Abstract
Respiratory oscillometry is widely explored in asthma management; however, there is currently no consensus on its routine work-up in patients with difficult-to-treat asthma. We conducted a retrospective, cross-sectional study involving patients with difficult-to-treat asthma at Asia University Hospital between January 2017 and October 2020. We aimed to correlate clinical significance of respiratory oscillometry and asthma treatment outcomes including symptoms control and exacerbation in patients with difficult-to-treat asthma. Among the 69 patients enrolled in the study, a total of 26.1% of the patients experienced at least one severe or two moderate exacerbations. Patients with ACT < 20 presented a higher prevalence of higher frequency-dependent resistance (FDR; the difference in resistance at 5 Hz and 20 Hz) and frequency of resonance (Fres) than those with ACT ≥ 20. In the multivariable analysis, comorbidities, COPD or allergic rhinitis, and FDR were independent factors in increasing the odds ratio in poorly controlled asthma. (FDR ≥ 0.10 vs. < 0.10, adjusted ORR = 5.05, P = 0.037) There was a higher proportion of frequent exacerbations in patients with higher FDR (FDR ≥ 0.10 vs. < 0.10 = 30.0%:20.7%), but IOS parameters failed to predict frequent exacerbations on further analysis. FDR may be a potential clinical parameter for predicting symptom control in patients with difficult-to-treat asthma.
Similar content being viewed by others
Introduction
Asthma is characterized by chronic airway inflammation, which results in airway hyperresponsiveness, obstruction, mucus hyperproduction, and airway remodeling1,2,3. The prevalence and economic burden of asthma increase yearly, especially in poorly-controlled asthma4,5,6. The definition of poorly-controlled asthma is re-aligned in 2019 Global Initiative For Asthma (GINA) guideline, which conceptualizes “Uncontrolled asthma,” “Difficult-to-treat asthma,” and “Severe asthma”7. Once patients are diagnosed with difficult-to-treat asthma, modifiable factors such as adherence, inhaler technique, medication side effects, and comorbidities should be reviewed and corrected. Patients with persistent uncontrolled asthma after maximal optimal therapy and treatment of contributory factors within the window of time were diagnosed with severe asthma. The clinicians heavily use patients' self-reported symptoms in the clinical assessment of asthma control and treatment modifications8. Pulmonary function also provides clinicians with another aspect of disease control; however, the discrepancy between asthma control scores and pulmonary function tests existed in previous studies9,10. Spirometry is not well-correlated with symptoms, although low forced expiratory volume in one second (FEV1) is associated with the risk of exacerbation11,12,13. Mostly, patients presented suboptimal asthma control but preserved FEV114.
Oscillometry measures respiratory mechanics at different frequencies, such as airway resistance and reactance, to evaluate subtle changes in the small airway, inhomogeneity, and compliance of the peripheral lung. Performing oscillometry requires minimal effort and cooperation, which allows most patients to undertake the test, including children, elders, and people with disabilities15,16,17,18. Although exploring oscillometry is widely accepted in asthma diagnosis, symptom control, and phenotyping, the clinical significance and management of small airway dysfunction remain unclear and controversial19,20,21,22. There is no consensus on the routine detection of small airway abnormalities in patients with difficult-to-treat asthma. This study aimed to determine the potential oscillometry parameters that determine the difference between asthma patients with good or poor symptomatic control, focusing on those diagnosed with difficult-to-treat asthma.
Methods
Study population
We conducted a cross-sectional study in October 2021 and retrospectively collected 488 patients between January 2017 and October 2021 from the asthma case payment registry at the Asia University Hospital. (Fig. 1.) The following patients were excluded from the study: patients who received GINA step 1–3 therapy (n = 394); patients who were currently smokers (n = 1); patients under GINA step 4–5 treatment for less than 3 months (n = 1); patients who were ineligible for spirometry and impulse oscillometry tests (n = 9), or had an inappropriate effort of spirometry and impulse oscillometry (n = 14). The final study population comprised of 69 patients with difficult-to-treat asthma. This study was conducted in accordance with the principles of the Declaration of Helsinki. The Institutional Review Board of Feng Yuan Hospital, Minister of Health and Welfare, approved our study (no.110016) and waived the requirement for informed consent.
Assessment and data collection
Data regarding patient demographics, including age, sex, smoking history, medical treatment, immunological profiles (e.g., blood eosinophils before treatment and peak value during follow-up), fraction of exhaled nitrogen oxide (FeNO), serum IgE level, and allergen test results (Phadiatop and multiple antigen simultaneous tests) were collected from the electronic medical records. Spirometry and oscillometry data were obtained from patients who underwent GINA steps 4–5. We performed spirometry using MasterScreen Body/Diff (CareFusion, San Diego, CA, USA) and interpreted it according to the American Thoracic Society/European Respiratory Society guidelines23,24. We performed oscillometry using MasterScreen Impulse Oscillometry System (IOS; CareFusion, San Diego, CA, U.S.) and performed FeNO using NIOX VERO (Circassia, Oxford, U.K.) All procedures of spirometry and IOS fulfilled European Respiratory Society guidelines and we perform IOS before spirometry prior to and after administration of albuterol 400 mg, with acceptable test quality16,23.
Outcomes
Outcome measurements were through asthma symptom control score and exacerbation calculated from at least 3 months of GINA steps 4–5 treatment. We used the asthma control test (ACT), a 5-item, patient-centered survey for assessing asthma control25, a cutoff score of 20 points to define patients with well-controlled or poorly controlled symptoms. Asthma exacerbation was classified with different degrees of severity based on electrical medical records, wherein: severe exacerbation is defined as emergency department visits or hospitalization requiring systemic corticosteroids or increasing dose from baseline; moderate exacerbation is defined as deterioration in the patient’s symptoms or lung function beyond day-to-day variations requiring a change of medication but that do not meet severe criteria26,27. Patients with at least one severe or two moderate exacerbations are defined as having frequent exacerbations.
Statistical analyses
Categorical data from patients’ profiles were presented as numbers (%) and compared using Pearson’s chi-square test and Fisher’s exact test, as appropriate. Continuous variables are presented as means with standard deviation or median with interquartile range based on the Kolmogorov–Smirnov normality test, followed by Student’s t-test or the Mann–Whitney U test, respectively. Baseline characteristics of patients, spirometry, and IOS parameters were calculated using logistic regression for study endpoint analysis and multivariable analysis using significant variables (P < 0.20) in the multivariable logistic regression analysis. All tests were two-sided, and statistical significance was set at P < 0.05. All analyses were performed using SPSS software (version 25.0, IBM Corp., Chicago, IL, USA).
Ethical approval
The Institutional Review Board of Feng Yuan Hospital, MOHW approved this study [111018].
Results
Among the 69 patients enrolled, the median follow-up time was 1279 days. Of the total number of patients 49.3% were women, 65.2% were never-smokers, and 24 of 43 patients had positive allergen test results (26 patients didn’t perform allergen test). As for adjunctive therapy for asthma, all patients received long-acting muscarinic antagonists, 28 received leukotriene receptor antagonists, 16 received theophylline, and 14 received biological agents. Bronchodilator reversibility was observed in 16.1% of patients. Approximately 26.1% of patients experienced frequent exacerbations. Out of all the patients, 29.0% were diagnosed with chronic obstructive pulmonary disease (COPD), 26.9% with rhinosinusitis, and 14.5% with coronary artery disease. The demographic distribution of patients, categorized by an ACT score of 20 points, was not significantly different in terms of age, sex, medication, and other variables, but patients with poorly controlled asthma (ACT < 20) presented a higher prevalence of COPD (Table 1; see Supplementary Table 1 for detailed demographic profiles).
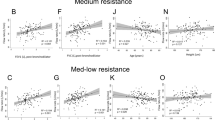
Spirometry and IOS studies showed that the poorly controlled asthma group had significantly higher frequency-dependent resistance (FDR; difference in resistance at 5 Hz and 20 Hz) and resonance frequency (Fres) than the well-controlled asthma group (ACT ≥ 20) (Fig. 2). In the multivariable logistic regression model, higher FDR was an independent factor in increasing the odds ratio in poorly-controlled asthma (adjusted OR = 453.67, P = 0.043) and other independent factors: comorbidities with COPD (adjusted OR = 15.03, P = 0.003) and rhinosinusitis (adjusted OR = 11.16, P = 0.006) (Supplementary Table 2).
Differences in parameters of spirometry and IOS between well- and poorly-controlled asthma. Abbreviation ACT, asthma control test; AX, reactance area; FDR, frequency-dependent resistance; difference in resistance at 5 Hz and 20 Hz; FEV1, forced expiratory volume in 1 s; Fres, resonance frequency; FVC, forced vital capacity; R5%pred, predicted percentage of resistance at 5 Hz.
In the ROC curve analysis for predicting poorly controlled asthma, FDR demonstrated acceptable accuracy, with an area under the ROC curve of 66.7%, and a 95% confidence interval of 52.8–80.5%. The optimal cutoff FDR was 0.10, with a sensitivity of 83.3% and a specificity of 52.3% (Supplementary Figure 1). In the multivariable logistic regression model, patients with FDR ≥ 0.10 presented a higher strength of association with poorly controlled asthma than those with FDR < 0.10 (FDR ≥ 0.10 vs. < 0.10, adjusted ORR = 5.05, P = 0.037) (Table 2).
Figure 3 shows the distribution of ACT scores and FDR in our study samples, labeled according to the presence of frequent exacerbations in 12 months. There was a higher proportion of frequent exacerbations in patients with low ACT scores and high FDR than in the other three groups. However, no significant differences were observed. Moreover, the IOS parameters in our study failed to predict frequent exacerbations in the multivariable analysis. (Supplementary Table 3).
Distribution of ACT score, FDR, and frequent exacerbations in the study population. Based on the distribution of ACT and FDR, 30% of patients with FDR ≥ 0.10 (dashed line) experienced frequent exacerbations (once per year of severe acute exacerbation or twice per year of moderate acute exacerbation), and 27.8% of patients with ACT < 20 (dashed line) experienced frequent exacerbations. There were higher proportions of frequent exacerbations in patients with FDR ≥ 0.10 and ACT < 20, but the statistical difference in group comparisons was not met. Abbreviation ACT, asthma control test; FDR, frequency-dependent resistance; difference in resistance at 5 Hz and 20 Hz.
Discussion
To date, there have been few studies on oscillometry parameters and asthma outcomes that have led to a similar conclusion19,20,28,29. Our study focused on evaluating oscillometry in patients with difficult-to-treat asthma and showed that FDR is an independent parameter associated with poor symptom control, irrespective of other comorbidities.
The goals of asthma management are to achieve optimum symptom control, reduce the future risk of exacerbations, optimize pulmonary functions, and minimize the adverse effects of medication. Assessment of clinical symptom scores is widely accepted in management of asthma. Previous studies used ACT as an appropriate measurement for various asthma outcomes8. However, we overestimated the clinical symptom scores of patients with poor perceptions or lack of knowledge regarding asthma control30,31. Clinical manifestations of asthma and the severity of airway inflammation remain imperfectly compatible. Pulmonary function is another aspect of clinical outcomes for the evaluation of airway remodeling. Previous reviews have claimed an association between spirometry and treatment outcome11,12,13,32; however, a discrepancy was still observed in several studies9,33. Patients with significant symptoms might have preserved FEV1 without fixed airway obstruction in real-world practice. Our results were consistent with those of previous studies and showed that the IOS parameters were more sensitive in predicting poor symptom control than spirometry in these patients20. Oscillometry requires minimal effort to perform and acts as an adjunctive tool for evaluating respiratory mechanics such as airway resistance and reactance. Regarding the instability of airway conditions in severe asthma patients, dynamic measurement of oscillometry parameters, including bronchodilator response and intrabreath difference, have proven to be effective in correlation to asthma outcomes29,34,35. Recent IOS studies have also explored the clinical utility of analyzing biological agents' therapeutic effects in severe asthma36,37. Pre- and post-treatment changes in IOS parameters could also indicate responsiveness38. Based on our findings and relevant studies, we suggest including oscillometry evaluation in the clinical assessment of difficult-to-treat asthma for the prognosis of symptom control and potential treatment responsiveness.
Although IOS parameters were associated with T2 inflammation and exacerbations in previous studies34,39,40, our data showed that IOS parameters did not significantly affect asthma exacerbations. Reports on performance variations among different devices should be taken into account. Previous studies have demonstrated variable respiratory impedance in the same model41. In the longitudinal outcomes of the ATLANTIC study, pre- and post-IOS parameter changes might predict the risk of exacerbation28. Moreover, lack of clinical data such as respiratory infection and allergen avoidance might also affect the data integrity of the analysis results.
However, our study has some limitations. First, it was a small, retrospective study with disproportional distributions of poorly- and well-controlled symptoms. Nonetheless, our findings are consistent with previous more extensive IOS studies, mainly focusing on patients undergoing GINA steps 4–5. Second, nearly 30% of patients had been diagnosed with COPD, and one-third of the patients were former smokers in our study population. The composition of patient demographics matches real-world practical scenarios rather than clinical trial settings. The selection bias between the exploration and management of comorbidities might have influenced clinical symptoms and treatment outcomes, such as pulmonary rehabilitation or consultation with other specialties. Despite these limitations, our study is representative of real-world experience. Further studies, in combination with imaging or pathology, are warranted to improve the clinical implications of IOS utility.
Conclusion
In conclusion, our study implies that IOS is more sensitive than spirometry in predicting poor symptom control in patients with difficult-to-treat asthma under GINA steps 4–5. The application of IOS in these patients might help clinicians evaluate disease control and biologic treatment responsiveness, which can significantly improve asthma management.
Data availability
All data that support the findings of this study are available from the corresponding authors, Huang, upon reasonable request.
References
Holgate, S. T. Innate and adaptive immune responses in asthma. Nat. Med. 18(5), 673–683. https://doi.org/10.1038/nm.2731 (2012).
Papi, A., Brightling, C., Pedersen, S. E. & Reddel, H. K. Asthma. Lancet. 391(10122), 783–800. https://doi.org/10.1016/S0140-6736(17)33311-1 (2018).
Hough, K. P. et al. Airway remodeling in asthma. Front. Med. (Lausanne). 7, 191. https://doi.org/10.3389/fmed.2020.00191 (2020).
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1204–1222 (2020).
Yaghoubi, M., Adibi, A., Safari, A., FitzGerald, J. M. & Sadatsafavi, M. The projected economic and health burden of uncontrolled asthma in the United States. Am. J. Respir. Crit. Care Med. 200(9), 1102–1112. https://doi.org/10.1164/rccm.201901-0016OC (2019).
Shantakumar, S. et al. Epidemiological, clinical and economic burden of severe eosinophilic asthma in Taiwan: Results from a large tertiary care hospital. Asian Pac. J. Allergy Immunol. https://doi.org/10.12932/AP-200220-0771 (2020).
Global Initiative for Asthma. Difficult-to-treat asthma and severe asthma in adolescent and adult patients. Diagnosis and Management. 2019. https://ginasthma.org/severeasthma/. Accessed 15 Oct 2021.
van Dijk, B. C. P. et al. Relationship between the asthma control test (ACT) and other outcomes: A targeted literature review. BMC Pulm. Med. 20(1), 79. https://doi.org/10.1186/s12890-020-1090-5 (2020).
Shirai, T., Furuhashi, K., Suda, T. & Chida, K. Relationship of the asthma control test with pulmonary function and exhaled nitric oxide. Ann. Allergy Asthma Immunol. 101(6), 608–613. https://doi.org/10.1016/S1081-1206(10)60223-2 (2008).
Park, S. Y. et al. Clinical factors affecting discrepant correlation between asthma control test score and pulmonary function. Allergy Asthma Immunol. Res. 7(1), 83–87. https://doi.org/10.4168/aair.2015.7.1.83 (2015).
Rosi, E., Ronchi, M. C., Grazzini, M., Duranti, R. & Scano, G. Sputum analysis, bronchial hyperresponsiveness, and airway function in asthma: Results of a factor analysis. J. Allergy Clin. Immunol. 103(2 Pt 1), 232–237. https://doi.org/10.1016/s0091-6749(99)70496-3 (1999).
Crimi, E. et al. Dissociation between airway inflammation and airway hyperresponsiveness in allergic asthma. Am. J. Respir. Crit. Care Med. 157(1), 4–9. https://doi.org/10.1164/ajrccm.157.1.9703002 (1998).
Kwon, J. W. et al. High ACT score is not sufficient to reduce the risk of asthma exacerbations in asthma with low lung function. Respir. Med. 150, 38–44. https://doi.org/10.1016/j.rmed.2019.02.010 (2019).
Lo, D. K. et al. Lung function and asthma control in school-age children managed in UK primary care: A cohort study. Thorax 75(2), 101–107. https://doi.org/10.1136/thoraxjnl-2019-213068 (2020).
Oostveen, E. et al. ERS Task Force on Respiratory Impedance Measurements. The forced oscillation technique in clinical practice: Methodology, recommendations and future developments. Eur. Respir. J. 22(6), 1026–41. https://doi.org/10.1183/09031936.03.00089403 (2003).
King, G. G. et al. Technical standards for respiratory oscillometry. Eur. Respir. J. 55(2), 1900753. https://doi.org/10.1183/13993003.00753-2019 (2020).
Bates, J. H. T., Irvin, C. G., Farré, R. & Hantos, Z. Oscillation mechanics of the respiratory system. Compr. Physiol. 1(3), 1233–1272. https://doi.org/10.1002/cphy.c100058 (2011).
Hellinckx, J., Cauberghs, M., De Boeck, K. & Demedts, M. Evaluation of impulse oscillation system: Comparison with forced oscillation technique and body plethysmography. Eur. Respir. J. 18(3), 564–570. https://doi.org/10.1183/09031936.01.00046401 (2001).
Jabbal, S., Manoharan, A., Lipworth, J. & Lipworth, B. Utility of impulse oscillometry in patients with moderate to severe persistent asthma. J. Allergy Clin. Immunol. 138(2), 601–603. https://doi.org/10.1016/j.jaci.2015.12.1336 (2016).
Chaiwong, W., Namwongprom, S., Liwsrisakun, C. & Pothirat, C. The roles of impulse oscillometry in detection of poorly-controlled asthma in adults with normal spirometry. J. Asthma. https://doi.org/10.1080/02770903.2020.1868499 (2021).
Abdo, M. et al. Small airway dysfunction links asthma severity with physical activity and symptom control. J. Allergy Clin. Immunol. Pract. 9(9), 3359-3368.e1. https://doi.org/10.1016/j.jaip.2021.04.035 (2021).
Chiu, H. Y. et al. Small airway dysfunction by impulse oscillometry in symptomatic patients with preserved pulmonary function. J. Allergy Clin. Immunol. Pract. 8(1), 229-235.e3. https://doi.org/10.1016/j.jaip.2019.06.035 (2020).
Miller, M. R. et al. Standardisation of spirometry. Eur. Respir. J. 26(2), 319–338. https://doi.org/10.1183/09031936.05.00034805 (2005).
Graham, B. L. et al. Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society technical statement. Am. J. Respir. Crit Care Med. 200(8), e70–e88. https://doi.org/10.1164/rccm.201908-1590ST (2019).
Nathan, R. A. et al. Development of the asthma control test: A survey for assessing asthma control. J. Allergy Clin. Immunol. 113(1), 59–65. https://doi.org/10.1016/j.jaci.2003.09.008 (2004).
Reddel, H. K. et al. American Thoracic Society/European Respiratory Society Task Force on Asthma Control and Exacerbations. An official American Thoracic Society/European Respiratory Society statement: Asthma control and exacerbations: Standardizing endpoints for clinical asthma trials and clinical practice. Am. J. Respir. Crit. Care Med. 180(1), 59–99. https://doi.org/10.1164/rccm.200801-060ST (2009).
Virchow, J. C. et al. Defining moderate asthma exacerbations in clinical trials based on ATS/ERS joint statement. Respir. Med. 109(5), 547–556. https://doi.org/10.1016/j.rmed.2015.01.012 (2015).
Kraft, M. et al. The role of small airway dysfunction in asthma control and exacerbations: A longitudinal, observational analysis using data from the ATLANTIS study. Lancet Respir. Med. 10(7), 661–668. https://doi.org/10.1016/S2213-2600(21)00536-1 (2022).
Chiabai, J. et al. Intrabreath oscillometry is a sensitive test for assessing disease control in adults with severe asthma. Ann. Allergy Asthma Immunol. 127(3), 372–377. https://doi.org/10.1016/j.anai.2021.06.005 (2021).
Chapman, K. R., Ernst, P., Grenville, A., Dewland, P. & Zimmerman, S. Control of asthma in Canada: Failure to achieve guideline targets. Can. Respir. J. 8(Suppl A), 35A-40A (2001).
van Schayck, C. P., van Der Heijden, F. M., van Den Boom, G., Tirimanna, P. R. & van Herwaarden, C. L. Underdiagnosis of asthma: Is the doctor or the patient to blame? The DIMCA project. Thorax. 55(7), 562–565. https://doi.org/10.1136/thorax.55.7.562 (2000).
van Dijk, B. C. P. et al. Relationship between the asthma control test (ACT) and other outcomes: A targeted literature review. BMC Pulm. Med. 20(1), 79. https://doi.org/10.1186/s12890-020-1090-5 (2020).
Schatz, M. et al. Asthma control test: Reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J. Allergy Clin. Immunol. 117(3), 549–556. https://doi.org/10.1016/j.jaci.2006.01.011 (2006).
Chan, R. & Lipworth, B. J. Oscillometry bronchodilator response in adult moderate to severe eosinophilic asthma patients: A prospective cohort study. Clin. Exp. Allergy. 52(9), 1118–1120. https://doi.org/10.1111/cea.14185 (2022).
Hantos, Z. Intra-breath oscillometry for assessing respiratory outcomes. Curr. Opin. Physiol. 22, 100441. https://doi.org/10.1016/j.cophys.2021.05.004 (2021).
Abdo, M. et al. Small airway dysfunction as predictor and marker for clinical response to biological therapy in severe eosinophilic asthma: A longitudinal observational study. Respir. Res. 21(1), 278. https://doi.org/10.1186/s12931-020-01543-5 (2020).
Chan, R., RuiWen Kuo, C. & Lipworth, B. Real-life small airway outcomes in severe asthma patients receiving biologic therapies. J. Allergy Clin. Immunol. Pract. 9(7), 2907–2909. https://doi.org/10.1016/j.jaip.2021.01.029 (2021).
Sugawara, H. et al. A retrospective analysis of usefulness of impulse oscillometry system in the treatment of asthma. Respir. Res. 21(1), 226. https://doi.org/10.1186/s12931-020-01494-x (2020).
Liu, L. et al. Study on small airway function in asthmatics with fractional exhaled nitric oxide and impulse oscillometry. Clin. Respir. J. 12(2), 483–490. https://doi.org/10.1111/crj.12548 (2018).
Kuo, C. R., Jabbal, S. & Lipworth, B. Is small airways dysfunction related to asthma control and type 2 inflammation?. Ann. Allergy Asthma Immunol. 121(5), 631–632. https://doi.org/10.1016/j.anai.2018.08.009 (2018).
Dandurand, R. J., Lavoie, J. P., Lands, L. C., Hantos, Z., Oscillometry Harmonisation Study Group. Comparison of oscillometry devices using active mechanical test loads. ERJ Open Res. 5(4), 00160. https://doi.org/10.1183/23120541.00160-2019 (2019).
Acknowledgements
The authors wish to thank all patients included in this study, as well as their families. The authors are also grateful to all the working staff at the Taipei Veterans General Hospital. The authors thank Banashree from Editage for English editing.
Funding
This research was funded by Asia University Hospital (Grant No. 11151015).
Author information
Authors and Affiliations
Contributions
Y.L.S wrote the main manuscript test and prepared the statistical analysis, tables, and figures. Y.A.H, Y.M.H, Y.H.P, L.I.C, F.C.D, Y.S.L, C.W.H. provided the database and supported the interpretation of data. C.W.H. organized the study group and supervised and revised the main manuscript. Y.L.S and C.W.H obtained the grants for this research. All authors already reviewed the final version of the manuscripts.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shen, YL., Hsieh, YA., Huang, YM. et al. Assessing the prognostic value of respiratory oscillometry in patients with difficult-to-treat asthma. Sci Rep 13, 2457 (2023). https://doi.org/10.1038/s41598-023-29672-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29672-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.