Abstract
As one of the most common neuropsychiatric complications after stroke, post-stroke depression can significantly affect the initiative of rehabilitation exercise and the rehabilitation of neurological function of patients. Virtual reality (VR) has been widely used in health-related fields in recent years. There is some evidence that VR-based interventions have benefits for depression. The aim of this study was to assess the effectiveness of VR-based intervention on depression in stroke patients. A total of 752 patients with stroke from 11 randomized controlled trials (RCTs) studies were included in this meta-analysis and the studies derived from seven electronic databases searched from database inception to August 2021. Different tools were used to measure depression. For continuous results, the standardized mean differences (SMDs) and 95% confidence intervals (CIs) were calculated to synthesize the effects. We assessed the risk of bias by using the Cochrane Collaboration criteria. The results showed that compared to the control group, VR-based interventions significantly decreased the depression scale score (SMD = − 0.75, 95% CI − 1.35, − 0.15). The meta-analysis indicated that VR-based intervention had a moderate effect on depression in stroke patients compared to control group. There was no evidence of potential publication bias as assessed by visual inspection of funnel plots in Egger and Begg tests. Substantial heterogeneity between studies was observed, meta-regression analysis showed that mean age might be the source of heterogeneity.
Similar content being viewed by others
Introduction
Stroke, as one of the most common neurological diseases resulting in permanent disability in adults1, has become a widespread health problem that affects people’s daily independent living2,3,4. For patients with stroke, the risk of impaired psychological health and depression increases5. About a third of stroke survivors experience post-stroke depression6. Patients with depression can lead to loss of interest and happiness, and produce anxiety, fear, hostility, sadness and anger7. For stroke patients, post-stroke depression not only delays the recovery of neurological deficits but also harms functional recovery and rehabilitation8,9,10,11, resulting in a decline in health-related quality of life12 and increasing mortality8. Such psychological states may lead to reduced motivation and low adherence to rehabilitation training5.
The current intervention methods mainly include drugs and psychotherapy. Studies have shown that up to 43% of patients with major depressive disorder may discontinue antidepressants due to adverse reactions during treatment13. So non-drug interventions are getting more and more attention. In recent years, VR-based intervention has been found to be effective for depression14,15,16. VR is a computer-generated high-tech simulation system that can create a sense of being there using computer electronic information simulation technology17. The characteristics of VR include non-immersion, immersion, interaction, and imagination18,19,20,21 etc. VR training, as a dynamic training method in line with daily life activities, can carry out active rehabilitation training from three levels of repetition, feedback, and motivation in a computer simulation of three-dimensional space. Therefore, this method can increase patients’ subjective initiative through multi-sensory feedback.
VR is widely used to treat people such as stroke21,22,23, chronic kidney24, and cerebral palsy25 to improve mobility, balance, or walking speed. The interventions based on VR are diverse, including virtual reality exposure therapy26,27, virtual reality cognitive behavioral therapy28,29, virtual reality sports games30, etc. Compared with traditional therapy, VR is more convenient to use, flexible and changeable in treatment content, more positive in users’ attitudes, and more pleasant in experience31. A variety of games can enable patients to have a deeper interest, and thus improve their subjective initiative resulting in various rehabilitation training being actively completed by patients32. As a result, a virtuous cycle can be formed, and their functional level is improved33.
Compared to traditional conventional rehabilitation training, VR is thought to reduce learning difficulty and make training safer34. However, the application of VR technology in the treatment of depression has not been promoted in clinical practice, and its effect is still being explored. While two22,23 meta-analyses have explored VR intervention for depression, they did not specify focus on the stroke population. Thus, the purpose of this study was to specifically analyze the effects of virtual reality-based intervention on depression in stroke patients.
Methods
Systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines35. A study protocol was registered at PROSPERO (CRD42020194244).
Literature inclusion and eligibility criteria
Studies were selected based on the following criteria: (a) study design must be randomized controlled trial (RCT); (b) the participants are stroke patients and older than 18 years old; (c) interventions in the experiment group were included all kinds of VR intervention, including VR games with exercise or VR psychotherapy. There was no restriction on the immersive levels of the VR environment displayed by the devices, such as a television, a screen, or a head-mounted display; (d) interventions in the control group are conventional rehabilitation training without VR, and not combined with other training. If there are both an active treatment group and a waiting-list group in the control group, the waiting-list group is selected; (e) depression is the primary outcome, and it must be measured. Useful data (e.g., sample size, mean and standard deviation) were reported in the published paper or could be retrieved by contacting the corresponding author of primary studies; (f) full-text articles published in peer-reviewed journals; (g) the number of participants including the experiment group and the control group is over 10; (h) the articles are published in Chinese or English.
Data sources and search strategy
Comprehensive systematic literature was performed using four English databases and three Chinese databases: Medline, PubMed, Web of Science, CINAHL, Chinese National Knowledge Infrastructure (CNKI), SinoMed (CBM), and Wanfang databases. Seven databases were searched from construction until August 2021. The following search items were adopted: virtual reality, VR, virtual environment, depression, depressive symptoms, depressive disorder, stroke, randomized controlled trial. Search strategies were included in Supplementary Appendix 1.
Study selection
Duplicate papers would be removed first before undertaking the screening. Two reviewers (HBL and ZHC) checked independently titles and abstracts of the retrieved articles according to the review criteria. Any disagreement was resolved by consensus and a third reviewer (SW) would arbitrate disagreements.
Data extraction
An electronic form was established to extract substantial contents, which includes the first author and publish year of the study, the sample size, nation, age, condition, pre-treatment and post-treatment score for depression, intervention period and frequency, the assessment tools for outcome measures, and interventions in experimental group and control group. Data extraction was carried out independently by two authors (HBL and ZHC). Any disagreement was be resolved by consensus and a third reviewer (YJ) was arbitrate disagreements.
Quality assessment
Based on the Cochrane Collaboration Risk of Bias tool36, the assessment of the methodological quality of included studies was assessed respectively independently by two review authors (HBL and ZHC) to evaluate the potential bias risk. Six perspectives pertained to bias risk including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, selective reporting, and other issues were also evaluated. Using this tool, the risk of bias was judged as ‘Low’, ‘High’, or ‘Unclear’.
Data analysis
Software stata 16.0 was used to analyze the outcome indicators of the included studies. The tools that measured depression were not always the same. For continuous results, the standardized mean difference (SMD) and 95% confidence intervals (CIs) were calculated. I2 was used to evaluate the heterogeneity in this study. When I2 ≤ 24%, there is no heterogeneity; 25% ≤ I2 ≤ 49%, low heterogeneity; 50% ≤ I2 ≤ 74%, mild heterogeneity; I2 ≥ 75%, high heterogeneity36. When I2 > 50%, the substantial heterogeneity was considered and a random effect model was selected, otherwise, a fixed effect model was selected for analysis33. Publication bias was explored using a funnel plot, Egger test37 and Begg test38. Sensitivity tests were also conducted to ensure the stability of the meta-analysis. Subgroups analyses explore potential differences and compare effect sizes between VR groups and control groups. Meta-regression was performed to explore the source of heterogeneity.
Results
Study selection
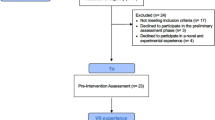
Figure 1 shows the study selection process. In total, 2214 records were identified by searching the databases, and 1282 potentially eligible articles were identified after removing duplicates. 61 studies were retrieved and reviewed by a more detailed assessment after screening the titles and abstract. After reviewing the full-text articles for eligibility, 11 studies were included.
Characteristics of included studies
Table 1 shows the characteristics of the included studies, in which the characteristics of experimental and control groups were shown in Supplementary Appendix 2. In this study, the 11 RCTs included were published between 2015 and 2021, including six English studies and five Chinese studies. The population sizes of the trials ranged from 21 to 145. All trials are recruited participants from the hospital who have been diagnosed with different types of stroke. Participants in all trials were not prescribed antidepressants. Among them, only one trial39 employed samples have been diagnosed with depression. The session duration of each intervention ranged from 15 to 60 min. One trial40 is a 2 weeks intervention period, five trials5,31,41,42,43 are a 4 weeks intervention period, two trials44,45 are a 6 weeks intervention period, and three trials39,46,47 are an 8 weeks intervention period. Six of the studies5,31,40,42,44,45 involved people with mild depression, five39,41,43,46,47 with moderate depression, and none with severe depression.
Assessment tools for depression included Hospital Anxiety and Depression Scale for Depression, Beck Depression Inventory, Hamilton Depression Scale, Self-rating depression scale, Korea geriatric depression scale, and Neurobehavioral Functioning Inventory Sub-scale.
Risk of bias
The risk-of-bias results are summarized for the included studies in Fig. 2. All the studies were described as randomized. Nine studies5,12,24,41,42,43,44,45,46 described the method of randomization used. Information on concealment of treatment allocation was reported in three studies5,31,44. No study described clearly blinding of the participants and personnel. VR interventions are difficult to blind, so blindness of participants and personnel was assessed as having a high risk of bias in all studies. Two trials44,46 reported adequate blinding of the outcome assessor. There was no study at unclear risk of bias about incomplete outcome data. The risk of bias due to selection reporting was low across all the studies. No other potential bias was found in all studies.
The effect of VR-based interventions on depression
A total of 752 patients with stroke from 11 RCTs studies were included. The mean age of the four studies was under the age of 60, and the mean age of seven studies was over 60 years. The random effects model was used to pool the SMDs and corresponding 95% CIs. As shown in Fig. 3A, the results showed that depression scores in the VR group were significantly lower than that in the control group after the intervention (SMD = − 0.75, 95% CI − 1.35, − 0.15). Significant heterogeneity was observed among the studies (I2 = 92.2%, p = 0.000). Egger test (p = 0.983) and Begg test (p = 0.755) (see Supplementary Appendix 3) and Funnel plot (in Fig. 4) showed no evidence for publication bias. The result of sensitivity analysis (see Supplementary Appendix 4) showed the heterogeneity did not decrease significantly and the pooled SMD varied from − 0.535 (− 1.111, − 0.042) (when excluding Yu et al.43) to − 0.881 (− 1.487, − 0.274) (when excluding Adomaviciene et al.40), which confirmed the robustness of the findings. The results indicated a high level of heterogeneity across the articles. Therefore, subgroup analysis and meta-regression analysis were used to further clarify the potential reasons for heterogeneity. Results of the meta-regression analysis showed that the heterogeneity could be explained by mean age (P = 0.029) (see Supplementary Appendix 5).
(A) Forest plot of the effect of VR on depression. (B) Forest plot of the effect of VR on depression in participants’ different mean age. (1 less than 60 years and 2 more than 60 years in figure). (C) Forest plot of the effect of VR on depression for different intervention duration (1 less than 6 weeks, and 2 more than 6 weeks). (D) Forest plot of the effect of VR on depression for different depression rating (1 mild depression, and 2 moderate depression).
Subgroup analyses were performed based on WHO’s definition of the elderly (age < 60, age ≥ 60), the total intervention duration (< 6 weeks, ≥ 6 weeks), and depression rating (mild, moderate). The mean age of the four studies42,43,46,47 was under the age of 60, and the mean age of seven studies5,31,39,40,41,44,45 was over 60 years. As shown in Fig. 3B, the results indicated that depression scores in the VR group were reduced in participants with mean ages under 60 compared to control group (pooled effect size = − 1.69, 95% CI − 2.29, − 1.10). Significant heterogeneity was observed among the studies (I2 = 75.1%, p = 0.007). However, depression scores are not reduced in participants with mean ages over 60 compared to controls (pooled effect size = − 0.21, 95% CI − 0.88, 0.45). Significant heterogeneity was observed among the studies (I2 = 90.4%, p = 0.000).
For the duration of the intervention, five RCTs39,44,45,46,47 lasted longer than 6 × weeks, six RCTs5,31,40,41,42,43 were 1ess than 6 weeks. As shown in Fig. 3C, the results showed that depression scores in the VR group were statistically reduced for intervention session duration longer than 6 weeks compared to control group (pooled effect size = − 0.80, 95% CI − 1.60, − 0.01). Significant heterogeneity was observed among the studies (I2 = 91.2%, p = 0.000). Depression scores in the VR group were decreased for intervention session duration 1ess than 6 weeks compared to control group (pooled effect size = − 0.71, 95% CI − 1.69, 0.27). Significant heterogeneity was observed among the studies (I2 = 93.8%, p = 0.000).
Six of the studies5,31,40,42,44,45 involved people with mild depression, five39,41,43,46,47 included people with moderate depression and none with severe depression. As shown in Fig. 3D, the results indicated that depression scores in the VR group were significantly reduced in participants with moderate depression than control group (pooled effect size = − 1.52, 95% CI − 1.77, − 1.26). Depression scores in the VR group were decreased in participants with mild depression compared to control group (pooled effect size = -0.23, 95% CI − 0.44, − 0.01). Significant heterogeneity was observed among the studies (I2 = 92.2%, p = 0.000).
Discussion
Our meta-analysis systematically reviews currently available articles and included 11 studies with 752 patients to evaluate the effect of VR-based intervention on depression. The research results showed that depression score of VR-based intervention was significantly lower than that of the control group. The results are consistent with previous VR studies14,30 that have shown VR intervention to be beneficial in ameliorating depression.
The subgroup analysis divide’s the population by 60 years of mean age as a cutpoint, to focus on the impact of VR-based intervention on elderly stroke patients. The subgroup analysis suggests that VR intervention may have no effect on people over 60 years of age. For some older people, contacting VR technology has a challenging due to the visual and auditory changes48. This may be because older people have difficulty adapting to the new treatment regimen.
As to the total duration of the interventions, the subgroup analysis indicated that an intervention duration longer than 6 weeks was better than the intervention duration less than six weeks. In another meta-analysis, the results of meta-regression analysis showed that total intervention time had a significant effect on depression outcomes. It suggests that future VR interventions be conducted for at least 6 weeks, and the duration should be longer for greater efficiency against depressive outcomes.
Subgroup analysis of different depression ratings showed that VR-based intervention for patients with moderate depression was more effective than patients with mild depression. The result is consistent with previous literature that patients with higher baseline severity scores received more benefit from active treatments than from control conditions49.
If without social support, it has been confirmed that patients may have higher disability and medical burdens, and lower independence. Patients are at greater risk of developing PSD due to stroke-related defects after stroke50,51,52. The pathophysiological processes underlying PSD are multiple, complex, and incompletely understood18,21,36. Some of the main processes that may contribute to PSD include decreased levels of monoamines, abnormal neurotrophic response to stroke, increased inflammation with dysregulation of hypothalamicpituitary-adrenal (HPA) axis, and glutamate-mediated excitotoxicity53,54. Several potential mechanisms might explain the effect of VR-based intervention on depression, which may be through game-playing experiences and exercise training. In most VR interventions, rehabilitation programs are integrated into the game so that patients can have fun during the rehabilitation process. Evidence from neuropsychological researches shows the therapeutic value of game-based digital interventions in depression therapy, finding that positive game-playing experiences trigger the release of hormones such as endorphins and striatal dopamine55,56 that are responsible for feelings of pleasure and well-being57,58. In most VR interventions, rehabilitation programs also involve some level of exercise and being physically active. Rehabilitation exercise can help to rebuild brain structure can activate the function of related brain regions and promote adaptive behavioral changes, so that, it can promote the generation of positive emotions and improve the ability to cope with the depressive emotion.
VR as a therapeutic tool is rapidly popularized and widely used due to its novel training methods and ability to provide personalized rehabilitation training59. At present, various professional technology platforms and treatment schemes based on VR are also under active development and research14. The research results in recent decades showed that VR technology can be used to treat phobias, stress, and pain. But few have tried to develop VR anti-depressant interventions. Compared with traditional rehabilitation training, VR technology can precisely provide more individualized rehabilitation training programs according to the disease characteristics of different patients and can upload the training data on the internet in real-time. Through the data synchronization between different devices to improve the rehabilitation effect, the VR can also promote interaction between patients and the health system6.
Currently, no research results show which form of VR technical training or which treatment intensity has the best effect, and there is also a lack of guidelines on the VR development process. In future studies, the same interventions for patients having the same disease can be developed to eliminate high heterogeneity14. Few articles have evaluated or described feelings of immersion during treatment. The feelings of immersion should be used as an indicator for observation in future research, and the system needs to be to support improved outcomes to clarify how immersive and sophisticated. Recently, commercialized VR has developed rapidly, so, it is important to consider the cost, feasibility, and accessibility of VR equipment60. Few articles report the cost of VR rehabilitation training and the economic benefits of this type’s training have not been compared with the control group. In future studies, the cost of different types rehabilitation training should be used as an indicator for observation14. VR may also be used to alleviate depression symptoms and prevent depression in healthy people with some clinically related depression symptoms or sub-domain depression in the future. Based on evidence-based treatment techniques, consumer-targeted VR interventions have great potential to have an impact on the public’s psychological health.
There were some limitations should be noted in this study. It is different in the VR intervention forms, intervention period and frequency, and outcome evaluation scales adopted in the included studies. In addition, it is not quite the same that VR technology equipment used and the conventional physical rehabilitation mode implemented by the control group in each study. Above differences may be the reason for the high heterogeneity of results. Due to the particularity of VR technology interventions, the blind method is difficult for patients in the experimental group, which may lead to the deviation of subjective data reported by patients in the result evaluation.
Conclusions and implications
The current meta-analysis indicates the VR-based intervention had a moderate effect on depression in stroke patients compared to control group. VR-based intervention session duration longer than 6 weeks was better than intervention session duration less than six weeks. For older adults with a mean age more than 60 years, depression scores of VR-based intervention on depression was not decreased than the control group. There was no evidence of potential publication bias based on the assessment of visual inspection to funnel plots Egger test and Begg test. Substantial heterogeneity between studies was observed, and meta-regression analysis showed that mean age might be the source of heterogeneity. This rehabilitation technology, suitable for promotion in family and community, has the advantages of saving manpower and low technical requirements. At the same time, clinical studies of different ages and different intervention duration also need further in-depth study.
Data availability
All data generated or analyzed during the study are included in this published article and its Supplementary Information document.
References
Szczepanska-Gieracha, J., Cieślik, B., Rutkowski, S., Kiper, P. & Turolla, A. What can virtual reality offer to stroke patients? A narrative review of the literature. NeuroRehabilitation 47, 109–120 (2020).
Rooij, I. J. M. D., Port, I. G. L. V., Visser-Meily, J. M. A. & Meijer, J. W. G. Virtual reality gait training versus non-virtual reality gait training for improving participation in subacute stroke survivors: Study protocol of the ViRTAS randomized controlled trial. Trials 20(1), 89 (2019).
Ezema, C. I. et al. Influence of post-stroke depression on functional independence in activities of daily living. Ethiop. J. Health Sci. 29(1), 841–846 (2019).
Ghaffari, A., Akbarfahimi, M. & Rostami, H. R. Discriminative factors for post-stroke depression. Asian J. Psychiatr. 48, 101863 (2020).
Lin, R. C. et al. Effectiveness of early rehabilitation combined with virtual reality training on muscle strength, mood state, and functional status in patients with acute stroke: A randomized controlled trial. Worldviews Evid. Based Nurs. 17(2), 158–167 (2020).
Schöttke, H. & Giabbiconi, C. M. Post-stroke depression and post-stroke anxiety: Prevalence and predictors. Int. Psychogeriatr. 27, 1805–1812 (2015).
Kim, J. L., Cho, J., Park, S. & Park, E. C. Depression symptom and professional mental health service use. BMC Psychiatry 15, 261 (2015).
Ma, C. et al. Probable REM sleep behavior disorder and risk of stroke: A prospective study. Neurology 88(19), 1849–1855 (2017).
Robinson, R. G. & Jorge, R. E. Post-stroke depression: A review. Am. J. Psychiatry 173(3), 221–231 (2016).
Medeiros, G. C., Roy, D., Kontos, N. & Beach, S. R. Post-stroke depression: A 2020 updated review. Gen. Hosp. Psychiatry 66, 70–80 (2020).
Das, J. & Rajanikant, G. K. Post stroke depression: The sequelae of cerebral stroke. Neurosci. Biobehav. Rev. 90, 104–114 (2018).
Hongting, B., Pingan, Q. & Xinke, L. Effect of virtual reality psychological rehabilitation on recovery of daily living ability in patients with post-stroke depression. Mod. Pract. Med. 32, 1419–1420 (2020).
Carvalho, A. F., Sharma, M. S., Brunoni, A. R., Vieta, E. & Fava, G. A. The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: A critical review of the literature. Psychother. Psychosom. 85(5), 270–288 (2016).
Fodor, L. A. et al. The effectiveness of virtual reality based interventions for symptoms of anxiety and depression: A meta-analysis. Sci. Rep. 8(1), 10323 (2018).
Tan, H. L. E., Chng, C. M. L., Lau, Y. & Klainin-Yobas, P. Investigating the effects of a virtual reality-based stress management programme on inpatients with mental disorders: A pilot randomised controlled trial. Int. J. Psychol. 56(3), 444–453 (2021).
Sohn, B. K. et al. Developing a virtual reality-based vocational rehabilitation training program for patients with schizophrenia. Cyberpsychol. Behav. Soc. Netw. 19(11), 686–769 (2016).
Wang, M., Lyu, X.-Q., Li, Y.-J. & Zhang, F.-L. VR content creation and exploration with deep learning: A survey. Comput. Vis. Media 6(1), 3–28 (2022).
Xie, X. & Huang, G. Z. Application study and progress on rehabilitation for stroke patients by virtual reality technology. Chin. J. Brain Dis. Rehabil. 4(4), 257–260 (2014).
Freeman, D. et al. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol. Med. 47(14), 2393–2400 (2017).
Martínez-Olmos, F. J. et al. An intradialytic non-immersive virtual reality exercise programme: A crossover randomized controlled trial. Nephrol. Dial. Transplant. 37(7), 1366–1374 (2022).
Bang, Y. S., Son, K. H. & Kim, H. J. Effects of virtual reality training using Nintendo Wii and treadmill walking exercise on balance and walking for stroke patients. J. Phys. Ther. Sci. 28(11), 3112–3115 (2016).
Dominguez-Tellez, P., Moral-Munoz, J. A., Casado-Fernandez, E., Salazar, A. & Lucena-Anton, D. Effects of virtual reality on balance and gait in stroke: A systematic review and meta-analysis. Rev. Neurol. 69(6), 223–234 (2019).
Garay-Sánchez, A., Suarez-Serrano, C., Ferrando-Margeli, M., Jimenez-Rejano, J. J. & Marcén-Román, Y. Effects of immersive and non-immersive virtual reality on the static and dynamic balance of stroke patients: A systematic review and meta-analysis. J. Clin. Med. 10(19), 4473 (2021).
Segura-Ortí, E. et al. Virtual reality exercise intradialysis to improve physical function: A feasibility randomized trial. Scand. J. Med. Sci. Sports. 29(1), 89–94 (2019).
Chen, Y., Fanchiang, H. D. & Howard, A. Effectiveness of virtual reality in children with cerebral palsy: A systematic review and meta-analysis of randomized controlled trials. Phys. Ther. 98(1), 63–77 (2018).
Botella, C., Fernández-Álvarez, J., Guillén, V., García-Palacios, A. & Baños, R. Recent progress in virtual reality exposure therapy for phobias: A systematic review. Curr. Psychiatry Rep. 19(7), 42 (2017).
Mitrousia, V. & Giotakos, O. Virtual reality therapy in anxiety disorders. Psychiatriki 27(4), 276–286 (2016).
Otte, C. Cognitive behavioral therapy in anxiety disorders: Current state of the evidence. Dial. Clin. Neurosci. 13(4), 413–421 (2011).
Norton, P. J. & Price, E. C. A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. J. Nerv. Ment. Dis. 195(6), 521–531 (2007).
Yen, H. Y. & Chiu, H. L. Virtual reality exergames for improving older adults’ cognition and depression: A systematic review and meta-analysis of randomized control trials. J. Am. Med. Dir. Assoc. 22(5), 995–1002 (2021).
Rogers, J. M., Duckworth, J., Middleton, S., Steenbergen, B. & Wilson, P. H. Elements virtual rehabilitation improves motor, cognitive, and functional outcomes in adult stroke: Evidence from a randomized controlled pilot study. J. Neuroeng. Rehabil. 16(1), 56 (2019).
Bevilacqua, R. et al. Non-immersive virtual reality for rehabilitation of the older people: A systematic review into efficacy and effectiveness. J. Clin. Med. 8(11), 1882 (2019).
Lei, C. et al. Effects of virtual reality rehabilitation training on gait and balance in patients with Parkinson’s disease: A systematic review. PLoS ONE 14(11), e0224819 (2019).
Laver, K. E. et al. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 11(11), CD008349 (2017).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 62(10), 1006–1012 (2009).
Higgins, J. P. T., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327(7414), 557–560 (2003).
Egger, M., Davey Smith, G., Davey, S., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109), 629–634 (1997).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4), 1088–1101 (1994).
Bi, H. T., Qian, P. A. & Li, X. K. Effect of virtual reality technology on recovery of daily living ability in patients with post-stroke depression. Mod. Pract. Med. 32(11), 1419–1420 (2020).
Adomavičienė, A., Daunoravičienė, K., Kubilius, R., Varžaitytė, L. & Raistenskis, J. Influence of new technologies on post-stroke rehabilitation: A comparison of armeo spring to the kinect system. Medicina (Kaunas) 55(4), 98 (2019).
Kim, J. W., Kim, J. H. & Lee, B. H. Effects of virtual reality-based core stabilization exercise on upper extremity function, postural control, and depression in persons with stroke. Phys. Ther. Rehabil. Sci. 9, 131–139 (2020).
Xu, N. J. & He, Y. G. Effects of Virtual reality rehabilitation on balance ability in patients with pusher syndrome after stroke. Henan Med. Res. 29(14), 2536–2538 (2020).
Yu, M. Q. et al. Effect of stroke unit combined with task-oriented training on young patients with ischemic stroke. Neural Inj. Funct. Reconstr. 16, 225–227 (2021).
De Rooij, I. J. M. et al. Effect of virtual reality gait training on participation in survivors of subacute stroke: A randomized controlled trial. Phys. Ther. 101(5), 051 (2021).
Zhang, X. X., Zheng, Y., Zhan, X. L., Ye, S. Z. & Hu, H. Effect of early virtual reality training on the rehabilitation of stroke patients with hemiplegia. Chin. J. Mod. Nurs. 23, 3704–3708 (2017).
Yan, S. et al. Effect of virtual reality training combined with psychological intervention on post-stroke depression. Chin. J. Rehabil. Med. 33(6), 727–729 (2018).
Eun, G. B. S. & Park, C. Effect of virtual reality games on stroke patients’ balance, gait, depression, and interpersonal relationships. J. Phys. Ther. Sci. 27, 2057–2060 (2015).
Dermody, G., Whitehead, L., Wilson, G. & Glass, C. The role of virtual reality in improving health outcomes for community-dwelling older adults: Systematic review. J. Med. Internet Res. 22, e17331 (2020).
Fournier, J. C. et al. Antidepressant drug effects and depression severity: A patient-level meta-analysis. JAMA 303(1), 47–53 (2013).
Guiraud, V. et al. Depression predictors within six months of ischemic stroke: The DEPRESS study. Int. J. Stroke 11, 519–525 (2016).
Shi, Y., Yang, D., Zeng, Y. & Wu, W. Risk factors for post-stroke depression: A meta analysis. Front. Aging Neurosci. 9, 218 (2017).
Volz, M., Voelkle, M. C. & Werheid, K. General self-efficacy as a driving factor of poststroke depression: A longitudinal study. Neuropsychol. Rehabil. 29, 1426–1438 (2019).
Loubinoux, I. et al. Post-stroke depression: Mechanisms, translation and therapy. J. Cell Mol. Med. 16, 19611969 (2012).
Robinson, R. G. & Jorge, R. E. Post-stroke depression: A review. Am. J. Psychiatry 173, 221–231 (2016).
Koepp, M. J. et al. Evidence for striatal dopamine release during a video game. Nature 393, 266–268 (1998).
Craig, A. B. et al. Social contracts and human-computer interaction with simulated adapting agents. Adapt. Behav. 21, 371–387 (2013).
Amir, S., Brown, Z. W. & Amit, Z. The role of endorphins in stress: Evidence and speculations. Neurosci. Biobehav. Rev. 4, 77–86 (1980).
Salamone, J. D. Dopamine, effort, and decision making: Theoretical comment on Bardgett et al.. Behav. Neurosci. 123, 463 (2009).
Torrisi, M. et al. Using telerehabilitation to improve cognitive function in post-stroke survivors: Is this the time for the continuity of care? Int. J. Rehabil. Res. 42(4), 344–351 (2019).
Mallari, B., Spaeth, E. K., Goh, H. & Boyd, B. S. Virtual reality as an analgesic for acute and chronic pain in adults: A systematic review and meta-analysis. J. Pain Res. 12, 2053–2085 (2019).
Acknowledgements
The authors thank the researchers who conducted the studies and the experts for their valuable opinions.
Funding
Health appropriate technology poverty project of Jilin Province [2020FP044].
Author information
Authors and Affiliations
Contributions
H.L. and Z.C. wrote the main manuscript text and table, and S.W. prepared all figures, and Y.J. modified manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, H., Cheng, Z., Wang, S. et al. Effects of virtual reality-based intervention on depression in stroke patients: a meta-analysis. Sci Rep 13, 4381 (2023). https://doi.org/10.1038/s41598-023-31477-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-31477-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.