Abstract
Little is currently known about the effect of smoking on osteoarthritis (OA). This study aimed to investigate the relationship between smoking and OA in the United States (US) general population. Cross-sectional study. Level of evidence, 3. 40,201 eligible participants from the National Health and Nutrition Examination Survey 1999–2018 were included and divided into OA and non-arthritis groups. Participants demographics and characteristics were compared between the two groups. Then the participants were divided into non-smokers, former smokers, and current smokers based on their smoking status, also demographics and characteristics among the three groups were compared. Multivariable logistic regression was used to determine the relationship between smoking and OA. The current and former smoking rate in the OA group (53.0%) was significantly higher than that in the non-arthritis group (42.5%; p < 0.001). Multivariable regression analysis including body mass index (BMI), age, sex, race, education level, hypertension, diabetes, asthma and cardiovascular disease showed that smoking was an association for OA. This large national study highlights a positive association between smoking and OA prevalence in the general US population. It is necessary to further study the relationship between smoking and OA in order to determine the specific mechanism of smoking on OA.
Similar content being viewed by others
Introduction
Osteoarthritis is a common disease in the elderly, characterized by progressive degeneration of articular cartilage, subchondral bone changes, and osteophyte formation1. OA is estimated to affect more than 240 million people worldwide, with more than 32 million estimated in the United States, resulting in a significant public health burden2. Based on data from the National Health Interview Survey, recently in the United States, there are approximately 14 million people who have symptomatic knee osteoarthritis of which approximately 3 million ethnic/racial minorities3. Thus, identifying potentially modifiable protective or risk factors may lead to the development of available strategies to delay the progression of OA and reduce the public health burden.
It is well-established that smoking is linked to chronic diseases such as diabetes, cardiovascular disease, and cancer. It is also a recognized risk factor for many chronic musculoskeletal diseases, including rheumatoid arthritis, degenerative disc disease, and low back pain. However, smoking is reportedly negatively associated with ulcerative colitis and Parkinson's disease. The relationship between smoking and OA has not been established4. Many clinical studies in different regions and populations have shown that smoking is negatively associated with the incidence of OA1,5,6,7. There is some evidence suggesting that the BMI of non-smokers is usually higher than that of smokers, leading to a high OA prevalence8,9. However, some scholars have raised doubts on the protective effect of smoking on OA observed in some epidemiological studies due to selection bias, especially hospital selection bias10. In a cross-sectional research of nationally representative data from South Korea, no association was found between direct smoking and previous smoking with the prevalence of OA11. A cross-sectional study from Denmark also found no association between current smoking and knee OA prevalence12. Given that the relationship between smoking and OA remains unclear, the results vary widely among different populations and regions. There are still contradictions and inconsistencies in the relationship between smoking and OA risk. In addition, few studies have examined in detail the relationship between current and former smokers and OA.
Therefore, this study aimed to explore the relationship between smoking and previous smoking on OA among US adults using national cross-sectional data. It also offered a valuable opportunity for assessing the potential of pooling OA preventive health information.
Methods
Study population data
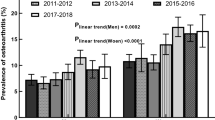
Data from ten discrete 2-year cycles (1999–2000 to 2017–2018) of the continuous National Health and Nutrition Examination Survey were used to examine the association of OA with smoking and BMI in US adults. NHANES (http://www.cdc.gov/nchs/nhanes.htm) is a national cross-sectional health survey in the US that collects laboratory, imaging, and radiological data in addition to health interviews and examination data13. Importantly, the Center for Disease Control (CDC) and Prevention uses a complex multi-stage probabilistic sampling design to examine a nationally representative sample across the country every 2 years. The NHANES study protocol has been approved by the Ethics Review Board of the National Center for Health Statistics (NCHS) Research, and all adult participants provided written informed consent. All studies were carried out in accordance with the Declaration of Helsinki. Details on Institutional Review Boards of the CDC and NCHS are available at (http://www.cdc.gov/nchs/nhanes/irba98.htm). Given the thoroughness of its methodology, NHANES data have been widely used to assess risk factors and prevalence of many diseases14. In this study, 116,876 participants older than or equal to 20 were selected from 1999 to 2018 NHANES (As shown in Fig. 1). Participants without OA data and with other types of arthritis were excluded. Participants with missing smoking, BMI, and other covariate data were also excluded.
OA criteria
The NHANES Medical Conditions Questionnaire is usually based on the "Medical condition" questionnaire of the American National Health Interview survey, and the OA status is investigated and collected. Participants are asked, "Has a doctor or other health professional ever told (you/s/he) that (you/s/he) . . .had arthritis?" If the answer to that question is "yes" the next question is "What type of arthritis was it?". Based on the different responses to these two questions, participants were divided into an OA group (solely had OA), other arthritis participants (which were excluded from further analysis) and no-arthritis group. Self-reported doctor-diagnosed OA is the most predominantly used case definition in epidemiological studies14. The agreement between self-reported OA and clinically confirmed OA was 81% in a previous study15.
Assessment of smoking volume, and other covariates
Variables associated with clinical characteristics were collected through physical examinations and self-reported questionnaires. Participants were divided into three categories based on their smoking status: never smokers (smoked less than 100 cigarettes in life), past smokers (smoked more than 100 cigarettes in life and smoke not at all now), and current smokers (smoked moth than 100 cigarettes in life and smoke some days or every day). The BMI (kg/m2) was recorded for all examinees by a trained examiner in the mobile examination center. According to the National Institutes of Health (NIH) guidelines16, BMI was divided into four grades: underweight (< 20.0 kg/m2), normal weight (20.0–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥ 30.0 kg/m2). Cardiovascular disease (CVD) included coronary heart disease, congestive heart failure, heart attack, stroke, and angina. Other covariates included discrete variables (sex, race/ethnicity, education, hypertension, diabetes mellitus (DM), asthma and marital status) and continuous variables (age, poverty status (family income to poverty ratio, PIR).
Statistical analyses
Data were processed by SPSS version 22.0 and R version 4.1.3. The Chi-square test was used to compare the constituent ratios of each group. Continuous variables were compared using Student's t-test or one-way analysis of variance (ANOVA), followed by multiple post-hoc comparisons using least significant difference (LSD), selected based on Levene statistics in the homogeneity of variance test. Variables with a p-value < 0.25 during univariate analysis were included in multivariable logistic regression analysis17. After adjusting for all covariables, logistic regression was performed to assess the association between smoking and OA. A p-value < 0.05 (two-sided) was statistically significant.
Results
Characteristics of participants
Participants younger than 20 years of age were excluded based on the epidemiological characteristics of OA. The prevalence of OA was 12.49% (n = 5022/40,201). The demographics and characteristics of participants in this study are shown in (Table 1).
We found that OA was more common in older women (age ≥ 50), the average age of the OA group was significantly higher than the non-arthritis group (63.92 ± 13.31 vs. 45.45 ± 16.97, p < 0.001), and the proportion of females with OA was higher than males (63.74% vs. 36.26%). The proportion of obese patients in the OA group was significantly higher than in the non-arthritis group (46.85% vs. 33.83%), and the proportion of non-Hispanic White also increased significantly (64.26% vs. 41.15%). At the same time, OA was associated with a higher level of education and annual household income. Besides diabetes, the prevalence of other comorbidities in the OA group was significantly higher than in the non-arthritis group (p < 0.001). Most importantly, the proportions of non-smokers and smokers in the OA group were lower than in the non-arthritis group, but the proportion of former smokers was significantly higher in the OA group (36.78% vs. 21.52%, p < 0.05).
Characteristics of participants by smoking status
The 40,201 participants were divided into never-smokers (n = 22,584), former smokers (n = 9419) and current smokers (n = 8198). The characteristics of 40,201 participants are shown in (Table 2).based on their smoking status. The average age of former smokers was the highest, and the average age of current smokers was the youngest (56.08 ± 17.12 vs. 42.96 ± 15.07 vs. 46.03 ± 17.59, p < 0.001). Never-smokers were predominantly women (57.59%). Compared with never-smokers, former smokers had a higher BMI, and current smokers had a lower BMI (28.89 ± 6.87 vs. 29.38 ± 6.43 vs. 27.90 ± 6.71, p < 0.001). This finding suggests that smoking may lead to a decrease in BMI, and quitting smoking increases BMI. Current smokers were associated with significantly lower levels of education, family income, and single status (including separated, divorced, widowed, and not being married, p < 0.001). In addition to asthma (smoking is considered an important risk factor) and CVD, other underlying diseases: hypertension, diabetes, smokers had significantly lower rates than non-smokers and quit smoking people (p < 0.001). Quit smoking people also had a higher prevalence of comorbidities than current smokers, which may be attributed to the fact that past smokers quit smoking after being diagnosed with comorbidities. The incidence of OA in the smoking group was 2.089 times higher than in the non-smoking group.
Association between OA and smoking
Figure 2 shows the crude and adjusted odds ratios for the association between OA and smoking. In the crude model, the smoking status was statistically significantly associated with OA as a categorical variable. The incidence of OA in the former smoker group was 2.09 times higher than in the non-smoker group (OR = 2.09, 95%CI 1.96–2.23, p < 0.001). However, there was no significant difference between the smoker and non-smoker groups (OR = 0.94, 95%CI 0.87–1.03, p = 1). After adjusting for age, gender, BMI, race, education, PIR, marital state, hypertension, diabetes, CVD, asthma, both current smoker and former smoker groups were associated with increased risk of OA compared to the non-smoker group (OR = 1.54, 95%CI 1.40–1.70, p < 0.001 and OR = 1.38, 95%CI 1.27–1.49, p < 0.001, respectively).
Discussion
Herein, we conducted a comprehensive study of OA using a large multi-year sample from NHANES 1999–2018. Indeed, previous knee OA studies on the NHANES database have been published in the literature, but one study was too old (being published in the 1970s), with a small number of participants and only cross-sectional associations between knee OA and various putative risk factors were explored18, and some studies did not focus on the relationship between smoking and OA19,20,21. The strength of this research is the numerous OA patients identified from a US population-based cross-sectional cohort. Another advantage is that, since they are acquired in the community, a lack of selection bias in exposure is assumed. Accordingly, we sought to explore the association between smoking and quitting smoking and OA. In the crude model, quitting smoking has a positive correlation with OA, while smoking has no correlation with OA. However, in our multivariable analysis model, which included variables measured in NHANES such as age, sex, BMI, and underlying disease to minimize the possibility of spurious association, we substantiated that current and past smokers had a higher risk of OA. The increased risk of OA attributed to smoking was not decreased significantly after quitting smoking (OR = 1.54, 95%CI 1.40–1.70, p < 0.001 and OR = 1.38, 95%CI 1.27–1.49, p < 0.001, respectively), continuing to smoke was associated with a greater risk of OA than in former smokers. Our study points out that high BMI and advanced age are significant risk factors for OA, and that women are at higher risk than men, which is consistent with previous reports22,23. In addition, our study shows that education level and underlying diseases such as hypertension and diabetes are also related to OA.
Large cohort studies based on the general population of the United Kingdom have shown that a weight gain of 4–5 kg after 12 months of smoking cessation may lead to increased knee degenerative disease8. Consistently, cohort studies in the Korean population have shown that a decrease in BMI caused by smoking may account for the protective effect of smoking against OA1. In accordance with previous studies, in this study, we found that an increase in BMI in former smokers and smoking led to a decrease in BMI. Among smokers, the proportion of overweight and obese people is 63.6%, which is the lowest among the three groups; among ex-smokers, the proportion of overweight and obese people is 75.9%, which is the highest among the three groups; among non-smokers, the proportion of overweight and obese people is 69.2%, the difference was statistically significant. However, after adjusting for BMI, a confounding factor, we still found a positive association between smoking and OA.
Smoking has been documented to exert heterogeneous effects on OA in different countries and regions. For example, smoking was found to be a protective factor against joint replacement with severe knee OA in a Singaporean Chinese cohort5. A cohort study on a Rotterdam population further showed that smoking was a risk factor for OA24. The reliability of many studies that concluded that smoking is a protective factor for OA was questioned due to study design bias. Indeed, hospital-based studies represent a significant source of bias. Smoking is more likely to cause health problems, which led to more non-osteoarthritis patients who smoke being included in the study10. It is widely established that the U.S. population is dominated by non-Hispanic whites. During multivariable regression analysis, the risk of OA in non-Hispanic whites was 2.39 times higher than in Mexican Americans. We suspect that the effects of smoking on different ethnic groups may lead to regional variations in studies. A multicenter trial in 2022 found an increased risk of gastrointestinal metaplasia (GIM) among Hispanics born outside the United States, but not among Hispanics born in the United States25. This finding suggests that members of the same ethnic group, born and living in different areas, may have different susceptibility to the same risk factors. Accordingly, the effect of smoking on OA varies across countries and regions.
At present, the exact mechanism between smoking and OA is poorly understood. Interestingly, studies have shown that nicotine alters 19 proteins, including several proteases and cytokines, in models of joint inflammation, including increased nicotine secretion of matrix metalloproteinase 1 and increased secretion of two proposed markers of OA, chitinase 3-like protein 1 fibronectin. Indeed, it is essential to increase awareness of the risk of OA, prevent its occurrence and improve the quality of life of this patient population. Current evidence suggests that age is the most significant risk factor for OA after age 30. In addition, the risk of OA was also significantly correlated with BMI, gender and race. Our findings suggest that people should reduce their smoking to reduce their risk of OA. In addition smoking causes a variety of harmful effects of carcinogens and chemicals.
The strengths of this study included its large-scale nature, the use of national cohort data, and the absence of selection bias. However, although NHANES is a representative sample of the general population in the United States, this is a cross-sectional study, which requires further validation of the effect of smoking on OA in prospective studies. In addition, a questionnaire was used to determine whether the participants were OA patients. Although the response rate was 81%, the gold standard for determining OA was imaging, and no physical examination was performed to determine whether participants had OA. And the absence of other covariates, such as job strain, physical activity, vitamin C, D, and K levels, and subsequent multivariate analysis in NHANES was also a limitation. Besides, we did not quantify smoking to explore the influence of the amount of smoking on the incidence of OA. However, we demonstrated that smoking increases the risk of OA in current smokers and past smokers based on data from a large population.
Conclusion
This large national cross-sectional study showed that smoking is positively associated with the prevalence of OA in the US population. It is necessary to further study the relationship between smoking and OA to determine the specific mechanism of smoking on OA.
Data availability
The datasets generated during the current study are available in the NHANES repository (http://www.cdc.gov/nchs/nhanes.htm).
References
Kwon, H. M. et al. Cigarette smoking and knee osteoarthritis in the elderly: Data from the Korean National Health and Nutritional Examination Survey. Exp Gerontol 133, 110873 (2020).
Katz, J. N., Arant, K. R. & Loeser, R. F. Diagnosis and treatment of hip and knee osteoarthritis: A review. JAMA 325(6), 568–578 (2021).
Vina, E. R. & Kwoh, C. K. Epidemiology of osteoarthritis: Literature update. Curr. Opin. Rheumatol. 30(2), 160–167 (2018).
Silverwood, V. et al. Current evidence on risk factors for knee osteoarthritis in older adults: A systematic review and meta-analysis. Osteoarthr. Cartil. 23(4), 507–515 (2015).
Leung, Y. Y. et al. Cigarette smoking and risk of total knee replacement for severe osteoarthritis among Chinese in Singapore–the Singapore Chinese health study. Osteoarthr. Cartil. 22(6), 764–770 (2014).
Takiguchi, R. et al. Modifiable factors associated with symptomatic knee osteoarthritis: The Murakami cohort study. Maturitas 128, 53–59 (2019).
Kong, L., Wang, L., Meng, F., Cao, J. & Shen, Y. Association between smoking and risk of knee osteoarthritis: A systematic review and meta-analysis. Osteoarthr. Cartil. 25(6), 809–816 (2017).
Zeng, C. et al. Does smoking cessation increase risk of knee replacement? A general population-based cohort study. Osteoarthr. Cartil. 29(5), 697–706 (2021).
Järvholm, B., Lewold, S., Malchau, H. & Vingård, E. Age, bodyweight, smoking habits and the risk of severe osteoarthritis in the hip and knee in men. Eur. J. Epidemiol. 20(6), 537–542 (2005).
Hui, M., Doherty, M. & Zhang, W. Does smoking protect against osteoarthritis? Meta-analysis of observational studies. Ann. Rheum. Dis. 70(7), 1231–1237 (2011).
Kang, K. et al. Association between direct and indirect smoking and osteoarthritis prevalence in Koreans: A cross-sectional study. BMJ Open 6(2), e010062 (2016).
Johnsen, M. B. et al. The association between smoking and knee osteoarthritis in a cohort of Danish patients undergoing knee arthroscopy. BMC Musculoskelet. Disord. 20(1), 141 (2019).
Dillon, C. F. & Weisman, M. H. US national health and nutrition examination survey arthritis initiatives, methodologies and data. Rheum. Dis. Clin. North Am. 44(2), 215–265 (2018).
Xu, Y. & Wu, Q. Trends and disparities in osteoarthritis prevalence among US adults, 2005–2018. Sci. Rep. 11(1), 21845 (2021).
Li, Y. et al. Associations of urinary levels of phenols and parabens with osteoarthritis among US adults in NHANES 2005–2014. Ecotoxicol. Environ. Saf. 192, 110293 (2020).
Clinical Guidelines on the Identification. Evaluation, and treatment of overweight and obesity in adults-the evidence report. National Institutes of Health. Obes. Res. 6(Suppl), 2 (1998).
Bursac, Z., Gauss, C. H., Williams, D. K. & Hosmer, D. W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 3, 17 (2008).
Anderson, J. J. & Felson, D. T. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am. J. Epidemiol. 128(1), 179–189 (1988).
Berry, K. M. et al. Obesity progression between young adulthood and midlife and incident arthritis: A retrospective cohort study of US adults. Arthr. Care Res. (Hoboken) 73(3), 318–327 (2021).
Hoeven, T. A. et al. Association of atherosclerosis with presence and progression of osteoarthritis: the Rotterdam Study. ANN. RHEUM. DIS. 72(5), 646–651 (2013).
Zertuche, J. P. et al. Alkylresorcinol, a biomarker for whole grain intake, and its association with osteoarthritis: The MOST study. Osteoarthr. Cartil. 30(10), 1337–1343 (2022).
Johnsen, M. B. et al. The mediating effect of body mass index on the relationship between smoking and hip or knee replacement due to primary osteoarthritis. A population-based cohort study (the HUNT Study). PLoS One 12(12), e0190288 (2017).
Sudo, A. et al. Prevalence and risk factors for knee osteoarthritis in elderly Japanese men and women. J. Orthop. Sci. 13(5), 413–418 (2008).
Szilagyi, I. A., Waarsing, J. H., Schiphof, D., van Meurs, J. B. J. & Bierma-Zeinstra, S. M. A. Towards sex-specific osteoarthritis risk models: Evaluation of risk factors for knee osteoarthritis in males and females. Rheumatology (Oxford) 61(2), 648–657 (2022).
Tan, M. C. et al. Race/ethnicity and birthplace as risk factors for gastric intestinal metaplasia in a multiethnic united states population. Am. J. Gastroenterol. 117(2), 280–287 (2022).
Funding
This work was funded by Medical Science and Technology Project of Zhejiang Province (Grant Number: 2020KY018, 2021KY028), Basic Public Welfare Research Program of Zhejiang Province (Grant Numbrer: LGF22H060029), National Natural Science Foundation of China (Grant Number: 81672769).
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, S., Ji, L., He, Z. et al. Association of smoking and osteoarthritis in US (NHANES 1999–2018). Sci Rep 13, 3911 (2023). https://doi.org/10.1038/s41598-023-30644-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30644-6
This article is cited by
-
Ideal cardiovascular health metrics have better identification of arthritis
BMC Public Health (2024)
-
Is occupational noise associated with arthritis? Cross-sectional evidence from US population
BMC Public Health (2024)
-
Circulating Copper Is Associated with Inflammatory Biomarkers in Greek Older Adults with Osteoarthritis
Biological Trace Element Research (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.