Abstract
According to World Health Organization (WHO), currently, 2.2 billion people are living with visual impairment worldwide, of which almost half could have been prevented. There are both modifiable and unmodifiable factors leading to visual disability and, ultimately, blindness. Several population-based studies in different parts of Iran have tried to determine these factors concerning their specific population and environment-related characteristics. AZAR Eye and Vision cohort is the second-largest cohort study in the whole country. AZAR Eye and Vision cohort is the ophthalmologic branch of AZAR cohort which is the largest eye cohort study in the country, which is trying to determine the prevalence and incidence of visual impairment, blindness, and other major ophthalmologic conditions and their associated risk factors in East Azerbaijan province located in Iran, a middle eastern country. A recently emerging phenomenon is the drying of the ultra-salty lake of Urmia located in the West Azerbaijan province which is a direct neighbor of our studied population and has caused recurrent salt storms in the immediate near areas. This phenomenon could adversely affect visual health via different conditions which our study will elucidate. The enrollment phase took place between 2014 and 2017 and 11,208 participants were enrolled out of 15,000 participants in the primary cohort. The resurvey phase will begin five years after the enrollment phase. In this phase, 30% of the participants are randomly selected to be reexamined and complete questionnaires. The participants showing any issues such as diabetes and being a glaucoma suspect will be included in the resurvey phase, too. Data categories gathered include demographics, lifestyle factors, past medical and drug histories, and a diet quality and quantity questionnaire including 130 edible items. Urine, hair, nail, and 25-ml blood samples, were collected from the participants. Then they were referred to an optometrist to complete an ophthalmologic questionnaire and undergo eye examination and lensometry. Then they underwent slit-lamp examinations and pictures were taken of the lens and fundus. People with suspected visual impairment were referred to an ophthalmology clinic. The data are processed and a four-level quality check is performed on each block. The most common visual impairment is cataracts. This study’s most important aim is to evaluate the effect of local environmental and ethnic factors on eye diseases in this specific population.
Similar content being viewed by others
What was the purpose of the cohort?
Visual impairment is a global health issue that is linked to a variety of functional and mental comorbidities. According to the World Health Organization, almost 2.2 billion people worldwide have vision impairment, with 36 million blind1. Visual abnormalities are preventable and treatable in about 80% of cases. As a result, several studies have been done to discover modifiable factors related to visual impairment2, and various preventative programs have been established based on these findings to prevent this issue. However, previous research has found that the prevalence of vision impairment and blindness is heavily influenced by ethnicity and environmental factors. As a result, determining the size and epidemiology of visual impairments and their risk factors in each location is critical for developing appropriate and successful strategies to address this problem.
In this context, a small number of population-based ocular studies in different parts of Iran attempt to answer this topic. The "Tehran eye study" is one of Iran's most significant eye studies, done in Tehran province [the country's capital city] with no follow-up phases3. However, prospective cohort studies are needed to better demonstrate the causation relationship for vision impairment and examine the gene-environment interaction. The Shahroud eye cohort was done on a 40–64-year-old population in North East Iran to determine the prevalence of eye illnesses and their prognosis and determinants4. Given that Iran is home to a diverse range of ethnic groups and distinct environmental risk factors in different parts of the country, it appears necessary to investigate genetic and environmental risk factors in each location. In this context, the Persian eye cohort study and the Persian cohort study in several regions of Iran, including the northwest, began in 2014. East Azerbaijan, located in Iran's northwestern corner, has recently experienced an environmental disaster in Lake Urmia (one of the largest salt lakes). It's been suggested that the Urmia lake drying in this area is linked to various health issues. There is a rare study regarding the effect of this disaster on the health status of the population in this region. The pilot study results indicated that Urmia lake drying provokes hypertension and anemia5. Hypertension increases the risk of some eye diseases such as cataracts6 and glaucoma7.
Moreover, there are reports that salt dust storms contain potentially toxic components which could threaten human health. According to the suggestion of all studies in this field, conducting well-designed prospective studies are necessary5,8,9. Therefore, the AZAR Eye and Vision cohort study aimed to determine environmental risk factors for eye diseases by comprehensively assessing external exposures, lifestyle (including physical activity, and dietary patterns), social determinants, and ethnic and individual characteristics; and to design population-based prospective studies of causal disease mechanisms by using the advantage of natural changes in regions of rapid environmental and social transition.
Who is a member of the cohort?
The AZAR cohort is a long-term cohort study of non-communicable diseases and associated risk factors in the Shabestar county of East Azarbaijan province, near the Urmia Lake in Iran's northwest10. The research included an epidemiologic investigation of eye disease among residents aged 35 to 70, which started in 2014 and concluded in 2017.
The AZAR cohort is a large population-based cohort that is part of the PERSIAN Cohort Study (Prospective Epidemiological Research Studies in Iran, ethics number: IR.TUMS.DDRI.REC.1396.1)11. The Ethical Committee of Tabriz University of Medical Sciences has authorized the AZAR cohort (record number: tbmed.rec.1393.205). We hereby confirm that all methods were performed in accordance with the with the declaration of Helsinki. All participants gave their written informed consent, and they were free to exit the study at any time and for any reason. The AZAR cohort population was detailed in further depth in the published cohort profile. Inclusion and exclusion criteria for AZAR Eye and Vision cohort study, are exactly the same as AZAR cohort study, previously published. The inclusion criteria was: (1) permanent or a minimum of 9 months residence each year in Shabestar district; (2) written informed consent; (3) at least one parent of Azeri ethnicity; and (4) age between 35 and 70 years at the time of enrollment in the study. Exclusion criteria was limited to having a disabling psychiatric condition or motor disability, which would limit effective cooperation with the interviewer or the examining physician.
The aims of the AZAR Eye and Vision cohort study were described to patients who participated in the AZAR Eye and Vision cohort study. When they agreed to participate in the AZAR Eye and Vision cohort, they were given an eye examination in addition to the AZAR cohort study protocols. Between October 2014 and June 2017, 11,028 people from the AZAR cohort took part in the AZAR Eye and Vision cohort study, out of 15,000 participants in the primary cohort. After six months, an optometrist and an ophthalmologist reexamined all individuals with diabetes (self-reported or newly confirmed diabetes) of 11,028 subjects.se
How often have they been followed up?
The study's enrollment phase was finished in February 2017. The study's resurvey phase was expected to begin five years following the enrolment phase but has been delayed due to the COVID-19 worldwide pandemic. In the interval between enrollment and resurvey phase completion, all participants are contacted by phone once a year. They've been questioned about all of their health-related problems including eye related problems (any newly diagnosed eye disease or any systemic diseases affecting the eyes, newly performed eye surgeries, ophthalmologist visits of any kind or any eye related hospital admissions) and finally they have been consulted on whether or not they should be referred to an ophthalmologist. One of the main purposes of these annual phone follow-ups between the enrollment and resurvey phase and the targeted questions surveyed during these contacts were to better assess for any possible detrimental effects of the drying of the Lake Urmia, on eye and visual health of the residents. As the drying of an ultra-salty lake is an extremely rare ecologic event in a human habited area, throughout the history, it makes this cohort very unique in its ability to register any possible correlation between eye diseases and this change; hence we have designed the study in a manner to minimize the possibility of missing any cause-and-effect relationship.
In the resurvey phase, thirty percent of the enrollment phase population will be randomly selected for reexamination by optometrists and ophthalmologists and completion of all enrollment phase questionnaires. All participants who had any concerning issue found in phase 1 (including diabetes, abnormal fundus or slit photo, any eye disease resulting in visual acuity < 7/10, being glaucoma suspect) will be followed up regardless of being included in the randomly selected 30% or not.
What has been measured?
Because this study is part of the AZAR cohort study, a large amount of information was gathered during the enrolling phase. The interviews were conducted using a block design, elaborated upon in great detail in prior published articles10. The following is a summary of the data gathered:
The most common data categories include demographics, socioeconomic status, lifestyle factors (such as physical activity and substance use), occupational history (including occupational exposures), past medical history, medicine use (past and present), family medical history including family history of eye diseases, gynecological and obstetrics history (for women), oral and dental health, circadian rhythm, and dietary habits (including food processing, water supply, housing, cellphone use, pesticide exposure). A food frequency questionnaire is employed to evaluate dietary consumption, consisting of 130 items such as bread and cereals, meats, dairy products, oils, sweets, legumes, vegetables, fruits, and sauces. Height, weight, waist, hip, wrist circumferences, and blood pressure were all measured (systolic and diastolic). In this study, participants' socioeconomic status was evaluated as the Wealth Score Index (WSI). Based on possession of a range of durable assets (for example, dishwasher, car, and TV), house condition (e.g., the number of rooms, type of ownership), and educational levels, WSI was calculated by Multiple Correspondence Analysis (MCA). WSI was classified into five WSI quintiles, ranging from the lowest to the highest ones (1st to 5th quintile, respectively).
Biological specimen
After an overnight fast of 12–14 h, 25-ml blood samples are drawn from peripheral veins, and serum, plasma, and buffy coat are separated. For future biochemical testing, the materials are kept at − 80 °C in two-dimensional barcoded aliquots. Following sample collection, biochemical parameters such as serum fasting blood glucose (FBS), complete blood count (CBC), blood urea nitrogen (BUN), creatinine, lipid profiles (total cholesterol, low- and high-density lipoprotein, triglyceride), and liver enzymes (aspartate, alanine, and gamma-glutamyl aminotransferase) are measured. Urine tests are performed. Urine, hair, and nail samples are collected and stored.
Section on ophthalmology
Participants were referred to an optometrist after completing all modules. The optometrist initially filled up a questionnaire for each individual, which consisted of seven questions and sixteen items. Information about the participants' medical conditions, such as diabetes history, family history of eye diseases like glaucoma, retinal detachment, keratoconus, and retinitis pigmentosa (RP) were noted in this questionnaire. In addition, the next section of the questionnaire asks about glasses/contact lens wearing, dry eye symptoms, amblyopia treatment, eye surgeries or procedures (such as cataract surgery, any type of laser photocoagulation therapy (including Pan-Retinal Photocoagulation [PRP]) for Proliferative Diabetic Retinopathy (PDR), corrective surgeries for refractive eye errors, glaucoma surgery, etc.), eye care and optometry appointments. The optometrist conducted an eye examination once the questionnaire was completed.
Examinations by an optometrist
During the trial, a single trained optometrist examined the participants' eyes. Lensometry of present glasses, measuring distance visual acuity, determining objective and subjective refraction, assessing eye movement, measuring IOP (intraocular pressure), and gross examination of lid lesions were all part of an optometry examination.
Lensometry
The non-automatic analog Topcon lensometer was used to assess the participants' spectacles if any were present (Topcon Corporation, Tokyo, Japan).
Visual acuity
The Snellen chart projector (CP-770, NIDEK, Japan) was used to determine uncorrected visual acuity (VA). As per the Persian cohort methodology, the right eye was measured first (submitted article|). The testing was done at a 6-m distance. The vision testing began at the top of the chart and proceeded until more than half of the letters were misread or the patient read all of the letters.
Refraction
The NIDEK Autorefractometer (AR1, NIDEK, and Japan) was initially used to assess non-cycloplegic autorefraction in the right eye. Reports of the sphere, cylinder, and axis were recorded automatically for each eye. In this section, the poor red reflex (PRP) and scissor motion (SM) of each participant were evaluated by optometrists.
Relative afferent pupillary defect test (RAPD)
The presence of Relative afferent Pupillary Defect (RAPD) in the AZAR Eye and Vision cohort population was checked using the swinging light test. This method was described briefly here and was explained in more detail in the other article (in press). After dimming the room's lighting, the light source from a direct ophthalmoscope (BETA ®200, HEINE, Germany) was held on each pupil for at least 3 s. Based on the simultaneous dilatation of both pupils, RAPD was defined.
Intraocular pressure
Goldman applanation tonometry (OPTILASA, Spain) was used to determine IOP. Each eye was measured once, with the right eye being measured first.
Other examination
Corneal opacities and eyelid lesions, such as ptosis, entropion, ectropion, etc., were evaluated by slit-lamp (SL-3G, TOPOCON, Japan).
Ocular photography
We took slit-lamp pictures of the lens and fundus for this study. A Topcon SL-3G Photo slit lamp (SL-3G, TOPOCON, Japan) was used for slit-lamp and lens photography. Slit-lamp photography is a photograph of the eye, including the lid margins, cornea, and iris. Dilation was used to photograph the lenses. The nucleus focuses on one photo, while the lens is retro illumination in the other. For fundus photography, we used a Digital Retinal Camera (CR2-AF Canon Japan) according to the Early Treatment Diabetic Retinopathy Study (ETDRS). In nondiabetic individuals, we took three conventional pictures from the first three ETDRS fields and one stereoscopic image from the optic nerve in each eye. Both eyes of diabetic patients were photographed using the ETDRS seven-standard field method. After maximum dilation of the pupils with mydrax 1% to each eye, two pictures were obtained using a digital fundus camera (CR2-AF Canon Japan) coupled with a 90-diopter lens camera (Volk Digital Wide Field ®, USA) according to the cohort protocol. At a 45° angle, all patients had two-field macula-centered fundus imaging. Participants were separated into three groups once the optometrists completed all necessary steps: normal, a requirement for spectacles, or referral to an ophthalmologist.
Criteria for referral
A comprehensive ophthalmic examination was performed on all who were referred. Diabetic, family history of glaucoma, IOP > 20 mmHg, Relative afferent pupillary deficit (RADP+), best-corrected visual acuity (BCVA) < 8/10, poor red reflex, moderate to severe dry eye symptoms, suspicion of scissor reflex, eyelid abnormalities and any other suspicious findings were among the criteria used by the optometrist to refer patients to an ophthalmologist.
Ophthalmologic examination
Those who were referred to an ophthalmologist underwent a thorough examination. First and foremost, the ophthalmologist examined the client's eyes with the naked eye. Examination of the eyelid (entropion, ectropion), lacrimal system, eyelid bulk, dry eye, extraocular muscles, and conjunctiva were among the items investigated. Slit-lamp biomicroscopy and intraocular pressure measurements were performed after these examinations. Dilatation of the pupils after pupil dilatation, clinical lens opacity grading, and vitreous examination was performed. The slit lamp was used to assess opacities, and direct and indirect ophthalmoscopy was used to examine the fundus. We employed an SL-3G, TOPOCON for slit-lamp (SL-3G, TOPCON, Japan).
After dilatation, lens opacity grading was performed at the slit lamp in addition to lens photography. The ophthalmologist used standard images from the WHO simplified cataract grading system to make comparisons. The ophthalmologist examined the retina and optic disc thoroughly and systematically with direct and indirect ophthalmoscopy, recording all findings.
Participants with resolvable eye issues were treated with the guidance and treatment of an ophthalmologist, or a treatment and follow-up program was established for them after a thorough ophthalmological examination.
People with suspected lesions, such as glaucoma or retinal disorders, were referred to an ophthalmology referral center for further diagnostic and treatment measures and counseling.
Quality control and data processing
A four-level quality check is performed on each block. A basic review is done by the software so that appropriate data are recorded in each part in terms of variable kinds, length, and measurement levels. The program conducts a basic check to verify that the correct data is captured in each questionnaire part. When information is missing, the operator is prompted to fill in the gaps. Furthermore, during the first phase, an independent staff member conducts frequent quality monitoring, which is monitored using a validated checklist. General inquiries, anthropometric measurements, medical and disease screening questionnaires, and biological sample collection and biobank maintenance are all examined by the team for each participant. If any information is missing or incomplete, the record will be indexed and sent to another team to finish. It is possible to import just verified entries into the database. An epidemiologist next evaluates the records. The quality control administrator, who is an AZAR principal investigator with full access to the whole records database, verifies the data at random. Moreover, the Persian cohort team performs central quality checks on quantitative data.
What has it found?
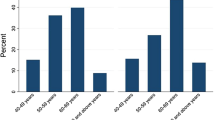
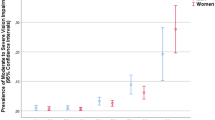
The baseline characteristics of the participant in the AZAR Eye and Vision cohort are presented in Table 1. As shown in Fig. 1, the most prevalent eye disease in males and females, at baseline was cataract 7.1% and 7.3% respectively. In Fig. 1, we observed that the prevalence of dry eye in females was significantly (P = 0.002) higher than males (0.3% vs. 0.04%). In both genders, the most prevalent family history of eye diseases was glaucoma (Fig. 2). Only 1% of the population has IOP > 21 mmHg (Table 2).
The frequency of using near and far glasses in females was significantly (P < 0.0001) higher than in males. Of 11,028 subjects, 2688 (23.9%) people were referred to an ophthalmologist by the optometrist.
The main reasons for referring to an ophthalmologist were BCVA < 8/10 (65.6%), diabetes (46.8%), suspicion of scissor reflex (4.4%), and IOP > 20 (4.6%).
What are the main strengths and weaknesses?
The AZAR Eye and Vision cohort study's key strength is the study's novel concept: to evaluate how a significant environmental change (natural changes at Lake Urmia) affects eye illnesses against a relatively steady genetic predisposition at a population level. The AZAR Eye and Vision cohort studies a population in a specific place with exact environmental change timing. As a result, it avoids several other studies' flaws. The ethnically homogeneous group of the AZAR Eye and Vision cohort will likely provide a higher capacity to test associations. AZAR Eye and Vision cohort is also the first and most extensive study to focus on people of Turkish descent. Another benefit of the experiment is a large amount of data obtained, which will aid in understanding ocular epidemiology and the possibility of investigating many possible correlations. Many procedures were used to ensure the quality of the data acquired. The study's drawback is that our sample size is limited to those aged 35 to 70; thus, issues at younger and older ages cannot be investigated.
Can I get ahold of the data? Where can I find out more?
The AZAR Eye and Vision cohort collaborates with foreign professionals to further strengthen national and international collaborations. It employs online communication methods, such as its website, to communicate information from the AZAR Eye and Vision cohort, raise project awareness, and attract international collaborators [http://azarcohort.tbzmed.ac.ir].
Ethics approval and consent to participate
This study was approved by the ethics committee of Tabriz University of medical sciences (tbzmed.rec.1393.205).
Data availability
The data that support the findings of this study are available from [Vice Chancellor for Research] but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of [Vice Chancellor for Research].
References
WHO.https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment 2021.
Brouwer, J. G. et al. Inflammatory potential of the diet and colorectal tumor risk in persons with Lynch syndrome. Am. J. Clin. Nutr. 106(5), 1287–1294 (2017).
Hashemi, H., Fotouhi, A. & Mohammad, K. The Tehran eye study: research design and eye examination protocol. BMC Ophthalmol. 3(1), 1–8 (2003).
Fotouhi, A. et al. Cohort profile: Shahroud eye cohort study. Int. J. Epidemiol. 42(5), 1300–1308 (2013).
Tabrizi, J. S. et al. Health consequences of Lake Urmia in crisis in the disaster area: A pilot study. Disaster Med. Public Health Prepar. 14(4), 442–448 (2019).
Yu, X., Lyu, D., Dong, X., He, J. & Yao, K. Hypertension and risk of cataract: A meta-analysis. PLoS ONE 9(12), e114012 (2014).
Mitchell, P., Lee, A. J., Rochtchina, E. & Wang, J. J. Open-angle glaucoma and systemic hypertension: The blue mountains eye study. J. Glaucoma 13(4), 319–326 (2004).
Schmidt, M., Gonda, R. & Transiskus, S. Environmental degradation at Lake Urmia (Iran): Exploring the causes and their impacts on rural livelihoods. GeoJ 86(5), 2149–2163 (2021).
Sadeghi-Bazargani, H., Allahverdipour, H., Jafarabadi, M. A. & Azami-Aghdash, S. Lakes drying and their adverse effects on human health: A systematic review. Iran J. Public Health 48(2), 227 (2019).
Farhang, S. et al. Cohort profile: The AZAR cohort, a health-oriented research model in areas of major environmental change in Central Asia. Int. J. Epidemiol. 48(2), 382-h (2019).
Poustchi, H. et al. Prospective epidemiological research studies in Iran (the PERSIAN Cohort Study): Rationale, objectives, and design. Am. J. Epidemiol. 187(4), 647–655 (2018).
Acknowledgements
The authors are grateful for the financial support of the liver and gastrointestinal diseases research center, at Tabriz University of Medical Sciences. The authors also are deeply indebted to all subjects who participated in this study. We appreciate the contribution of the investigators and the staff of the AZAR cohort study. We thank the close collaboration of the Shabestar health center. In addition, we would like to thank the Persian cohort study staff for their technical support.
Funding
This study was supported by the liver and gastrointestinal diseases research center, at Tabriz University of Medical Sciences. The funder had no role in the study design, data analysis, interpretation, and writing the manuscript in this study. Grant Number 700/108 on 14 March 2016. The Iranian Ministry of Health and Medical Education has contributed to the funding used in the PERSIAN cohort through Grant no.700/534.
Author information
Authors and Affiliations
Contributions
In the process of writing the main manuscript, preparing the table, and reviewing the manuscript, all Authors cooperated together equally.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Somi, M.H., Nikniaz, Z., Ostadrahimi, A. et al. AZAR eye and vision cohort study. Sci Rep 13, 7998 (2023). https://doi.org/10.1038/s41598-023-30212-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30212-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.