Abstract
The transanal/perineal (ta/tp) endoscopic approach has been widely used for anorectal surgery in recent years, but carbon dioxide embolism is a possible lethal complication. The frequency of this complication in this approach is not known. In this study, we investigated the frequency of intraoperative (including occult) carbon dioxide embolism using transesophageal echocardiography. Patients who underwent surgery via the ta/tp approach and consented to participate were included. Intraoperative transesophageal echocardiography was used to observe the right ventricular system in a four-chamber view. Changes in end-tidal carbon dioxide (EtCO2), oxygen saturation (SpO2), and blood pressure were taken from anesthesia records. Median maximum insufflation pressure during the ta/tp approach was 13.5 (12–18) mmHg. One patient (4.8%) was observed to have a bubble in the right atrium on intraoperative transesophageal echocardiography, with a decrease in EtCO2 from 39 to 35 mmHg but no obvious change in SpO2 or blood pressure. By lowering the insufflation pressure from 15 to 10 mmHg and controlling bleeding from the veins around the prostate, the gas rapidly disappeared and the operation could be continued. Among all patients, the range of variation in intraoperative EtCO2 was 5–22 mmHg, and an intraoperative decrease in EtCO2 of > 3 mmHg within 5 min was observed in 19 patients (median 5 mmHg in 1–10 times).Clinicians should be aware of carbon dioxide embolism as a rare but potentially lethal complication of anorectal surgery, especially when using the ta/tp approach.
Similar content being viewed by others
Introduction
The transanal/transperineal (ta/tp) endoscopic approach is the only approach from below that can be used in anorectal endoscopic surgery and is useful in cases of a narrow pelvis, bulky tumor, or obesity, where it is difficult to reach the deep pelvis via a transabdominal approach1,2,3. However, with the growing number of cases, there has been an increase in the number of reports of carbon dioxide embolism (CDE) as a complication when using this technique4,5,6. CDE is a potentially fatal complication but is rare in laparoscopic surgery, with a frequency of 0.0014–0.6%7. On the other hand, it has been suggested that the incidence of CDE is higher with the ta/tp endoscopic approach (0.39–3.8%) than with laparoscopic surgery8,9. However, the exact incidence of CDE when using the ta/tp approach and ways to prevent and respond to it remain unclear.
Clinically significant CDE has a mortality rate as high as 28%10. In the management of CDE, early diagnosis and treatment are important for improving prognosis. Transesophageal echocardiography (TEE) is useful for the early diagnosis of CDE and is reported to be able to detect asymptomatic CDE by confirming bubbles in the right heart system. Studies using TEE in laparoscopic surgery have detected intracardiac bubbles in 69% of cholecystectomies, 17.1% of radical prostatectomies, and 100% of hysterectomies11,12,13. However, there are still few relevant reports on CDE using the ta/tp approach. The aims of this study were to investigate the frequency of subclinical CDE detected by monitoring with TEE during anorectal surgery and to find opportunities for early diagnosis of CDE.
Patients and methods
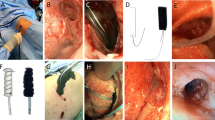
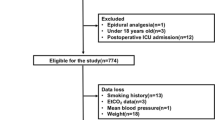
Patients who underwent surgery via the ta/tp approach for anorectal disease and who consented to participate in the study were included. Patients who were deemed unsuitable for TEE or who did not provide consent were excluded. Surgery was performed using the ta/tp approach as previously reported3,14,15,16. Briefly, total mesorectal excision was performed simultaneously (two-team approach) with the laparoscopic approach in the head-down position. Using the ta/tp approach, CO2 was insufflated using an AirSeal system (ConMed, Utica, NY) with high-flow smoke evacuation settings, and surgery was mainly performed using electrocautery. Ultrasonic incision devices and vessel sealers were used for larger vessels. Intraoperative TEE was used to observe the right ventricular system in a four-chamber view at the following time points: (1) before and after induction of anesthesia,(2) immediately after the start of insufflation,(3) immediately after starting the ta/tp approach,(4) when the insufflation pressure of the ta/tp approach was increased,(5) when EtCO2 decreased by > 3 mmHg within 5 min,(6) when significant bleeding occurred, and (7) at the end of insufflation. Blood gas tests were also performed at each of these time points. Changes in end-tidal carbon dioxide (EtCO2), oxygen saturation (SpO2), and blood pressure over time were taken from the anesthesia records. The grade of CDE was assessed by (1) presence of bubbles in the right atrium and (2) changes in EtCO2 and vital signs, as reported by Feigl et al. (Table 1)17.
The study was approved by the Fukuoka University Medical Ethics Committee (approval number U19-10-006). Informed consent was obtained from all patients who participated in the study. The study was conducted in accordance with the Declaration of Helsinki and followed the recommendations of the CONSORT Statement.
Results
Twenty-one patients were enrolled between November 2018 and June 2021. The patient background data are shown in Table 2. The indications for surgery were rectal cancer in 19 cases, chronicgranulomatosis in 1, and local recurrence of cervical cancer in 1. The transanal approach was used in 4 cases and the transperineal approach in 17. The surgical procedures were low anterior resection in 2 cases, intersphincteric resection in 2, abdominoperineal resection in 13, and total pelvic exenteration in 4. The median maximum insufflation pressure when the ta/tp approach was used was 13.512,13,14,15,16,17,18 mmHg.
The results of Intraoperative TEE monitoring are shown in Table 3. One case (4.8%) was observed to have a bubble in the right atrium; in this case, there was no change in blood pressure, SpO2, or pulse rate but there was a decrease in EtCO2 from 39 to 35 mmHg, and the patient was classified as grade 3. When the anesthesiologist confirmed the bubble by TEE (Supplemental Movie), the insufflation pressure was decreased from 15 to 12 mmHg to 10 mmHg until the surgeon identified the bleeding site, which was found to be a branch of the internal pudendal vein. Immediately after the bleeding was stopped, TEE confirmed that the bubble had disappeared. EtCO2 returned to its original value in 15 min and remained stable thereafter (Fig.1). There were no findings of right heart loading, even in the case where a bubble was observed in the right ventricular system by TEE. The surgery was continued using the two-team approach with TEE monitoring and was completed with no further complications.
No bubble was found in the right atrium on TEE in any other cases. Among all patients, the range of variation in intraoperative EtCO2 was 5–22 mmHg (median 16.5). A decrease in intraoperative EtCO2 by > 3 mmHg within 5 min was observed in 90.5% (19/21) of patients (median 5 mmHg in 1–10 times) but TEE revealed a bubble in the atrium in only 1 case.
Discussion
The incidence of CDE when performing anorectal surgery via the ta/tp approach has been increasingly reported in recent years8. At our institution, symptomatic CDE has occurred in 2 (1.6%) of 120 cases, which is similar to the 3 (4%) of 80 cases reported by Harnsberger et al9. On the other hand, occult (asymptomatic) CDE was observed in 1 (4.8%) of our 21 cases in this study, which was lower than the rate at which TEE detected asymptomatic CDE in various organs11,12,13.
The incidence of CDE is reported to be higher with the ta/tp approach than with routine laparoscopic surgery. Possible reasons for this are as follows: (1) ta/tp requires a high insufflation pressure to secure the operative field18; (2) the veins around the perineum are relatively large and flow into the systemic circulation; and 3) the high pelvic position results in low central venous pressure, which promotes uptake of CO2 easily when a small hole is formed.
A sudden decrease in SpO2 or blood pressure accompanied by a rapid decrease in EtCO2 should raise suspicion for CO2 embolism, which is diagnosed using TEE or transthoracic echocardiography19,20. However, the decrease in EtCO2 can fluctuate depending on various factors, such as ventilator settings. In our study, a decrease in EtCO2 by > 3 mmHg within 5 min, which is an indicator used to grade CDE, was observed a total of 77 times in 19 cases (1–10 times) without any sign of bubbles on TEE. Therefore, comprehensive judgment is necessary rather than relying on only changes in EtCO2 as an indicator of CDE. When performing operations in areas of the perineum with a well-developed venous plexus, it is important to be vigilant for CDE and changes in EtCO2, SpO2, or vital signs. A visible venous lumen in the absence of bleeding means that the insufflation pressure is higher than the central venous pressure, which increases the risk of CDE. If respiratory and circulatory changes are detected, CDE should be suspected and TEE used for a definitive diagnosis while promptly discontinuing delivery of air.
We have previously had a case of CDE during tp-TPE in which the patient's condition worsened due to delayed diagnosis of CDE and conversion to laparotomy was required21. Early detection and management of CDE is important to prevent a deteriorating situation. Early diagnosis of CDE and lowering of the insufflation pressure in the patient with asymptomatic CDE in our present study resulted in prompt disappearance of the bubble without serious complications, and surgery could be continued more safely with monitoring by TEE.
This study has several limitations. First, it included only 21 cases. Second, TEE was not performed continuously, so the possibility that some bubbles were missed cannot be excluded. Lack of continuous monitoring might be the reason for wide variation in the detection rate of bubbles across studies (17.1–100%)11,12,13. Finally, although TEE monitoring may contribute to early detection of CDE, it is not realistic to use this method routinely in the clinical setting because of the cost, equipment, and personnel required, and the need for prolonged placement in the esophagus. However, our experience is that if CDE is suspected, it can be diagnosed immediately by TEE, and if vital signs are stable after insufflation is stopped, surgery can be continued more safely with ta/tp by monitoring with TEE. Both surgeons and anesthesiologists should keep CDE in mind and collaborate closely to detect and manage this complication19,20.
Conclusions
In this study, TEE monitoring in patients undergoing anorectal surgery via a ta/tp approach detected asymptomatic CDE in 1 of 21 cases (4.8%). Clinicians should be aware of this rare but potentially lethal complication in view of the ever-increasing popularity of the ta/tp approach.
Data availability
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
References
Rouanet, P. et al. Transanal endoscopic proctectomy: An innovative procedure for difficult resection of rectal tumors in men with narrow pelvis. Dis. Colon. Rectum. 56(4), 408–415 (2013).
Tuech, J. J. et al. A step toward NOTES total mesorectal excision for rectal cancer: Endoscopic transanal proctectomy. Ann. Surg. 261(2), 228–233 (2015).
Araujo, S. E., Crawshaw, B., Mendes, C. R. & Delaney, C. P. Transanal total mesorectal excision: A systematic review of the experimental and clinical evidence. Tech. Coloproctol. 19(2), 69–82 (2015).
Shiraishi, T. et al. Carbon dioxide embolism during transanal total mesorectal excision (taTME). Tech. Coloproctol. 22(9), 735–738 (2018).
Bolshinsky, V., Shawki, S. & Steele, S. CO(2) embolus during transanal total mesorectal excision: Thoughts on aetiology. Colorectal Dis. 21(1), 6–7 (2019).
Ratcliffe, F., Hogan, A. M. & Hompes, R. CO(2) embolus: An important complication of TaTME surgery. Tech. Coloproctol. 21(1), 61–62 (2017).
Gutt, C. N. et al. Circulatory and respiratory complications of carbon dioxide insufflation. Dig. Surg. 21(2), 95–105 (2004).
Dickson, E. A. et al. Carbon dioxide embolism associated with transanal total Mesorectal excision surgery: A report from the international registries. Dis. Colon. Rectum. 62(7), 794–801 (2019).
Harnsberger, C. R. et al. CO(2) embolism can complicate transanal total mesorectal excision. Tech. Coloproctol. 22(11), 881–885 (2018).
Cottin, V., Delafosse, B. & Viale, J. P. Gas embolism during laparoscopy: A report of seven cases in patients with previous abdominal surgical history. Surg. Endosc. 10(2), 166–169 (1996).
Derouin, M., Couture, P., Boudreault, D., Girard, D. & Gravel, D. Detection of gas embolism by transesophageal echocardiography during laparoscopic cholecystectomy. Anesth. Analg. 82(1), 119–124 (1996).
Hong, J. Y., Kim, W. O. & Kil, H. K. Detection of subclinical CO2 embolism by transesophageal echocardiography during laparoscopic radical prostatectomy. Urology 75(3), 581–584 (2010).
Kim, C. S. et al. Venous air embolism during total laparoscopic hysterectomy: Comparison to total abdominal hysterectomy. Anesthesiology 111(1), 50–54 (2009).
Hompes, R. Reply to Gachabayov et al. ‘Consensus statement on TaTME other thoughts’. Colorectal Dis. 23(553), 5 (2021).
International expert consensus guidance on indications. implementation and quality measures for transanal total mesorectal excision. Colorectal Dis. 22(7), 749–755 (2020).
Hasegawa, S., Okada, T., Hida, K., Kawada, K. & Sakai, Y. Transperineal minimally invasive approach for extralevator abdominoperineal excision. Surg. Endosc. 30(10), 4620–4621 (2016).
Feigl, G. C. et al. Neurosurgical procedures in the semisitting position: evaluation of the risk of paradoxical venous air embolism in patients with a patent foramen ovale. World Neurosurg. 81(1), 159–164 (2014).
Adamina, M., Buchs, N. C., Penna, M. & Hompes, R. St. Gallen consensus on safe implementation of transanal total mesorectal excision. Surg. Endosc. 32(1091), 103 (2018).
MillerR. Miller’sanesthesia. 7th edition ed: UK: ChurchillLivingstone; 2009.
Mirski, M. A., Lele, A. V., Fitzsimmons, L. & Toung, T. J. Diagnosis and treatment of vascular air embolism. Anesthesiology 106(1), 164–177 (2007).
Matsumoto, Y. et al. A case of carbon dioxide embolism during the transperineal approach in total pelvic exenteration for advanced anorectal cancer. Asian J. Endosc. Surg. 14(1), 97–101 (2021).
Author information
Authors and Affiliations
Contributions
Y.M., S.H., Y.Y., and G.Y. wrote and revised the main manuscript text. R.O., R.K., T.M., H.N., A.K., N.A., K.M., K.S., and K.A. did data collection. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Video 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matsumoto, Y., Hasegawa, S., Ohno, R. et al. Detection of carbon dioxide embolism by transesophageal echocardiography during transanal/perineal endoscopic surgery: a pilot study. Sci Rep 12, 20487 (2022). https://doi.org/10.1038/s41598-022-24888-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-24888-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.