Abstract
Delirium is a common, serious, and often preventable neuropsychiatric emergency mostly characterized by a disturbance in attention and awareness. Systemic insult and inflammation causing blood–brain-barrier (BBB) damage and glial and neuronal activation leading to more inflammation and cell death is the most accepted theory behind delirium's pathophysiology. This study aims to evaluate the relationship between brain injury biomarkers on admission and delirium in acutely ill older patients. We performed a prospective cohort study which analyzed plasma S100B levels at admission in elderly patients. Our primary outcome was delirium diagnosis. Secondary outcomes were association between S100B, NSE and Tau protein and delirium diagnosis and patients’ outcomes (admissions to intensive care, length of hospital stay, and in-hospital mortality). We analyzed 194 patients, and 46 (24%) developed delirium, 25 on admission and 21 during hospital stay. Median of S100B at admission in patients who developed delirium was 0.16 and median was 0.16 in patients who didn’t develop delirium (p: 0.69). Levels S100B on admission did not predict delirium in acutely ill elderly patients.
Trial registration: The study was approved by the local institutional review board (CAPPESq, no. 77169716.2.0000.0068, October 11, 2017) and registered in Brazilian Clinical Trials Registry (ReBEC, no. RBR-233bct).
Similar content being viewed by others
Introduction
Delirium is a common, serious, and often preventable neuropsychiatric emergency that is characterized by a disturbance in attention and awareness1,2. It represents an acute and severe brain dysfunction, and it is associated with increased hospital and Intensive Care Unit (ICU) length of stay, persistent cognitive decline, and increased mortality3.
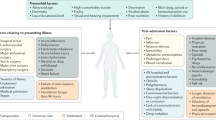
Systemic insult and inflammation causing blood–brain-barrier (BBB) damage, and glial and neuronal activation leading to more inflammation and cell death is the most accepted theory behind delirium's pathophysiology4. In addition to cognitive tests5, several plasma biomarkers and cytokines have been previously studied for delirium diagnosis6. Promising biomarkers are S100 calcium binding protein B (S100B) which is expressed by astrocytes and not only reflects cell death, but also BBB integrity and permeability; neuron-specific enolase (NSE) an isoenzyme highly specific to neurons, a biomarker of hypoxic brain damage and a marker of poor outcome after cardiac arrest; and Tau protein which maintains microtubules stability in axons and relates to forms of cognitive-impairment7,8,9. There are, however, many gaps in the literature to fully understand how these molecules interact and how they are associated with delirium occurrence10,11. Specifically, data on S100B are conflicting, since some studies have shown that patients with delirium had a higher serum level of S100B, and other studies have shown no association between this protein and delirium or other adverse outcomes10. Furthermore, there are no studies evaluating the association between inflammatory and brain-related biomarkers with Emergency Department (ED) delirium11,12.
Our primary goal was to evaluate S100B levels on admission and their association with delirium occurrence in acutely ill older adults. We also aimed to evaluate the association between S100B, NSE, Tau and cytokine panel (IL-1B, IL-4, IL-10, TNF-α and IFN-γ) with delirium. We hypothesized that increased levels of S100B, NSE and Tau would be associated with an increased risk of delirium.
Methods
Design, setting, and population
We prospectively screened patients admitted to the ED of a tertiary university hospital between September 30, 2019, and March 17, 2020. Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo is a 2200-bed hospital located in Sao Paulo, Brazil, dedicated to the care of high-complexity medical and surgical patients. This report is published in accordance with the STROBE guideline and recommendations13.
Eligible patients were 65 years or older and hospitalized for less than 24 h. We excluded candidates according to the following criteria: (a) previous hospitalization in the 30 days preceding admission; (b) hospitalization for end-of-life care; and (c) expected hospital discharge in 48 h or less.
The study was approved by the local institutional review board (Comissão de Ética para Análise de Projetos de Pesquisa do HCFMUSP [CAPPESq], no. 77169716.2.0000.0068, October 11, 2017) and registered in Brazilian Clinical Trials Registry [(ReBEC), no. RBR-233bct)]. We obtained written informed consent from all participants or their legal representatives and used REDCap® (Research Electronic Data Capture) resources to secure and manage all study-related data14.
Baseline characteristics
Trained investigators completed the study interviews and assessments using standardized REDCap forms. We collected baseline sociodemographic and clinical data including age, sex, literacy level, medical history, Charlson comorbidity index (Charlson)15, frailty status using the FRAIL scale16, polypharmacy (chronic use of five or more medications), and admission diagnoses. We performed functional and cognitive assessments using the activities of daily living (ADL) and the 10-point Cognitive Screener (10-CS) scales, respectively17.
Delirium assessments
We completed the Confusion Assessment Method (CAM) algorithm5 twice daily to detect delirium. We performed the first assessment in the ED, and the following evaluations in Wards or ICUs, according to patients’ allocation. Our standardized interview protocol incorporated a brief neuropsychiatric anamnesis, cognitive screening (10-CS), attention testing (days of the week backwards and vigilance A test)18, level of consciousness assessment (Richmond Agitation and Sedation Scale [RASS])19, and electronic medical record revisions20. Delirium episodes were considered resolved if the patient was non-delirious for two consecutive evaluations.
Although our raters attended training sessions before the study initiation, which included simulations and bedside evaluations, and we achieved high interrater reliability levels for CAM-based delirium diagnosis (> 95%), whenever our raters were uncertain regarding the presence of delirium, two experienced physicians (JCGA and FBG) repeated or reviewed the assessments to confirm the final diagnosis.
Blood samples
We collected the following laboratory tests upon study inclusion: blood count, C-reactive protein, platelets, creatinine, blood urea nitrogen, bilirubin, inflammatory biomarkers (IL-1B, IL-4, IL-10, INF-g and TNF-α and neuronal injury biomarkers (S100B, Neuron Specific Enolase and Tau protein).
Three registered nurses performed the sampling while patients were in the ED, which consisted of 30 ml of blood collected by venipuncture. Blood samples used for brain injury biomarkers analysis were immediately centrifuged for 10 min, and plasma was preserved at − 20 °C for up to 48 h before being transferred to a − 80 °C freezer for long-term storage and further processing.
We measured cytokine plasma levels using the magnetic bead immunoassay Milliplex® and the MAGPIX® System (Merck Millipore, USA).
The sampling procedures were performed on inclusion (S1) and repeated 72 h after inclusion (S2)21. Participants who were discharged or died within 72 h of admission, or refused to provide additional samples, were not punctured again. We obtained a third sample (S3) from participants who converted either from a negative to positive CAM (incident delirium) or from a positive to negative CAM (delirium resolution) after S2 (Fig. 1).
Statistical analyses
Our primary outcome was the overall occurrence of delirium based on the CAM criteria. Secondary outcomes were association between S100B, NSE and Tau protein and delirium diagnosis and patients’ outcomes (admissions to intensive care, length of hospital stay, and in-hospital mortality).
We used a convenience sample, which limited the total number of enrolled patients22. Despite our ED providing medical care to 800 elderly patients monthly and 30% of them being eligible for hospitalization, most of these patients are transferred from other less complex hospitals and had been hospitalized for more than 24 h at the time of recruitment. Therefore, 200 patients were predicted to be enrolled for 6 months, with the expectation of 7–10 eligible patients per week. We finished our recruitment a month ahead of schedule because of the beginning of the COVID-19 pandemic.
All enrolled patients were included in the analysis of primary and secondary outcomes on an intention-to-treat basis. We initiated the analysis using the Shapiro–Wilk test to determine which variables were normally and non-normally distributed, especially results of S100B. Then, we performed analysis according to delirium occurrence using unpaired t-tests or Kruskal–Wallis for normal and non-normal variables respectively, and categorical variables were analyzed using Pearson’s χ2 test.
All analyses were performed with Stata software, version 10.
Ethics approval and consent to participate
This study was approved by the São Paulo University’s Research Ethics Committee Comissão de Ética para Análise de Projetos de Pesquisa do HCFMUSP (CAPPESq), no. 77169716.2.0000.0068 on October 11, 2017, and registered in Brazilian Clinical Trials Registry (ReBEC, no. RBR-233bct). All participants or legal representatives provided written informed consent prior to enrolment in the study.
Results
Patient characteristics
We included 194 participants (Fig. 2 and Table 1). They were mostly female (60.52%), had a mean age of 74.7 (± 7.4) years, and were hospitalized for a median 8 (4–15) days. The main cause of admission was sepsis (49 patients, 25%), followed by cardiovascular disease (20%), cerebrovascular disease (14%) and abdominal surgical conditions (10%). Overall, 72% were referral to ward, and 28% of our sample required ICU admission, with a stay of 4 (2–7) days, 22% required invasive mechanical ventilation and 14% died. (Supplementary Appendix: Outcomes). We detected delirium in 46 individuals (24%)—25 on admission (prevalent delirium) and 21 during hospital stay (incident delirium). Delirium patients were significantly older and had more history of cerebrovascular accident or dementia. Furthermore, delirium patients had longer days of hospitalization (mean 10 vs 7, p = 0.0212), increased need of ICU care (41.3% vs 24.3%, p = 0.0256), and increased mortality (32.61% vs 7.43%, p < 0.0001) (Table 1).
Association of S100B and other biomarkers with delirium occurrence
Plasma S100B and other biomarkers concentrations at ED admission were not associated with an increased risk of delirium diagnosis during hospitalization (Table 2) (Supplementary Appendix: Results Biomarkers).
In a post-ROC analysis, only patients at risk of developing delirium were evaluated (i.e., those without delirium at enrollment), and 25 patients admitted with CAM positive were excluded. Table 3 compares plasma levels of S100B, NSE and Tau between patients who developed and those who did not develop delirium during hospitalization.
Association of S100B and other biomarkers with delirium diagnosis
Plasma S100B, NSE and Tau were measured before and during delirium in 21 patients with delirium during hospital stay (delirium incidence). Levels did not differ significantly in the two groups (Table 4).
Association of S100B and other biomarkers with outcomes
Plasma S100B, NSE and Tau protein levels were not significantly associated with outcomes (Table 5).
Discussion
Our study demonstrated that serum S100B on admission were not associated with delirium in acutely ill older patients.
Previous studies have demonstrated an association between plasma levels of S100B and delirium occurrence23,24 and duration25 in ICU patients. The mechanism behind the increase of S100B in blood is uncertain. Authors have hypothesized that cerebral or extra-cerebral cellular damage caused by multiple different mechanisms (such as hypoxia) could lead to neuroinflammation and subsequent increased permeability of the BBB, ultimately upregulating S100B production by astrocytes26. These results are not unanimous, and previous studies with ICU patients did not confirm the association between plasma levels of S100B and the occurrence of delirium27.
Our results are consistent with McNeil et al. in Delineate study, which did not demonstrate an association between serum S100B levels and delirium duration12. We consider that delirium’s pathogenesis is multifactorial, probably include systemic inflammation and endothelial dysfunction, but this association may be modified by baseline patient’s conditions.
On the other hand, van Munster et al. demonstrated that plasma levels of S100B were higher in critically ill elderly patients during and after delirium than in patients without delirium28. These results were not reproduced in our patients. The authors reported that S100B levels remain high after delirium, which could indicate an active stimulation of astrocytes or an increase of BBB’s permeability. It is worth mentioning that they did not assess the role of S100B in delirium occurrence and measurements S100B occurred 48 h after admission.
Interestingly, van Munster also studied the role of S100B in predicting delirium, and demonstrated that among patients undergoing surgery, S100B levels were higher in those who developed delirium than in patients who did not29. These findings were not reproduced by the same author when she evaluated the preoperative role of S100B in cerebrospinal fluid (CSF)30.
Our study does not demonstrate a statistically significant association between plasma NSE or Tau levels at admission in ED and occurrence of delirium during hospitalization. As far as we are aware, this is the first study to analyze these proteins while patients were in the ED. Our findings differ from previous studies that demonstrated this association in clinical and surgical patients in the ICU setting24,27,31,32.
Limitations
Several limitations need to be acknowledged. First, S100B values were measured in peripheral blood and may not necessarily correspond to values in the brain. Under normal conditions, serum S100B content is lower than that in CSF33. However, we were searching a feasible and reproducible serum biomarker. Second, there were a sizeable number of patients who were not enrolled during the study period. Our research team recruited patients daily in the morning, however, some patients stayed a few hours in the ED before being transferred to wards or ICUs. Our sample size could associate our results with a type 2 error. Nevertheless, with a sample size of almost 200 patients, we believe that the effect size would be too small and even irrelevant to had not been established in this pragmatic ED study. Finally, probably not all delirium results from neuronal injury or BBB damage. There are other causes of delirium, including sepsis-associated encephalopathy and drug withdrawal. This means that S100B may not raise in all delirium patients and further research should explore the association between S100B, NSE, Tau and subsequent cognitive decline.
Conclusions
S100B and other brain injury biomarkers measured on admission are not associated with delirium in acutely ill older patients. Future studies with others and serial biomarker measurements throughout delirium’s course and long-term cognitive outcome are needed to better clarify these relationships.
Data availability
All data generated or analyzed during this study are included in this published article (Supplementary files “Results Biomarkers” and “Outcomes”).
Abbreviations
- 10-CS:
-
10-Point Cognitive Screener
- ADL:
-
Activities of daily living
- BBB:
-
Blood–brain-barrier
- CAM:
-
Confusion assessment method
- CSF:
-
Cerebrospinal fluid
- ED:
-
Emergency department
- ICU:
-
Intensive care unit
- NSE:
-
Neuron-specific enolase
- RASS:
-
Richmond Agitation and Sedation Scale
- REDCap:
-
Research Electronic Data Capture
- S100B:
-
S100 calcium binding protein B
References
Oliveira, J. S. L. et al. Risk factors for delirium in older adults in the emergency department: A systematic review and meta-analysis. Ann. Emerg. Med. 78, 549–565 (2021).
Barron, E. A. & Holmes, J. Delirium within the emergency care setting, occurrence and detection: A systematic review. Emerg. Med. J. 30(4), 263–268. https://doi.org/10.1136/emermed-2011-200586 (2013).
Inouye, S. K., Westendorp, R. G. & Saczynski, J. S. Delirium in elderly people. Lancet 383(9920), 911–922 (2014).
Maldonado, J. R. Neuropathogenesis of delirium: Review of current etiologic theories and common pathways. Am. J. Geriatr. Psychiatry 21(12), 1190–1222 (2013).
Inouye, S. K. et al. Clarifying confusion: The confusion assessment method: A new method for detection of delirium. Ann. Intern. Med. 113(12), 941–948. https://doi.org/10.7326/0003-4819-113-12-941 (1990).
Smith, R. J. et al. Cytokine profiles in intensive care unit delirium. Acute Crit. Care. 37, 415–428 (2022).
Bialowas-McGoey, L. A., Lesicka, A. & Whitaker-Azmitia, P. M. Vitamin E increases S100B-mediated microglial activation in an S100B-overexpressing mouse model of pathological aging. Glia 56(16), 1780–1790 (2008).
Daubin, C. et al. Serum neuron-specific enolase as predictor of outcome in comatose cardiac-arrest survivors: A prospective cohort study. BMC Cardiovasc. Disord. 11, 48. https://doi.org/10.1186/1471-2261-11-48 (2011).
Parker, M. et al. Cohort analysis of the association of delirium severity with cerebrospinal fluid amyloid-tau-neurodegeneration pathologies. J. Gerontol. A Biol. Sci. Med. Sci. 77(3), 494–501 (2022).
Macedo, R. C. et al. Lack of association of S100β and neuron-specific enolase with mortality in critically ill patients. Braz. J. Psychiatry 35(3), 267–270 (2013).
Gao, Y., Duan, J., Ji, H. & Lu, W. Levels of S100 calcium binding protein B (S100B), neuron-specific enolase (NSE), and cyclophilin A (CypA) in the serum of patients with severe craniocerebral injury and multiple injuries combined with delirium transferred from the ICU and their prognostic value. Ann. Palliat. Med. 10(3), 3371–3378 (2021).
McNeil, J. B. et al. Plasma biomarkers of inflammation, coagulation, and brain injury as predictors of delirium duration in older hospitalized patients. PLoS ONE 14(12), e0226412 (2019).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 370(9596), 1453–1457 (2007).
Harris, P. A. et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 95, 103208. https://doi.org/10.1016/j.jbi.2019.103208 (2019).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 40(5), 373–383. https://doi.org/10.1016/0021-9681(87)90171-8 (1987).
Morley, J. E., Malmstrom, T. K. & Miller, D. K. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J. Nutr. Health Aging. 16(7), 601–608. https://doi.org/10.1016/j.physbeh.2017.03.040 (2012).
Apolinario, D. et al. Using temporal orientation, category fluency, and word recall for detecting cognitive impairment: The 10-point cognitive screener (10-CS). Int. J. Geriatr. Psychiatry 31(1), 4–12. https://doi.org/10.1002/gps.4282 (2016).
Tieges, Z., Brown, L. J. E. & MacLullich, A. M. J. Objective assessment of attention in delirium: a narrative review. Int. J. Geriatr. Psychiatry 29(12), 1185–1197. https://doi.org/10.1002/gps.4131 (2014).
Sessler, C. N. et al. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 166(10), 1338–1344. https://doi.org/10.1164/rccm.2107138 (2002).
Krewulak, K. D. et al. Adaptation and validation of a chart-based delirium detection tool for the ICU (CHART-DEL-ICU). J. Am. Geriatr. Soc. 69(4), 1027–1034. https://doi.org/10.1111/jgs.16987 (2021).
Wu, L. et al. The dynamic change of serum S100B levels from day 1 to day 3 is more associated with sepsis-associated encephalopathy. Sci. Rep. 10(1), 7718. https://doi.org/10.1038/s41598-020-64200-3 (2020).
Bacchetti, P., McCulloch, C. E. & Segal, M. R. Simple, defensible sample sizes based on cost efficiency. Biometrics 64(2), 577–585. https://doi.org/10.1111/j.1541-0420.2008.01004_1.x (2008).
Pfister, D. et al. Cerebral perfusion in sepsis-associated delirium. Crit Care. 12(3), R63. https://doi.org/10.1186/cc6891 (2008).
Mietani, K. et al. Elevated neuron-specific enolase level is associated with postoperative delirium and detection of phosphorylated neurofilament heavy subunit: A prospective observational study. PLoS ONE 16(11), e0259217. https://doi.org/10.1371/journal.pone.0259217 (2021).
Khan, B. A. et al. S100 calcium binding protein B as a biomarker of delirium duration in the intensive care unit—An exploratory analysis. Int. J. Gen. Med. 6, 855–861. https://doi.org/10.2147/IJGM.S51004 (2013).
Townend, W. et al. Rapid elimination of protein S-100B from serum after minor head trauma. J. Neurotrauma 23(2), 149–155. https://doi.org/10.1089/neu.2006.23.149 (2006).
Grandi, C. et al. Brain-derived neurotrophic factor and neuron-specific enolase, but not S100β, levels are associated to the occurrence of delirium in intensive care unit patients. J. Crit Care. 26(2), 133–137. https://doi.org/10.1016/j.jcrc.2010.10.006 (2011).
van Munster, B. C. et al. Serum S100B in elderly patients with and without delirium. Int. J. Geriatr. Psychiatry 25(3), 234–239. https://doi.org/10.1002/gps.2326 (2010).
van Munster, B. C. et al. Cortisol, interleukins and S100B in delirium in the elderly. Brain Cogn. 74(1), 18–23. https://doi.org/10.1016/j.bandc.2010.05.010 (2010).
van den Boogaard, M. et al. Biomarkers associated with delirium in critically ill patients and their relation with long-term subjective cognitive dysfunction; indications for different pathways governing delirium in inflamed and noninflamed patients. Crit. Care 15(6), R297. https://doi.org/10.1186/cc10598 (2011).
McKay, T. B. et al. Tau as a serum biomarker of delirium after major cardiac surgery: A single centre case-control study. Br. J. Anaesth. 129(1), e13–e16. https://doi.org/10.1016/j.bja.2022.04.002 (2022).
Ballweg, T. et al. Association between plasma tau and postoperative delirium incidence and severity: A prospective observational study. Br. J. Anaesth. 126(2), 458–466. https://doi.org/10.1016/j.bja.2020.08.061 (2021).
Gonçalves, C. A., Leite, M. C. & Nardin, P. Biological and methodological features of the measurement of S100B, a putative marker of brain injury. Clin. Biochem. 41(10–11), 755–763. https://doi.org/10.1016/j.clinbiochem.2008.04.003 (2008).
Acknowledgements
The authors thank all the staff of the Emergency Department of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo.
Funding
This study was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), Grant #2016/14.566-4.
Author information
Authors and Affiliations
Contributions
J.C.G.A., F.B.G., T.J.A.S. and H.P.S. were involved in planning and supervised the work. J.C.G.A., S.M.L.R., F.B.G. and S.S.M.F. performed the measurements, J.C.G.A., A.A.S.P., L.O.J.S., L.M.S., and V.V.V. processed the experimental data, drafted the manuscript, and designed the figures and tales. LMGG performed the statistical analysis. All authors discussed the results and commented on the manuscript. All authors have read and approved the submission of the manuscript. The manuscript has not been published and is not being considered for publication elsewhere, in whole or in part, in any language. We obtained written informed consent, which included authorization for publication, from all participants or their legal representatives.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Alencar, J.C.G., Garcez, F.B., Pinto, A.A.S. et al. Brain injury biomarkers do not predict delirium in acutely ill older patients: a prospective cohort study. Sci Rep 13, 4964 (2023). https://doi.org/10.1038/s41598-023-32070-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-32070-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.