Abstract
Blood pressure (BP) control is a global health issue with an increase in BP beyond the normal BP leading to different stages of hypertension in humans and hence the need to identify risk factors of BP for efficient and effective control. Multiple BP measurement have proven to provide BP readings close to the true BP status of the individual. In this study, we used multiple BP measurement data on 3809 Ghanaians to determine risk factors associated with BP. The data were obtained from World Health Organization study on Global AGEing and Adult Health. We defined high blood pressure (HBP) as \(\ge\) 130/80 mmHg or normal as \(\le\) 130/80 mmHg. We provide summary statistics and also used the Chi-Square test to assess significance of association between HBP versus risk factors of HBP. The aim of this study is to identify risk factors of BP using the mixed effects logistic regression model. Data were analyzed using R version 4.2.2. The results showed that the risk of high blood pressure (HBP) decreases across the three measurement periods. There is reduced risk (OR = 0.274, 95% CI = 0.2008, 0.405) of HBP among male participants relative to female participants. The risk (OR = 2.771, 95% CI = 1.8658, 4.1145) of HBP increased by 2.771-folds among those who are 60 years and above relative to those below the age of 60 years. Those whose work involves/requires vigorous exercise has 1.631-fold increase in the risk (OR = 1.631, 95% CI = 1.1151, 2.3854) of HBP relative to those whose work does not involve vigorous exercise. There is approximately 5-folds increased in the risk (OR = 4.896, 95% CI = 1.9535, 12.2268) of among those who have ever been diagnosed with diabetes. The results also revealed high risk (OR = 1.649, 95%CI = 1.1108, 2.4486) of HBP among those who have formal education. The risk (OR = 1.009, 95% CI = 1.0044, 1.0137) of HBP increases with increasing weight and a reduced risk (OR = 0.996, 95% CI = 0.9921, 0.9993) of HBP with increasing height. We found that sad experience, either mild, moderate or severe, is associated with a reduced risk of HBP. Those who have vegetable servings at least 2 cups per day have increased risk of HBP and those who have fruits servings at least 2 cups per day is associated with a reduced risk of HBP, however this is not statistically significant. To achieve success in BP control, programs should be designed with the aim of reducing weight, educate those with formal eduction on issues relating to HBP. Those whose work requires vigorous exercise are recommended to have regular check-ups to ensure that pressure build-up in the lungs is cleared. SBP is lower for women at young age but continue to increase after menopause as their BP increase becomes salt-sensitive. Hence there is need to give more attention to menopausal women so as to improve BP. Both young and old individuals are recommended to practice regular exercise since this has shown to reduce risk of being overweight or becoming diabetic and reduces the risk of HBP at yong age and old age. Also, to improve blood pressure control, programs for management of blood pressure or hypertension should focus more short stature individuals since such people are more likely to experience HBP.
Similar content being viewed by others
Introduction
High Blood pressure is a global health problem, especially for developing countries1,2. Hypertension, which is associated with high BP (HBP) has become an increasingly common public health problem. Hypertension is known to be the most common cause of death globally3,4,5. The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of HBP (JNC7) defined hypertension as a SBP \(\ge\)140 mmHg and DBP \(\ge 90\) mmHg6. Other reports/guidelines also accept these value as a tool for hypertension diagnosis6,7,8. Hypertension arises when the blood pushing against the walls of arteries in the body creates pressure higher than the normal BP9,10. The SBP and DBP are often used to measure BP. The SBP is the pressure in the arteries when the heart beats, whereas the DBP is the pressure in the arteries when the heart rests. For normal BP, the SBP is less than 120 millimetres of mercury (mmHg), and the DBP is less than 80 mmHg, often described/written as 120/80 mmHg. Every country has an adopted definition for high blood pressure which is more often guided by the WHO criteria. Some guidelines suggest that HBP should be defined as BP which is consistently higher than 130/80 mmHg, while WHO guidelines suggest higher than 140/90 mmHg9,10,11. Elevated SBP is a leading global health risk12,13. Various studies12,13,14,15 have shown that SBP of at least 110 mmHg is associated with multiple cardiovascular and renal outcomes, including ischemic heart disease, cerebrovascular disease, and chronic kidney disease. Global obesity epidemic is likely to increase SBP among certain group of people3,12,13.
The global policy agenda aimed at controlling BP remains a challenge, and BP-related hypertension is the leading cause of cardiovascular disease (CVD) worldwide16. In Africa, the prevalence of hypertension is the highest relative to rest of the world with 27% of adults having hypertension16. Hypertension is a major public health issue in Sub-Saharan Africa17 where it is estimated that about 10-20 million people are living with hypertension18. The 2014 Ghana Health Service report indicates that high number of out-patient cases is attributed to hypertension. There is consistent increase in hypertension prevalence in Ghana19. Studies have shown that BP-related hypertension is one of the leading cause of admission and mortality in Ghana19,20,21. In 2017, hypertension accounted for 4.7% of the total admissions and 15.3% of total deaths in Ghana21. Hypertension is the leading cause of medical emergencies such as heart22 and renal23 failures and it is the key risk factor of stroke in Ghana. The incidence of stroke among people who are above 60 years increases with increasing level of BP24. Also, the Ghanaian Society of Cardiology (GSC), the Stroke Association Support Network-Ghana (SASNET-Ghana) in partnership with the World Heart Federation, reported that an estimated 34% of the population between the ages of 30 and 70 years has hypertension or high blood pressure. These bodies revealed that this percentage is slightly more than half of the estimated number of people living with hypertension25.
Literature on BP revealed that the burden of SBP still remains high even though there are preventive interventions and anti-hypertensive medications that are effective and low-cost12,13. The paradigm of determining high BP or hypertension has shifted towards SBP26. For instance Lloyd-Jones and colleagues27 revealed that SBP is more likely to correctly classify subjects as having high BP or hypertension relative to diastolic BP. The article by Pogue et al.28, published in 1996, also noted that it is SBP, not the DBP, that is the key determinant of appropriate classification of middle-aged and older persons as well as those undergoing treatment as having high BP or hypertension. Using the data from the Framingham Heart Study cohort, Kannel et al.29 found in 1971 that SBP is an appropriate determinant of outcomes such as high BP, hypertension and cardiovascular diseases. Several other studies confirmed this finding including that of Ali and colleagues30. It took 22 years for SBP to be recognized as even equally important to DBP in classifying individuals as having high BP or hypertensive26,27. Lloyd-Jones et al.27 pointed out the importance of SBP measurement and Fisher31 even suggested that we should ignore DBP measurement. But for the fact that pulse rate is a better predictor of events than SBP, especially in older persons32,33,34 and we cannot compute pulse rate without DBP measurement, we still need to measure DBP. There is no need emphasizing on the clinical relevance of SBP over DBP35; elevated SBP predicts the risk of cardiovascular disease better than DBP36.
Studies have shown that although SBP measurements are more variable, it is easier to be measured and also serve as an appropriate tool for correct risk classification than DBP. BP is associated with age36. Among people aged 50, hypertension is associated with risk of coronary heart disease, left ventricular hypertrophy, congestive heart failure, renal failure, and mortality than DBP36. Basile36 revealed that a stiffened arterial tree, given the same stroke volume and ejection rate, will produce a higher SBP, a lower diastolic BP (DBP) and a wider pulse pressure (PP), but the mean BP (MBP) will be unchanged, emphasizing on the importance of SBP as a determinant of cardiovascular event/outcome. Imai and colleagues37 examined risk factors of BP using community-based sample in northeastern Japan. They found that age, heart rate, and pulse rate are associated with BP. Several other studies have evaluated the effect of various factors on HBP or hypertension38,39. These authors examined factors such as geographical location or country of origin, gender and age.
Wang et al. (pp. 1555–1562) study on influences of obesity on BP in China shows that measurement such as visceral fat index (VFI) or the VFI to percentage body fat ratio (VFI/PBF) is likely to provide better understanding of adiposity-related risks for hypertension40,41. Meta-analysis of a randomized control trial of potassium supplementation revealed that a significant reduction in BP is associated with potassium supplementation among trial subjects who are not on any anti-hypertensive medication40,41,42. Laine et al.43 published work on relationship between exercise and hypertension showed that vigorous physical activity during young adulthood is associated with lower age-adjusted prevalence of hypertension compared to those who did not. Stress is also another factor found to be associated with BP elevation in both gender and elevated night-time BP among men44. Other factors associated with BP are foetal growth restriction or prematurity, organ damage, cardiovascular risk predictor45, N-terminal proB-type natriuretic peptide (NT-proBNP), where association of BP variability with NT-proBNP levels may give an indication that blood pressure variability is associated with organ damage or complications46.
Various authors have studied systolic BP and associated factors using different methods. Alexander et al.47 used the Multivariable Cox survival model to determine the effect of the burden of systolic and diastolic hypertension on a composite outcome of myocardial infarction, ischemic stroke, or hemorrhagic stroke over a period of 8 years. Their study also adjusted for the effects of demographic characteristics and coexisting conditions. In order to evaluate the association between SBP and the burden of different causes of death and disability by age and sex, Forouzanfar et al.12,13 used Spatiotemporal Gaussian process regression to produce mean SBP and adjusted variance for each age, sex, country, and year. Their results revealed that SBP-related deaths is associated with ischemic heart disease, hemorrhagic stroke, and ischemic stroke. In Ghana there is evidence of hypertension control benefits, however, the control rates are low16. Okai and colleagues16 assessed the associations between patient background characteristics and hypertension control using Chi-Square tests and studied the relationship between these characteristics and hypertension control using logistic regression. On the other hand, Tannor et al.18 used simple and multiple logistic regression determine the risk factors of hypertension in Ghana.
Taking multiple SBP/DSP measurements has proven to provide BP reading close to the true BP status of the individual48,49,50. This paper considered analysis of BP measurements taken repeatedly on the same subject within 3 minutes between each measurement, but at the same visit, using the mixed effects logistic regression model51,52,53. Taking multiple measurements provides more information and hence improves precision of estimates for appropriate policy formulations towards blood pressure control. The key hypothesis that drives this study is that high blood pressure is associated with some of the exposure variables in this study.
Methods
In this section, we give a brief description of the data. We also discuss the outcome variable in this study as well measurement scales of risk factors used. We then discuss the methods for modeling the outcome variable. Here, we will discuss the structure of the BP variable. This provides a framework for building a model that establishes the relationship between the outcome variable and the various risk factors. Our model formulation is based on the logistic mixed effects model54 and we will assess the effect of gender on BP over the three BP measurements adjusting for other risk factors of BP in Ghana.
Data and variables
The data used in this study were obtained from World Health Organization (WHO) study on Global AGEing and Adult Health (SAGE). The data collection was completed in 2014/15 and data were released in the public domain in 202055. The data used in this analysis consist of several variables including systolic and diastolic BP data on 3,809 Ghanaians in 2015.
Outcome variable
The outcome variable used in this study is BP. The BP measurements are categorized as high BP (\(\ge\) 130/80 mmHg) or normal BP (\(\le\) 130/80 mmHg). The BP variable takes a value of 1 if BP measurement is (\(\ge\) 130/80 mmHg) or 0 if BP measurement is (\(\le\) 130/80 mmHg). Both SBP and DBP data were collected 3 times on the same subject with one minute between each measurement for both males and females.
Risk factors
This study considers several risk factors of BP. However, detailed discussion and conclusions would be based on only the significant risk factors from the best fitting model. We considered continuous risk factors as weight in kg and height cm. The categorical variable considered are age (takes value of 1 if age is 60 years and above and 0 if age is less than 60 years), gender (takes value of 1 if male or 0 if female), marital status (takes the value of 0 if never married, 1 if currently married, 2 if cohabiting, 3 if divorced, or 4 if widowed), ever been to school (1 if yes or 0 if no), ever feel sad (0 if no, 1 if mild, 2 if moderate, 3 if severe or 4 if extreme), ever feel worried (0 if no, 1 if mild, 2 if moderate, 3 if severe or 4 if extreme), ever smoked tobacco (1 if yes or 0 if no), ever consumed alcohol (1 if yes or 0 if no), work involves vigorous exercise (1 if yes or 0 if no), ever diagnosed with arthritis (1 if yes or 0 if no), ever diagnosed with angina (1 if yes or 0 if no), ever diagnosed with diabetes (1 if ye or 0 if no), ever diagnosed with asthma (1 if yes or 0 if no), fruits servings (1 if fruits servings is at leas 2 cups per day or 0 if fruits servings is less than 2 cup served per day). Descriptive statistics of these variables including the outcome variable are shown in The Table 1, 2.
Logistic mixed effects model
Since the outcome variable consist of binary repeated records on the status of BP, the logistic mixed effects model (LMM)56 is assumed for the BP status variable. This is because the LMM is used to model repeated measurements on the same subject by adding a subject-specific random effect to the model. This random effect captures all the unobserved subject-specific characteristics. The logistic mixed effects regression model is used to model binary outcome variables where the log odds of the outcomes are modeled as a linear combination of the risk factors when there are both fixed and random effects.
Let \({\textbf{Y}}_{i} = \left( Y_{i1}, Y_{i2}, \ldots , Y_{in} \right)\) denotes an N-dimensional vector of BP status (1 or 0) for the \(i{\text {th}}\) subject. We note that the response \({Y}_{ij}\) is recorded for each subject \(i, i = 1, \ldots , N\) at time \(j, j = 1, \ldots , n\). In this study, all measurements were observed, there is no missing values57,58,59. The interest is how the status of the response is affected by the \({\textbf{X}}_{i}\), an \(N \times p\) design matrix of risk factor for the \(i^{\text {th}}\) subject. The general form of the LMM can be written as57,58,59
where \(\pmb {\beta }\) is a \(p \times 1\) vector of the fixed effects; which represents the effects of the risk factors on the BP, \(\pi _{ij}\) is the probability of having HBP, \({\textbf{Z}}_{i}\) is a \(N \times q\) design matrix for the q random effects, \({\textbf{b}}_{i}\) are patient-specific random effect and is assumed to follow the normal distributions such that \({\textbf{b}}_{i} \sim N \left( \pmb {0}, \sigma ^2_{b}\right)\).
From model (1), our potential logistic mixed model to be fitted can be written as
where \(\text {b}_{0i}\) represents the patient-specific random effect. It is assumed that \(\text {b}_{0i}\) are independently distributed as \(\text {b}_{0i} \sim N\left( 0,\sigma ^2_{b0}\right)\). Note that the variable for gender is Gender, Marital status is Married, ever been to school is School, ever feel sad is Sad, ever feel worried is Worried, ever smoke tobacco is Tobacco, ever consume alcohol is Alcohol, work involves vigorous exercise is Exe, ever diagnosed with arthritis is Arthritis, ever diagnosed with angina is Angina, ever diagnosed with diabetes is Diabetes, ever diagnosed with asthma Asthma, ever diagnosed with hypertension is Hypertension, age category is Age, height in cm is Height, weight in kg is Weight, fruits servings per day is Fruit, vegetables servings per day is Veg and time is Time.
Analysis and results
In this section, we first present descriptive statistics of the variables in the data and then performed bivariate analysis on BP and each of the categorical risk factors using the Chi-Square test60,61,62 of association and the continuous risk factors using the t-test63,64,65,66. The purpose of this exercise is to identify potential risk factors of BP. Significant risk factors under these analyses were then used in the logistic mixed effects model to determine their individual contributions to BP after adjusting for other risk factors. Also, in the logistic mixed effects model, variables that were found to be statistically insignificant after adjusting for other risk factors were removed from the model. Statistical analyses in this paper were performed using R version 4.2.2.67. Logistic mixed effects models52,53,68,69,70 were fitted using the glmer function and performance of the fitted models compared and best model selected using the Akaike’s information criterion (AIC)71,72,73,74,75 and Bayesian information criterion (BIC)75,76,77,78.
Descriptive statistics
Table 1, 2 shows that out of the total number of 3809 Ghanaians enrolled into the study, 1976 (51.88%) are males and 1833 (48.12) are females. Out of the 3809, 2080 (54.60%) have high blood pressure and 1729 (45.40%) have normal blood pressure (NBP). High proportion, 2102 (55.19%), of the study participants are currently married. The proportion 1666 (43.74%) of those who have never been to school lower than the proportion, 2143 (56.26%), of those who have ever been to school. The proportion, 1791 (47.02%) of the study participants who never feel sad is higher than those whose sadness levels can be described as mild followed by moderate, severe, and extreme. The proportion, 1532 (40.22%) of the study participants who never feel worried is high relative to those who extremely feel worried followed by those whose feeling is described as mild, moderate and severe. We observed that small proportion, 987 (25.94%), of the study subjects ever smokes tobacco compared with a proportion 2818 (74.06%) never smoke tobacco. Majority, 2210 (58.08%), of the study subjects ever consume alcohol and high proportion, 2146 (56.40%), of the study participants’ work does not involve vigorous exercise.
Only 524 (13.77%) of the subjects have ever been diagnosed with arthritis and few, 128 (3.36%) of participants has ever been diagnosed with angina. The proportions of those who have ever been diagnosed with diabetes and asthma are 154 (4.02%) and 144 (3.78%) respectively. We observed that 519 (13.64%) of the study subjects have ever been diagnosed with hypertension. Majority, 2243 (58.89%), of the study participants are at least 60 years old with those less than 60 years old representing 1566 (41.11%). The statistics also showed that high proportion, 2849 (74.80%), of the study participants have vegetables servings at least 2 cups per day. Those who have fruits serving at least 2 cups per day is lower, 1329 (34.89%), then those who have less than 2 cups per day. The average height of the study participants is approximately 165 cm and mean weight of 165 kg.
Bivariate analysis of BP versus risk factors
We carried out bivariate analysis between the BP as a binary response variable versus categorical and continuous risk factors of BP. For the categorical risk factors, we used the Chi-Square test of association to test for significance of association between the two variables (binary response versus categorical risk factors). For the continuous risk factors, we used the t-test to test for significant difference in the means of the continuous risk factors between the two groups (high blood pressure and normal blood pressure). The categorical and continuous risk factors are shown in Tables 1, 2. The Chi-Square and t-test results in Table 3 presents only risk factors that are significantly associated with the response variable (blood pressure). These significant variables are then considered in our subsequent analysis using the logistic mixed effects model (1).
Logistic mixed effects model
Based on the significant risk factors (in Tables 1, 2), our logistic mixed effects model to be fitted can be written as
Only risk factors in the best fitting model will be discussed in detailed in the discussion and conclusion Sect. “Outcome variable”. To select the best fitting model for the BP variable, we performed step-wise variable selection procedure79,80,81.
Our best fitting model from the variable selection procedure is specified in Model (4) and the results are presented in Table 4.
where Exe is vigorous exercise, Veg is vegetables servings, and Mild, Moderate, and Server represent those who describe their sadness level as mild, moderate and severe respectively.
The results in Table 4 showed that the risk (OR = 0.631, 95% CI = 0.5814, 0.6843) of high blood pressure (HBP) decreases across the three measurement periods. There is significant reduction in the risk (OR = 0.2740, 95% CI = 0.1847, 0.4058) of HBP among male participants relative to female participants. We found that those who have ever felt sad (mild, moderate or severe) have reduced risk of HBP compared with those who have never felt sad. There is approximately 2-folds increase in the risk (OR = 1.649, 95% CI = 1.1108, 2.4486) of HBP among those who have formal education relative to those who has no formal eduction. The study results revealed that there is 2.77-folds increase in the risk (OR = 2.771, 95% CI = 1.8658, 4.1145) of HBP among those who are 60 years and above relative to those below the age of 60 years. The results also revealed that those who have vegetable servings at least 2 cup per day have increase risk of HBP. We observed that those whose work involves/requires vigorous exercise has 1.631-folds increase in the risk (OR = 1.631, 95% CI = 1.1151, 2.3854) of HBP relative to those whose work does not involve vigorous exercise. The risk of HBP increases with increasing weight. However, a reduced risk of HBP is associated with increasing height. Diabetes was found to be positively associated with an increase risk of high blood pressured.
Discussion and conclusions
In this paper, we investigated the effects of variables as potential risk factors of BP. We provided summary of statistics of the variables used and then performed Chi-Square test of association to predetermine variables that may be identified as potential risk factors for inclusion in the subsequent analysis. In this study, we modeled the BP data using the mixed effects logistic regression model56.
Our study results revealed that SBP significantly decreases across the three measurement times. This finding suggests that there is some level of variability associated with measuring BP, even in the same subject, and hence using a single value as a measure of BP may produce BP values that are not actual representation of one’s BP level. This finding agrees with findings of various authors48,49,50 that SBP measurements within one minute between measurements is associated with decreasing SBP. Repeatedly measuring SBP provides a means of validating the accuracy of the SBP as well as the appropriate SBP of a given subject. That is studies should be design to repeatedly measure SBP on the same subject to aid in making decision on the actual BP of the subject. This finding agrees with the standard practice of using multiple SBP values to determine the SBP actual value of an individual.
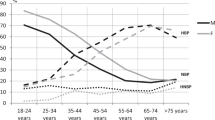
Higher SBP is observed among females subjects compared to their male counterparts. This finding is contrary to the finding by Hussein and colleagues82,83 where SBP was found to be significantly higher in males relative to females. This is often the case when studies participants are younger age group. In Hussein and colleagues82 paper, ages of participants range from 18 to 26 years. In this study, ages of the study participants range from 51 to 114 years and 2199 (58.67%) of the participants are more than 50 years. Systolic BP is lower in female during early adulthood and the reverse is true for 50 years and above83,84. High BP related hypertension is associated with increasing age and is higher among men at younger age and higher among women at older age. The gender difference in BP control is largely determined by sex hormones in females which shows to be protective against high BP83,84. However, BP to increase among menopausal women since BP becomes salt-sensitive after menopause83,84. The implication of this finding is that females are at high risk of higher SBP at old age relative to young age. This calls for blood pressure control programs to pay special attention to both gender groups in relation to their respective age categories in which their are noted to be relatively more susceptible to high SBP. Specifically, blood pressure control programs should focus more on women at menopause since women are highly susceptible to high SBP at this stage of their life.
This study results also revealed that high BP is associated with the older age. This finding is in line with findings from various studies82,83,85,86. From pathophysiology perspective, high BP with increasing age is mostly related to changes in arterial and arteriolar stiffness87. That is, large artery stiffness is often caused by arteriosclerotic structural alterations and calcification, which the leads to earlier reflected pressure waves from the arterioles towards the heart during BP wave propagation87. Various studies88,89,90 showed that high BP related hypertension is associated with increasing age, where BP is lower among women at younger age and high among women at older age. The chance of having high blood pressure BP increases as you get older, especially isolated systolic hypertension. Before the age of 55 years, men are more likely to experience high BP pressure. However, after the age of 55 years, women are more likely to experience high BP. Blood pressure increase with increasing age is a major risk factor for cardiovascular and renal disease, stroke, and type 2 diabetes mellitus89,90 and age-related increases in blood pressure have been observed in almost every population. The China Peace Collaborative Group91 revealed that high blood pressure is associated with increasing age and that the risk of high BP almost 3-folds across subgroups, indicating subgroup differences in biology, behaviour, or exposures. These authors noted that anti-hypertension strongly reduces the association between age and blood pressure as well as diminishes the variation91. However, there some exposure groups where age and blood pressure association is negative. That is, among certain group of individuals, BP may decrease with increasing age and mostly occur among people suffering from illness such as Alzheimer’s and other forms of dementia, cancer or impaired ventricular function which may occur after myocardial infarction87. Michael and colleagues89,90 noted that increase in BP is observed in almost every population except hunter-gatherers, farmers, and pastoralists.
We found an increased risk of high BP with increasing weight. Our finding agrees other studies82,83,85,86,92 in the literature. These studies revealed that overweight subjects have more body fat which increases the BP than that of the normal weight subjects. Identifying factors responsible for changes in BP levels became an important topic upon which an initial group of articles focused on40,41,93. In both children and adults, the association between obesity and hypertension is well established. However, the pathogenesis of obesity induced hypertension is an active area of research93. Although it is well established that increase in the risk of hypertension is associated with obesity, it is also known that many obese individuals do not develop hypertension40,41. Studying the influence of interaction between air pollution and obesity on blood pressure in Chinese children in China94 shows that obesity increases the association of long-term air pollution with blood pressure and hypertension in Chinese. Also, investigating the influence of obesity on BP in a large population study in China by Wang and colleagues40,41,95 in children showed measurements of the visceral fat index (VFI) or of the VFI to percentage body fat ratio (VFI/PBF) may offer a better understanding of adiposity-related risks for hypertension and pre-hypertension. Body mass index (BMI) is stronger predictor of BP96. Common conclusions or recommendations among researcher is that reducing or eliminating overweight and obesity has the potential which could lead to a reduction in the risk of high BP97 and Bin and colleagues98 noted that eliminating overweight and obesity could reduce 14.4% of high BP cases among Chinese children. Even in children (both boys and girls), the prevalence of high BP is high and overweight and obese children had a significantly higher prevalence of high BP than non-overweight children98. There is therefore the need for primary prevention of hypertension among children and preventive measures should focus on weight control and healthy lifestyle habits. The policy implication is that BP control programs should focus on promoting weight reduction programs such as daily exercise, taking supplements/medications that burn fat, and healthy life style.
Our study results showed that there is a reduced risk of HBP among those whose work does not involve vigorous exercise compared with those whose work involves vigorous exercise. One would have expect that exercise should always decrease BP. However, BP increase or reduction is largely dependent on the degree, frequency, and duration of the exercise. A study conducted on Korean adults who self-reported that they practice regular exercise revealed that there slower rate of progression to hypertension relative to those who do not exercise99,100. Kim and colleagues99 study revealed that study participants whose level of physical activity is low are exposed to higher risk hypertension when compared with individuals whose physical activity level is moderate100,101. Progression to hypertension is associated with an increased risk of high BP among those whose work requires vigorous exercise. Faselis and colleagues102 studied male veterans in the United State of America found that there was high risk of progression to hypertension with associated decrease in cardiorespiratory fitness. Also, vigorous physical activity during young adulthood is protective against hypertension in the future. Reports on former elite athletes versus controls (those who are not former athletes) showed lower age-adjusted risk of hypertension among former elite athletes relative to the controls103. These authors noted that lower prevalence of hypertension is not only associated with such athletes in the future, but also the current volume of leisure-time physical activity is inversely related to the presence of hypertension103. For the purpose of reducing BP, individuals are recommended to engage in moderate exercise104. Various hypertension guidelines105,106 recommended aerobic exercise such as jogging, walking, and swimming for management of high BP related hypertension. Some of the guidelines include the Canada’s 2018 hypertension guidelines107, the Japanese Society of Hypertension Guidelines for the Management of Hypertension108, and 2010 Chinese guidelines for the management of hypertension109. WHO guidelines on management of hypertension recommend regular aerobic exercise for more than 30 min every day110. There is therefore the need for blood pressure control authorities to intensify campaign on need for daily exercise during young age and old age.
We found that BP is high among those who have vegetable servings at least 2 cups per day. Also, normal blood pressure is associated with those who say they have ever felt sad (mild, moderate or severe) relative to those who never felt sad. These findings suggest that using ever felt sad as a measure BP status may not be appropriate since BP level may return to normal after spike in sadness (depression or anxiety). Studies have also shown that there is no justification that anxiety and depression are directly linked to high blood pressure. This means that being sad can cause a steep rise in blood pressure. However, the blood pressure returns to its original level after the sadness. One’s feeling (anxiety or depressed) should not be used as a measure of BP status since these conditions can be sudden and may not last long with bloop pressure returning to normalcy.
The results revealed that a reduced risk of HBP is associated with increasing height; a finding which agrees with various studies in the literature111. A study by Stanaway and colleagues112 have shown that height is positively associated with hypertension. The problem with this finding is that the results was difficult to interpret. This is because the body size, which was adjusted for during the analyses, was correlated with adult height. The implication is that the body size/weight could be a mediator instead of confounder in the association between height and BP113. Subsequent to this finding, Bourgeois and colleagues113 found a negative association between height and SBP and pulse pressure as well as positive association between height and DBP. Various studies studies have established that there is an inverse relationship between height and BP114,115 and Das Gupta and colleagues found that for each 10cm increase in height, the odds of hypertension decreases 10% in adult Nepalese population116. Several factors account for this inverse association between height and BP/Hypertension111. For instance, an increases in height leads to a corresponding increase in the diameter of the coronary vessels111. These anatomical factors reduces the risk of atherosclerosis and hypertension111,117. Importantly, there proper lung function among taller individuals compared with short stature people and this may be responsible for the inverse relationship between height and hypertension118,119,120. Although, the mechanism explaining the relationship between height and BP/hypertension is unclear, hypertension management should centered among short individuals.
We found that there is approximately 5-fold increase in the risk of HBP among subjects who ever been diagnosed with diabetes. Our finding is in line with various studies121 that diabetes is a significant predictor of hypertension. Other studies122,123 have found that hypertension is twice as frequent in patients with diabetes compared with those who do not have diabetes. Hypertension and diabetes share common risk factors and often occur together. High blood pressure (BP) was reported as a significant predictor of type 2 diabetes124. It has been established that subjects with HBP have approximately 60% increased risk of developing type 2 diabetes. Various studies have identified hypertension as an independent risk factor for cardiovascular events. However, the relationship between blood pressure and the risk of new onset diabetes is remains unclear125.
Also, our results revealed that there is an increase risk of HBP among subjects with formal education background relative to those without formal education. Our finding is contrary to almost all the recent studies on impact of education on blood pressure and hypertension. Years of schooling was found have negative relationship with systolic blood pressure after adjusting for age, gender and race126. Even further adjustment for mother’s education, childhood verbal intelligence quotient, childhood health and childhood socioeconomic status was found to have little influence this conclusion. However, years of schooling became statistically insignificant (but positive association with BP) after adjusting for degree attained in the fully model126. Comparison of graduates versus high school degree-holders showed that graduate degree still had significantly lower systolic blood pressure than high school degree-holders126. As study that was designed to evaluate the impact of education on cardiovascular risk control and target BP values in hypertensive outpatients found no correlation between education intensity and the achieved BP reduction127. Other studies128 have revealed that less educated hypertensive were characterized by a significantly higher prevalence of patients with greater global cardiovascular risk rather than medium-high educated hypertensive subjects. Studies have reveled that hypertension is a prevalent condition among the least educated and poorest people in low-and middle-income countries128,129.
Contributions of the study; firstly, when the objective of a study is to collect data repeatedly, on the response variable, for each study participant within a specified time interval(s) or at some selected time points, then any method of analysis that assumes that such measurements in the response variable are independent is likely to produce invalid statistical inferences54,57,58,59. This means that the linear regression model that assumes that the responses are independent cannot be used to provide valid statistical inferences. In this study, we used the logistic mixed effects model54 to account for correlation between the repeated measurements in the BP data. The logistic mixed effects model achieves this by introducing a subject-specific random effect, which captures all unobserved subject-specific characteristics69,70. Secondly, this study used repeated binary BP data on 3809 Ghanaians to study the BP changes (high or low blood pressure) across the measurement periods as well determine risk factors associated with BP. In this way, one would be able to determine whether there is variability associated with BP measurements at the different periods. The study revealed that there is variability among the BP status across the measurement periods, an indication that using multiple measurements to evaluate true BP is a recommended practice and should be encourages. However, this study is unable to consider more than 3 repeated measurements to check if mean BP values would decrease or remain horizontal after some number of repeated measurements. So this study is unable to determine the number measurements required to estimate the true systolic blood pressure value in a subject under study.
Data availability
Supporting data for this manuscript results are available at [https://www.who.int/data/data-collection-tools/study-on-global-ageing-and-adult-health/sage-waves] upon request from “@World Health Organization (WHO) study on Global AGEing and Adult Health (SAGE)”. The authors have no right to release the data to a third party.
References
Mittal, Bharati V. & Singh, Ajay K. Hypertension in the developing world. Challenges and opportunities. Am. J. Kidney Dis. 55, 590–598 (2010).
Chow, Clara K. & Gupta, Rajeev. Blood pressure control: A challenge to global health systems. Lancet 394, 613–615 (2019).
Kearney, P. M., Whelton, M., Reynolds, K., Whelton, P. K. & He, J. Worldwide prevalence of hypertension: A systematic review. J. Hypertens. LWW 22(1), 11–19 (2004).
Murray, C. J. L. & Lopez, A. D. Mortality by cause for eight regions of the world: Global burden of disease study. Lancet 349(9061), 1269–1276 (1997).
Göktaş, O.,Şentürk, T., Ersoy, C. Factors affecting hypertension in the adult population of the Marmara region, Turkey: A descriptive field study. Int. J. Hypertens. (2020).
Chobanian, A. V. et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure, hypertension. Am. Heart Assoc. 42(6), 1206–1252 (2003).
Williams, B. et al. ESC scientific document group, 2018 ESC/esh guidelines for the management of arterial hypertension, evaluation, and treatment of high blood pressure. Eur. Heart J. 39(33), 3021–3104 (2018).
Reboussin, D. M. et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension 71(6), e116–e135 (2018).
Desai, A. N. High Blood Pressure. J. Am. Med. Assoc. 324(12), 1254–1255 (2020).
Desai, A. N. High blood pressure. Am. Med. Assoc. 324, 1254–1255 (2020).
Plumettaz, C., Viswanathan, B. & Bovet, P. Hypertension prevalence based on blood pressure measurements on two vs. one visits: A community-based screening programme and a narrative review. Int. J. Environ. Res. Public Health 17, 9395 (2020).
Forouzanfar, M. H. et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. Am. Med. Assoc. 3172, 165–182 (2017).
Forouzanfar, M. H. et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. J. Am. Med. Assoc. 317, 165–182 (2017).
Collins, R. et al. Blood pressure, stroke, and coronary heart disease: Part 2, short-term reductions in blood pressure: Overview of randomised drug trials in their epidemiological context. Lancet 335(8693), 827–838 (1990).
Wright, J. T. Jr. et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. J. Am. Med. Assoc. 288(19), 2421–2431 (2002).
Okai, D. E. et al. Patient-level factors influencing hypertension control in adults in Accra, Ghana. BMC Cardiovasc. Disord. 20(1), 1–7 (2020).
Tannor, E. K. et al. Prevalence of hypertension in Ghana: Analysis of an awareness and screening campaign in 2019. Clin. Med. Insights Cardiol. 16, 11795468221120092 (2022).
Tannor, E. K. et al. Burden of hypertension in Ghana-Analysis of awareness and screening campaign in the Ashanti Region of Ghana. JRSM Cardiovasc. Dis. 11, 20480040221075520 (2022).
Bosu, W. K. & Bosu, D. K. Prevalence, awareness and control of hypertension in Ghana: A systematic review and meta-analysis. PloS One 16, e0248137 (2021).
Ghana Health Service, The health sector in Ghana: facts and figures 2018. Minist Heal Ghana 1–50 (2018).
Nuamah, K. et al. Characteristics of inpatient hypertension cases and factors associated with admission outcomes in Ashanti Region, Ghana: An analytic cross-sectional study. Int. J. Hypertens. Hindawi2017 (2017).
Owusu, I. K. & Adu-Boakye, Y. Prevalence and aetiology of heart failure in patients seen at a teaching hospital in Ghana. J. Cardiovasc. Dis. Diagn 1, 131 (2013).
Plange-Rhule, J. et al. Hypertension and renal failure in Kumasi, Ghana. J. Hum. Hypertens. 13(1), 37–40 (1999).
Sarfo, F. S. et al. Low blood pressure levels & incident stroke risk among elderly Ghanaians with hypertension. J. Neurol. Sci. 413, 116770 (2020).
Ghanaian Society of Cardiology (GSC). Stroke Association Support Network–Ghana (SASNET-Ghana). WHF Roundtables on hypertension in Accra, Ghana, Vol. 16 (2022).
Black, H. R. The paradigm has shifted, to systolic blood pressure. Hypertension 34(3), 386–387 (1999).
Lloyd-Jones, D. M. et al. Differential impact of systolic and diastolic blood pressure level on JNC-VI staging. Hypertension 34(3), 381–385 (1999).
Pogue, V. A., Ellis, C., Michel, J. & Francis, C. K. New staging system of the fifth Joint National Committee report on the detection, evaluation, and treatment of high blood pressure (JNC-V) alters assessment of the severity and treatment of hypertension. Hypertension 28(5), 713–718 (1996).
Kannel, W. B., Gordon, T. & Schwartz, M. J. Systolic versus diastolic blood pressure and risk of coronary heart disease: The Framingham study. Am. J. Cardiol. 27(4), 335–346 (1971).
Alli, C. et al. The long-term prognostic significance of repeated blood pressure measurements in the elderly: SPAA (Studio sulla Pressione Arteriosa nell’Anziano) 10-year follow-up. Arch. Intern. Med. 159(11), 1205–1212 (1999).
Fisher, C. M. The ascendancy of diastolic blood pressure over systolic. Lancet 326, 1349–1350 (1985).
Madhavan, S., Ooi, W. L., Cohen, H. & Alderman, M. H. Relation of pulse pressure and blood pressure reduction to the incidence of myocardial infarction. Hypertension 23(3), 395–401 (1994).
Chae, C. U. et al. Increased pulse pressure and risk of heart failure in the elderly. Am. Med. Assoc. 281(7), 634–643 (1999).
Black, H. R. & Yi, J.-Y. A new classification scheme for hypertension based on relative and absolute risk with implications for treatment and reimbursement. Hypertension 28, 19–724 (1996).
Smulyan, H. & Safar, M. E. Systolic blood pressure revisited. J. Am. Coll. Cardiol. 29(7), 1407–1413 (1997).
Basile, J. N. Systolic blood pressure: It is time to focus on systolic hypertension-especially in older people. BMJ 325, 917–918 (2002).
Imai, Y. et al. Factors that affect blood pressure variability. Am. J. Hypertens. 10(11), 1281–1289 (1997).
Ueshima, H., Zhang, X. H. & Choudhury, S. R. Epidemiology of hypertension in China and Japan. J. Hum. Hypertens. 14(10), 765–769 (2000).
Wolf-Maier, K. et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. J. Am. Med. Assoc. 289(18), 2363–2369 (2003).
Zanchetti, A. Factors influencing blood pressure levels. J. Hypertens. 33(8), 1497–1498 (2015).
Zanchetti, Alberto. Factors influencing blood pressure levels. Hypertension 33, 1497–1498 (2015).
Binia, A., Jaeger, J., Hu, Y., Singh, A. & Zimmermann, D. Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials. J. Hypertens. 33(8), 1509–1520 (2015).
Laine, M. K. et al. A former career as a male elite athlete-does it protect against type 2 diabetes in later life. Diabetologia 57(2), 270–274 (2014).
Schoen, T. et al. Plasma copeptin levels and ambulatory blood pressure characteristics in healthy adults. J. Hypertens. 33, 1571–1579 (2015).
Juonala, M., Viikari, J. S. A. & Raitakari, O. T. Main findings from the prospective cardiovascular risk in young Finns study. Curr. Opin. Lipidol. 24, 57–64 (2013).
Satoh, M. et al. N-terminal pro-B-type natriuretic peptide is not a significant predictor of stroke incidence after 5 years–The Ohasama study. Circ. J. CJ–17 (2018).
Flint, A. C. et al. Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N. Engl. J. Med. 381, 243–251 (2019).
Jose, A. P. et al. Impact of repeated blood pressure measurement on blood pressure categorization in a population-based study from India. J. Hum. Hypertens. 33, 594–601 (2019).
Baron, R. B. Treating Blood Pressure Correctly by Measuring It Correctly. Intern. Med. 178, 860–861 (2018).
Einstadter, D., Bolen, S. D., Misak, J. E., Bar-Shain, D. S. & Cebul, R. D. Association of repeated measurements with blood pressure control in primary care. Intern. Med. 178, 858–860 (2018).
Thomas, R., Have, T., Kunselman, A. R., Pulkstenis, E. P., & Landis, J. R. Mixed effects logistic regression models for longitudinal binary response data with informative drop-out. Biometrics 367–383 (1998).
Ugwu, C. L. J. & Zewotir, T. T. Using mixed effects logistic regression models for complex survey data on malaria rapid diagnostic test results. Malar. J. 17, 1–10 (2018).
Ugwu, C. L. J. & Zewotir, T. T. Using mixed effects logistic regression models for complex survey data on malaria rapid diagnostic test results. Malar. J. 17, 1–10 (2018).
Laird, N. M. & Ware, J. H. Random-effects models for longitudinal data. Biometrics 4, 963–974 (1982).
WHO, Study on Global AGEing and Adult Health (SAGE), https://apps.who.int/healthinfo/systems/surveydata/index.php/catalog/sage/about, May 27 (2022).
Agresti, A. Categorical Data Analysis (Wiley Hoboken, 2012).
Iddrisu, A.-K. & Gumedze, F. Application of sensitivity analysis to incomplete longitudinal CD4 count data. J. Appl. Stat. 46, 754–769 (2019).
Iddrisu, A.-K. & Gumedze, F. An application of a pattern-mixture model with multiple imputation for the analysis of longitudinal trials with protocol deviations. BMC Med. Res. Methodol. 19, 1–23 (2019).
Iddrisu, A.-K. & Gumedze, F. Freedom, sensitivity analysis for the generalized shared-parameter model framework. J. Biopharm. Stat. 30, 197–215 (2020).
McHugh, M. L. The chi-square test of independence. Biochem. Med. 23, 143–149 (2013).
Shen, C., Panda, S. & Vogelstein, J. T. The chi-square test of distance correlation. J. Comput. Graph. Stat. 31, 254–262 (2022).
He, X. et al. The poor prognosis and influencing factors of high D-dimer levels for COVID-19 patients. Sci. Rep. 11, 1830 (2021).
Kim, T. K. T test as a parametric statistic. Korean J. Anesthesiol. 68, 540–546 (2015).
Cressie, N. A. C. & Whitford, H. J. How to use the two sample t-test. Biom. J. 28, 131–148 (1986).
Wright, D. B. Comparing groups in a before-after design: When t test and ANCOVA produce different results. Br. J. Educ. Psychol. 76, 663–675 (2006).
Novak, S. Y. On the T-test. Stat. Prob. Lett. 189, 109562 (2022).
Rizzo, Maria L. Statistical Computing with R (Chapman and Hall/CRC, 2019).
Guo, R., Xin, C., Lin, P. & Kourtellis, A. Mixed effects logistic model to address demographics and neighborhood environment on pedestrian injury severity. Transp. Res. Rec. 2659, 174–181 (2017).
Zhao, Y., Xu, D., Duan, X. & Du, J. A semiparametric Bayesian approach to binomial distribution logistic mixed-effects models for longitudinal data. J. Stat. Comput. Simul. 92, 1438–1456 (2022).
Tapia, A., Leiva, V., Diaz, M. D. P. & Giampaoli, V. Influence diagnostics in mixed effects logistic regression models. Test 28, 920–942 (2019).
Portet, S. A primer on model selection using the Akaike Information Criterion. Infect. Dis. Model. 5, 111–128 (2020).
Arnold, T. W. Uninformative parameters and model selection using Akaike’s Information Criterion. J. Wildl. Manag. 74, 1175–1178 (2010).
Cavanaugh, J. E. & Neath, A. A. The Akaike information criterion: Background, derivation, properties, application, interpretation, and refinements. Wiley Interdiscip. Rev. Comput. Stat. 11, e1460 (2019).
Bozdogan, H. Model selection and Akaike’s information criterion (AIC): The general theory and its analytical extensions. Psychometrika 52, 345–370 (1987).
Chakrabarti, A. & Ghosh, J. K. AIC, BIC and recent advances in model selection. Philos. Stat. 583–605 (2011).
Weakliem, D. L. A critique of the Bayesian information criterion for model selection. Sociol. Methods Res. 27, 359–397 (1999).
Neath, A. A. & Cavanaugh, J. E. The Bayesian information criterion: Background, derivation, and applications. Wiley Interdiscip. Rev. Comput. Stat. 4, 199–203 (2012).
Bayarri, M. J. et al. Prior-based Bayesian information criterion. Stat. Theory Relat. Fields 3, 2–13 (2019).
Chowdhury, M. Z. I., & Turin, T. C. Variable selection strategies and its importance in clinical prediction modelling. Fam. Med. Commun. Health8 (2020).
Heinze, G., Wallisch, C. & Dunkler, D. Variable selection-a review and recommendations for the practicing statistician. Biom. J. 60, 431–449 (2018).
Ahrens, A., Hansen, C. B. & Schaffer, M. E. lassopack: Model selection and prediction with regularized regression in Statan. Stata J. 20, 176–235 (2020).
Alhawari, H. H. et al. Blood pressure and its association with gender, body mass index, smoking, and family history among university students. Int. J. Hypertens.2018 (2018).
Ghosh, S., Mukhopadhyay, S. & Barik, A. Sex differences in the risk profile of hypertension: A cross-sectional study. BMJ Open 6, e010085 (2016).
Oparil, S. & Miller, A. P. Gender and blood pressure. J. Clin. Hypertens. 7, 300–309 (2005).
Menacho, A. A. et al. Nutritional status and blood pressure in adolescent students. Arch. Argent. Pediatr. 112, 302–307 (2014).
Santosa, A. et al. Gender differences and determinants of prevalence, awareness, treatment and control of hypertension among adults in China and Sweden. BMC Public Health 20, 1–13 (2020).
Pinto, E. Blood pressure and ageing. Postgrad. Med. J. 83, 109–114 (2007).
Buford, T. W. Hypertension and aging. Ageing Res. Rev. 26, 96–111 (2016).
Gurven, M., Blackwell, A. D., Rodríguez, D. E., Stieglitz, J. & Kaplan, H. Does blood pressure inevitably rise with age, Longitudinal evidence among forager-horticulturalists. Hypertension 60, 25–33 (2012).
Gurven, M. et al. Does blood pressure inevitably rise with age?. Longitud. Evid. Among Forager-hortic. Hypertens. 60, 25–33 (2012).
China PEACE Collaborative Group and others. Association of age and blood pressure among 3.3 million adults insights from China PEACE million persons project. Hypertension 39, 1143–1154 (2021).
Chen, F. et al. Association between childhood obesity and metabolic syndrome: Evidence from a large sample of Chinese children and adolescents. Blood Press. 10, e47380 (2012).
Kotsis, V. et al. Mechanisms of obesity-induced hypertension. Hypertens. Res. 33, 386–393 (2010).
Dong, G. H. et al. Interactions between air pollution and obesity on blood pressure and hypertension in Chinese children. Epidemiology 26, 740–747 (2010).
Wang, Z. et al. Association of visceral and total body fat with hypertension and prehypertension in a middle-aged Chinese population. Hypertension 33, 1555–1562 (2015).
Wang, H. et al. Adiposity measures and blood pressure in Chinese children and adolescents. Arch. Dis. Child. 93, 738–744 (2008).
Dong, B., Wang, Z., Wang, H. J. & Ma, J. Population attributable risk of overweight and obesity for high blood pressure in Chinese children. Blood Press. 24, 230–236 (2015).
Bin, D., Jun, M. A., Wang, H. J. & Wang, Z. Q. The association of overweight and obesity with blood pressure among Chinese children and adolescents. Biomed. Environ. Sci. 26, 437–444 (2013).
Kim, S. J. et al. Cardiovascular risk factors for incident hypertension in the prehypertensive population. Epidemiol. Health32 (2010).
Diaz, K. M. & Shimbo, D. Physical activity and the prevention of hypertension. Curr. Hypertens. Rep. 15, 659–668 (2013).
Zheng, L. et al. Predictors of progression from prehypertension to hypertension among rural Chinese adults: Results from Liaoning Province. Eur. J. Prev. Cardiol. 17, 217–222 (2010).
Faselis, C. et al. Exercise capacity and progression from prehypertension to hypertension. Hypertension 60, 333–338 (2012).
Laine, M. K. et al. Former male elite athletes and risk of hypertension in later life. Hypertension 33, 1549–1554 (2015).
Sharman, J. E., La Gerche, A. & Coombes, J. S. Exercise and cardiovascular risk in patients with hypertension. Am. J. Hypertens. 28, 147–158 (2015).
Zhu, Z. et al. Association between exercise and blood pressure in hypertensive residents: A meta-analysis. Evid.-Based Complement. Altern. Med.2020 (2020).
Zhu, Z. et al. Association between exercise and blood pressure in hypertensive residents: A meta-analysis. Evid.-Based Complement. Altern. Med. (2022).
Nerenberg, K. A. et al. Hypertension Canada’s 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can. J. Cardiol. 34, 506–525 (2018).
Shimamoto, K. et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens. Res. 37, 253–390 (2014).
Liu, L.-S. et al. 2010 Chinese guidelines for the management of hypertension. Zhonghua xin xue guan bing za zhi 39, 579–615 (2011).
Chalmers, J. et al. 1999 world health organization-international society of hypertension guidelines for the management of hypertension, guidelines sub-committee of the World Health Organization. Clin. Exp. Hypertens. 21, 1009–1060 (1999).
Gupta, R. D. et al. Association between height and hypertension among US adults: Analyses of national health and nutrition examination survey 2007–18. Clin. Hypertens. 21, 1–12 (2021).
Stanaway, J. D. et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1923–1994 (2018).
Brianna, B. et al. Associations between height and blood pressure in the United States population. Medicine96 (2017).
London, G. M. et al. Body height as a determinant of carotid pulse contour in humans. Hypertension 10, S93–S96 (1992).
Langenberg, C., Hardy, R., Kuh, D. & Wadsworth, M. E. J. Influence of height, leg and trunk length on pulse pressure, systolic and diastolic blood pressure. Hypertension 21, 537–543 (2003).
Gupta, Das et al. Association between height and hypertension in the adult Nepalese population: Findings from a nationally representative survey. Health Sci. Rep. 2, e141 (2019).
Palmer, J. R., Rosenberg, L. & Shapiro, S. Stature and the risk of myocardial infarction in women. Am. J. Epidemiol. 10, 27–32 (1990).
Elzinga, G. & Westerhof, N. CMatching between ventricle and arterial load. Evol. Process Circ. Res. 68, 1495–1500 (1991).
Smulyan, H. et al. Comparative effects of aging in men and women on the properties of the arterial tree. J. Am. Coll. Cardiol. 37, 1374–1380 (2001).
Sin, D. D., Wu, L. & Man, S. P. The relationship between reduced lung function and cardiovascular mortality: A population-based study and a systematic review of the literature. Chest 127, 1952–1959 (2005).
Tsimihodimos, V. et al. Hypertension and diabetes mellitus: Coprediction and time trajectories. Hypertension 71, 422–428 (2018).
Petrie, J. R., Guzik, T. J. & Touyz, R. M. Diabetes, hypertension, and cardiovascular disease: Clinical insights and vascular mechanisms. Can. J. Cardiol. 34, 575–584 (2018).
Petrie, J. R., Guzik, T. J. & Touyz, R. M. Diabetes, hypertension, and cardiovascular disease. Clinical insights and vascular mechanisms. Can. J. Cardiol. 34, 575–584 (2018).
Kim, Min-Ju., Lim, Nam-Kyoo., Choi, Sun-Ja. & Park, Hyun-Young. Hypertension is an independent risk factor for type 2 diabetes: The Korean genome and epidemiology study. Hypertens. Res. 38, 783–789 (2015).
Wise, J. High blood pressure is linked to increased risk of diabetes. BMJ351 (2015)
Liu, S. Y. et al. The association between blood pressure and years of schooling versus educational credentials: Test of the sheepskin effect. Ann. Epidemiol. 21, 128–138 (2011).
Żylińska, E. & Kosior, D. A. Education, cardiovascular risk factors and blood pressure control in hypertensive outpatients. Kardiol. Polska (Polish Heart Journal) 76, 1551–1561 (2018).
Chiara, Di. et al. Education and hypertension: Impact on global cardiovascular risk. Acta Cardiol. 72, 507–513 (2017).
Choi, J. W. et al. Factors related to blood pressure control and the effect of an education program performed by family physicians on patients with hypertension. Korean J. Fam. Pract. 8, 175–181 (2018).
Acknowledgements
We thank the World Health Organization (WHO) for making data, on “study on Global AGEing and Adult Health (SAGE)”, available for the study.
Author information
Authors and Affiliations
Contributions
A.I. conceptualized this research and is responsible for writing the methodology, formal analysis, and draft of the original version of this manuscript. I.B.K., J.G.J., B.A., and D.A.E. wrote the introduction and provided also interpretation of the results, revisions and editing of the manuscript. The authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iddrisu, AK., Besing Karadaar, I., Gurah Junior, J. et al. Mixed effects logistic regression analysis of blood pressure among Ghanaians and associated risk factors. Sci Rep 13, 7728 (2023). https://doi.org/10.1038/s41598-023-34478-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34478-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.