Abstract
Person-centered cardiovascular health (CVH) may facilitate cardiovascular disease primordial prevention in low resources settings. The study aims to assess the validity of person-centered CVH compared to gold standard measured CVH by examining the concordance between person-centered vs. measured CVH together with their respective association with incident cardiovascular disease events (CVD). Life’s Simple 7 (LS7) CVH metrics, including non-smoking, Body Mass Index, diet, physical activity, blood glycemia, blood pressure, and blood cholesterol were collected from 19,473 adults participating in the e-cohort NutriNet-Santé study from 2011 to 2014 and were followed until September 2020. Clinical examinations and blood analyses defined the measured biological metrics, while diagnoses, medication, or treatment for type 2 diabetes, hypertension, and hypercholesterolemia defined person-centered biological metrics. Declared behavioral metrics were common for both measured and person-centered CVH. The study included 18,714 CVD-free participants (mean age 51 years, 73% women), among whom 16.52% and 38.75% had 5–7 ideal LS7 metrics according to measured and person-centered CVH, respectively. Weighted concordance of person-centered and measured CVH was 0.87 [0.86; 0.88]. Over median follow-up of 8.05 years, 749 CVD events occurred. There was a 7% (HR 0.93 [0.88; 0.99]) and 13% (HR 0.87 [0.83; 0.92]) risk reduction of CVD risk by additional measured and person-centered ideal metrics, respectively. In conclusion, person-centered CVH may represent a reliable alternative to measured CVH.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVD) are associated with the highest disease burden globally, with a 2019 prevalence of 523 million, nearly double the figure observed in 1990. During the same period, CVD mortality increased from 12.1 million 95% UI [11.4; 12.6] to 18.6 million 95% UI [17.1; 19.7]. The contribution of CVD to Disability Adjusted Life Years (DALYs) doubled in 2019 compared to 19901. While primary prevention has been shown to explain more than half of the decline in CVD mortality in industrialized countries2, the figures above underline the need to do more, particularly in low and middle-income countries (LMIC) that are witnessing an epidemiological transition3. In addition to controlling risk factors once they are in place (primary prevention), preventing their onset in the first place might be an additional complementary preventative strategy, the so-called primordial prevention.
Primordial prevention is increasingly recognized as a key strategy for early CVD population prevention4. To this end, the American Heart Association defined Life’s Simple 7 (LS7) cardiovascular health (CVH) score, which includes four behavioral metrics (non-smoking, and ideal levels of body mass index, physical activity, and diet), and three biological metrics (untreated ideal levels of fasting plasma glucose, blood pressure, and total cholesterol), as a tool to monitor the level of cardiovascular health at the population level5. The clinical relevance of CVH has been established in various populations, whereby a higher CVH level is associated with lower CVD incidence6. However, the prevalence of ideal CVH, i.e. 5 or 6 to 7 ideal LS7 metrics, remains low, below 15% in the adult population6,7. Widespread use of cardiovascular health score is hindered by the prerequisite of clinical examinations and blood analyses. Moreover, blood biomarker measurements are particularly challenging to acquire in LMIC. From a global health perspective, given the high burden of CVD, the high prevalence of CVD risk factors, as well as socioeconomic disadvantages in LMIC1,8, one avenue to improve ideal CVH figures could be to adopt a person-centered CVH promotion model. Person-centered care approaches whereby individuals are informed and actively participate in their care are rapidly developing9. This approach could be extended to primordial prevention in which individuals have agency over their prevention and are empowered to adopt health-promoting behaviors. Nonetheless, the validity of person-centered CVH compared to the gold standard measured CVH and direct comparisons of their respective associations with incident CVD is currently unidentified. Therefore, the main study objective is to assess the validity of person-centered CVH compared to gold standard measured CVH. To address this question, (1) the concordance between person-centered vs. measured LS7 metrics was investigated; and (2) to provide clinical relevance to the findings, a qualitative comparison was conducted for the associations of person-centered vs. measured LS7 metrics with incident CVD.
Methods
The NutriNet-Santé Study (https://clinicaltrials.gov/, Registration Number: NCT03335644) is an ongoing web-based e-cohort launched in 2009 that examines the relationship between nutrition and health and determinants of dietary patterns and nutritional status10. The study recruited 171,000 participants aged ≥ 18 years from all over France with internet access. Between 2011 and 2014, blood measurements and physical examinations were recorded in a subsample of 19,473 participants, who represent the target population for the main analysis. The study was approved by the Institutional Review Board of the French Institute for Health and Medical Research and the National Commission on Informatics and Liberty, CNIL (n°908,450/ n°909,216). The participants consented after being informed about the study objectives and details. All research procedures were conducted in accordance with the declaration of Helsinki and relevant guidelines and regulations.
Data acquisition
The participants completed annual validated questionnaires on the NutriNet-Santé online platform (https://etude-nutrinet-sante.fr/). The questionnaires included sociodemographic and lifestyle questionnaires, comprising data on smoking of cigarettes, cigars, and pipes, an International Physical Activity Questionnaire (IPAQ)11, an anthropometric questionnaire for weight and height12,13, and a series of three nonconsecutive multi-seasonal web-based 24-h dietary records on two weekdays and one weekend day14,15,16. Recurrent 3-month questionnaires collected information on medical treatment and disease conditions.
During a clinical examination, height was measured by a stadiometer to the nearest 0.5 cm, and weight was measured by a calibrated scale to the nearest 0.1 kg (body composition analyzer BC-418MA, TANITA, Tokyo, Japan). Blood pressure was measured 3 times at 1-min intervals in a seated position after 5 min of rest using an automatic sphygmomanometer (Omron HEM-7015IT®; OMRON). The average of the recorded values was used in the present study. The participants were requested online to visit a participating Local Sample Collection Centers (LSCC) equipped for blood sample draws. Total serum cholesterol was measured by enzymatic cholesterol oxidase (Architect c8000®, Abbott). Fasting plasma glucose (FPG) was measured by hexokinase/G-6-PDH (Architect c8000®, Abbott).
CVH metrics
Definitions
Table 1 lists the definitions of person-centered and measured CVH metrics. Ideal levels for the behavioral metrics correspond to BMI < 25 kg/m2, never smoker and quitter > 12 months, ≥ 75 min/week of vigorous physical activity, ≥ 150 min/week of moderate physical activity, or a combination of the two, and ≥ 4 optimal diet items (the equivalent of 5 servings per day of fruits and vegetables or 400 gm/day (according to the national French nutrition and health program), the equivalent of fish consumption ≥ 2 times/week or average consumption of ≥ 100 gm/day, average sodium consumption < 1.5 gm/day, average fiber intake ≥ 25 gm/day, average intake of sugary drinks ≤ 152 ml/day). The ideal levels for the measured biological metrics correspond to untreated fasting blood glucose < 100 mg/dl, untreated blood pressure (BP) < 120/80 mmHg, and untreated total serum cholesterol < 200 mg/dl. The ideal level for the person-centered biological metrics corresponds to the absence of declared medication, treatment, or diagnosis for type 2 diabetes (T2D), hypertension, or hypercholesterolemia. The main exposure is the number of person-centered and measured ideal metrics (range 0–7). The number of person-centered and measured ideal metrics was also categorized as 0–2, 3–4, 5–7 ideal metrics to denote low, intermediate, and high CVH levels17.
Data sources
The completed questionnaires were used to define the person-centered behavioral metrics and the biological metrics, while the data collected during the physical examination (blood pressure) and blood tests (total serum cholesterol and fasting plasma glucose) were employed to define the measured biological metrics. Person-centered weight and height were shown to be adequately concordant with their measured counterparts in the Nutrinet-Santé Study, with an interclass correlation ICC 0.97 of measured and person-centered BMI12,13.
Alignment of health questionnaires and clinical appointment
The following approach was used to align the dates of health questionnaires (person-centered biological and behavioral metrics) with the dates of clinical appointment (measured biological metrics): for participants whose clinical appointment date was < 2 years from their recruitment date, their first questionnaire-based CVH metrics were used to define person-centered biological and behavioral metrics; and for those whose clinical appointment date was ≥ 2 years from their recruitment date, their follow-up questionnaire-based CVH metrics the closest to the clinical appointment date, which ensured a lag time less than two years were selected (time range: 0.55 to 63.52 months, Supplementary Fig. S1). In any case, the date of clinical appointment was used as the starting point for CVD events follow-up (see “Statistical methods”).
Covariates
The Educational attainment categories were (1) less than high school, (2) less than 2 years after high school), and (3) more than or equal to 2 years after high school. The occupational categories were (1) liberal profession: farmer, craftsperson, merchant, company director, specialized personnel, (2) intellectual profession, (3) intermediary profession, and (4) worker/employee. Alcohol use was calculated as daily average ethanol consumption (gm/day). CVD family history was defined by declared first-degree relative with CVD history.
CVD ascertainment
The primary outcome was fatal and non-fatal CVD events as of September 2020. The participants reported health events through a yearly health questionnaire, a check-up questionnaire every 3 months, or at any time through a dedicated platform on the study’s website. Participants’ families or doctors were contacted in case of no response on the study website for more than 1 year. A committee of physicians reviewed the medical data to validate major health event diagnoses, hospital admissions, and records, i.e. radiological reports and electrocardiograms. If necessary, the study doctors contacted the participants’ doctors or medical facilities, i.e. clinics, hospitals, or laboratories, to collect additional information. The data from the population-based cohort was linked to the medico-administrative databases of national health insurance (SNIIRAM); thus, limiting potential bias induced by unreported CVD. Fatal or non-fatal CVD cases were defined by the International Classification of Diseases ICD-10-CM, Tenth Revision. Hemorrhagic/ischemic stroke (ICD-10-I64), transient ischemic attack (ICD-10-G45.8 and ICD-10-G45.9), angina pectoris (ICD-10- I20.9), acute coronary syndrome (ICD-10- I24.9 and ICD-10-I21.4), myocardial infarction (ICD-10-I21), sudden cardiac death (ICD-10-I46.1, ICD-10-I46.9), coronary angioplasty (ICD-10-Z95.5), were included. For deceased participants, the causes of death were ascertained by linkage to the national registry of the causes of death, Center for Epidemiology of Causes of Death (CépiDC).
Statistical methods
The percentage agreement between low, intermediate, and high levels of the measured and person-centered CVH; percentage agreements between measured poor, intermediate, and ideal biological metrics vs. ideal/non-ideal person-centered biological metrics were estimated. Such analysis was not conducted for the behavioral LS7 metrics since they are common to person-centered and measured CVH. Weighted Gwet AC2/Brennan and Prediger coefficients assessed the inter-rater reliability (IRR) of the person-centered and measured number of ideal LS7 metrics (range 0–7)18,19, and they were quadratically weighed to allocate more weight to farther misclassifications of person-centered CVH according to the measured CVH level. Their value ranges from 0 to 1; the closer to 1, the more substantial the concordance. Sensitivity (Se), specificity (Sp), negative and positive predictive value test concordance statistics (NPV and PPV), and diagnostic accuracy (i.e. the proportion of correctly classified participants) were calculated using the measured CVH as a gold standard. These statistics were computed for the global CVH and individual biological metrics.
For survival analysis, person-time started at the date of the clinical appointment, and the event date was the first non-fatal CVD event, fatal CVD event, or mortality. Event-free participants’ follow-up was censored at their last answered questionnaire. Kaplan–Meier curves were used to plot the cumulative incidence of CVD using time-in-study, according to the low (0–2), intermediate (3–4), and high (5–7) measured and person-centered CVH levels. Survival curves were compared across CVH levels using the log-rank trend test. The hazard ratios (HR) and their 95% confidence intervals (CIs) for incident CVD were estimated per one point increase in the number of ideal LS7 metrics and for intermediate or high vs. low measured and person-centered CVH. Cox proportional hazard models using age as the time scale were stratified by birth-year (5-year intervals) and were adjusted for prespecified covariates including baseline sex, cohabitation status, educational attainment, occupational category, alcohol use, and CVD family history. The proportionality assumption was assessed using Schoenfeld’s residuals plot/test and negative log (log survival) plots. The linearity assumption between ideal metrics and incident CVD was tested via martingale residual analysis. Multiple imputations by chained equations were used to handle missing LS7 metrics (n = 2417) and missing covariates (n = 585), using linear or logistic regression models adjusted for demographic and socioeconomic variables. Fifty imputed datasets were produced, and the estimation method was Rubin’s combination rule.
Additional analyses
The robustness of the study results was evaluated by the following additional analyses. To assess the potential influence of latent CVD, the analyses were conducted by excluding participants who developed CVD during the first year of follow-up. To further explore to which extent the difference in definition between person-centered vs. measured biological metrics impacted the HR estimate, the hazard ratio estimates were computed exclusively for the biological LS7 metrics (i.e. per number of ideal metrics, ranging 0–3). Complete case analysis was conducted to evaluate the potential impact of missing values on the regression estimates. The competing risk of non-CVD mortality was estimated using the Fine and Gray method20. Given prior evidence relying measured CVH with non-CVD mortality7, the association of person-centered CVH with non-CVD-mortality was further evaluated. Population attributable preventive fraction was estimated for the hypothetical scenario in which all the population would have attained current high-level CVH. Lastly, to further evaluate the relevance of person-centered CVH, the association between change in person-centered CVH over 5 years and subsequent risk of CVD was assessed in the full sample recruited since 2009. The data retrieval, management, and statistical analyses were carried out using SAS Enterprise Guide® 7.1, Oracle® 12.2.0., and Stata® 17.0 (StataCorp, Tex).
Results
Main characteristics
The study population included 18,714 adult CVD-free participants (Fig. 1), average age 51 years, 73% women. Table 2 summarizes the sample characteristics according to the levels of measured and person-centered CVH. In both measured and person-centered CVH, people with higher CVH were more frequently younger (43.58, 48.60 years), women (77.59%, 75.63%), of higher educational attainment (44.72%, 38.94%), drinking less alcohol (6.90 gm/day, 5.56 gm/day), and less frequently having CVD family history (26.98%, 34.29%). The percentages of ideal person-centered and measured LS7 metrics are reported in Supplementary Table S1.
Concordance between measured and person-centered CVH
As reported in Table 3, the concordance between low, intermediate, and high person-centered vs. measured CVH was high, with Gwet AC2 estimate of 0.92, 95% CI [0.91; 0.93], and Brennan and Prediger estimate of 0.87, 95% CI [0.86; 0.88]. The sensitivity and specificity of person-centered CVH were 96.94% and 72.83%, and the PPV and NPV were 41.52% and 99.17%, respectively; the diagnostic accuracy was 76.83% When examining the biological metrics separately (Table 4), the sensitivity ranged from 93.44% (hypertension) to 99.87% (T2D), and the specificity ranged from 15.37% (T2D) to 39.89% (hypertension), the PPV from 37.15% (hypercholesterolemia) to 88.14% (T2D) and the NPV from 79.60% (hypertension) to 95.95% (hypercholesterolemia) respectively. The diagnostic accuracy was 88.29%, 72.51%, and 46.86% for person-centered T2D, hypertension, and hypercholesterolemia, respectively.
Association between measured and person-centered CVH metrics with incident CVD
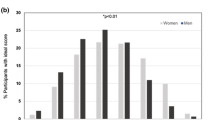
After a median follow-up time of 8.05 (25th;75th percentiles: 6.19; 9.30) years, 749 incident CVD events occurred, including 724 non-fatal CVD events, comprising 351 coronary heart disease CHD and 373 stroke events, yielding an incidence rate of 5.31 per 1000 person-years, 95% CI [4.92; 5.72]. Kaplan- Meier curves suggest that the CVD incidence rate decreased progressively from low to high person-centered CVH (Fig. 2. Panel A, p for log-rank trend < 0.05), and measured CVH (Fig. 2. Panel B, p for log-rank trend < 0.05) levels. In multivariable models, there was a 7% (HR = 0.93, 95% CI [0.88; 0.99]) and 13% (HR = 0.87, 95% CI [0.83; 0.92]) risk reductions of CVD per additional increase in measured and person-centered ideal LS7 metrics, respectively (Table 5). Also, there was a 29% (HR = 0.71, 95% CI [0.53; 0.95]) and a 40% (HR = 0.60, 95% CI [0.49; 0.74]) risk reduction of CVD events for high (5 ideal metrics or more) versus low (2 ideal metrics or less) category of measured and person-centered CVH, respectively (Table 5). The findings suggest no sex modification effect between person-centered or measured CVH and incident CVD (Fig. 3), and no educational attainment level (p for interaction = 0.60 and 0.20) or occupational category moderating effect (p for interaction = 0.85 and 0.60), not shown.
Hazard ratios and 95% confidence intervals for incident CVD per unit increase in ideal measured and person-centered CVH metrics, overall and by sex. Hazard ratios and 95% confidence intervals were estimated by Cox proportional models using age as a timescale, stratified by birth year (5-year intervals), and adjusted for baseline sex (when appropriate), cohabitation status, educational attainment, occupational category, alcohol use, and CVD family history.
Additional analyses results
The results of additional analyses are reported in Supplementary Table S2. The estimates remained consistent with those reported in the main analysis after excluding first-year incident CVD (n = 139 events), considering the number of ideal biological metrics only (range 0–3), considering the complete case analysis, or accounting for competing risk by non-CVD mortality. Also, measured and person-centered CVH were equally and inversely related to non-CVD mortality (n = 169 deaths). Moreover, the estimated population attributable preventive fraction (PPF) is 29.37%, 95% CI [7.04; 46.33] and 15.54%, 95% CI [5.52; 24.49] for the measured and person-centered CVH, respectively.
The change analysis of person-centered CVH included 126,871 participants evaluated at baseline (2009 to 2014) and after 5 years, excluding CVD events in the interval. Overall, 56.04% maintained their CVH level at the 2 time points, including 3.54% at low CVH (0–2 ideal LS7 metrics), 59.29% at intermediate CVH (3–4 ideal LS7 metrics), and 37.17% at high CVH (5–7 ideal LS7 metrics). Secondly, 25.61% declined in CVH, including 67.90% and 25.39% of participants initially with intermediate and high CVH. Thirdly, 18.36% improved their CVH, including 20.40% and 42.89% of participants initially with low and intermediate CVH. Over a median follow-up of 6.98 years after the second CVH evaluation, 955 CVD events occurred. The risk of CVD decreased by 13% per increase in ideal person-centered LS7 metric independently of the baseline number of ideal person-centered LS7 metrics (Supplementary Table S3).
Discussion
In this prospective e-cohort study conducted in 18,714 adult CVD-free adults, we report for the first time the results of a head-to-head comparison of person-centered CVH vs. measured CVH regarding their concordance and their respective associations with incident CVD in the same sample. The findings suggest that person-centered CVH data is a reliable approximate of measured CVH, which may have important implications for the spread of primordial prevention in the community.
Several points indicate that person-centered CVH is a reliable approximate of measured CVH. Firstly, concordance between person-centered and measured CVH was high, both for the global CVH and for most (biological) metrics. Still, person-centered data on ideal cholesterol status (i.e. non-hypercholesterolemic) exhibited the least concordance with its measured counterpart (i.e. ideal total serum cholesterol). Insufficient surveillance and public awareness of hypercholesterolemia in middle-aged adults may contribute to the lower concordance of the person-centered and measured hypercholesterolemia compared to hypertension and T2D21,22. So far, only one previous cross-sectional study conducted in 8,943 middle-aged Brazilians has compared person-centered and measured CVH23. In that study, the sensitivity and specificity of the person-centered CVH were 92.4 and 48.5%, compared to 93.6 and 72.1% in the current study. Direct comparisons between the two studies are difficult owing to the differences in high CVH level definition, ≥ 4 ideal metrics vs. ≥ 5 ideal metrics in the current study. We extended the previous study results to twice the number of participants, by using weighted concordance analysis, allocating more weight to misclassifications in higher CVH categories, and conducting a concordance analysis for each biological CVH metric.
Second, as for the measured CVH, the person-centered CVH was associated with a risk reduction of CVD per additional increase in ideal LS7 metric. Of note, however, the risk reduction per additional ideal metric was overestimated compared to the measured CVH (13% vs. 7%). Such difference is likely due to misclassification of person-centered biological LS7 metrics, since behavioral LS7 metrics are common to both person-centered and measured CVH. This is illustrated in the supplementary analyses, comparing the associations between person-centered and measured biological CVH with incident CVD. The findings on person-centered CVH and incident CVD are nevertheless consistent with those reported in postmenopausal women, even though no comparison with measured CVH was conducted in that study24.
Lastly, change in person-centered CVH (i.e. increase in the number of ideal metric) is associated with CVD risk reduction independent from baseline CVH, in accordance to what has been previously found for the change in measured CVH in other studies25.
The findings may have global health implications for primordial prevention. The results of the concordance analysis and the head-to-head comparison of the associations with CVD events suggest that person-centered CVH may represent an acceptable alternative to measured CVH. A person-centered CVH method has advantages over measured CVH defined by clinical examination and laboratory-based biomarkers: it is economical and more feasible to monitor, both on the individual and mass levels. Additionally, person-centered CVH may facilitate self-evaluation of CVH in the population, which may help incentivize the participation of individuals in their CVD risk assessment and prevention, and empower their decision to adopt healthier behaviors, i.e. participatory medicine26. In this context, the advent of wearable devices that measure physical activity, heart rate, or sleep patterns represents opportunities to self-evaluate CVH and endorse active person-centered CVH monitoring. From the health care provider’s point of view, a person-centered CVH may facilitate closer monitoring of CVH in the population, and screening of vulnerable sub-populations, and it may also help launch appropriate interventions to target CVH population prevention goals. For instance, in the secondary prevention setting, e-health interventions have been proposed to improve chronic disease outcomes27,28. Also, self-monitoring and telemonitoring have been suggested to be cost-effective management approaches for BP reduction in the UK29. Similar approaches might be extended to primordial and primary CVD prevention. Furthermore, person-centered CVH might be particularly useful in low and middle-resource settings or medically underserved high-income regions, where access to preventive cardiovascular services is challenging. However, future studies should evaluate the concordance of person-centered vs. measured CVH in LMICs or undeserved high-income areas finally, we estimated that 15.54% of CVD events could be prevented under the hypothesis that all of the population would acquire an ideal person-centered CVH. However, these results represent a conservative estimate, approximately half of that derived from the measured CVH in the current study population and the US adult population30.
Limitations
The high concordance between person-centered and measured CVH may be in part due to the inclusion of more participants who are women and of higher socioeconomic level compared to the general French population. Therefore, study participants may have been more aware of their hypertensive or diabetic statuses than the general population. However, it is unlikely to have impacted the comparative associations between person- centered or measured CVH and CVD events, since direct comparison of person-centered and measured CVH was conducted for the same individuals. The over-representation of women in this study may also have contributed to not detecting sex interactions in the associations between person-centered or measured CVH and CVD, despite prior evidence in sex-difference in the CVH distribution31. Measured biological LS7 metrics were assessed once, precluding the estimation of the concordance of the measured vs. person-centered CVH change and their respective associations with incident CVD. Despite model adjustment for potential confounders, residual confounding cannot be ruled out when comparing the association of measured and person-centered CVH with incident CVD. At the time of the study, the participants’ ethnicity data were not available. The present study was conducted in a high-resource setting, future studies should examine the relevance of person-centered CVH in different global health contexts.
Conclusions
Person-centered CVH represents a reliable alternative to measured CVH and therefore might be useful for monitoring population CVH, a global health priority, particularly in underserved HIC areas and LMICs.
Data availability
Researchers from public institutions can submit a collaboration request to Dr. Mathilde Touvier via collaboration@etude-nutrinet-sante.fr, including information on the institution and a brief description of the project.All requests will be reviewed by the steering committee of the NutriNet-Santé study. If the collaboration is accepted, a data access agreement will be necessary, and appropriate authorizations from competent administrative authorities may be needed. In accordance with existing regulations, no personal data will be accessible. The analyses code can be requested from the authors.
Abbreviations
- CVH:
-
Cardiovascular health
- LS7:
-
Life’s simple 7
- LMICs:
-
Low and middle-income countries
- BMI:
-
Body mass index
- T2D:
-
Type 2 diabetes mellitus
- CVD:
-
Cardiovascular disease
- SNIIRAM:
-
The medico-administrative databases of the national health insurance (France)
- BP:
-
Blood pressure
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
Unal, B., Critchley, J. A. & Capewell, S. Explaining the decline in coronary heart disease mortality in england and wales between 1981 and 2000. Circulation 109, 1101–1107 (2004).
Yusuf, S. et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N. Engl. J. Med. 371, 818–827 (2014).
Weintraub, W. S. et al. Value of primordial and primary prevention for cardiovascular disease. Circulation 124, 967–990 (2011).
Lloyd-Jones, D. M. et al. Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation 121, 586–613 (2010).
Ramírez-Vélez, R. et al. Ideal cardiovascular health and incident cardiovascular disease among adults: A systematic review and meta-analysis. Mayo Clin. Proc. 93, 1589–1599 (2018).
Younus, A. et al. A systematic review of the prevalence and outcomes of ideal cardiovascular health in US and Non-US populations. Mayo Clin. Proc. 91, 649–670 (2016).
Rosengren, A. et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: The Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob. Health 7, e748–e760 (2019).
Håkansson Eklund, J. et al. “Same same or different?” A review of reviews of person-centered and patient-centered care. Patient Educ. Couns. 102, 3–11 (2019).
Hercberg, S. et al. The Nutrinet-Santé Study: A web-based prospective study on the relationship between nutrition and health and determinants of dietary patterns and nutritional status. BMC Public Health 10, 242 (2010).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395 (2003).
Lassale C, Péneau S, Touvier M, Julia C, Galan P, Hercberg S, Kesse-Guyot E. Validity of Web-Based Self-Reported Weight and Height: Results of the Nutrinet-Santé Study. Journal of Medical Internet Research [Internet]. 2013 [cited 2022 Mar 21]; 15 https://www.ncbi.nlm.nih.gov/sites/ppmc/articles/PMC3742400/.
Touvier, M. et al. Comparison between web-based and paper versions of a self-administered anthropometric questionnaire. Eur. J. Epidemiol. 25, 287–296 (2010).
Touvier, M. et al. Comparison between an interactive web-based self-administered 24 h dietary record and an interview by a dietitian for large-scale epidemiological studies. Br. J. Nutr. 105, 1055–1064 (2011).
Lassale, C. et al. Validation of a Web-based, self-administered, non-consecutive-day dietary record tool against urinary biomarkers. Br. J. Nutr. 113, 953–962 (2015).
Lassale, C. et al. Correlations between fruit, vegetables, fish, vitamins, and fatty acids estimated by web-based nonconsecutive dietary records and respective biomarkers of nutritional status. J. Acad. Nutr. Diet. 116, 427-438.e5 (2016).
Xanthakis, V. et al. Ideal cardiovascular health. Circulation 130, 1676–1683 (2014).
Gwet, K. L. Computing inter-rater reliability and its variance in the presence of high agreement. Br. J. Math. Stat. Psychol. 61, 29–48 (2008).
Wongpakaran, N., Wongpakaran, T., Wedding, D. & Gwet, K. L. A comparison of Cohen’s Kappa and Gwet’s AC1 when calculating inter-rater reliability coefficients: A study conducted with personality disorder samples. BMC Med. Res. Methodol. 13, 61 (2013).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94, 496–509 (1999).
Lu, Y. et al. Comparison of prevalence, awareness, treatment, and control of cardiovascular risk factors in China and the United States. J. Am. Heart Assoc. 7, e007462 (2018).
Lee, Y. et al. Serum cholesterol concentration and prevalence, awareness, treatment, and control of high low-density lipoprotein cholesterol in the korea national health and nutrition examination surveys 2008–2010: Beyond the tip of the Iceberg. J. Am. Heart Assoc. 3, e000650 (2014).
Moreira, A. D., Gomes, C. S., Machado, Í. E., Malta, D. C. & Felisbino-Mendes, M. S. Cardiovascular health and validation of the self-reported score in Brazil: Analysis of the National Health Survey. Cien Saude Colet 25, 4259–4268 (2020).
Foraker, R. E. et al. Cardiovascular health and incident cardiovascular disease and cancer: The women’s health initiative. Am. J. Prev. Med. 50, 236–240 (2016).
van Sloten, T. T. et al. Association of change in cardiovascular risk factors with incident cardiovascular events. JAMA 320, 1793–1804 (2018).
Springer, M. V. & Skolarus, L. E. Community-based participatory research. Stroke 50, e48–e50 (2019).
Renzi E, Gasperini G, Baccolini V, Marzuillo C, De Vito C, Villari P, Massimi A. The impact of e-Health interventions on promoting Self-Care in Chronic Patients: an Umbrella Review. European Journal of Public Health. 2020;30:ckaa165.1104.
Beratarrechea, A. et al. The impact of mobile health interventions on chronic disease outcomes in developing countries: A systematic review. Telemed. J. E Health 20, 75–82 (2014).
Monahan, M. et al. Cost-effectiveness of telemonitoring and self-monitoring of blood pressure for antihypertensive titration in primary care (TASMINH4). Hypertension 73, 1231–1239 (2019).
Bundy, J. D. et al. Estimated impact of achieving optimal cardiovascular health among US adults on cardiovascular disease events. J. Am. Heart Assoc. 10, e019681 (2021).
Simon, M. et al. Sex disparities in ideal cardiovascular health. Heart 103, 1595–1601 (2017).
Acknowledgements
Due thanks to Younes Esseddik (IT manager), Thi Hong Van Duong, Régis Gatibelza, Jagatjit Mohinder and Aladi Timera (computer scientists); Fabien Szabo de Edelenyi, Julien Allegre, Nathalie Arnault, Laurent Bourhis, Nicolas Dechamp (data-manager/statisticians); Cédric Agaësse, Alexandre De Sa, Rebecca Lutchia (dietitians), Merveille Kouam (health event validator); Maria Gomes (Nutrinaut support); Nathalie Druesne-Pecollo (operational coordinator) for their technical contribution to the NutriNet-Santé study. We thank all the volunteers of the NutriNet-Santé study.
Funding
The NutriNet-Santé study was supported by the following public institutions: the Ministry of Health, Public Health France, the National Institute of Health and Medical Research (INSERM), the National Institute of Agricultural, Food and Environmental Research (INRAE), the National Conservatory of Arts and Crafts (CNAM) and Université Sorbonne Paris Nord. O.D. was supported by a grant from the Foundation for Medical Research (FRM, grant # ECO202106013757). C. D. was supported by a grant from the French National Cancer Institute (INCa, grant #2019–158). The funders had no role in the study design, the collection, analysis, data interpretation, report writing, and the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
L.F., M.D.T., E.K.G., P.G., S.H., and M.T. contributed to the NutriNet-Santé study conceptualization, data curation, and funding acquisition. O.D. contributed to the methodology, formal analysis, writing the original draft, visualization and revised the manuscript based on comments from T.V.S., C.D., L.F., E.K.G., M.T. and J.P.E. J.P.E. and M.T. contributed to project administration and resources. O.D., T.V.S., R.C., C.D., L.F. M.D.T., X.J., E.K.G., P.G., S.H., M.T., and J.P.E. contributed to reviewing the manuscript. J.P.E coordinated the project. All authors reviewed and approved the manuscript for submission. All authors had the final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deraz, O., Van Sloten, T., Climie, R. et al. Person-centered and measured life’s simple 7 cardiovascular health concordance and association with incident cardiovascular disease. Sci Rep 13, 5247 (2023). https://doi.org/10.1038/s41598-023-32219-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-32219-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.