Abstract
To construct and validate prediction formulae of sagittal alignment in thoracolumbar kyphosis secondary to ankylosing spondylitis (AS) after osteotomy. A total of 115 AS patients who suffered from thoracolumbar kyphosis and underwent osteotomy were enrolled, with 85 patients in derivation group and 30 patients in validation group. Radiographic parameters were measured on lateral radiographs, including thoracic kyphosis, lumbar lordosis (LL), T1 pelvic angel (TPA), sagittal vertical axis (SVA), osteotomized vertebral angle, pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), and PI and LL mismatch (PI-LL). Prediction formulae of SS, PT, TPA and SVA were established; and their effectiveness was evaluated. There was no significant difference in baseline characteristics between the two groups (p > 0.05). In derivation group, LL and PI-LL were correlated with SS, and were then used to establish the prediction formula of SS[SS = − 12.791–0.765 × (LL) + 0.357 × (PI-LL), R2 = 68.3%]; PI and PI-LL were correlated with PT, and the prediction formula of PT were thus established[PT = 12.108 + 0.402 × (PI-LL) + 0.252 × (PI), R2 = 56.8%]; PT, PI-LL and LL were correlated with TPA, and were used to establish the prediction formula of TPA[TPA = 0.225 + 0.597 × (PT) + 0.464 × (PI-LL)-0.161 × (LL), R2 = 87.4%]; PT, PI-LL and age were correlated with SVA, and were used to establish the prediction formula of SVA[SVA = 36.157 + 2.790 × (PI-LL) + 1.657 × (Age)-1.813 × (PT), R2 = 41.5%]. In validation group, the predictive SS, PT, TPA and SVA were basically consistent with corresponding real values; and the mean error between predictive values and real values was of 1.3° in SS, 1.2° in PT, 1.1° in TPA and 8.6 mm in SVA. Postoperative SS, PT, TPA and SVA could be predicted with PI and the planned LL and PI-LL using prediction formulae, providing a method for AS kyphosis to plan postoperative sagittal alignment. Change of pelvic posture after osteotomy was quantitatively evaluated using the formulae.
Similar content being viewed by others
Introduction
Sagittal malalignment causes internal fixation failure and low health-related quality of life in ankylosing spondylitis (AS) after osteotomy1,2,3,4. The causes of sagittal malalignment are mainly linked to inadequate kyphosis correction and mismatched spinopelvic harmony5,6,7. Reconstructing balanced sagittal alignment and harmonious spinopelvic relationship are necessary to maintain kyphosis correction and achieve satisfactory clinical outcome in AS patients8,9. In our previous study10, the risk factors of sagittal malalignment after osteotomy were evaluated, and the postoperative immediate sagittal vertical axis (SVA) of ≤ 74 mm was recommended for preventing sagittal imbalance. However, given the complex interaction compensatory mechanism between spine and pelvis, how to achieve SVA of ≤ 74 mm has not been established. Generally, postoperative sagittal alignment is constructed by surgeon according to the plan. And an appropriate surgical plan is the key step to construct a proper sagittal alignment. Predicting sagittal alignment and knowing the required degree of osteotomy can be of great help in designing a successful surgical plan. However, there is no clear method to predict the postoperative sagittal alignment for AS kyphosis, especially to evaluate the change of pelvic posture after osteotomy11,12,13, which might hamper the development of an appropriate surgical plan. In adult spinal deformity (ASD), Lafage et al.14,15 proposed two formulae to predict the postoperative pelvic tilt (PT) and SVA, and guide the formulation of surgical plans, which contributed to resolving the problem in ASD. However, whether the sagittal alignment of AS kyphosis after osteotomy could be predicted and used for devising a surgical plan remains unclear.
Therefore, in this study, we aimed to construct and validate prediction formulae for predicting pelvic posture [PT, sacral slope (SS)] and global alignment [T1 pelvic angel (TPA), SVA] in thoracolumbar kyphosis secondary to AS after osteotomy; and proposed a novel method to devise surgical plans for these patients.
Materials and methods
Subjects and study design
Consecutive AS thoracolumbar kyphosis cases who underwent osteotomy between January 2010 and January 2020, were retrospectively reviewed. Anteroposterior and lateral radiographs of whole spine were obtained in all patients, who were instructed to stand in a freestanding position with elbows flexed at approximately 45° and fingertips under the chin. This position allowed for consistent technique and comparative analysis11,16,17. Indications for surgery were that: (1) thoracolumbar kyphosis with global kyphosis > 50°, SVA > 50 mm or PT > 25°, (2) impaired quality of life, including having trouble in walking upright, lying flat and seeing horizontally, and (3) strong desire for surgical treatment. Patients aged ≥ 18 years and with osteotomy on thoracolumbar/lumbar vertebrae were enrolled in this study. Those with hip or knee contracture or ankylosis, postoperative pseudarthrosis or instrumentation failure during the follow-up were excluded. Finally, a total of 115 AS patients met the criteria and were randomly divided into two groups, with 85 patients in derivation group and 30 patients in validation group. The data from derivation group was used for exploring and developing prediction formulae, including analyzing correlation between age, spinal and pelvic parameters, and establishing prediction formulae of postoperative SS, PT, TPA and SVA. The data from validation group was used for assessing and validating the formulae, including evaluating reliability of prediction formulae, and comparing difference between predictive value and real value.
Data collection
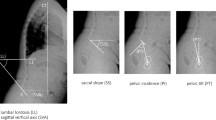
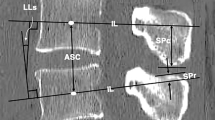
Standing anteroposterior and lateral radiographs of the whole spine were obtained preoperatively and postoperatively (6 months after surgery). The radiographic parameters were measured on lateral radiographs using Surgimap Spine Software (version 2.3.1.3, Nemaris Inc., New York, USA), including thoracic kyphosis (TK), lumbar lordosis (LL), TPA, SVA, osteotomized vertebral angle (OVA) (for two-level osteotomy, OVA was defined as the sum of two Cobb angles measured in two osteotomized vertebrae), pelvic incidence (PI), PT, SS, and PI and LL mismatch (PI-LL) (Fig. 1). All parameters were measured independently by two experienced professionals. PI was considered as a fixed parameter before and after surgery in this study18,19. The demographic and surgical data was collected and recorded for all patients.
Illustration of radiographic parameters measurement. Thoracic kyphosis (TK): the Cobb angle from the T4 upper endplate to the T12 lower endplate; lumbar lordosis (LL): the Cobb angle from the L1 upper endplate to the S1 upper endplate; T1 pelvic angle (TPA): the angle between a line joining the center of T1 and the femoral head axis and a line from the center of the femoral head axis to the midpoint of the S1 upper endplate; sagittal vertical axis (SVA): the distance between the C7 plumb line and the posterosuperior corner of S1; osteotomized vertical angle (OVA): the angle between the lower endplate of the osteotomized vertebra and the upper endplate of the cranial adjacent vertebra; pelvic incidence (PI) : the angle between the line perpendicular to the S1 upper endplate and the line from the center of the S1 upper endplate to the center of the femoral head axis; pelvic tilt (PT): the angle between the vertical line and the line from the center of the S1 upper endplate to the center of the femoral head axis; sacral slope (SS): the angle between the S1 upper endplate and the horizontal line; PI and LL mismatch (PI-LL): the pelvic incidence value minus the lumbar lordosis value.
Statistical analysis
Measurement data were expressed as the mean ± standard deviation. Statistical analysis was performed using SPSS software (version 22.0, SPSS, Inc., Chicago, IL). Baseline characteristics of demographic and radiographic data in two groups were compared using two independent samples t-tests and chi-square tests. Correlation between age, spinal and pelvic parameters were determined using Pearson’s coefficient analysis. Based on correlation between target parameters (SS, PT, TPA and SVA) and the surgically controllable parameters (LL and PI-LL), prediction formulae were then established using multiple stepwise linear regression analysis. Differences between predictive values and real values were evaluated using paired t-tests in validation group. Correlation between osteotomy parameters (sites of osteotomy and OVA correction) and the correction of target parameters were analyzed using Spearman (for sites of osteotomy) and Pearson (for OVA corrections) coefficients analysis. Effect of different sites of osteotomy on the correction of target parameters was determined using analysis of variance. A difference with a p-value < 0.05 was considered statistically significant.
Ethical approval
The study was performed in accordance with the Declaration of Helsinki, and approved by the institutional review board of Shenzhen University General Hospital. The informed consent was obtained from all participants for both study participation and publication of identifying information/images in an online open-access publication.
Results
Comparison of baseline characteristics between two groups
A total of 115 AS patients (102 men and 13 women) with an average age of 37.3 ± 8.1 years (range, 20–64 years) were enrolled, including 85 in derivation group and 30 in validation group. Eighty-nine patients underwent one-level osteotomy and 26 patients underwent two-level osteotomy. There was no significant difference in demographic and radiographic data between the derivation group and the validation group (all p > 0.05) (Table 1).
Correlation between age, spinal and pelvic parameters
The postoperative SS was strongly correlated with LL, PI and PI-LL (r = − 0.732, 0.595 and − 0.397, respectively, p < 0.05); the postoperative PT was significantly correlated with LL, PI and PI-LL (r = 0.380, 0.433 and 0.711, respectively, p < 0.05); the postoperative TPA was significantly correlated with LL, PT, PI, SS, PI-LL and age (r = 0.450, 0.867, 0.467, − 0.290, 0.826 and 0.223, respectively, p < 0.05); and the postoperative SVA was significantly correlated with LL, PT, PI, PI-LL and age (r = 0.357, 0.281, 0.265, 0.588 and 0.261, respectively, p < 0.05) (Table 2).
Prediction formulae of postoperative SS, PT, TPA and SVA
Based on the correlation between SS, PT, TPA and SVA, and other postoperative parameters, the prediction formulae of SS, PT, TPA and SVA were then established using multiple stepwise linear regression analysis.
The LL, PI and PI-LL were entered into analysis, after which only the LL and PI-LL were included in the model. The prediction formula of SS was thus established: SS = − 12.791–0.765 × (LL) + 0.357 × (PI-LL), p < 0.001, with adjusted R2 = 68.3% (Table 3).
The LL, PI and PI-LL were entered into analysis, and only the PI and PI-LL were included in the model. The prediction formula of PT was thus established: PT = 12.108 + 0.402 × (PI-LL) + 0.252 × (PI), p < 0.001, with adjusted R2 = 56.8% (Table 3).
The LL, PT, PI, SS, PI-LL and age were entered into analysis, after which the PT, PI-LL and LL were included in the model. The prediction formula of TPA was thus established: TPA = 0.225 + 0.597 × (PT) + 0.464 × (PI-LL)-0.161 × (LL), p < 0.001, with adjusted R2 = 87.4% (Table 3).
The LL, PT, PI, PI-LL and age were entered into analysis, after which the PI-LL, PT and age were included in the model. The prediction formula of SVA was thus established: SVA = 36.157 + 2.790 × (PI-LL) + 1.657 × (Age)-1.813 × (PT), p < 0.001, with adjusted R2 = 41.5% (Table 3).
Validation of the prediction formulae
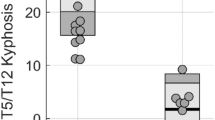
In derivation group, the predictive SS, PT, TPA and SVA which were calculated using the prediction formulae with postoperative PI, PI-LL and LL (surgically controllable parameters), were basically in agreement with the postoperative real values (R2 = 69.1%, 57.8%, 87.2% and 42.2%, respectively, Fig. 2A–D). The data from validation group confirmed that, the postoperative SS, PT, TPA and SVA could be predicted with postoperative PI, PI-LL and LL through the prediction formulae (R2 = 32.4%, 41.8%, 79.2% and 39.1%, respectively, Fig. 3A–D), and the mean error between the predictive values and the real values was of 1.3 ± 7.7° in SS, 1.2 ± 7.7° in PT, 1.1 ± 4.8° in TPA and 8.6 ± 48.6 mm in SVA (Table 4).
Effects of different osteotomy sites on SS, PT, TPA and SVA correction
Eighty-six cases of AS kyphosis who underwent one-level osteotomy at L1, L2 and L3 were included for analyzing the effect of osteotomized sites on pelvic posture and global alignment. Sites of osteotomy were correlated with SVA correction (r = 0.307, p = 0.004); and the OVA correction was correlated with TPA and SVA correction (r = 0.697 and 0.365, respectively, p < 0.05). But both the osteotomy sites and OVA correction were not statistically correlated with the correction of SS and PT (p > 0.05) (Table 5). There was no significant difference in the corrections of OVA, SS, PT and TPA at different sites of osteotomy (p > 0.05, Table 6). The SVA correction achieved at L2 (p = 0.029) and L3 (p = 0.068) osteotomy was larger than that achieved at L1 osteotomy (Table 6).
Case illustration for surgical plan
Predictive ability of the formulae could be applied in surgical plan. The planned PI-LL in regional curvatures achieved by osteotomy, along with the fixed PI, were used to predict the postoperative SS, PT, TPA and SVA. The PI (40.5°) was the only parameter that required to be measured in preoperative radiograph (Fig. 4). With the planned PI-LL (3.0°), the LL was calculated using equation of LL = PI-3.0 = 37.5°. The planned PI-LL and LL were then used to predict SS and PT using the formulae. Subsequently, the TPA and SVA were then predicted with the predictive PT and age (42). The detail of calculation was as follows:
and
A 42-year-old man suffered from thoracolumbar kyphosis secondary to ankylosing spondylitis. (A) Preoperative radiographs showed severe global kyphosis and sagittal imbalance. (B) The patient underwent one-level three-column osteotomy on L2, following which the kyphosis was corrected and the sagittal alignment was restored.
Analysis of the results indicated that the predictive SS, PT and TPA were similar to the postoperative real values (Table 7, Fig. 4). The postoperative real SVA was 8.1 mm larger than the predictive SVA, and it would be closer to the predictive value with lower site of osteotomy.
Discussion
Sagittal malalignment following osteotomy is a major determinant of clinical outcome in AS patients2,6. Given the complex interactional compensatory mechanisms between spine and pelvis, it is difficult for the surgeon to control and correct sagittal malalignment, especially to restore the neutral pelvic position11,13. Moreover, the retroversion of pelvis cannot be corrected directly, and is restored mainly by reconstructing lumbar lordosis and spinopelvic harmony12,20. However, the correlation between postoperative sagittal alignment and compensatory pelvic rotation is unclear, and the extent to which sagittal alignment should be reconstructed after osteotomy to compensate for pelvic rotation remains unknown.
In this study, the pelvic parameters (SS and PT) were significantly correlated with LL, PI and PI-LL; and the predictive formulae of SS and PT were then established based on the correlation. The formulae make it possible to evaluate the extent of sagittal alignment reconstruction to compensate for postoperative pelvic rotation. Using the formulae, the predictive SS and PT could be estimated with the fixed PI and the planned PI-LL and LL (surgically controllable parameters). Subsequently, the change of pelvic posture after osteotomy was predicted, which was reflected by the correction of SS and PT. Notably, the formulae revealed that the key to restoring pelvic position was to construct lumbar lordosis (LL) and correct spinopelvic harmony (PI-LL), which was consistent with the conclusions of Schwab21 and Liu22. The accurately predicted postoperative pelvic parameters (SS and PT) play an important role in devising proper and individualized plan. For example, the predictive SS could be used in the ASKyphoplan23 for devising individualized plan according to the individual pelvic pattern, instead of using the same angle of 40° (normal range) for every patient24. The PT prediction formula of AS kyphosis was particularly suitable for Song’s method17 to devise a personalized plan based on the specificity of disease, instead of using the prediction formula of PT = − 7 + 0.37 × PI in asymptomatic subjects19. Although PT could be calculated with PI and predictive SS using the formula of PT = PI-SS25, it might include some calculation error by using predictive SS for further predicting PT. Hence, it would be more reliable to use the original PI and planned PI-LL to predict postoperative PT through the prediction formula instead of PI-predictive SS, which was also proven by our data (difference between the predictive PT calculated by our prediction formula and the one calculated by PI-predictive SS was 0.4°, p < 0.001).
The global alignment parameters (TPA and SVA) were significantly correlated with LL, PT, PI, PI-LL and age. The prediction formulae of TPA and SVA were then established. With the predictive PT and the planned PI-LL and LL, the postoperative TPA and SVA were calculated using the formulae. Subsequently, the aforementioned postoperative immediate SVA of ≤ 74 mm was thus predicted and applied for preventing sagittal imbalance10. The capability of the prediction formulae to predict TPA and SVA was different. The prediction formulae of TPA to predict postoperative TPA was more precise and reliable than the prediction formulae of SVA to predict postoperative SVA (adjusted R2: 87.4% vs. 41.5%). It was possibly because TPA was less affected by patient’s standing posture, and was more accurate than SVA in reflecting global alignment. Therefore, the TPA could be a better choice for the reference of assessing postoperative global alignment in surgical planning.
In this study, there was no significant correlation between the sites of osteotomy and the correction of SS and PT, which indicated that the sites of osteotomy might not affect the pelvis rotation postoperatively, but were positively correlated with SVA correction. The results were in contrast to Lafage26, who reported that the sites of osteotomy were correlated with changes of SS and PT, but not with the change of SVA in ASD. The contrasting results might be due to the different pathogenic processes between AS and ASD. In AS kyphosis, the sagittal alignment were stiff and fused, without pelvic version accommodation; the change of pelvic posture (SS and PT) was mainly achieved by using femoral head as fulcrum and rotating anteriorly. With a similar OVA correction, the lower site of osteotomy was selected, and the larger correction of global alignment (TPA and SVA) was achieved in AS kyphosis24,27,28. However, in ASD, the sagittal alignment was flexible and showed dynamic change, leaving variable modifications to SS, PT, TPA and SVA after osteotomy.
In the past, it was common to plan a surgery by calculating required osteotomized vertebral angle24,28,29. Ondra et al.28 proposed a mathematical method to calculate the osteotomized vertebral angle for correcting the kyphosis; but they failed to consider the pelvis compensation in their method. Van Royen et al.24 assumed an SS of 40° (normal range) as postoperative pelvis position, and then calculated the required osteotomized angle by trigonometric method. Obviously, the assumption of SS = 40° was not an appropriate angle for devising an individualized plan. Zheng30 and Song17 considered the pelvic compensation and used the theoretical PT as reference for plan; however, not all AS patients could totally compensate the PT to a theoretical value. The present study provided a novel method for devising individualized plan for AS kyphosis using the prediction formulae, which considered the correlation between pelvis compensation and sagittal alignment. In this method, planning proper target of PI-LL and performing it strictly were the key steps for successful radiographic outcome. PI-LL reflected spinopelvic harmony, and was linked to sagittal balance. The optimal PI-LL of ± 9 was recommended for the young, but some adjustments may be needed for older adults21,31. Lafage and colleagues14,15 used the prediction formulae of PT and SVA to devise a surgical plan for ASD, and obtained satisfactory radiographic outcome. Similarly, the prediction formulae of SS, PT, TPA and SVA in this study were a potentially useful method to devise individualized plan for AS kyphosis.
Limitations
First, the planning method was performed using planned LL and PI-LL to predict postoperative sagittal alignment, which was only available to those with thoracolumbar/lumbar vertebrae osteotomy, but might be unsuitable for those with thoracic vertebrae osteotomy. For patients with ankylosed cervical vertebrae, PI-LL should be carefully and conservatively planned to ensure horizon vision and avoid over correction postoperatively. Second, the prediction formulae were applicable to patients with complete pelvis compensatory capacity; those with hip or knee soft-tissue contracture or ankylosis might lose pelvic compensatory ability and were unsuitable for the prediction formulae. Third, the effect of two-level osteotomy on sagittal alignment has not been analyzed for limited samples. In the future, a prospective and multi-center study with a larger sample size is required to confirm the conclusions.
Conclusions
Postoperative SS, PT, TPA and SVA could be predicted with the fixed PI and the planned LL and PI-LL using prediction formulae, providing a method for AS kyphosis to plan postoperative sagittal alignment. Change of pelvic posture after osteotomy was quantitatively evaluated with the formulae. Selection of vertebral sites of osteotomy affected the global alignment correction but not the pelvis rotation.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Zhao, S. Z., Qian, B. P., Qiao, M., Jiang, J. & Qiu, Y. Does solid fusion eliminate rod fracture after pedicle subtraction osteotomy in ankylosing spondylitis-related thoracolumbar kyphosis?. Spine J. 19, 79–86. https://doi.org/10.1016/j.spinee.2018.05.024 (2019).
Qian, B. P. et al. Radiographical predictors for postoperative sagittal imbalance in patients with thoracolumbar kyphosis secondary to ankylosing spondylitis after lumbar pedicle subtraction osteotomy. Spine 38, E1669-1675. https://doi.org/10.1097/BRS.0000000000000021 (2013).
Zhao, S. Z. et al. Failure patterns and related risk factors of sagittal reconstruction following pedicle subtraction osteotomy in patients with ankylosing spondylitis and thoracolumbar kyphosis. Neurosurg. Focus 51, E7. https://doi.org/10.3171/2021.7.Focus21146 (2021).
Yilgor, C. et al. Global alignment and proportion (GAP) score: Development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J. Bone Joint Surg. Am. 99, 1661–1672. https://doi.org/10.2106/jbjs.16.01594 (2017).
Schwab, F. J. et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: A prospective multicenter analysis. Spine 38, E803-812. https://doi.org/10.1097/BRS.0b013e318292b7b9 (2013).
Huang, J. C. et al. What is the optimal postoperative sagittal alignment in ankylosing spondylitis patients with thoracolumbar kyphosis following one-level pedicle subtraction osteotomy?. Spine J. 20, 765–775. https://doi.org/10.1016/j.spinee.2019.11.005 (2020).
Schwab, F. J. et al. Sagittal realignment failures following pedicle subtraction osteotomy surgery: Are we doing enough?: Clinical article. J. Neurosurg. Spine 16, 539–546. https://doi.org/10.3171/2012.2.Spine11120 (2012).
Sato, T. et al. Relationship between characteristics of spinopelvic alignment and quality of life in Japanese patients with ankylosing spondylitis: A cross-sectional study. BMC Musculoskelet. Disord. 21, 41. https://doi.org/10.1186/s12891-020-3040-z (2020).
Shin, J. K., Lee, J. S., Goh, T. S. & Son, S. M. Correlation between clinical outcome and spinopelvic parameters in ankylosing spondylitis. Eur. Spine J. 23, 242–247. https://doi.org/10.1007/s00586-013-2929-8 (2014).
Luo, J. et al. Preoperative prediction of sagittal imbalance in kyphosis secondary to ankylosing spondylitis after one-level three-column osteotomy. BMC Musculoskelet. Disord. 23, 790. https://doi.org/10.1186/s12891-022-05740-9 (2022).
Qian, B. P. et al. The presence of a negative sacral slope in patients with ankylosing spondylitis with severe thoracolumbar kyphosis. J. Bone Joint Surg. Am. 96, e188. https://doi.org/10.2106/JBJS.M.01070 (2014).
Hu, J. et al. Can acetabular orientation be restored by lumbar pedicle subtraction osteotomy in ankylosing spondylitis patients with thoracolumbar kyphosis?. Eur. Spine J. 26, 1826–1832. https://doi.org/10.1007/s00586-016-4709-8 (2017).
Zhao, S. Z. et al. The relationship between global spinal alignment and pelvic orientation from standing to sitting following pedicle subtraction osteotomy in ankylosing spondylitis patients with thoracolumbar kyphosis. Arch. Orthop. Trauma Surg. 139, 761–768. https://doi.org/10.1007/s00402-018-03107-1 (2019).
Lafage, V. et al. Spino-pelvic parameters after surgery can be predicted: A preliminary formula and validation of standing alignment. Spine 36, 1037–1045. https://doi.org/10.1097/BRS.0b013e3181eb9469 (2011).
Lafage, V. et al. Multicenter validation of a formula predicting postoperative spinopelvic alignment. J. Neurosurg. Spine 16, 15–21. https://doi.org/10.3171/2011.8.SPINE11272 (2012).
Marks, M. C., Stanford, C. F., Mahar, A. T. & Newton, P. O. Standing lateral radiographic positioning does not represent customary standing balance. Spine 28, 1176–1182. https://doi.org/10.1097/01.Brs.0000067271.00258.51 (2003).
Song, K. et al. A new method for calculating the exact angle required for spinal osteotomy. Spine 38, E616-620. https://doi.org/10.1097/BRS.0b013e31828b3299 (2013).
Legaye, J., Duval-Beaupère, G., Hecquet, J. & Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 7, 99–103. https://doi.org/10.1007/s005860050038 (1998).
Vialle, R. et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J. Bone Joint Surg. Am. 87, 260–267. https://doi.org/10.2106/jbjs.D.02043 (2005).
Celestre, P. C., Dimar, J. R. 2nd. & Glassman, S. D. Spinopelvic parameters: Lumbar lordosis, pelvic incidence, pelvic tilt, and sacral slope: What does a spine surgeon need to know to plan a lumbar deformity correction?. Neurosurg. Clin. N. Am. 29, 323–329. https://doi.org/10.1016/j.nec.2018.03.003 (2018).
Schwab, F., Patel, A., Ungar, B., Farcy, J. P. & Lafage, V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 35, 2224–2231. https://doi.org/10.1097/BRS.0b013e3181ee6bd4 (2010).
Liu, Z. J. et al. Does postoperative PI-LL mismatching affect surgical outcomes in thoracolumbar kyphosis associated with ankylosing spondylitis patients?. Clin. Neurol. Neurosurg. 169, 71–76. https://doi.org/10.1016/j.clineuro.2018.04.006 (2018).
van Royen, B. J., Scheerder, F. J., Jansen, E. & Smit, T. H. ASKyphoplan: A program for deformity planning in ankylosing spondylitis. Eur. Spine J. 16, 1445–1449. https://doi.org/10.1007/s00586-007-0371-5 (2007).
Van Royen, B. J., De Gast, A. & Smit, T. H. Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur. Spine J. 9, 492–498. https://doi.org/10.1007/s005860000183 (2000).
Le Huec, J. C., Aunoble, S., Philippe, L. & Nicolas, P. Pelvic parameters: Origin and significance. Eur. Spine J. 20(Suppl 5), 564–571. https://doi.org/10.1007/s00586-011-1940-1 (2011).
Lafage, V. et al. Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction?. J. Neurosurg. Spine 14, 184–191. https://doi.org/10.3171/2010.9.Spine10129 (2011).
Zavras, A. G. et al. Lumbar level significantly influences postoperative global sagittal balance following pedicle subtraction osteotomy. Glob. Spine j. https://doi.org/10.1177/21925682211032563 (2021).
Ondra, S. L., Marzouk, S., Koski, T., Silva, F. & Salehi, S. Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine 31, E973-979. https://doi.org/10.1097/01.brs.0000247950.02886.e5 (2006).
Min, K., Hahn, F. & Leonardi, M. Lumbar spinal osteotomy for kyphosis in ankylosing spondylitis: The significance of the whole body kyphosis angle. J. Spinal Disord. Tech. 20, 149–153. https://doi.org/10.1097/01.bsd.0000211252.67576.d9 (2007).
Zheng, G. et al. How to calculate the exact angle for two-level osteotomy in ankylosing spondylitis?. Spine 41, E1046-e1052. https://doi.org/10.1097/brs.0000000000001610 (2016).
Lafage, R. et al. Defining spino-pelvic alignment thresholds: Should operative goals in adult spinal deformity surgery account for age?. Spine 41, 62–68. https://doi.org/10.1097/brs.0000000000001171 (2016).
Funding
This study was funded by National Natural Science Foundation of China (81970761), Shenzhen Major Project of Fundamental Research (JCYJ20200109114233670), Sanming Project of Medicine in Shenzhen (SZSM201911011), Key Research and Development Program of Guangdong Province (2020B0909020002) and Shenzhen Key Laboratory Fund (ZDSYS20200811143757022).
Author information
Authors and Affiliations
Contributions
J.Z.L. and Z.L.Y. collected the radiographic and clinical data, C.G.D. and X.J.F. measured parameters. L.T., Y.Z.W. and L.J. analyzed the clinical data and measurements. J.Z.L. wrote the manuscript, T.L.W. revised the manuscript. J.Z.L. and T.L.W. conceived the idea and designed the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luo, J., Yang, Z., Duan, C. et al. Prediction formulae of sagittal alignment in thoracolumbar kyphosis secondary to ankylosing spondylitis after osteotomy. Sci Rep 13, 7747 (2023). https://doi.org/10.1038/s41598-023-34475-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34475-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.