Abstract
The need of palliative care at the end-of-life in the emergency departments (ED) is growing. The study aims to investigate the epidemiology of patients who died during care in ED using nationwide database, and to estimate the need for palliative care in the ED. A retrospective observational study was conducted using the National Emergency Department Information System (NEDIS) database. Patients who died during ED care between 2016 and 2019 were included. Palliative care-eligible disease was defined as cancer (C00–C99 of ICD-10), chronic respiratory disease (CRD, J44–J46), chronic liver disease (CLD, K70–K77), and heart failure (HF, I50). Among the 36,538,486 ED visits during 4 years, 34,086 ED deaths were included. The crude incidence rate of ED deaths per 100,000 person-year was steady between 16.6 in 2016 and 16.3 in 2019 (p-for-trend = 0.067). Only 3370 (9.9%) ED deaths were injury, while 30,716 (90.1%) deaths were related to diseases. The most common ED diagnosis was cardiac arrest (22.1%), followed by pneumonia (8.6%) and myocardial infarction (4.7%). In cases of disease-related ED deaths, about 34.0% stayed longer than 8 h in the ED (median (interquartile range): 4.5 (1.9–11.7) h) and 44.2% received cardiopulmonary resuscitation (CPR) at end-of-life time. A quarter of the disease-related ED deaths were diagnosed with palliative care eligible disease: cancer (16.9%), CLD (3.8%), HF (3.5%), and CRD (1.4%). Cancer patients received less CPR (23.4%) and stayed longer in the ED (median (interquartile range): 7.3 (3.2–15.9) h). Over the past 4 years, more than 30,000 patients, including 5200 cancer patients, died during care in the ED. A quarter of disease-related ED death were patients with palliative care-eligible condition and more than 30% of them stayed longer than 8 h in the ED before death. It is time to discuss about need of palliative care in the ED.
Similar content being viewed by others
Introduction
The importance of palliative and end-of-life care is emphasized1,2,3 to an extent where the World Health Organization (WHO) recommends providing palliative care for most incurable patients and recognizing end-of-life care as an ethical obligation3,4. This is, however, still in an introductory stage and is provided only in limited places and to limited subjects5. In Korea, the need for palliative and end-of-life care is increasing after the enactment of “Act on Hospice and Palliative Care and Decisions on Life-Sustaining Treatment for Patients at the End-of-Life” (hospice act) in 20186.
The emergency department (ED) is a specialized space for treating acute medical problems and saving lives, and therefore mortality rate in the EDs is relatively higher than that of general wards7. Some people die in ED from results of unexpected events or from sudden development of acute illnesses such as acute myocardial infarction or traumatic brain injury, while some patients with chronic diseases visit the ED to control rapidly worsening symptoms and serious complications of treatment and die in the ED8,9. Death during emergency care in the ED can be unavoidable for critically ill patients; however, there are little information about how many patients and who died in the ED10.
As prevalence of the advanced disease increases, there is an increase in ED visits at end-of-life for patients with terminal cancer or chronic illnesses8,9,11,12,13. People in proximity to death use more acute healthcare services than people who are not14. Among them, patients diagnosed with cancer and respiratory diseases are more likely to use acute-based healthcare service such as ED15. More than half of elderly patients who passed away in the ED had serious chronic illnesses and required palliative care16,17. Many ED visits in these terminally ill patients are considered avoidable, therefore, the need for palliative care at the end-of-life in ED is emphasized in many countries18,19. In the Unites States, there is a guideline for hospice care-eligible patients who visit the ED, and ED-initiated palliative care is recommended for patients with advanced cancer to improve the patients’ quality of life20,21. United Kingdom also reported end-of-life care recommendations for dying patients in the ED22. However, there is currently insufficient information on how patients who need end-of-life care are being treated in the ED and how many patients with incurable diseases received life-sustaining treatment such as cardiopulmonary resuscitation (CPR) in the ED before death. To improve the palliative care at end-of-life for terminally ill patients, it is necessary to understand the epidemiologic characteristics of patients who died in the ED18,23.
The purpose of this study is to investigate the epidemiologic characteristics of patients who died in the ED using representative nationwide database and to identify the reasons of ED visits of those patients. The study intends to estimate the need for palliative care at end-of-life in the ED and to accumulate the baseline data for future research.
Methods
Study design and data sources
This is a retrospective observational study using data from the National Emergency Department Information System (NEDIS) database. The Ministry of Health and Welfare constructed this nationwide ED-based database in 2013. NEDIS collected administrative and clinical information of all patients who visited EDs in real time from a total of 402 EDs across the country in 201924,25,26. The information includes patient demographics, prehospital, and ED treatment. All patient-related information was automatically transferred from each ED to a central government server within 14 days of discharge from the ED or hospital. The trained coordinators designated in each institution managed the data uploading process. The NEDIS data is updated by the National Emergency Medical Center and is approved annually by National Statistics for data quality management.
Study setting
Korea has a total population of 50 million, while the annual death rate was about 0.3 million in 2019. More than 70% of deaths occurred in medical institutions, and 14% at homes. The most common causes of death were cancer, heart disease, and pneumonia27.
The National Health Insurance (NHI) of Korea covers the entire population for inpatient, outpatient, and ED treatment. EDs are classified into 3 levels according to resources and capacity (including facilities, equipment, and medical staff), which are defined by the Ministry of Health and Welfare: 38 Level 1 EDs, 125 Level 2 EDs, and 239 Level 3 EDs (a total of 402 EDs), that are operational as of 2020. Level 1 ED provide the highest level of emergency care services in the country, and is designed to accommodate and to provide definite care to critically ill and severe emergency patients. Level 1 and 2 are emergency centers which take charge of treating critical ill patients, and Level 3 is in charge of general urgent care and primary responses 24 h a day, 7 days a week. Under this healthcare system, EDs are open to all beneficiaries without restriction, and patients have high accessibility to the ED care28.
Hospice and palliative care was first introduced to Korea in 2015 with inpatient hospice beds. Consultation-based hospice care for non-hospice wards and outpatients started as a pilot project in 2017 and home-based hospice care was officially started in 202029. The hospice act defined four disease groups as target disease for palliative care: cancer, Acquired Immunodeficiency Syndrome (AIDS), chronic respiratory disease, and chronic liver cirrhosis as target disease for palliative care6. However, it is still in the introductory stage; there are not many providers of hospice ward and home-based hospice. The consultation-based hospice is mainly for inpatients and outpatients, and rarely applied to patients in ED.
Study population
The study subject were patients who died during care in the ED (hereafter, ED deaths) in Korea for 4 years from January 2016 to December 2019. Death on arrival (DOA), patients who had already had cardiac arrest at ED arrival and did not receive any resuscitation efforts, patients who visited ED for non-medical reasons such as issuance of medical certificates, and patients who had unknown information of age or reason for ED visit were excluded.
Variables and measurements
Based on the reason for ED visit, all ED deaths were initially classified into a disease-related group and injury-related (injury) group. For disease-related ED deaths group, the specific reasons for ED visits were classified based on the ED diagnosis codes of the international classification of diseases, 10th edition (ICD-10) in the ED discharge records written by emergency physicians.
Palliative care-eligible disease was defined based on the hospice act and literature review: cancer, chronic respiratory disease, chronic liver disease, and heart failure30. Palliative care-eligible disease was defined based on the ED diagnosis: cancer (ICD-10 code, C00–C99), chronic respiratory disease (chronic obstructive pulmonary disease and asthma, J44–J46), chronic liver disease (K70–K77), and heart failure (I50).
The following variables were collected from the NEDIS database to investigate the characteristics of ED deaths: 1. patient demographics (age, sex, and insurance), 2. prehospital and ED information (date and time of ED visit, mode of ED visit (use of ambulance or not), route of ED visit (direct visit or transfer-in from other hospital), region of ED (metropolitan or urban/rural), and level of ED (level 1, 2 and 3)), 3. care and outcomes (mental status at ED entrance, ED length of stay (ED-LOS), life-sustaining treatment (CPR and endotracheal intubation), ED diagnosis (ICD-10 code, multiple choice up to 20 codes), ED disposition (place, date and time of disposition), and ED death)31,32.
Statistical analysis
A descriptive analysis was conducted to investigate epidemiologic characteristics of the study population. Categorical variables were presented as counts and proportions and differences across groups were tested by Chi-square test. Continuous variables were presented as medians and interquartile ranges (IQR) and differences across groups were tested by Wilcoxon rank-sum test.
The characteristics were compared according to the reason for ED visit (disease-related and injury-related). The most common diagnoses were investigated for the disease-related ED deaths group and cancer-related ED deaths.
The epidemiologic trends of all ED deaths and ED deaths of patients with palliative care-eligible conditions were investigated. The crude and the age- and sex- standardized incidence rates per 100,000 person-years were calculated. Direct standardization method was used using the 2020 mid-year census population as the standard population33.
NEDIS database collected during 2016–2019 were analyzed in July 2021. All statistical analyses were conducted using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was taken as P < 0.05.
Ethical statement
This study was approved by the Institutional Review Boards of Seoul National University Hospital (approval No. SNUH-2012–104-1183), and the requirement for informed consent was waived due to the retrospective nature of this study. Patient information was anonymized prior to analysis. All methods were performed in accordance with relevant guidelines and regulations.
Patient and public involvement statement
The National Emergency Medical Center under the Ministry of Health and Welfare was involved in the design and conduct of this research, but it was not possible to involve patients in our research.
Results
Study population
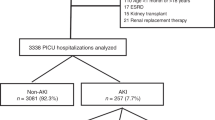
Between 2016 and 2019, the total number of ED visits was 36,538,486 of which total death toll was 117,256 (0.3%). Among them, 34,086 ED deaths were included as a study population, excluding cases that were already in cardiac arrest at the ED entrance (n = 81,222) and cases with unknown information on age (n = 3) and reason for ED visit (n = 1945) (Fig. 1). Approximately 8500 patients per year died in the ED during the ED care.
Characteristics of the ED deaths
Among the 34,086 ED deaths, 3370 (9.9%) died from injury while 30,716 (90%) died from diseases. The median age of ED deaths was 75 (63–83) years old. 32.2% (n = 10,961) had an alert mental status upon ED arrival. Median (IQR) ED-LOS was 4.4 (2.0–11.2) h and 32.8% (n = 11,183) stayed in the ED over 8 h before death. CPR was provided in 45.4% and endotracheal intubation was performed in 48.6%. Compared to the injury-related ED deaths group, the disease-related ED deaths group was older (76 (64–83) vs. 68 (54–79) years old, p < 0.01) and had longer ED-LOS (4.5 (1.9–11.7) vs. 3.6 (2.0–6.9) h, p < 0.01) (Table 1).
Among the disease-related ED deaths, the most common diagnoses were cardiac arrest (22.1%), followed by pneumonia (8.6%) and myocardial infarction (4.7%). In cancer patients, the most common diagnoses excluding cancer diagnoses (42.7%) were pneumonia (6.5%), followed by cardiac arrest (6.3%) and dyspnea (3.8%) (Table 2).
Characteristics of the disease-related ED deaths
Among 30,716 disease-related ED deaths, 7855 (25.6%) were ED deaths of patients with palliative care-eligible: 16.9% (n = 5187) was related with cancer, 1.4% (n = 416) with chronic respiratory disease, 3.8% (n = 1176) with chronic liver disease, and 3.5% (n = 1076) with heart failure. The ED deaths of patients with palliative care-eligible conditions had longer median ED-LOS, compared to ED deaths of patients without palliative care-eligible conditions (p < 0.01). Regarding life-sustaining treatment, 2327/7855 (29.6%) received CPR and 2707/7855 (34.5%) received endotracheal intubation before death. Cancer patients received relatively less life-sustaining treatment: 23.4% received CPR and 27.1% received endotracheal intubation (Table 3). Demographics according to the ED-LOS are presented in Supplementary Table S1.
Regarding provision of CPR, 55.8% (n = 17,154) of the 30,716 disease-related ED deaths did not receive CPR prior to death. Patients who did not receive CPR had longer ED-LOS than those who received CPR (6.5 (2.6–16.0) vs. 3.0 (1.6–6.8) h, p < 0.01). Of the ED deaths that received CPR, 17.2% were diagnosed with palliative care-eligible diseases (cancer 9.0%, chronic respiratory disease 1.1%, chronic liver disease 3.6%, and heart failure 3.5%). (Table 4). The provision of CPR for the ED deaths of patients with palliative care-eligible diseases are presented in Supplement Table S2.
Epidemiologic trends of ED deaths
The crude incidence rate of ED deaths per 100,000 person-years was 16.6 in 2016, 16.7 in 2017, 17.0 in 2018, and 16.3 in 2019, respectively, showing a steady trend during the study period (p-for-trend = 0.067). The age- and sex- standardized incidence rate of ED deaths per 100,000 person-years decreased from 19.7 in 2016 to 17.1 in 2019 (p-for-trend < 0.001). Both disease (17.5 to 15.6) and injury (2.2 to 1.4) were on the decline (p-for-trend < 0.001) (Fig. 2). ED deaths with cancer were slightly increased with crude rate from 2.3 to 2.7 and standardized rate from 2.7 to 2.9 (Fig. 3).
Discussion
During the 4 years between 2016 and 2019, a total of 34,086 patients died in the ED during care, approximating to 2.9% of all deaths in Korea. Among those ED deaths, 90% were disease-related death. Patients stayed for a median 4.4 h before death in the ED, of which only 45.4% received CPR. A quarter of disease-related ED deaths had a condition eligible for palliative care. They stayed in the ED longer while receiving less life-sustaining treatment (29.6% received CPR) before death, compared to other patients. Cancer-related ED deaths accounted for 16% of disease-related ED deaths: half of them died after staying for more than 8 h in the ED and a quarter of them received CPR before death. This study found that nearly 8500 patients die in the ED every year and the annual incidence rate of ED deaths was about 17 per 100,000 person-year in Korea. To the best of current knowledge, it is the first study to investigate the magnitude of ED deaths nationwide.
In Korea, the death rates per 100,000 person-years in 2019 were 574.8 for all cause of death and 158.2 due to cancer, accounting for 27.5% of all deaths27. Since the ED is for providing acute care for critically ill patients, death in the ED is unavoidable. However, not much is known about patients who die in an ED13,34. In this study, only 10% of the ED deaths were caused by injuries such as traffic accidents or falls. This was smaller than a single center study done in Switzerland10. 90% of the ED deaths were disease-related patients, and one quarter of them had diagnosis codes subject to palliative care. Previous studies have reported that 30 ~ 50% of death in the ED were related to serious chronic illnesses or palliative care needs16,17,35. Since this study classified only four representative diseases as palliative care-eligible diseases, size of the palliative care subjects may be smaller than other studies. Theoretically, all patients with imminent death are eligible for palliative care, including those who die in the ED2.
In this study, ED deaths happened after a median 4.4 h in the ED, and 30% of disease-related ED deaths occurred after 8 h in the ED. It was previously reported in US that all ED visit patients stayed for median 4 h in the ED, and that more than 8 h of stay is defined as a long stay31,32. Other studies reported that, among ED visits, discharged patients stayed for median 2.5 h and hospitalized patients stayed for 4 h36,37. Patients who die in ED may stay for relatively longer periods of time in the ED and utilize more resources than patients who survived. Among all ED deaths, about half of ED deaths received CPR (45.4%) and endotracheal intubation (48.6%) before death in this study. It aligns with other studies in that more than 50% of the patients died in the ED without CPR38,39,40. Moreover, 30% of ED deaths with palliative care-eligible diseases and a quarter of cancer-related ED deaths received CPR before death, which is 4–7 times higher than that of a German study41. CPR is a life-saving treatment for acute stage patients, but it could be a life-sustaining treatment with little meaning for incurable and terminally ill patients. A hospital-level study or qualitative study is needed to know how life-sustaining treatment is provided in individual patients. The results of this study show the possibility that there still is a substantial unmet need for palliative care in the ED and the need for follow-up studies42,43.
In this study, about half of ED deaths with palliative care-eligible diseases and cancer-related ED deaths stayed over 8 h before death in the ED. During ED care, 30% of ED deaths with palliative care-eligible diseases and a quarter of cancer-related ED deaths received CPR before death. More attention would be needed on how to provide end-of-life care in times of expected death in the ED. This discussion encompasses not only which care should be provided for dying patients, but also whether it would be suitable for such patients to stay in ED for such long times. This study showed overall epidemiologic characteristics of ED deaths using a nationally representative emergency database. Considering that patients who died within 72 h after visiting the ED, as well as ED death, are also eligible for palliative care, the need for palliative care at the end-of-life in the ED would increase (Supplement Table S3). Based on the need for palliative care at end-of-life in the ED in this study, it is necessary to develop a strategy for improving end-of-life care in the ED.
This study has several limitations. First, the NEDIS database does not collect information on whether the patients have previously completed advance directives or physician orders for life-sustaining treatment (POLST). Further study is needed to determine whether patients with palliative-care eligible conditions have a plan before visiting the ED and can receive proper end-of-life care through this. As a limitation of the studies using a large database, it is necessary to comprehensively interpret the results of this study by referring to the results of studies focusing on individual patients. Second, whether the patient had a disease subject to palliative care was determined based on the diagnosis codes in the ED medical records. Whether that disease was previously diagnosed or first diagnosed in the ED is unknown. Third, the NEDIS data does not collect information of test results and medication prescription. It is difficult to know whether the dying patient received sufficient supportive care in the ED before death, such as pain control. Fourth, Korea has the NHI service is implemented, and palliative care services are in the introduction stage. It is difficult to generalize the result to other countries with different healthcare system and accessibility to palliative care.
In conclusion, more than 30,000 people died during care in the ED over the past four years. At least a quarter of disease-related ED deaths were owed to palliative care-eligible diseases. More than 30% of disease-related ED deaths and 40% of cancer-related ED deaths happened at least 8 h after arrival in the ED. About half of disease-related ED deaths and 30% of ED deaths with palliative care-eligible diseases received CPR before death. Increased efforts to understand death in the ED may improve end-of-life care in the ED.
Data availability
The data of this study were obtained from the National Emergency Medical Center under the Ministry of Health and Welfare in Korea but restrictions apply to the availability of these data and so are not publicly available, but are available from the corresponding author on reasonable request.
Change history
13 February 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-29430-1
References
Mitchell, G. Rapidly increasing end-of-life care needs: A timely warning. BMC Med. 15(1), 1–2 (2017).
Morrison, R. S. & Meier, D. E. Palliative care. N. Engl. J. Med. 350(25), 2582–2590 (2004).
Sepúlveda, C., Marlin, A., Yoshida, T. & Ullrich, A. Palliative care: The World Health Organization’s global perspective. J. Pain Symptom Manage. 24(2), 91–96 (2002).
Singer, P. A., Martin, D. K. & Kelner, M. Quality end-of-life care: Patients’ perspectives. JAMA 281(2), 163–168 (1999).
Won, Y.-W. et al. Life-sustaining treatment states in Korean cancer patients after enforcement of act on decisions on life-sustaining treatment for patients at the end of life. Cancer Res. Treat. 53, 908–916 (2021).
Kim, J. S. et al. Implication of the life-sustaining treatment decisions act on end-of-life care for Korean terminal patients. Cancer Res. Treat. 52(3), 917 (2020).
Smulowitz, P. B., Honigman, L. & Landon, B. E. A novel approach to identifying targets for cost reduction in the emergency department. Ann. Emerg. Med. 61(3), 293–300 (2013).
Panattoni, L. et al. Characterizing potentially preventable cancer-and chronic disease–related emergency department use in the year after treatment initiation: A regional study. J. Oncol. Pract. 14(3), e176–e185 (2018).
Rivera, D. R. et al. Trends in adult cancer–related emergency department utilization: An analysis of data from the nationwide emergency department sample. JAMA Oncol. 3(10), e172450 (2010).
Heymann, E. P., Wicky, A., Carron, P.-N. & Exadaktylos, A. K. Death in the emergency department: A retrospective analysis of mortality in a Swiss university hospital. Emerg. Med. Int. 2019, 1–9 (2019).
Tang, N., Stein, J., Hsia, R. Y., Maselli, J. H. & Gonzales, R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA 304(6), 664–670 (2010).
Grudzen, C. R., Richardson, L. D., Morrison, M., Cho, E. & Sean, M. R. Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad. Emerg. Med. 17(11), 1253–1257 (2010).
Kenen, J. Palliative care in the emergency department: New specialty weaving into acute care fabric. Ann. Emerg. Med. 56(6), A17–A19 (2010).
Canova, C. et al. Use of healthcare services at the end of life in decedents compared to their surviving counterparts: A case-control study among adults born before 1946 in Friuli Venezia Giulia. PLoS ONE 14(2), e0212086 (2019).
BarbielliniAmidei, C. et al. Hospitalizations and emergency department visits trends among elderly individuals in proximity to death: A retrospective population-based study. Sci. Rep. 11(1), 1–10 (2021).
Beynon, T. et al. How common are palliative care needs among older people who die in the emergency department?. Emerg. Med. J. 28(6), 491–495 (2011).
Pal, R. Y., Kuan, W. S., Koh, Y., Venugopal, K. & Ibrahim, I. Death among elderly patients in the emergency department: A needs assessment for end-of-life care. Singapore Med. J. 58(3), 129 (2017).
Barbera, L., Taylor, C. & Dudgeon, D. Why do patients with cancer visit the emergency department near the end of life?. CMAJ 182(6), 563–568 (2010).
Alsirafy, S. A. et al. Emergency department visits at the end of life of patients with terminal cancer: Pattern, causes, and avoidability. Am. J. Hospic Palliat. Med. 33(7), 658–662 (2011).
Lamba, S. & Quest, T. E. Hospice care and the emergency department: Rules, regulations, and referrals. Ann. Emerg. Med. 57(3), 282–290 (2011).
Grudzen, C. R. et al. Emergency department–initiated palliative care in advanced cancer: A randomized clinical trial. JAMA Oncol. 2(5), 591–598 (2016).
Harrison, S. Leadership alliance for the care of dying people, ONE CHANCE TO GET IT RIGHT: Improving people’s experience of care in the last few days and hours of life. London: LACDP, 2014, 168pp (Pbk). Publications Gateway Reference 01509, free of charge. Health Soc. Care Chaplaincy 2(1), 146–148 (2014).
Leak, A., Mayer, D. K., Wyss, A., Travers, D. & Waller, A. Why do cancer patients die in the emergency department? An analysis of 283 deaths in NC EDs. Am. J. Hospice Palliat. Med. 30(2), 178–82 (2013).
Pak, Y. S. et al. Effects of emergency care-related health policies during the COVID-19 pandemic in Korea: A quasi-experimental study. J. Korean Med. Sci. 36(16), e121 (2021).
Jung, E., Ro, Y. S., Ryu, H. H., Shin, S. D. & Moon, S. Interaction effects between COVID-19 outbreak and community income levels on excess mortality among patients visiting emergency departments. J. Korean Med. Sci. 36(13), e100 (2021).
Kim, K. H. et al. Association between time to emergency neurosurgery and clinical outcomes for spontaneous hemorrhagic stroke: A nationwide observational study. PLoS ONE 17(4), e0267856 (2022).
Korea, S. Causes of Death Statistics in 2019. (National statistics, 2020). http://kostat.go.kr/portal/eng/pressReleases/8/10/index.board?bmode=read&aSeq=385629&pageNo=&rowNum=10&amSeq=&sTarget=&sTxt=.
Lee, S. Y., Khang, Y.-H. & Lim, H.-K. Impact of the 2015 middle east respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med. J. 60(8), 796–803 (2019).
Kim, C. G. Hospice & palliative care policy in Korea. Korean J. Hospice Palliat. Care 20(1), 8–17 (2017).
Kelley, A. S. & Morrison, R. S. Palliative care for the seriously ill. N. Engl. J. Med. 373(8), 747–755 (2015).
Liew, D., Liew, D. & Kennedy, M. P. Emergency department length of stay independently predicts excess inpatient length of stay. Med. J. Aust. 179(10), 524–526 (2003).
Rathlev, N. K. et al. Time series analysis of variables associated with daily mean emergency department length of stay. Ann. Emerg. Med. 49(3), 265–271 (2007).
Korea, S. Population of the Middle of the Year. Accessed 26, December, https://www.kosiskr/statHtml/statHtmldo?orgId=101&tblId=DT_1B040M5 (2019).
Bailey, C. J., Murphy, R. & Porock, D. Dying cases in emergency places: Caring for the dying in emergency departments. Soc. Sci. Med. 73(9), 1371–1377 (2011).
Tardy, B. et al. Death of terminally ill patients on a stretcher in the emergency department: A French speciality?. Intensive Care Med. 28(11), 1625–1628 (2002).
Le, S. T. & Hsia, R. Y. Timeliness of care in US emergency departments: An analysis of newly released metrics from the Centers for Medicare & Medicaid Services. JAMA Intern. Med. 174(11), 1847–1849 (2014).
Kocher, K. E., Meurer, W. J., Desmond, J. S. & Nallamothu, B. K. Effect of testing and treatment on emergency department length of stay using a national database. Acad. Emerg. Med. 19(5), 525–534 (2012).
Wallace, D. J. et al. Referral regions for time-sensitive acute care conditions in the United States. Ann. Emerg. Med. 72(2), 147–155 (2018).
Thatcher, J. L., Gilseth, T. A. & Adlis, S. Improved efficiency in acute myocardial infarction care through commitment to emergency department initiated primary PCI. J. Invasive Cardiol. 15(12), 693–698 (2003).
Boulanger, J. et al. Canadian stroke best practice recommendations for acute stroke management: Prehospital, emergency department, and acute inpatient stroke care, update 2018. Int. J. Stroke 13(9), 949–984 (2018).
Dasch, B. et al. Prevalence of therapeutic and diagnostic procedures in the last 14 days of life in hospital patients: A single-center observational study from Germany. Ann. Palliat. Med. 39(6), 972–981 (2021).
Smith, A. K. et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J. Pain Symptom Manage. 39(6), 972–981 (2010).
Smith, A. K. et al. Am I doing the right thing? Provider perspectives on improving palliative care in the emergency department. Ann. Emerg. Med. 54(1), 86–93 (2009).
Funding
The present study was supported by grants from the Clinical Medicine Research Institute at Chosun University Hospital (2022). This funding source had no role in the study design, execution, analyses, interpretation of the data, or decision to submit results.
Author information
Authors and Affiliations
Contributions
Drs. Ro and Lee had full access to all of the data in the study and take responsibility for the integrity of the data as well as the accuracy of the data analysis. Study concept and design: Drs. Ro, Lee, and Shin. Acquisition, analysis, or interpretation of data: Drs. Lee, Ro, Ko, and Kim. Drafting of the manuscript: Drs. Lee and Ro. Critical revision of the manuscript for important intellectual content: Drs. Ro, Kim and Shin. Statistical analysis: Drs. Lee and Ro. Obtained funding: Administrative, technical or material support: Drs. Ro, Ko, and Kim. Study supervision: Drs. Kim and Shin. Manuscript approval: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained errors in Tables 1 and 3. Full information regarding the corrections made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, S., Ro, Y., Shin, S. et al. Epidemiology of patients who died in the emergency departments and need of end-of-life care in Korea from 2016 to 2019. Sci Rep 13, 686 (2023). https://doi.org/10.1038/s41598-023-27947-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-27947-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.