Abstract
This prospective study aimed to evaluate presepsin use as a biomarker of on postoperative infectious complications after gastrectomy, compared to C-reactive protein (CRP), white blood cells (WBCs), and neutrophils (Neuts). Overall, 108 patients were enrolled between October 2019 and December 2020. Presepsin, CRP, WBC, and Neut levels were measured preoperatively and on postoperative days (PODs) 1, 3, 5, and 7, using a postoperative morbidity survey. Grade II or higher infectious complications occurred in 18 patients (16.6%). Presepsin levels on all evaluated PODs were significantly higher in the infectious complication group than in the non-complication group (p = 0.002, p < 0.0001, p < 0.0001, and p = 0.025, respectively). The area under the curve (AUC) values were the highest for presepsin on PODs 3 and 7 (0.89 and 0.77, respectively) and similar to that of CRP, with a high value > 0.8 (0.86) on POD 5. For presepsin, the optimal cut-off values were 298 pg/mL (sensitivity, 83.3%; specificity, 83.3%), 278 pg/mL (sensitivity, 83.3%; specificity, 82.2%), and 300 pg/mL (sensitivity, 83.3%; specificity, 82%) on PODs 3, 5, and 7, respectively. Presepsin levels on PODs 3, 5, and 7 after gastrectomy is a more useful biomarker of postoperative infectious complications compared to CRP, WBCs, and Neuts, with a high sensitivity and specificity.
Similar content being viewed by others
Introduction
Gastric cancer is the fourth leading cause of cancer-related deaths and the fifth most common cancer worldwide1. The incidence and mortality of gastric cancer are increased in men compared to those in women2. Gastrectomy with lymph node dissection is the only method for curing gastric cancer3. The standardization of surgical techniques and perioperative management, as well as improved instrumentation, have led to a low mortality of approximately 1.5% according to the National Clinical Database (NCD)4 in Japan. However, the morbidity rates are still high, at 14.2% for distal gastrectomy5 and 21.5% for total gastrectomy6. Postoperative complications of gastric cancer reduce long-term prognosis7, and high postoperative C-reactive protein (CRP) levels are related to poor prognosis8. Therefore, the early detection of infectious complications at a clinically asymptomatic stage is important to prevent serious complications.
CRP is often used as an inflammatory biomarker because of its simplicity, versatility, and low cost9. However, the CRP levels do not increase in the early stages of infection and have the disadvantage of a slow peak or half-life10. In addition, the CRP levels are elevated in various inflammatory conditions other than infection, as well as in invasion such as surgery and trauma, thus making it difficult to determine whether they indicate the presence of infection in clinical practice.
Presepsin, which is the soluble fraction of cluster of differentiation 14 (CD14), is thought to be associated with infections11, based on the fact that a subtype of CD14 is present inside and on the cell membranes of macrophages, monocytes, and granulocytes, and is responsible for intracellular transduction of endotoxin signals. Presepsin is a novel biomarker for infection and sepsis. The presepsin levels are increased early in the development of sepsis12,13 and are less sensitive to invasion, such as trauma14. However, few reports have examined the usefulness of presepsin as a biomarker for infectious complications after gastrointestinal surgery15,16,17, and there have been no relevant reports following gastrectomy.
In laparoscopic sleeve gastrectomy for bariatric surgery, presepsin was more useful for gastric leaks than CRP, white blood cells (WBCs), and neutrophils (Neuts), but not for gastric cancer18. However, there have been reports on presepsin as a biomarker of postoperative infectious complications for other cancer types or gastric interventions. Therefore, we hypothesized that presepsin would be useful for infectious complications after gastrectomy for gastric cancer.
This study aimed to evaluate the usefulness of presepsin for determining infectious complications after gastrectomy for gastric cancer, compared with CRP, WBCs, and Neuts.
Results
Patients’ characteristics and morbidity
In total, 108 patients who underwent gastrectomy were enrolled in this study. Of these, 75 were men and 33 were women, with a median age of 71 years. The American Society of Anesthesiologists (ASA) scores, surgical dates, and pathological characteristics are shown in Table 1.
Infectious complications occurred postoperatively in 18 patients (16.6%) (Table 2). Anastomotic leakage was the most commonly observed complication (n = 7), followed by abdominal abscess (n = 4), pancreatic fistula (n = 3), pneumonia (n = 2), cholecystitis (n = 1), and urinary tract infection (n = 1). The median time of infectious disease diagnosis after gastrectomy was 5.8 days.
When the patients’ characteristics were compared between the complication and non-complication groups, there were no significant differences in the patients’ background characteristics, including age, sex, ASA score, or surgical date (Table 3). Regarding surgical factors, only the amount of blood loss was higher in the complication group than in the non-complication group.
Biomarker levels
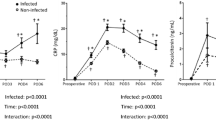
The box plot of each biomarker in the perioperative change is shown in Fig. 1a–d. In the 90 patients with no infectious complications, median presepsin levels were 157 pg/mL (25th to 75th percentile: 33–707 pg/mL) and 180 pg/mL (64–1134 pg/mL), 169 pg/mL (56–621 pg/mL), 159 pg/mL (35–792 pg/mL), and 165 pg/mL (48–997 pg/mL), preoperatively and on PODs 1, 3, 5, and 7, respectively. The postoperative values were the same as the preoperative values. In the 18 patients with postoperative infectious complications, the median presepsin levels were 161 pg/mL (25th to 75th percentile: 50–430 pg/mL) and 263 pg/mL (150–1446 pg/mL), 360 pg/mL (211–1097 pg/mL), 450 pg/mL (128–1251 pg/mL), and 380 (76–650 pg/mL), respectively. Preoperative measurements of the presepsin levels were not significantly different between the non-complication and complication groups (p = 0.45). However, presepsin levels on PODs 1, 3, 5, and 7 (p = 0.002, p < 0.0001, p < 0.0001, and p = 0.025, respectively) were significantly higher in the complication group compared to the non-complication group (Table 4).
CRP, WBC, and Neut levels, unlike presepsin, increased and then decreased postoperatively, regardless of infectious complications. CRP and presepsin levels were not significantly different preoperatively between the two groups (p = 0.77), but were significantly higher in the complication group than in the non-complication group on PODs 1, 3, 5, and 7 (p = 0.03, p < 0.0001, p < 0.0001, p = 0.03, respectively). WBC and Neut levels showed no significant differences between the complication and non-complication groups preoperatively (p = 0.24 and 0.45, respectively) and on POD 1 (p = 0.06 and 0.09, respectively), but were significantly higher in the complication group than in the non-complication group on PODs 3 (p = 0.003 and 0.0002, respectively), 5 (p = 0.01 and 0.012, respectively), and 7 (p = 0.01 and 0.01, respectively).
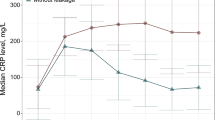
Receiver operator characteristics analysis of the biomarker
We compared the AUC values of presepsin, CRP, WBC, and Neuts, on PODs 1, 3, 5, and 7 between the groups (Fig. 2a–d). The AUC values in the pooled prediction model were comparable to those considered separately. The AUC values were highest for presepsin on PODs 1, 3, and 7 (0.731, 0.89, and 0.77, respectively). On POD 5, the AUC value of presepsin was similar to that of CRP, with a high value > 0.8 (0.86). The AUC values of presepsin were > 0.7 on all days, including on PODs 1, 3, 5, and 7.
Then, the ROC curve was used to calculate the cut-off value for each infectious complication of the PODs (Table 5). On POD 1, the sensitivity and positive predictive value (PPV) of presepsin exceeded 90%, but the specificity and negative predictive value (NPV) were generally as low as 50%. For CRP, WBCs, and Neuts, all values for sensitivity, specificity, the PPV, and NPV were low at 50–70%. On PODs 3, 5, and 7, all the values for sensitivity, specificity, the PPV, and NPV exceeded 80% for presepsin. However, CRP and WBCs showed sensitivity and a PPV that exceeded 80% on PODs 3, 5, and 7, and Neuts showed sensitivity and a PPV exceeding 80% on PODs 5 and 7. For the other parameters, except for presepsin, specificity and NPV did not exceed 80% at any time postoperatively.
Discussion
Several meta-analyses have reported that presepsin is a valuable biomarker for sepsis19,20,21. However, there are few reports on the relationship between postoperative infectious complications and presepsin levels15,16,17,22,23. Moreover, there are only two reports on postoperative gastrointestinal surgery15,16,17, and to the best of our knowledge there have been no reports on postoperative gastrectomy. The results of the present study showed, for the first time, that presepsin was useful as a biomarker for determining infectious complications after gastrectomy for gastric cancer, both in terms of sensitivity and specificity. High postoperative CRP levels are related to poor prognosis of gastric cancer 8. Therefore, in the early detection of infectious complications, presepsin is useful in improving prognosis because it allows for appropriate therapeutic intervention, thereby contributing in minimizing elevated CRP levels.
Cikot et al. reported that presepsin is a useful biomarker for gastrointestinal anastomotic leakage16. However, Cikot et al. revealed that the only intended complication was anastomotic leakage, and the details of the surgical procedure, including the operative time, blood loss, and surgical approach, were unknown. Therefore, the effect of surgical invasiveness remains unknown. In a series of 30 cases, Takeuchi et al. reported that presepsin was an accurate diagnostic marker of postoperative infectious complications after esophagectomy15, and they also compared presepsin to procalcitonin preoperatively, immediately post-surgery, and on PODs 1, 2, 3, 5, and 7. Nevertheless, the sample size of the study was small.
In our study, presepsin had some advantages over other parameters, with a sensitivity and specificity > 80% on PODs 3, 5, and 7. However, on POD 1, presepsin showed low specificity (54.6%) and high sensitivity (94.4%). The median number of days of diagnosis of infectious complications was 5.8 days after gastrectomy. Three patients had onset of an infectious complication on POD 3, and none had onset of an infectious complication before that. In addition, seven patients developed infectious complications after POD 7. This supports the low specificity of presepsin on POD 1 because postoperative adverse events had not yet occurred.
Shi et al. reported that CRP levels on PODs 3 and 5 were significantly useful in the diagnosis of infectious complications after gastrectomy24. Our results similarly showed that serum levels of CRP on PODs 3 and 5 were useful inflammatory biomarkers, with an AUC value of 0.8 or higher. However, the specificity of presepsin was higher than that of CRP. In the non-complication group, CRP, WBC, and Neut levels were transiently elevated due to the effects of surgical invasion, but the levels of presepsin did not change. Although esophagectomy is one of the most invasive surgical procedures in gastrointestinal surgery, Takeuchi et al. reported that presepsin levels did not change significantly after esophagectomy in the non-complication group15. This finding indicates that presepsin expression was not affected by postoperative invasion. Amanai et al. reported that prespsin levels did not change significantly after colorectal surgery but increased with infectious complications, making it a useful marker when used in combination with CRP17.
The reference range for presepsin from healthy volunteers assayed using the PATHFAST presepsin assay was 314 pg/mL or less25. This value was close to the cut-off value for postoperative infectious complications in our study. Furthermore, the cut-off values remained almost the same for all periods (PODs 3, 5, and 7) and can be interpreted as a risk of postoperative infectious complications if they exceed the reference values. However, the cut-off value of CRP was different for each period, and the cut-off value was much higher than the reference value (< 0.8 mg/mL), making it difficult to determine postoperative infectious complications.
The present study has several limitations that need to be acknowledged. First, this was a single-center study limited to the Japanese population. However, we believe that the infectious complication rate in this study is comparable to that of the NCD in Japan and is consistent with that in the perioperative period of gastrectomy for gastric cancer, as gastrectomy has been performed in recent years with a high percentage of laparoscopic procedures. Second, only presepsin and routine blood test variables, such as CRP, WBC, and Neut levels, were measured, whereas other inflammatory biomarkers, such as procalcitonin, were not. There are reports that procalcitonin is useful for the accurate diagnosis of infectious complications after gastrectomy for gastric cancer26,27, but there are no reports directly comparing procalcitonin and presepsin. Presepsin has been reported to be superior to procalcitonin in the diagnosis of infectious complications after esophagectomy for esophageal cancer15. Therefore, it is necessary to compare presepsin with procalcitonin in the future, and to examine whether the combined use of these inflammatory biomarkers will improve diagnostic accuracy. Third, the number of patients with infectious complications was low at 18 (16.6%). Since the rate of complications is not high, the cost-effectiveness of routine measurement of presepsin should be further considered. Finally, because of the difference in presepsin levels between the non-complication and complication groups on POD 1, it is crucial to consider whether there are factors other than infectious complications that affect presepsin. Unlike other biomarkers, presepsin is less affected by postoperative invasion15,17. No significant differences were found in patients’ background characteristics, including age, sex, ASA score, disease state, or surgical date between the non-complication and complication groups. Therefore, case accumulation and multivariate analysis are required to examine influencing factors.
Presepsin levels on PODs 3, 5, and 7 after gastrectomy for gastric cancer are valuable biomarkers for detecting postoperative infectious complications, compared with other inflammatory biomarkers such as CRP, WBCs, and Neuts. Presepsin is a very simple biomarker that can be used to suspect postoperative infectious complications when the reference value is exceeded, even after gastrectomy, regardless of the number of postoperative days.
Methods
Ethics statements
This study protocol was conducted in accordance with the Declaration of Helsinki and its latest amendments. The study protocol was approved by the ethics committee of Osaka Medical and Pharmaceutical University Hospital (approval number: 2020-005). Informed consent was obtained from all patients.
Patients
This was a single-institution prospective observational study. Between October 2019 and December 2020, 113 patients with gastric cancer underwent curative gastrectomy at Osaka Medical and Pharmaceutical University Hospital in Japan. Two patients who did not give consent for this study, two patients with active infection before gastrectomy, and one patient undergoing emergency surgery for bleeding, were excluded. Therefore, data from 108 patients were analyzed in the present study.
Measurements and study endpoint
We measured presepsin in addition to CRP, WBCs, and Neuts, which are usually measured in the perioperative period. We examined presepsin by collecting at least 2 mL of blood samples preoperatively and at 1, 3, 5, and 7 days post-gastrectomy, at 7:00 a.m. Presepsin was measured with a fully automated immunoassay analyzer (PATHFAST, LSI Medience Corporation, Tokyo, Japan), according to the manufacturer’s instructions25. For patients with infectious complications, the blood samples collected after the onset of complications were not included in the analysis. The primary endpoint was the ability of presepsin to detect postoperative infectious complications in patients who underwent curative gastrectomy for cancer.
Surgical procedures
Lymph node dissection, surgery, and gastric reconstruction were performed according to the Japanese Gastric Cancer Treatment Guidelines28. At our institute, almost all resections for gastric cancer are performed laparoscopically or robotically regardless of the clinical stage, except for clinical trials limited to open surgical procedures and emergency surgery, such as surgery for perforation or acute bleeding. The pathological stage and residual tumor status were confirmed according to the Japanese classification of gastric carcinoma29.
Perioperative management
At our institute, the enhanced recovery after surgery protocol has been introduced in perioperative care30. The patients took 250 mL of an oral carbohydrate solution at night before surgery and 2 h before anesthesia. On POD 1, the patients started walking and were allowed to drink clear fluid. The patients started to ingest a liquid diet on POD 2, after which the diet was continued through four daily steps to eventually consume regular food on POD 6. Acetaminophen was administered orally twice daily until POD 5. Prophylactic antimicrobials were administered before incision and 3 h after the first dose during the surgical operation.
Postoperative complications
Postoperative complications were diagnosed up to 30 days after the gastrectomy. Pancreatic fistula was diagnosed based on the definitions of the International Study Group on Pancreatic Fistula31. Anastomotic leakage was diagnosed via a radiological examination using an orally administered contrast medium.
Statistical analysis
All statistical analyses were performed using JMP Pro 15 (version 15, SAS Institute, Cary, NC, USA). Continuous variables are presented as mean ± standard deviation and were compared using the Wilcoxon rank-sum test. The chi-square test and Fisher exact probability test were used to compare the differences in categorical variables between the complication and non-complication groups. Receiver operating characteristic (ROC) analysis was performed to assess the diagnostic accuracy of infectious complications by evaluating the area under the curve (AUC). An AUC ≥ 0.8 was considered to show high diagnostic accuracy, with those closest to 1 considered to be the most predictive. Statistical significance was set at p < 0.05.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN sstimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Yao, Q., Qi, X. & Xie, S. H. Sex difference in the incidence of cardia and non-cardia gastric cancer in the United States, 1992–2014. BMC Gastroenterol. 20, 418 (2020).
Colvin, H. et al. Gastroenterological surgery in Japan: the past, the present and the future. Ann. Gastroenterol. Surg. 1, 5–10 (2017).
Hasegawa, H. et al. Surgical outcomes of gastroenterological surgery in Japan: Report of the National Clinical Database 2011–2017. Ann. Gastroenterol. Surg. 3, 426–450 (2019).
Kunisaki, C. et al. Modeling preoperative risk factors for potentially lethal morbidities using a nationwide Japanese web-based database of patients undergoing distal gastrectomy for gastric cancer. Gastric Cancer 20, 496–507 (2017).
Kikuchi, H. et al. Development and external validation of preoperative risk models for operative morbidities after total gastrectomy using a Japanese web-based nationwide registry. Gastric Cancer 20, 987–997 (2017).
Tokunaga, M., Tanizawa, Y., Bando, E., Kawamura, T. & Terashima, M. Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann. Surg. Oncol. 20, 1575–1583 (2013).
Kurokawa, Y. et al. Prognostic value of postoperative C-reactive protein elevation versus complication occurrence: A multicenter validation study. Gastric Cancer 23, 937–943 (2020).
Oliveira, C. F. et al. Procalcitonin versus C-reactive protein for guiding antibiotic therapy in sepsis: a randomized trial. Crit. Care Med. 41, 2336–2343 (2013).
Vigushin, D. M., Pepys, M. B. & Hawkins, P. N. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J. Clin. Invest. 91, 1351–1357 (1993).
Shozushima, T. et al. Usefulness of presepsin (sCD14-ST) measurements as a marker for the diagnosis and severity of sepsis that satisfied diagnostic criteria of systemic inflammatory response syndrome. J. Infect. Chemother. 17, 764–769 (2011).
Liu, B., Chen, Y. X., Yin, Q., Zhao, Y. Z. & Li, C. S. Diagnostic value and prognostic evaluation of presepsin for sepsis in an emergency department. Crit. Care 17, R244 (2013).
Ulla, M. et al. Diagnostic and prognostic value of presepsin in the management of sepsis in the emergency department: A multicenter prospective study. Crit. Care 17, R168 (2013).
Hoshino, K. et al. Incidence of elevated procalcitonin and presepsin levels after severe trauma: a pilot cohort study. Anaesth. Intensive Care 45, 600–604 (2017).
Takeuchi, M. et al. The perioperative presepsin as an accurate diagnostic marker of postoperative infectious complications after esophagectomy: A prospective cohort study. Esophagus 17, 399–407 (2020).
Cikot, M. et al. The importance of presepsin value in detection of gastrointestinal anastomotic leak: A pilot study. J. Surg. Res. 228, 100–106 (2018).
Amanai, E. et al. Usefulness of presepsin for the early detection of infectious complications after elective colorectal surgery, compared with C-reactive protein and procalcitonin. Sci. Rep. 12, 3960 (2022).
Binboga, S. et al. Plasma presepsin in determining gastric leaks following bariatric surgery. Turk. J. Biochem. 44, 565–573 (2019).
Zhang, X., Liu, D., Liu, Y. N., Wang, R. & Xie, L. X. The accuracy of presepsin (sCD14-ST) for the diagnosis of sepsis in adults: A meta-analysis. Crit. Care 19, 323 (2015).
Wu, J., Hu, L., Zhang, G., Wu, F. & He, T. Accuracy of presepsin in sepsis diagnosis: A systematic review and meta-analysis. PLoS ONE 10, e0133057 (2015).
Tong, X. M., Cao, Y. T., Yu, M. & Han, C. W. Presepsin as a diagnostic marker for sepsis: Evidence from a bivariate meta-analysis. Ther. Clin. Risk Manag. 11, 1027–1033 (2015).
Clementi, A. et al. Presepsin and procalcitonin levels as markers of adverse postoperative complications and mortality in cardiac surgery patients. Blood Purif. 47, 140–148 (2019).
Koakutsu, T., Sato, T., Aizawa, T., Itoi, E. & Kushimoto, S. Postoperative changes in presepsin level and values predictive of surgical site infection after spinal surgery: A single-center, prospective observational study. Spine (Phila Pa 1976) 43, 578–584 (2018).
Shi, J. et al. Clinical predictive efficacy of C-reactive protein for diagnosing infectious complications after gastric surgery. Therap. Adv. Gastroenterol. 13, 1756284820936542 (2020).
Okamura, Y. & Yokoi, H. Development of a point-of-care assay system for measurement of presepsin (sCD14-ST). Clin. Chim. Acta 412, 2157–2161 (2011).
Yang, W. C. et al. Procalcitonin as an early predictor of intra-abdominal infections following gastric cancer resection. J. Surg. Res. 258, 352–361 (2021).
Thereaux, J. A commentary on: diagnostic accuracy of procalcitonin as an early predictor of infection after radical gastrectomy for gastric cancer: A prospective bicenter cohort study. Int. J. Surg. 75, 150–151 (2020).
Japanese Gastric Cancer Association. Japanese Gastric Cancer Treatment Guidelines 2018 (5th edition). Gastric Cancer 24, 1–21 (2021).
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer English edition 14, 101–112 (2011).
Tanaka, R. et al. Protocol for enhanced recovery after surgery improves short-term outcomes for patients with gastric cancer: a randomized clinical trial. Gastric Cancer 20, 861–871 (2017).
Bassi, C. et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138, 8–13 (2005).
Acknowledgements
The authors would like to thank the staff at the Departments of General and Gastroenterological Surgery at Osaka Medical and Pharmaceutical University. We would like to also thank Editage (www.editage.com) for English language editing. This research was partially supported by a grant from the Japan Society for the Promotion of Science KAKENHI (Grant number: 2787).
Author information
Authors and Affiliations
Contributions
Y.I., R.T., K.H., K.M., and S.-W.L. conceived and design the study. Y.I., R.T., K.H., and K.M. acquired the data. Y.I. and K.T. analyzed and interpreted the data. Y.I. and S.-W.L. drafted the original manuscript. Y.I., R.T., K.T., M.A., and S.-W.L. reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Imai, Y., Tanaka, R., Honda, K. et al. The usefulness of presepsin in the diagnosis of postoperative infectious complications after gastrectomy for gastric cancer: a prospective cohort study. Sci Rep 12, 21289 (2022). https://doi.org/10.1038/s41598-022-24780-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-24780-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.