Abstract
Chronic shortened sleep can increase several cardiovascular risk factors, including depression, anxiety, metabolic syndrome, diabetes and hypertension. In the current study, we aimed to investigate the relationship between sleep patterns and the incidence of coronary heart disease (CHD). A total of 9704 healthy participants were recruited for the MASHAD cohort study. Within 6 years of follow-up, participants were categorized into four groups based on their number of hours of nightly sleep. Cox’s proportional hazard model was used to assess relative risks (RRs) and 95% confidence intervals (CIs). During the study, 235 heart problems, including myocardial infarction, stable angina and unstable angina, were confirmed. There were significant differences between men and women who had short and long nightly sleep (p < 0.05). The incidence of CHD was significantly higher in participants with very short night sleep durations than in those with longer hours of night sleep. The subjects with very short nightly sleep were more susceptible to unstable angina (RR: 2.614 (CI 1.354–5.047)) (p < 0.05). We found that shortened nightly sleep was associated with an increased incidence of coronary heart disease in an Iranian population. These findings suggest that sleep disorders, especially shortened night sleep, can be a risk factor for CHD.
Similar content being viewed by others
Introduction
Sleep is an essential indicator of well-being and health in humans. It has been proposed that a healthy sleep pattern is associated with reduced risks of different life-threatening diseases such as cardiovascular disease (CVD)1,2. Lack of or shortened sleep adversely affects physical health, temper, mood, and cognitive function3. People who complain of chronic loss and shortened sleep have problems staying asleep as long as qualified and generally suffer from sleepiness, being tired and lethargic, irritability, distressed and poor mood during the day4,5, so their quality of life is affected3.
Some studies indicated an emerging decrease in sleep duration in developed and industrialized countries such as the north American and European countries5. A study of more than 50 epidemiological studies showed that the prevalence of poor sleep and insomnia differs from 6 to 33%6. It is estimated that 10% to 30% of the US general population suffers from this problem6. Other investigations appraised that more than 30% of adults, as well as over 50% of the population older than 65 years, have current features of sleep disorders5.
In recent years, the problem of chronic loss or shortened sleep as well as insomnia has received special attention because some growing evidence suggests that poor sleep can increase some cardiovascular risk factors, such as the development of diabetes3, high blood pressure7, weight gain and obesity8, elevated resting heart rate (RHR)4, metabolic syndrome9, depression10, and immune system and cytokine titers3. Consequently, sleep seems to play important roles in cardiovascular health8. Coronary heart disease (CHD) is among the most important causes of fatality and morbidity worldwide11,12. The immune system, endocrine function, and inflammatory markers and cytokines seem to be associated with sleep duration and CVD13. However, to date, the available documents are not quite consistent, and most evidence has not been repeated clearly14.
In this study, we aimed to investigate the importance of pattern and timing of sleep in the incidence of coronary heart disease, a main cause of death worldwide, and its risk factors in a representative Iranian population sample from northeastern Iran after 6 years of follow-up.
Materials and methods
Study population
The MASHAD study, a cardiovascular risk factor cohort, was initiated in 2010 using a cluster-randomized methodology and invited volunteers aged 35–65 years who were living in the city of Mashhad in northeastern Iran15. Informed consent was obtained from all subjects. The exclusion criteria for recruitment at baseline including those without history of CHD. This study was approved by the Ethics Committee of the Mashhad University of Medical Sciences (MUMS) (MASHAD study code: 85134)15. All methods were performed in accordance with the relevant guidelines and regulations. Data on demographics, history of disease, smoking, depression and anxiety was collected using Beck and cardiovascular questionnaire at baseline.
Follow up
We followed up individuals from 2011 to 2014 by phone. A total of 646 subjects were declared CHD events, so we invited them to the clinic to confirm CHD events. All patients were visited by cardiologist, and if needed, echocardiography assessment, cardiac scan and other examinations were done. Finally, cases with a possible CHD event were reviewed by a panel of specialists who agreed on a definite diagnosis. As a result of this follow-up, CHD events, including MI, stable angina and unstable angina, were confirmed in 219 subjects16.
Anthropometric, biochemical data and nightly sleep
Systolic and diastolic blood pressure (SBP and DBP) were measured using a standard sphygmomanometer17. Fasting blood glucose, serum total cholesterol, LDL and high-density lipoprotein (HDL) cholesterol, triglycerides, uric acid and hs-CRP were measured as previously described18. The level of nightly sleep duration was assessed by questionnaire (self-reported), and based on the answer given to the question “how many hours do you sleep at night”, patients were categorized into four groups: < 5 h: very short nightly sleep, 5–6 h: short nightly sleep, 7–8 h: normal nightly sleep and > 9 h: long nightly sleep, in line with the majority of published studies19,20. Individuals who were night workers were determined20 by a self-questionnaire and excluded from the study.
QRISK
QRISK is an estimation of the 10-year risk of CHD, and it was calculated with adjustments made as suggested by the Joint British Societies’ (JBS2) paper and the JBS Cardiovascular Risk Assessor (patient.info/doctor/cardiovascular-risk-calculator)21,22.
Statistical analysis
Subjects in this study were divided into four groups according to nightly sleep: nightly sleep < 5 h, 5–6 h, 7–8 h and ≥ 9 h. Descriptive statistics, including the mean ± standard deviation, were considered for normally distributed variables or the median and interquartile range for variables that were not normally distributed. Differences in variables among nightly sleep were determined using ANOVA for normally distributed variables and Kruskal–Wallis H (the normality of distribution was evaluated using the Kolmogorov–Smirnov test). Chi square (or Fisher’s exact test) analysis was used for categorical parameters. Multinomial logistic regression was used to evaluate the odds ratio (OR) of event status and nightly sleep categorization. Relative risks (RRs) and 95% confidence intervals (CIs) of morbidity of all cases for nightly sleep were determined by using Cox’s proportional hazard model. All statistical analyses were undertaken by SPSS version 18 (SPSS Inc. Chicago, IL, USA). GraphPad Prism 6 and Adobe Illustrator CC | Graphic Design Software for figures were used. All the analyses were two-sided, and a p-value < 0.05 was considered significant.
Results
General characteristics of the subjects
Some characteristics of the subjects are shown in Table 1. Of the 9596 subjects in this study, 456 (4.8%) were found to have very short nightly sleep (< 5 h), 3065 (31.9%) had short nightly sleep (5–6 h), 5092 (53.1%) had normal nightly sleep (7–8 h) and 983 (10.2%) had long nightly sleep > 8 h). The mean ages of the groups were 51.27 ± 7.76, 48.99 ± 7.96, 47.33 ± 8 and 46.81 ± 8.2 years. The prevalence of short nightly sleep among the study population was 33.7% and 30.8% in men and women, respectively; and the prevalence of long nightly sleep was 8.2% and 11.6% in men and women, respectively. There were significant differences between men and women in short and long nightly sleep (p < 0.05) (Table 1).
The prevalence of no smoker, ex-smoker and current smoker in subjects with long nightly sleep were 8.7%, 11.4% and 14.5%, respectively. Current smoker subjects had significantly more nightly sleep > 8 h than other groups (p < 0.05). The mean weight, uric acid, hsCRP and QRISK of subjects with very short nightly sleep were significantly higher than those of the other groups (p < 0.05) (Table 1). The mean systolic and diastolic blood pressure and BMI were significantly lower in the groups with normal and long nightly sleep (p < 0.05).
Prevalence of CHD events according to nightly sleep
Of the individuals with stable angina, 9.5%, 29.7%, 51.4% and 9.5% had very short, short, normal and long nightly sleep, respectively. Incidence of CHD was significantly higher in participants with very short sleep duration than other groups. Of the group with unstable angina, 12.5%, 33.3%, 45.8% and 8.3% had very short, short, normal and long nightly sleep, respectively, and of the individuals with MI, 15%, 22.5%, 55% and 7.5% had very short, short, normal and long nightly sleep, respectively (Fig. 1). There were significant differences between very short nightly sleep with unstable and MI (p < 0.05).
Nightly sleep indices as risk factors for CHD events
Multinomial logistic regression was performed to assess the odds ratio (OR) of the association between nightly sleep and CHD events. According to the data presented in Table 2, subjects with very short (< 5 h) nightly sleep had 2.831 OR of total event (CI 1.852–4.329), 3.241 OR of unstable angina (CI 1.772–5.925) and 2.525 OR of MI (CI 1.113–5.728). These data were recalculated after adjusting for sex, age, smoking, BMI, and systolic and diastolic blood pressure, and retained for total event and unstable angina (OR: 2.453 (CI 1.465–4.108)) (p < 0.05).
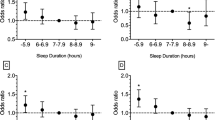
The relationship between CHD events and nightly sleep is presented in Fig. 2. According to this result, subjects with very short nightly sleep (< 5 h) had an increased relative risk for total event (RR: 2.939 (CI 1.878–4.770)) and unstable angina (RR: 2.614 (CI 1.354–5.047)) (p < 0.05). These results were confirmed after adjusting for sex, age, smoking, BMI, and systolic and diastolic blood pressure (Fig. 2). There were no significant differences between nightly sleep and the risk of stable angina and MI (Fig. 2).
Based on results shown in Table 3, there were 5 and 13 events at end of 108 and 120 months in nightly sleep < 5 h and hazard rate for these subjects was 0.002 and 0.01, respectively (the number of events and hazard rate for other groups are reported in Table 3). Also, for all the four groups, the survival during the follow up period is given in Fig. 3.
Discussion
Our project was the first study to investigate the association of sleep patterns with the incidence of coronary heart disease in a large cohort study in an Iranian population.
The results showed that there were significant differences between men and women in short and long nightly sleep. Current smoker subjects had significantly nightly sleep ≥ 9 h more than other groups. There were significant differences in mean weight, uric acid, hsCRP and QRISK between individuals with very short nightly sleep and other groups. The incidence of CHD was significantly higher in participants with very short sleep durations (< 5 h) than in other groups (p < 0.001). There were significant differences between very short nightly sleep and unstable and MI, and subjects with very short (< 5 h) nightly sleep had 3.241 OR of unstable angina (CI 1.772–5.925) and 2.525 OR of MI (CI 1.113–5.728). Subjects with very short nightly sleep (< 5 h) had an increased relative risk for unstable angina after adjusting for sex, age, smoking, BMI, and systolic and diastolic blood pressure.
Association of unhealthy sleep behaviors and poor sleep with survival and CVD outcomes and risk factors, has been previously reported3,8,11,23.
Grandner et al. concluded that inadequate sleep duration and sleep disturbance are related to obesity, dyslipidemia, diabetes, inflammation, high blood pressure and CVD. Therefore, it could be proposed that lack of or shortened sleep is a risk factor for cardiometabolic disability and fatality8.
In Taiwanese people, Chao et al. investigated association between length of sleep and prediabetes or newly diagnosed diabetes. Shortened of sleep could be a risk factor for the development of diabetes mellitus as well as sleep length were independently related to recently diagnosed diabetes24. Ferrie et al. revealed that an increase 2 h to night sleep associated with high incidence of diabetes in comparison to reference group with sufficient and proper sleep (7 h), odds ratio 1.65 [95% CI 1.15, 2.37] obtained with adjusted for age, gender, an occupation status, and ethnic categories. These results could be interpreted with weight gain in this group25. Kowall et al. also evaluated the role of sleep in incident prediabetes and type 2 diabetes mellitus as CVD risk factor in large population-based study. They demonstrated that there is a U-shaped correlation between sleep duration and incident diabetes also there isn’t any significant association between daily nap and incidence of it17.
Vozoris et al. found that sleep disorder symptoms accompanied with chronic short sleep time could be positively correlated to increased blood pressure, but the absence of relation with objective hypertension measures proposes that there might be no accurate association present18. Clark et al. examined significance of disturbed sleep on high blood pressure, diabetes mellitus and dyslipidemia as risk factors for CVD in 8 years follow up of the Finnish Public Sector study population. The results indicated that impaired sleep could be a predictor of hypertension and dyslipidemia with hazard ratio = 1.22, 95% CI 1.04–1.44 and HR = 1.17, 95% CI 1.07–1.29, respectively in completely adjusting26. Khan and Aouad examined some articles about sleep disorder, CVD and its risk factors like diabetes, high systolic blood pressure and cytokine concentrations. They expressed that people with normal blood pressure status suffered from chronic loss and shortened of sleep have shown increased or blunting systolic blood pressure (SBP) at night comparison to control group with normal sleep matched for age and gender3,27 as well as the rate of type 2 diabetes mellitus developed in subjects with sleep disorder28.
Spiegelhalder et al. in their systematic review, include of 10 studies, found that there were significant association between sleep disorder and coronary artery disease may be due to high blood pressure or elevated RHR. The risk ratios (RR) for CVD in individual with poor sleep was 1.5–3.9 when adjusted for some CVD risk factors such as smoking, hypertension, diabetes mellitus, age and fatness4.
In subjects of 385 292 UK Biobank study, the association of loss and shortened of sleep with genetic predisposition, and incidence of CVD have been investigated and their results indicated that appropriate and adequate sleep status have decreased risk of CVD between individual with low, intermediate, or high genetic risk11.
Li et al. assessed relationship among sleep disorder symptoms and fatality in US men population longitudinally during 6 years. Men with difficulty in beginning sleep and staying asleep, respectively had a 55% (HR 1.55; 95% CI1.19–2.04; p-trend = 0.01) and 32% (HR 1.32; 95% CI 1.02–1.72; p-trend = 0.002) high risk of CVD fatality, compared to men with normal sleep status29.
Bertisch and colleagues investigated the effect of chronic shortened of sleep on incident CVD and fatality in 4994 subjects of Sleep Heart Health Study (SHHS) well accomplished baseline polysomnography. Their findings showed that short sleep duration (< 5) related with an increased risk of CVD30.
Sofi et al. in their systematic review investigated the relationship of sleep disturbance with CVD in 122,501 individuals in 13 cohort studies. This population were followed 3 up to 20 years. They provided evidence that insomnia has led to an increased risk (45%) or mortality of CVD (RR, 1.45, 95% CI, 1.29–1.62; p < 0.00001)5.
Spiegelhalder et al. in their systematic review, include of 10 studies, found that there were significant association between sleep disorder and coronary artery disease may be due to high blood pressure or elevated RHR. The risk ratios (RR) for CVD in individual with poor sleep was 1.5–3.9 when adjusted for some CVD risk factors such as smoking, hypertension, diabetes mellitus, age and fatness4.
Li et al. in their meta-analysis of 17 cohort studies through 17 May 2014, showed that loss and shortened sleep were significantly related to the development risk of CVD and death after adjusting for classic CVD risk factors. They interpreted the association of insomnia with CVD through metabolic or endocrine modifications by increased concentrations of inflammatory cytokines6. Carreras et al., examined the effects of Sleep Fragmentation (SF) on function of endothelial and vessel wall construction in mice. They found that SF might lead to inflammation, and changes in structure of vessel and endothelial dysfunction31. Also, inadequate sleep duration might affect ghrelin and leptin level; this may lead to increased appetite and consequently obesity, impaired glycemic control, higher levels of cortisol, changes in growth hormone concentration, coronary artery calcification, and higher risk of atherosclerosis13,23.
Our results demonstrated that the incidence of CHD was significantly higher in participants with very short sleep durations than in other groups, and subjects with shortened sleep durations (< 5 h) had an increased relative risk for unstable angina after adjusting for several CVD risk factors. The results of the current study are largely consistent with the studies mentioned above and showed that inadequate sleep duration is associated with increased risk of CHD. Thus, we emphasize the importance of maintaining healthy/normal sleep pattern for prevention of CVD1.
Conclusion
We found that chronic shortened sleep were associated with increased incident coronary heart disease in an Iranian population. There were significant differences between shortened nightly sleep with unstable and MI. Subjects with very short sleep had an increased relative risk for unstable angina after adjusting for several CHD risk factors. These findings suggest that sleep disorders, especially lack or shortened sleep, could be a risk factor for CHD.
Limitation
This experiment should be re-conducted over a longer follow-up period for CHD events. Moreover, since we performed this research in MASHAD cohort study (i.e. on the participants recruited from Mashhad, eastern Iran), other populations of different genetic background and with different environmental exposures should be considered in future studies.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due copy right in Mashhad university of medical sciences but are available from the corresponding author on reasonable request.
References
Zhou, T. et al. Adherence to a healthy sleep pattern is associated with lower risks of all-cause, cardiovascular and cancer-specific mortality. J. Intern. Med. 291(1), 64–71 (2022).
Morovatdar, N. et al. Sleep duration and risk of atrial fibrillation: A systematic review. J. Atrial Fibrill. 11(6), 2132 (2019).
Khan, M. S. & Aouad, R. The effects of insomnia and sleep loss on cardiovascular disease. Sleep Med. Clin. 12(2), 167–177 (2017).
Spiegelhalder, K., Scholtes, C. & Riemann, D. The association between insomnia and cardiovascular diseases. Nat. Sci. Sleep 2, 71 (2010).
Sofi, F. et al. Insomnia and risk of cardiovascular disease: A meta-analysis. Eur. J. Prev. Cardiol. 21(1), 57–64 (2014).
Li, M., Zhang, X.-W., Hou, W.-S. & Tang, Z.-Y. Insomnia and risk of cardiovascular disease: A meta-analysis of cohort studies. Int. J. Cardiol. 176(3), 1044–1047 (2014).
Meng, L., Zheng, Y. & Hui, R. The relationship of sleep duration and insomnia to risk of hypertension incidence: A meta-analysis of prospective cohort studies. Hypertens. Res. 36(11), 985–995 (2013).
Grandner, M. A. et al. Sleep: Important considerations for the prevention of cardiovascular disease. Curr. Opin. Cardiol. 31(5), 551 (2016).
Troxel, W. M. et al. Sleep symptoms predict the development of the metabolic syndrome. Sleep 33(12), 1633–1640 (2010).
Baglioni, C. et al. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 135(1–3), 10–19 (2011).
Fan, M. et al. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: A prospective study of 385,292 UK biobank participants. Eur. Heart J. 41(11), 1182–1189 (2020).
Poorzand, H. et al. Risk factors of premature coronary artery disease in Iran: A systematic review and meta-analysis. Eur. J. Clin. Investig. 49(7), e13124 (2019).
Krittanawong, C. et al. Association between short and long sleep durations and cardiovascular outcomes: A systematic review and meta-analysis. Eur. Heart J. Acute Cardiovasc. Care 8(8), 762–770 (2019).
Feige, B. et al. Does REM sleep contribute to subjective wake time in primary insomnia? A comparison of polysomnographic and subjective sleep in 100 patients. J. Sleep Res. 17(2), 180–190 (2008).
Ghayour-Mobarhan, M. et al. Mashhad stroke and heart atherosclerotic disorder (MASHAD) study: Design, baseline characteristics and 10-year cardiovascular risk estimation. Int. J. Public Health 60(5), 561–572 (2015).
Sadabadi, F. et al. Decreased threshold of fasting serum glucose for cardiovascular events: MASHAD cohort study. Rep. Biochem. Mol. Biol. 9(1), 64 (2020).
Kowall, B. et al. Associations among sleep disturbances, nocturnal sleep duration, daytime napping, and incident prediabetes and type 2 diabetes: The Heinz Nixdorf Recall Study. Sleep Med. 21, 35–41 (2016).
Vozoris, N. T. The relationship between insomnia symptoms and hypertension using United States population-level data. J. Hypertens. 31(4), 663–671 (2013).
Grandner, M. A., Chakravorty, S., Perlis, M. L., Oliver, L. & Gurubhagavatula, I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 15(1), 42–50 (2014).
Darroudi, S. et al. Overweight and obesity are potential risk factors for disrupted nocturnal sleep in Iranian adults: A cross-sectional study. Int. J. Public Health 66, 633183 (2021).
Collins, G. S. & Altman, D. G. Predicting the 10 year risk of cardiovascular disease in the United Kingdom: Independent and external validation of an updated version of QRISK2. BMJ 344, e4181 (2012).
Darroudi, S. et al. Prevalence of combined and noncombined dyslipidemia in an Iranian population. J. Clin. Lab. Anal. 32(8), e22579 (2018).
Kwok, C. S. et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: A dose-response meta-analysis. J. Am. Heart Assoc. 7(15), e008552 (2018).
Chao, C.-Y. et al. Sleep duration is a potential risk factor for newly diagnosed type 2 diabetes mellitus. Metabolism 60(6), 799–804 (2011).
Ferrie, J. E. et al. Change in sleep duration and type 2 diabetes: The Whitehall II Study. Diabetes Care 38(8), 1467–1472 (2015).
Clark, A. J. et al. Onset of impaired sleep and cardiovascular disease risk factors: A longitudinal study. Sleep 39(9), 1709–1718 (2016).
Lanfranchi, P. A. et al. Nighttime blood pressure in normotensive subjects with chronic insomnia: Implications for cardiovascular risk. Sleep 32(6), 760–766 (2009).
Buxton, O. M. et al. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes 59(9), 2126–2133 (2010).
Li, Y. et al. Association between insomnia symptoms and mortality: A prospective study of US men. Circulation 129(7), 737–746 (2014).
Bertisch, S. M. et al. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep 41(6), 047 (2018).
Carreras, A. et al. Chronic sleep fragmentation induces endothelial dysfunction and structural vascular changes in mice. Sleep 37(11), 1817–1824 (2014).
Acknowledgements
The authors thank all the patients and their family members who volunteered to participate in this study.
Funding
This work was supported by the Deputy of Research, Mashhad University of Medical Sciences [Grant Number 930940].
Author information
Authors and Affiliations
Contributions
F.S., S.D., Z.A. (follow-up patients and data collection). S.D. (Data analysis). H.E. (Data analysis). F.S., S.D., A.H.N. (wrote the main manuscript text). A.H.M. (scientific editing). G.A.F. (scientific and grammatical editing). M.M., M.G.-M. (corresponding author, designed the study).
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sadabadi, F., Darroudi, S., Esmaily, H. et al. The importance of sleep patterns in the incidence of coronary heart disease: a 6-year prospective study in Mashhad, Iran. Sci Rep 13, 2903 (2023). https://doi.org/10.1038/s41598-023-29451-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29451-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.