toxigenic potential and possible quality control measures of six imported seasoning powders on the Ghanaian market. J. Nutr. Health Food Eng. 8, 24–35 (2018).
Kortei, N. K., Tetteh, R. A., Wiafe-Kwagyan, M., Amon, D. N. K. & Odamtten, G. T. Mycobiota profile, phenology, and potential toxicogenic and pathogenic species associated with stored groundnuts (Arachis hypogaea L.) from the Volta Region, Ghana. Food Sci. Nutr. https://doi.org/10.1002/fsn3.2719 (2022).
Ahene, R., Odamtten, G. T. & Owusu, E. Fungal and bacterial contaminants of six spices and spice products in Ghana. Afr. J. Environ. Sci. Technol. 5, 633–640 (2011).
Kottoh, D. Radiation decontamination of three local spices and khebab spice-mix and some aspects of their physiochemical and nutritional properties before and after gamma irradiation. MPhil Thesis, School of Nuclear and Allied Sciences, College of Basic and Applied Sciences, University of Ghana, Legon, pp 119 (2011).
Wareing, P. W., Westby, A., Gibbs, J. A., Allotey, L. T. & Halm, M. Consumer preferences and fungal and mycotoxin contamination of dried cassava products from Ghana. Int. J. Food Sci. Technol. 36, 1–10 (2001).
Minamor, A. A. & Odamtten, G. T. Radial growth of three Paecilomyces species isolated from two Ghanaian maize varieties Abeleehi and Obaatanpa on five different media and the effects of their culture filtrate on seed germination and radicle elongation of Abeleehi and Obaatanpa. Int. J. Curr. Microbiol. Appl. Sci. 5, 604–617 (2016).
Minamor, A. A. & Odamtten, G. T. Influence of the culture filtrate of three Paecilomyces species on some growth parameters, chlorophyll content, and root anatomy of two Ghanaian maize varieties (Abeleehi and Obaatanpa) and on germination capacity of tomato and pepper seeds. Am. J. Microbiol. Res. 5, 51–58 (2017).
Addo, A. Premilinary studies on the microbiological and nutrient quality of three local spices on the Ghanaian market and the control of resident microflora by gamma irradiation: BSc. BSc. Hons Dissertation, Department of Botany, University of Ghana, Legon (2005).
Ofori-Appiah, D. Decontamination of sliced and powdered okra (Abelmoschus esculentus) and some aspects of nutrient quality before and after gamma irradiation. MPhil Thesis, School of Nuclear and Allied Sciences, College of Basic and Applied Sciences, University of Ghana, Legon, 197 (2012).
Agyemang, A. Radiation preservation of tiger nut (Cyperus esculentus L.) with special reference to fungi and the effect on some aspects of the physico-chemical properties of the nuts before and after radiation MPhil Thesis. Radiation Processing, School of Nuclear and Allied Sciences, College of Basic and Applied Sciences, University of Ghana 172 (2011).
Odamtten, G. T. Studies on the control of fungal contamination and aflatoxin production by Aspergillus flavus Link in a cereal grain by the combination treatment of heat and irradiation. PhD Thesis, Wageningen Agricultural University and Research Centres, Department of Food Science, Microbiology and Hygeine, PUDOC Publication. pp190 (Wageningen University and Research, 1986).
Odamtten, G. T., Appiah, V. & Langerak, D. Influence of inoculum size of Aspergillus flavus link on the production of aflatoxin B1 in maize medium before and after exposure to combination treatment of heat and gamma radiation. Int. J. Food Microbiol. 4, 119–127 (1987).
Odamtten, G.T. A survey of the mycoflora of maize grains stored at 26±3° C and 75±5% RH. In: Proceedings 12th Biennial Conf. of the Ghana Sci. Assoc.5–11th April, 1981, pp 14.
Odamtten, G.T. Plant Diseases, Crop Production and Food Security in Ghana. Inaugural Lecture delivered as a fellow of the Ghana Academy of Arts and Sciences, GAAS, 22nd June 2017 (2017).
Odamtten, G. T., Appiah, V. & Langerak, D. I. Preliminary studies of the effects of heat and gamma irradiation on the production of aflatoxin B1 in static liquid culture, by Aspergillus flavus link NRRL 5906. Int. J. Food Microbiol. 3, 339–348 (1986).
Kortei, N. K. et al. The occurrence of aflatoxins and human health risk estimations in randomly obtained maize from some markets in Ghana. Sci. Rep. 11, 1–13 (2021).
Kortei, N. K. et al. Exposure and risk characterizations of ochratoxins A and aflatoxins through maize (Zea mays) consumed in different agro-ecological zones of Ghana. Sci. Rep. 11, 1–19 (2021).
Kpodo, K., Sørensen, A. & Jakobsen, M. The occurrence of mycotoxins in fermented maize products. Food Chem. 56, 147–153 (1996).
Kpodo, K. & Halm, M. Fungal and aflatoxin contamination of maize stored in silos and warehouses in Ghana (1990).
Kpodo, K., Thrane, U. & Hald, B. Fusaria and fumonisins in maize from Ghana and their co-occurrence with aflatoxins. Int. J. Food Microbiol. 61, 147–157 (2000).
Kpodo, K. A. Fusaria and Fumonisins in Maize and Fermented Maize Products from Ghana, Royal Veterinary and Agricultural University, Department of Dairy and Food (2001).
Kpodo, K., Ayernor, G., Shephard, G. & Jakobsen, M. Exposure to fumonisins through Kenkey–a Ghanaian fermented maize product. Mycotoxins and phycotoxins, 209 (2006).
Atter, A., Ofori, H., Anyebuno, G. A., Amoo-Gyasi, M. & Amoa-Awua, W. K. Safety of a street vended traditional maize beverage, ice-kenkey, in Ghana. Food Control 55, 200–205 (2015).
Kumi, J. et al. Aflatoxins and fumonisins contamination of home-made food (weanimix) from cereal-legume blends for children. Ghana Med. J. 48, 121–126 (2014).
Opoku, N., Achaglinkame, M. A. & Amagloh, F. K. Aflatoxin content in cereal-legume blends on the Ghanaian market far exceeds the permissible limit. Food Secur. 10, 1539–1545 (2018).
Omari, R. & Anyebuno, G. Risk assessment of aflatoxins in maize-groundnuts complemen-tary foods consumed by Ghanaian infants. J. Food qual. Hazards Control https://doi.org/10.18502/jfqhc.7.3.4144 (2020).
Kortei, N. K., Agyekum, A. A., Akuamoa, F., Baffour, V. K. & Alidu, H. W. Risk assessment and exposure to levels of naturally occurring aflatoxins in some packaged cereals and cereal based foods consumed in Accra Ghana. Toxicol. Rep. 6, 34–41 (2019).
Blankson, G., Mills-Robertson, F. & Ofosu, I. Survey of occurrence levels of aflatoxins in selected locally processed cereal-based foods for human consumption from Ghana. Food Control 95, 170–175 (2019).
Kortei, N. K. et al. Aflatoxins in randomly selected groundnuts (Arachis hypogaea) and its products from some local markets across Ghana: Human risk assessment and monitoring. Toxicol. Rep. 8, 186–195 (2021).
Awuah, R. T. & Kpodo, K. A. High incidence of Aspergillus flavus and aflatoxins in stored groundnut in Ghana and the use of a microbial assay to assess the inhibitory effects of plant extracts on aflatoxin synthesis. Mycopathologia 134, 109–114 (1996).
Bediako, K. A. et al. Prevalence of fungi and aflatoxin contamination in stored groundnut in Ghana. Food Control 104, 152–156 (2019).
Anyebuno, G., Kyei-Baffour, V. & Narh, D. Effect of manual sorting on Aflatoxins content in peanuts (Arachis Hypogaea, L) from a Ghanaian market. Ghana J. Agric. Sci. 52, 5–15 (2018).
Omore, A. O. et al. Employment Generation Through Small-scale Dairy Marketing and Processing: Experiences from Kenya, Bangladesh and Ghana: A Joint Study by the ILRI Market-oriented Smallholder Dairy Project and the FAO Animal Production and Health Division (Food & Agriculture Org, 2004).
Addo-Boadu, C. Aflatoxin M1 Contamination of Raw Cow Milk, Milk Products and Dietary Exposure (2019).
Kortei, N. K. et al. Exposure assessment and cancer risk characterization of aflatoxin M1 (AFM1) through ingestion of raw cow milk in southern Ghana. Toxicol. Rep. 9, 1189–1197 (2022).
Kortei, N. K. et al. Aflatoxin M1 exposure in a fermented millet-based milk beverage ‘brukina’and its cancer risk characterization in Greater Accra, Ghana. Sci. Rep. 12, 1–13 (2022).
Kortei, N. K. & Annan, T. Aflatoxin M1 contamination of Ghanaian traditional soft cottage cheese (Wagashie) and health risks associated with its consumption. J. Food Qual. 2022, 1–12 (2022).
Mensah, J., Owusu, E. & Anyebuno, G. Growth and production of aflatoxins by a flavus in aqueous fruit extracts of pepper, okra and tomato (2014).
Anyebuno, G. Mycoflora and aflatoxin levels in millet samples from ten markets in Accra (2002).
Kortei, N. K. et al. Mycoflora, aflatoxins, and antimicrobial properties of some Ghanaian local spices and herbs. J. Food Saf. 42, e12996 (2022).
Kortei, N. K. et al. Toxicogenic fungi, aflatoxins, and antimicrobial activities associated with some spices and herbs from three selected markets in Ho municipality, Ghana. Int. J. Food Sci. 2022, 1–15 (2022).
Kortei, N. K. et al. Dietary exposure to aflatoxins in some randomly selected foods and cancer risk estimations of cereals consumed on a Ghanaian market. J. Food Qual. 2022, 1–11 (2022).
Kpodo, K. A. & Bankole, S. A. Mycotoxin contamination in foods in West and Central Africa. Mycotoxins: Detection Methods, Management, Public Health and Agricultural Trade, CABI Publishing, Wallingford, UK, 103–116 (2008).
Kyei-Baffour, V. O. et al. A validated HPLC–FLD method for the determination of mycotoxin levels in sun dried fermented cocoa beans: Effect of cola nut extract and powder. LWT 148, 111790 (2021).
GS Service. 2010 Population & Housing Census Report: Urbanisation in Ghana (Ghana Statistical Service, 2014).
Hymery, N. et al. Filamentous fungi and mycotoxins in cheese: A review. Compr. Rev. Food Sci. Food Saf. 13, 437–456 (2014).
Udomkun, P. et al. Mycotoxins in Sub-Saharan Africa: Present situation, socio-economic impact, awareness, and outlook. Food Control 72, 110–122 (2017).
Akpo-Djènontin, D. O. O., Gbaguidi, F., Soumanou, M. M. & Anihouvi, V. B. Mold infestation and aflatoxins production in traditionally processed spices and aromatic herbs powder mostly used in West Africa. Food Sci. Nutr. 6, 541–548 (2018).
Hell, K. & Mutegi, C. Aflatoxin control and prevention strategies in key crops of Sub-Saharan Africa. Afr. J. Microbiol. Res. 5, 459–466 (2011).
Vismer, H. F., Shephard, G. S., Rheeder, J. P., van der Westhuizen, L. & Bandyopadhyay, R. Relative severity of Fumonisin contamination of cereal crops in West Africa. Food Addit. Contam. 32, 1952–1958 (2015).
Jonathan, S. G., Adeniyi, M. A. & Asemoloye, M. D. Fungal biodeterioration, aflatoxin contamination, and nutrient value of “suya spices”. Scientifica 2016, 1–6 (2016).
Haruna, M. et al. Incidence of fungal flora and aflatoxin in some spices sold in central market, Funtua, Nigeria. UMYU J. Microbiol. Res. 2, 47–53 (2017).
Chilaka, C. A., De Boevre, M., Atanda, O. O. & De Saeger, S. Occurrence of Fusarium mycotoxins in cereal crops and processed products (Ogi) from Nigeria. Toxins 8, 342 (2016).
Njumbe Ediage, E., Hell, K. & De Saeger, S. A comprehensive study to explore differences in mycotoxin patterns from agro-ecological regions through maize, peanut, and cassava products: A case study, Cameroon. J. Agric. Food Chem. 62, 4789–4797 (2014).
Magembe, K., Mwatawala, M., Mamiro, D. & Chingonikaya, E. Assessment of awareness of mycotoxins infections in stored maize (Zea mays L.) and groundnut (Arachis hypogea L.) in Kilosa district, Tanzania. Int. J. Food Contam. 3, 1–8 (2016).
Mwangi, W. W., Nguta, C. M. & Muriuki, B. G. Aflatoxin contamination in selected spice preparations in the Nyahururu retail market, Kenya. J. Sci. Res. Rep. 3, 917–923 (2014).
Kankolongo, M. A., Hell, K. & Nawa, I. N. Assessment for fungal, mycotoxin and insect spoilage in maize stored for human consumption in Zambia. J. Sci. Food Agric. 89, 1366–1375 (2009).
Lukwago, F. B., Mukisa, I. M., Atukwase, A., Kaaya, A. N. & Tumwebaze, S. Mycotoxins contamination in foods consumed in Uganda: A 12-year review (2006–18). Sci. Afr. 3, e00054 (2019).
Motloung, L. et al. Study on mycotoxin contamination in South African food spices. World Mycotoxin J. 11, 401–409 (2018).
El-Tahan, F., El-Tahan, M. & Shebl, M. Occurrence of aflatoxins in cereal grains from four Egyptian governorates. Nahrung 44, 279–280 (2000).
El-Kady, I., El-Maraghy, S. & Mostafa, M. E. Natural occurrence of mycotoxins in different spices in Egypt. Folia Microbiol. 40, 297–300 (1995).
Kortei, N. et al. Knowledge and Attitude of consumers about natural food toxins: A case of tertiary students in the Volta region of Ghana. J. Food Qual. Hazards Control https://doi.org/10.18502/jfqhc.8.3.7196 (2021).
Jere, G. M., Abong, G., Njue, L., Masamba, K. & Omayio, D. Exposure of school children to aflatoxins and fumonisins through maize-based diets in school meals programme in Salima District, Malawi. Afr. J. Food Agric. Nutr. Dev. 20, 16793–16809 (2020).
Kamala, A. et al. Risk of exposure to multiple mycotoxins from maize-based complementary foods in Tanzania. J. Agric. Food Chem. 65, 7106–7114 (2017).
Ezekiel, C. N. et al. Mycotoxins in uncooked and plate-ready household food from rural northern Nigeria. Food Chem. Toxicol. 128, 171–179 (2019).
Jolly, C. M., Bayard, B., Awuah, R. T., Fialor, S. C. & Williams, J. T. Examining the structure of awareness and perceptions of groundnut aflatoxin among Ghanaian health and agricultural professionals and its influence on their actions. J. Socio-Econ. 38, 280–287 (2009).
Lesuuda, L., Obonyo, M. A. & Cheserek, M. J. Determinants of knowledge about aflatoxin and fumonisin contamination in sorghum and postharvest practices among caregivers of children aged 6–59 months in Kerio Valley, Kenya. Food Sci. Nutr. 9, 5435–5447 (2021).
Azaman, N. N. M., Kamarulzaman, N. H., Shamsudin, M. N. & Selamat, J. Stakeholders’ knowledge, attitude, and practices (KAP) towards aflatoxins contamination in peanut-based products. Food Control 70, 249–256 (2016).
Richard, J. L. Mycotoxins-an overview. Romer Labs Guide Mycotoxins 1, 1–48 (2000).
Centers for Disease Control and Prevention. Outbreak of aflatoxin poisoning-eastern and central provinces, Kenya, January–July 2004. MMWR Morb. Mortal. Wkly. Rep. 3, 790–793 (2004).
Toma, A. Knowledge, attitude and practice of farmers’ towards aflatoxin in cereal crops in Wolaita zone, Southern Ethiopia. EC Nutr. 14, 247–254 (2019).
Misihairabgwi, J., Ezekiel, C., Sulyok, M., Shephard, G. & Krska, R. Mycotoxin contamination of foods in Southern Africa: A 10-year review (2007–2016). Crit. Rev. Food Sci. Nutr. 59, 43–58 (2019).
Nicholaus, C., Martin, H., Matemu, A., Kimiywe, J. & Kassim, N. Risks of aflatoxin exposure among adolescents in boarding schools in Kilimanjaro region, Tanzania. World Mycotoxin J. 14, 221–235 (2021).
Florkowski, W. J. & Kolavalli, S. Aflatoxin control strategies in the groundnut value chain in Ghana. IFPRI Ghana Strategy Support Program Working Paper 33 (2013).
Gichohi-Wainaina, W. N., Kumwenda, N., Zulu, R., Munthali, J. & Okori, P. Aflatoxin contamination: Knowledge disparities among agriculture extension officers, frontline health workers and small holder farming households in Malawi. Food Control 121, 107672 (2021).
Ilesanmi, F. & Ilesanmi, O. Knowledge of aflatoxin contamination in groundnut and the risk of its ingestion among health workers in Ibadan, Nigeria. Asian Pac. J. Trop. Biomed. 1, 493–495 (2011).
Achaglinkame, M. A., Opoku, N. & Amagloh, F. K. Aflatoxin contamination in cereals and legumes to reconsider usage as complementary food ingredients for Ghanaian infants: A review. J. Nutr. Intermed. Metab. 10, 1–7 (2017).
Nakavuma, J. L. et al. Awareness of mycotoxins and occurrence of aflatoxins in poultry feeds and feed ingredients in selected regions of Uganda. Int. J. Food Contam. 7, 1–10 (2020).
Kortei, N. K., Asiedu, P., Annan, T., Deku, J. G. & Boakye, A. A. Fungal diversity of “solom” a Ghanaian traditional beverage of millet (Pennisetum glaucum). Food Sci. Nutr. https://doi.org/10.1002/fsn3.2045 (2020).
Eric, O.-O. & Gyapong, A.-Y. The contribution of the ghana schools feeding programme to basic school participation: A study of selected schools in the Kwaebibirim district of Ghana. Dev. Ctry. Stud. 4, 40–50 (2014).
Afoakwa, E. O. & Chiwona-Karltun, L. Building Sustainable Agricultural Development through Home-Grown School Feeding-The African Approach (2008).
Drake, L., Woolnough, A., Bundy, D. & Burbano, C. Global School Feeding Sourcebook: Lessons from 14 Countries (World scientific, 2016).
Atta, G. P. & Manu, J. Ghana school feeding program: A retrospective review. Int. J. Innov. Res. Dev. 4, 402–410 (2015).
Acknowledgements
We acknowledge and sincerely extend our heartfelt appreciation to Mr. Philemon Yaw Atsugah formerly of the Department of Food Science and Technology, Ho Technical University for his enormous effort in the data collection process. A big thank you also goes to all the respondents who participated in this research for their immense contribution. Lastly, to the staff of the Department of Nutrition and Dietetics, University of Health and Allied Sciences for their support.
Author information
Authors and Affiliations
Contributions
N.K.K., G.T.O., S.B., S.N., and. M.W.-K. performed the experiments and wrote the manuscript. S.N., N.K.K., G.T.O. were responsible for statistical analysis. G.T.O., N.K.K., M.W.-K. and D.N.K.A. helped conceive the experiments and prepared the manuscript. N.K.K., S.B., S.N., M.W-K. and G.T.O. conceived the original study and N.K.K., G.T.O., S.N. and D.N.K.A. led the sampling and study in Ghana. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kortei, N.K., Badzi, S., Nanga, S. et al. Survey of knowledge, and attitudes to storage practices preempting the occurrence of filamentous fungi and mycotoxins in some Ghanaian staple foods and processed products. Sci Rep 13, 8710 (2023). https://doi.org/10.1038/s41598-023-35275-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35275-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.