Abstract
To examine factors for adherent and non-adherent behavior in patients with cluster headache and migraine. Adults with cluster headache or migraine were included in this anonymous online survey using a questionnaire accessed via homepages of headache support groups. Medication adherence in preventive treatment was measured with the Medication Adherence Report Scale (MARS-D). Factors for non-adherent behavior were examined (subjective socioeconomic status, psychological comorbidities, self-efficacy, coping, side effects, expectations of treatment, information on medical treatment, and trust in the physician/treatment concept). 200 participants (n = 58 with cluster headache, n = 142 with migraine) were included. The rate of medication adherence in preventive treatment was 32.8% for participants with cluster headache and 20.4% for migraine. The most common reasons for low adherence in participants with cluster headache were altering the prescribed medication dose (34%) or taking less than instructed (14%), which was mostly due to insufficient benefit from the medication or side effects. Positive expectations of medical treatment (p ≤ 0.05) correlated significantly with adherent behavior in cluster headache. Furthermore, the adherence-promoting factors coping and self-efficacy were more pronounced in patients with cluster headache than in those with migraine (p < 0.05). This study is the first to comprehensively investigate medication adherence and factors influencing adherent/non-adherent behavior in patients with cluster headache. Patients with cluster headache had similar adherence levels to patients with migraine, but had higher resources of adherence-promoting factors.
Similar content being viewed by others
Introduction
Cluster headache (CH) is amongst the most severe and disabling painful conditions1,2. CH is also called "suicide headache" because the pain intensity and impairment of quality of life can be so severe that sufferers tend to have suicidal thoughts and tendencies3. It is further associated with psychiatric comorbidities such as depression, anxiety, or aggressive behavior3,4, especially in chronic CH. Diagnosis of chronic CH requires cluster attacks occurring for one year or longer without remission, or with remission periods lasting less than 3 months and therefore often represent an even greater burden for the patient than episodic CH1. This results in high direct and indirect costs for both the affected patients and the healthcare system, especially in chronic cases5. The main focus of treating CH is on acute suppression of attacks through medication and a prophylactic treatment with daily intake to reduce attack frequency6.
A pivotal factor for successful treatment is high adherence7. This concept of treatment compliance is defined as the extent to which a person's behavior—taking medication, following a therapeutic concept or changing one’s lifestyle—is in line with the agreed recommendations of a healthcare provider8. Due to the multiple interactions between treatment provider, patient and the healthcare system, adherence is a complex construct that is influenced by multiple factors. The World Health Organization (WHO) distinguishes between the following factors: patient-related factors (e.g. self-efficacy), health system-related factors (e.g. trust in the doctor and in the treatment), therapy-related factors (e.g. strong burden of side effects), condition-related factors (e.g. comorbidities) and socioeconomic factors (e.g. low socioeconomic status)8. Whereby self-efficacy is the personal conviction of people to be able to cope with difficult demands by their own efforts9. Self-efficacy expectations arise from confidence in one's own ability to act and describe a person's expectation that they can consciously influence themselves and things in the world. Self-efficacy expectations contribute to the activation and maintenance of health-relevant behaviour and are positively related to the development of adherent behaviour10.
Non-adherent behavior is a great challenge in providing efficient medical care. It has even been described as the “Achilles’ heel of modern medicine”, and leads to higher morbidity, mortality, unnecessary utilization of healthcare resources11. 25–50% of headache patients are non-adherent to preventive medication12. In patients with chronic headache adherence to prescribed medication treatments is even lower, with non-adherence rate of 50–60%11. However, no patients with CH were studied in these trials. Medication adherence is a particularly important aspect in CH, as medication over a long period of time is the mainstay of clinical treatment in this severe pain disorder.
While adherence in the treatment of migraine is already relatively well explored13,14,15,16, studies of adherence in the treatment of CH are rare. The aim of the present study was to examine the hypothesis that adherence in patients with CH differs from that in migraine and that there are different factors for adherent and non-adherent behaviour in patients with CH versus migraine.
Methods
Participants
The present study included participants aged 18 years and older with a medical history of cluster headache or migraine with or without aura. Diagnoses were based on participants’ self-report at the beginning of an anonymous online survey with a browser-based questionnaire, whose link was provided on the homepages of headache support groups. The online questionnaire took about 10 min to complete. All study participants were provided with written information about the study procedure prior to inclusion. Inclusion was only possible if participants provided informed consent, which was confirmed by sending the data at the end of the survey. The data were recorded anonymously and documented using EvaSys (Education Survey Automation Suite), a software package for online surveys of the IT Center of the University of Rostock.
Measures
To assess medication adherence and factors included in the WHO report8 known to influence adherent behavior, we developed a comprehensive questionnaire consisting of standardized self-rating procedures and items constructed for the purpose of this investigation.
Medication adherence was measured with the German version of the Medication Adherence Report Scale (MARS-D), which consists of five items. A score of 25 indicates maximum adherent behavior. The psychometric properties of the MARS-D have been tested in two study populations, and it is the questionnaire with the best psychometric properties for the German-speaking area17,18.
In total, eight factors for non-adherent behavior were examined: Subjective socioeconomic status was measured with the German version of the MacArthur Scale19.To assess mental comorbidities, the Prime MD Patient Health Questionnaire (PHQ) in its German version (PHQ-D) was used20. Self-management skills like self-efficacy and coping are important factors for adherence. To assess these factors, we used the Questionnaire for the Assessment of Resources and Self-Management Skills (FERUS) which contains 66 items allocated to the following seven scales: motivation to change, coping, self-observation, self-efficacy, self-verbalization, hope, and social support21. As there were no suitable questionnaires for further examined factors on non-adherent behavior (like side effects, expectations of the treatment, information on medical treatment, and trust in the doctor and the treatment concept) these factors were measured using items constructed for the purpose of the present survey, with items rated on a 5-point Likert scale from “always” to “never” (See Supplementary Table 1).
Analyses
The data were analyzed using the statistical program SPSS (version 23.0). The main variables were analyzed using descriptive statistics. Pearson's Phi correlation (between two dichotomous variables) and Eta correlation (between dichotomous and metric variables) were used to measure the strength of association.
To compare means between two independent samples, under the assumption of a normal distribution, t-tests were used. In the case of non-normal distribution, Mann–Whitney U tests were applied. As this was an exploratory study results were not corrected for multiple testing.
Ethical approval and informed consent
This online survey was approved by the Ethics committee of the University Medical Center Rostock (A2016-0051). Written informed consent was obtained from all participants.
Results
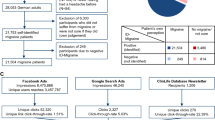
From the beginning of May 2016 to the middle of June 2016, n = 200 patients took part in the survey, of whom n = 58 were allocated to group 1, with the medical diagnosis of cluster headache, and n = 142 to group 2, with the medical diagnosis of migraine with or without aura (see Table 1). For the inclusion of the patients in the study, see the flowchart (Fig. 1). The patients with cluster headache had been suffering for an average of 15.8 years (SD = 11.1). The medical diagnosis had been made 8.4 years ago (SD = 7.9), and treatment had begun 8.6 years ago (SD = 8.3). The patients with migraine had been suffering for an average of 22.8 years (SD = 13.3), the medical diagnosis had been made 15.9 years ago (SD = 12.4) and medical treatment had begun 13.1 years ago (SD = 11.4). The majority of patients in both groups were severely impaired (Supplementary Table 2a,b).
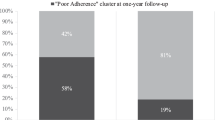
Rate of medication adherence
The rate of medication adherence using the MARS-D scale, reached a mean score of 22.4 (SD = 2.9) in the group of CH patients and 21.9 (SD = 3.0) in the group of migraine patients. In line with the literature, the cut-off for adherence was set strictly at a score of 25, and a score ≤ 24 was accordingly rated as non-adherent behavior22,23. This resulted in an adherence rate of 32.8% for patients with cluster headache and 22.0% for migraine patients (p = 0.112). Adherence to general medication was assessed with the MARS-D test. No distinction was made between acute pain medication and prophylactic medication.
The individual behavioral aspects contributing either to adherent or non-adherent behavior are evident from the various items of the MARS-D. Tables 2, 3, 4 and 5 presents the distribution of response frequencies for the groups of patients with CH and migraine. None of the patients with CH reported forgetting to take their medication “always” or “often”. Only 8.6% of the patients “sometimes” forgot to take their medication, and 91.4% “never” or “rarely” forgot to do so. Likewise, patients also reported “rarely” or “never” purposely skipping medication (93.1%) or reducing the dose (86.2%). Patients were most likely to report altering the dose, with only 65.5% of patients indicating that they “never” or “rarely” do so. The group of migraine patients showed similar behavior. An item-wise comparison between participants with CH and migraine showed no statistically significant differences for the percentages of responses for all 5 items of the MARS-D.
Reasons for stopping the medication
In the questionnaire, CH and migraine patients were asked whether they had ever stopped taking prescribed medication for headache treatment, and if so for what reason. Multiple responses could be given. Figure 2 shows that in total, 36.2% of the CH patients and 31.7% of the migraine patients indicated that they had never stopped taking prescribed medication (p = 0.027). Another reason given significantly more often by migraine patients than by CH patients was "concern about side effects" (p = 0.042). The most frequently mentioned reason for stopping medication, regardless of medical prescription, was "side effects" and the second most frequent was "no effect" of the therapy in both groups (Fig. 2).
Medications in cluster headache patients
In both patient groups, the patients who were taking regular medication for headache prevention at the time of the survey were asked which medications they were taking, whether they were able to tolerate these medications, and whether they were effective. Thirty-eight CH patients were regularly taking medication for preventive purposes at the time of the survey. Table 6 demonstrates that the majority (71.1%) were taking verapamil. Moreover, tolerability and effectiveness were also most frequently reported for verapamil (85.2% and 70.4%, respectively).
Factors for non-adherent behavior
We examined the association between adherence and possible factors for non-adherent behavior based on the WHO classification. For this purpose, correlations between the level of adherence (MARS-D) and the factors subjective socioeconomic status (MacArthur Scale), mental comorbidities (PHQ), self-efficacy (FERUS), coping (FERUS), side effects, expectations of the treatment, information on medical treatment, trust in the doctor and the treatment concept, keeping medical appointments and impairment were assessed. Table 7 depicts the strength of correlations (r) and the significance (p) between adherence (yes/no) and the possible factors for non-adherent behavior for CH and migraine patients respectively.
In the group of migraine patients there was a statistically significant correlation between adherence and "Trust in doctor and treatment concept" with a small effect size (Cohen’s d = 0.29). With a Cohen’s d = 0.09, the difference between adherent and non-adherent migraine patients regarding “Coping” is negligible, even though it is statistically significant. In the group of CH patients there was a statistically significant correlation for adherence with “expectations on the therapy” with a large effect size (Cohen’s d = 0.82) (Table 7).
In the group comparison, statistically significant higher rates of self-efficacy (p = 0.005) and coping (p = 0.028) were found in the CH patients compared to the migraine patients (Table 8). For mental comorbidities, there was no statistically significant difference between the groups, nor between the subgroups of adherent patients (Table 9).
Comparison of patients with chronic and episodic cluster headache
In the present survey, 24 patients (41.4%) reported suffering from chronic CH and 34 patients (58.6%) from episodic CH. Adherence as measured with the MARS-D was comparable between both groups (chronic CH: mean = 21.58, SD = 3.41; episodic CH: mean = 22.94; SD = 2.37).
Discussion
This study is the first study to comprehensively investigate medication adherence and factors influencing adherent/non-adherent behaviour in patients with CH in comparison to another disabling primary headache, migraine. Adherence, as a concept of treatment fidelity and mutual co-operation between treatment provider and patient, is a complex construct which is subject to the influence of multiple factors. With the present survey, we first examined the level of adherence, and investigated factors which may influence non-adherent behavior. The results show that the adherence rate is numerically higher in CH patients than in those with migraine, however, the difference did not reach statistical significance (33% vs. 22%). We were also able to show that factors such as "positive expectations of medical treatment" are significantly correlated with adherent behaviour in CH patients, while "coping" and "trust in doctor and treatment concept" are significantly associated with adherent behaviour in migraine patients.
It is known from the literature that migraine patients show low adherence and persistence (i.e. the time for which a patient takes a prescribed medication) for prophylactic migraine medication15,24. The reasons for low adherence can be attributed to altering the prescribed medication dose, or temporarily stopping medication; in contrast, forgetting to take medication did not constitute a relevant reason (Tables 2, 3, 4 and 5). On a critical note, it should be mentioned that in line with the literature22,23, we chose a conservative and strict definition of non-adherent behavior with MARS-D scores of ≤ 24. However, in the literature, there are also several studies which set less restrictive cut-off scores of ≥ 2325 or > 2326 for adherent behavior. To overcome the potential limitations of a strict definition of adherence, we conducted additional analyses using a more permissive approach, the adherence sum score. For this, we examined the sum score of the individual MARS-D items without finding statistically significant differences for the two headache groups (Table 4).
Although no statistically significant difference could be found for the level of adherence between CH and migraine it remains intriguing that a highly burdensome and impairing disorder like CH would imply higher adherence to medical treatment. However, impairment as measured with the HIT-6 did not exert a statistically relevant influence on treatment adherence, neither in CH nor migraine. A higher degree of coping and self-efficacy could be identified as a pivotal factor of adherence in CH patients.
A correlation analysis of the socio-demographic and headache-related factors with the adherence sum score also showed no significant differences compared to the correlation analysis of the cut-off adherence score.
The most frequent reason for skipping or stopping medication mentioned in both groups was "side effects" and the second most frequent was "no effect" of the therapy in line with literature on treatment adherence in migraine. While "concern about side effects" was a significantly more frequent reason for skipping or stopping medication in migraine patients than in CH patients. For prophylactic medications in migraine, it is known from the literature that the side effects are perceived as particularly burdensome and likely to lead to a discontinuation of treatment15.
CH patients using prophylactic medication at the time of the survey were asked which medications they took and how they rated tolerability and effectiveness of the respective medication. 71% of the patients took verapamil, 21% took topiramate and 13% took lithium, which essentially corresponds to the national guidelines on first- and second-line prophylactic medication in the treatment of CH27. For verapamil, 85% reported good tolerability and 70% reported effectiveness (Table 6). As an insufficient effectiveness of prophylactic medication and side effects were mentioned as the most frequent reasons for stopping medication and thus for non-adherent behavior, it would be interesting for future research to determine how newer treatments, for instance with CGRP receptor/ligand antibodies28,29, or also neuromodulatory procedures30, are evaluated by patients in terms of effectiveness and treatment adherence. Discontinuation rates in the large phase 3 trials for galcanezumab in episodic and chronic migraine compared to episodic and chronic CH were higher in migraine. A discontinuation rate of 12%31 was found for episodic migraine and 5.4%32 for chronic migraine compared to 8%28 for episodic CH, and 3.4%33 for chronic CH. However, this may not fully reflect treatment adherence in a real-world setting.
In CH patients we could show that positive expectations of medical treatment is significantly correlated with adherent behavior while for migraine patients “coping” and “trust in doctor and treatment concept” is significantly correlated with adherent behavior. These findings are in accordance with research on adherence in other diseases. Comprehensive information plays a pivotal role in the development of realistic expectations towards medical treatment and thus strengthens adherent behavior34,35,36. Coping as a factor of self-efficacy correlated with adherent behaviour in the migraine group, as expected, whereas we could not show this for CH patients. Regarding the influence of self-efficacy on adherence, the influences described in the literature are also contradictory34,37, although the majority of studies show that high self-efficacy is associated with adherent behaviour11,38. However, excessive levels of self-efficacy may also have opposite effects34. Why "expectations of therapy" were more important for adherence in patients with CH, while "coping" and "trust in the doctor" were more important in migraine patients can only be speculated. It is possible that patients with CH have a more bio-pharmacological understanding of the disease and that drug therapy is of particular importance for them, whereas migraine patients have more of a bio-psycho-social understanding of the disease and that other factors are also important for therapy for them. Interestingly, we found significantly higher self-efficacy and coping in CH patients than in migraine patients in the group comparison suggesting headache-specific aspects of disease management.
For the following factors which we examined in line with the WHO report8 in terms of an influence on adherence, we found no significant influence on adherence in patients with CH contrary to our assumptions: socioeconomic status, mental comorbidity, self-efficacy, coping, side effects, and trust in the doctor and the treatment concept. From studies on other diseases, it is known that a higher socioeconomic status can correlate with adherent behavior39,40, although several studies also found no relation between socioeconomic status and medication adherence11. Moreover, it has been suggested that the influence of educational level on adherence is often overestimated41. For psychiatric disorders such as major depression, we found a negative correlation with adherent behaviour in both CH and migraine patients, although this was not statistically significant.
Adherence is a complex construct. However, the study also shows that knowledge of headache-specific aspects could be helpful for education and patient care. With this knowledge, the treating physician can focus on a more detailed explanation of the drug therapy for CH patients, while for migraine patients, strengthening the doctor-patient relationship and coping factors is conducive to better adherence.
Limitations
Limitations of the present study may arise from the smaller sample size in the group of CH patients and a potential selection bias given that the participants were recruited using an online resource only. Additionally, it was not possible to individually verify the diagnosis by a physician. Furthermore, the reliable assessment of adherence constitutes is challenging7. There are direct and indirect procedures for measuring adherence. In the direct procedures, for example, the number of skipped tablets are counted or the level of medication in the patient’s blood is determined. Such procedures are often more precise, but are also more laborious, in part invasive, and linked to a greater cost expenditure.
Using indirect procedures, self-observation or self-rating instruments can be employed7. Indirect procedures are fundamentally more economical and have a greater reach, but often tend to overestimate adherence within the self-rating, possibly due to a retrospective bias or socially desirable response tendencies42. For the present analysis, we employed an indirect procedure in the form of a self-rating instrument presented as an anonymous online survey. Compared to direct surveys, this procedure has the great advantage that the anonymous data collection increases the likelihood of authentic, open responding with respect to possible non-adherent behavior, meaning that biases regarding socially desirable response tendencies are rather low. The self-rating questionnaire used to assess medication adherence in its German-language version (MARS-D) is a test instrument that has been examined with respect to its internal consistency, test–retest reliability18 and validity43.
Conclusion
This study is the first to comprehensively investigate medication adherence and factors influencing adherent/non-adherent behavior in patients with CH compared to patients with migraine. Contrary to our expectations, we found similar adherence rates for patients with CH and migraine and were able to show that there are headache-specific differences that influence adherence. This should be taken into account in treatment with regard to adherence and thus have very practical implications for therapy.
Data availability
All data generated or analysed during this study are included in this published article o rare available from the corresponding author on reasonable request.
References
May, A. et al. Cluster headache. Nat. Rev. Dis. Primers 01(4), 18006 (2018).
Hoffmann, J. & May, A. Diagnosis, pathophysiology, and management of cluster headache. Lancet Neurol. 17(1), 75–83 (2018).
Louter, M. A. et al. Cluster headache and depression. Neurology 87(18), 1899–1906 (2016).
Jürgens, T. P. et al. Impairment in episodic and chronic cluster headache. Cephalalgia 31(6), 671–682 (2011).
Negro, A., Sciattella, P., Spuntarelli, V., Martelletti, P. & Mennini, F. S. Direct and indirect costs of cluster headache: A prospective analysis in a tertiary level headache centre. J. Headache Pain 21(1), 44 (2020).
Robbins, M. S., Starling, A. J., Pringsheim, T. M., Becker, W. J. & Schwedt, T. J. Treatment of cluster headache: The American Headache Society evidence-based guidelines. Headache 56(7), 1093–1106 (2016).
Osterberg, L. & Blaschke, T. Adherence to medication. N. Engl. J. Med. 353(5), 487–497 (2005).
Sabaté, E. Adherence to Long-Term Therapies: Evidence for Action (2003).
Bandura, A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 84(2), 191–215 (1977).
Older people in the field of medication. Nurs. Older People. 14 (5), 9. https://doi.org/10.7748/nop.14.5.9.s11 (2002).
Rains, J. C., Lipchik, G. L. & Penzien, D. B. Behavioral facilitation of medical treatment for headache–part I: Review of headache treatment compliance. Headache 46(9), 1387–1394 (2006).
Ramsey, R. R. et al. Treatment adherence in patients with headache: A systematic review. Headache 54(5), 795–816 (2014).
Seng, E. K., Robbins, M. S. & Nicholson, R. A. Acute migraine medication adherence, migraine disability and patient satisfaction: A naturalistic daily diary study. Cephalalgia 37(10), 955–964 (2017).
Hepp, Z. et al. Adherence to oral migraine-preventive medications among patients with chronic migraine. Cephalalgia 35(6), 478–488 (2015).
Hepp, Z., Bloudek, L. M. & Varon, S. F. Systematic review of migraine prophylaxis adherence and persistence. J. Manag. Care Pharm. 20(1), 22–33 (2014).
Seng, E. K., Rains, J. A., Nicholson, R. A. & Lipton, R. B. Improving medication adherence in migraine treatment. Curr. Pain Headache Rep. 19(6), 24 (2015).
Horne, R. et al. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the Necessity-Concerns Framework. PLoS ONE 8(12), e80633 (2013).
Mahler, C. et al. Assessing reported adherence to pharmacological treatment recommendations. Translation and evaluation of the Medication Adherence Report Scale (MARS) in Germany. J. Eval. Clin. Pract. 16(3), 574–579 (2010).
Adler, N. E., Epel, E. S., Castellazzo, G. & Ickovics, J. R. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. 19(6), 586–592 (2000).
Spitzer, R. L., Kroenke, K. & Williams, J. B. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 282(18), 1737–1744 (1999).
Znoj, H., Baumgartner, S., Klinische Untersuchungsverfahren. & Jack, M. FERUS-Fragebogen zur Erfassung von Ressourcen und Selbstmanagementfähigkeiten. Zeitschrift für klinische Psychologie und Psychotherapie (2007).
Gialamas, A. et al. Does point-of-care testing lead to the same or better adherence to medication? A randomised controlled trial: The PoCT in General Practice Trial. Med. J. Aust. 191(9), 487–491 (2009).
George, J., Kong, D. C. M., Thoman, R. & Stewart, K. Factors associated with medication nonadherence in patients with COPD. Chest 128(5), 3198–3204 (2005).
Lafata, J. E., Tunceli, O., Cerghet, M., Sharma, K. P. & Lipton, R. B. The use of migraine preventive medications among patients with and without migraine headaches. Cephalalgia 30(1), 97–104 (2010).
Alsous, M. et al. Adherence to 6-Mercaptopurine in children and adolescents with Acute Lymphoblastic Leukemia. PLoS ONE 12(9), e0183119 (2017).
van den Bemt, B. J. F. et al. Adherence rates and associations with nonadherence in patients with rheumatoid arthritis using disease modifying antirheumatic drugs. J. Rheumatol. 36(10), 2164–2170 (2009).
LL 54-ll-Clusterkopfschmerz und trigeminoautonome Kopfschmerzen—Deutsche Gesellschaft für Neurologie e. V. [Internet]. Deutsche Gesellschaft für Neurologie e. V. [cited 2020 Dec 3]. Available from: https://dgn.org/leitlinien/ll-54-ll-clusterkopfschmerz-und-trigeminoautonome-kopfschmerzen/.
Goadsby, P. J. et al. Trial of galcanezumab in prevention of episodic cluster headache. N. Engl. J. Med. 381(2), 132–141 (2019).
Ruscheweyh, R. et al. Effect of calcitonin gene-related peptide (-receptor) antibodies in chronic cluster headache: Results from a retrospective case series support individual treatment attempts. Cephalalgia 17, 333102420949866 (2020).
Rimmele, F. & Jürgens, T. P. Neuromodulation in primary headaches: Current evidence and integration into clinical practice. Curr. Opin. Neurol. 33(3), 329–337 (2020).
Skljarevski, V. et al. Efficacy and safety of galcanezumab for the prevention of episodic migraine: Results of the EVOLVE-2 Phase 3 randomized controlled clinical trial. Cephalalgia 38(8), 1442–1454 (2018).
Detke, H. C. et al. Galcanezumab in chronic migraine: The randomized, double-blind, placebo-controlled REGAIN study. Neurology 91(24), e2211–e2221 (2018).
Dodick, D. W. et al. Phase 3 randomized, placebo-controlled study of galcanezumab in patients with chronic cluster headache: Results from 3-month double-blind treatment. Cephalalgia 40(9), 935–948 (2020).
Johnson, M. J., Williams, M. & Marshall, E. S. Adherent and nonadherent medication-taking in elderly hypertensive patients. Clin. Nurs. Res. 8(4), 318–335 (1999).
Garnett, W. R. Antiepileptic drug treatment: Outcomes and adherence. Pharmacotherapy 20(8 Pt 2), 191S-199S (2000).
Donovan, J. L. & Blake, D. R. Patient non-compliance: Deviance or reasoned decision-making?. Soc. Sci. Med. 34(5), 507–513 (1992).
Dunbar-Jacob, J. & Mortimer-Stephens, M. K. Treatment adherence in chronic disease. J. Clin. Epidemiol. 54(Suppl 1), S57-60 (2001).
Rains, J. C., Penzien, D. B. & Lipchik, G. L. Behavioral facilitation of medical treatment for headache–part II: Theoretical models and behavioral strategies for improving adherence. Headache 46(9), 1395–1403 (2006).
Golin, C. E. et al. A prospective study of predictors of adherence to combination antiretroviral medication. J. Gen. Intern. Med. 17(10), 756–765 (2002).
Bhat, V. G. et al. Factors associated with poor adherence to anti-retroviral therapy in patients attending a rural health centre in South Africa. Eur. J. Clin. Microbiol. Infect. Dis. 29(8), 947–953 (2010).
Delaney, C. Reducing recidivism: Medication versus psychosocial rehabilitation. J. Psychosoc. Nurs. Ment. Health Serv. 36(11), 28–34 (1998).
Garber, M. C., Nau, D. P., Erickson, S. R., Aikens, J. E. & Lawrence, J. B. The concordance of self-report with other measures of medication adherence: A summary of the literature. Med. Care 42(7), 649–652 (2004).
Sampaio, R., Azevedo, L. F., Dias, C. C., Horne, R. & Castro Lopes, J. M. Portuguese version of the Medication Adherence Report Scale (MARS-9): Validation in a population of chronic pain patients. J. Eval. Clin. Pract. 25(2), 346–352 (2019).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
F.R.: drafted the manuscript, analysis and interpretation and revising the manuscript; B.M.: analysis, interpretation and revising the manuscript; N.B.: acquisition, analysis, interpretation and revising the manuscript; S.W.: analysis, interpretation and revising the manuscript; S.R.: interpretation and revising the manuscript; P.K.: analysis, interpretation and revising the manuscript; T.P.J.: conception, analysis, interpretation and revising the manuscript.
Corresponding author
Ethics declarations
Competing interests
FR served on advisory boards and/or as speaker for Allergan, Novartis, Teva, Ipsen. He has received royalties from Elsevier. BM, NB, SW declared no competing interest. SR declared no competing interests. PK served on advisory boards and/or as speaker for Allergan, Novartis, Teva and Lilly. TPJ served on advisory boards and/or as speaker for Allergan, Autonomic Technologies, Desitin, Grünenthal, Hormosan, Novartis, Lilly, Lundbeck, Sanofi and Teva.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rimmele, F., Müller, B., Becker-Hingst, N. et al. Medication adherence in patients with cluster headache and migraine: an online survey. Sci Rep 13, 4546 (2023). https://doi.org/10.1038/s41598-023-30854-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30854-y
This article is cited by
-
Interdisziplinäre multimodale Schmerztherapie bei Kopfschmerzerkrankungen
Der Schmerz (2024)
-
Challenging the "Topical Medications-First” Approach to Glaucoma: A Treatment Paradigm in Evolution
Ophthalmology and Therapy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.