Abstract
The infant mortality rate remains unacceptably high in sub-Saharan African countries. Ethiopia has one of the highest rates of infant death. This study aimed to identify individual-and community-level factors associated with infant death in the rural part of Ethiopia. The data for the study was obtained from the 2016 Ethiopian Demographic and Health Survey. A total of 8667 newborn children were included in the analysis. The multilevel logistic regression model was considered to identify the individual and community-level factors associated with new born mortality. The random effect model found that 87.68% of the variation in infant mortality was accounted for by individual and community level variables. Multiple births (AOR = 4.35; 95%CI: 2.18, 8.69), small birth size (AOR = 1.29; 95%CI: 1.10, 1.52), unvaccinated infants (AOR = 2.03; 95%CI: 1.75, 2.37), unprotected source of water (AOR = 1.40; 95%CI: 1.09, 1.80), and non-latrine facilities (AOR = 1.62; 95%CI: 1.20) were associated with a higher risk of infant mortality. While delivery in a health facility (AOR = 0.25; 95%CI: 0.19, 0.32), maternal age 35–49 years (AOR = 0.65; 95%CI: 0.49, 0.86), mothers receiving four or more TT injections during pregnancy (AOR = 0.043, 95% CI: 0.026, 0.071), and current breast feeders (AOR = 0.33; 95% CI: 0.26, 0.42) were associated with a lower risk of infant mortality. Furthermore, Infant mortality rates were also higher in Afar, Amhara, Oromia, Somalia, and Harari than in Tigray. Infant mortality in rural Ethiopia is higher than the national average. The government and other concerned bodies should mainly focus on multiple births, unimproved breastfeeding culture, and the spacing between the orders of birth to reduce infant mortality. Furthermore, community-based outreach activities and public health interventions focused on improving the latrine facility and source of drinking water as well as the importance of health facility delivery and received TT injections during the pregnancy.
Similar content being viewed by others
Introduction
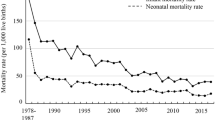
The infant mortality rate is the most significant public health predictor, as it represents children’s and communities’ access to basic health measures such as vaccination, infectious disease care treatment, and proper nutrition1. The Sustainable Development Goals (SDG) child mortality objective seeks to bring an end to preventable deaths of newborns and children under-five years of age by 2030, with all countries aiming to reduce newborn mortality to at least as low as 12 deaths per 1000 live births and under-five mortality to at least as low as 25 deaths per 1000 live births. In 2018, 4.1 million children died worldwide in their first year of life2,3,4,5.More than one million children die in Africa alone before celebrating their first birthday. These values are approximately equivalent to 2,808 deaths per single day or about two deaths every minute. Since the Millennium Development Goals (MDGs) were adopted, the countries of Sub-Saharan Africa have achieved incredible success and increases in infant survival, but the infant mortality rate in Sub-Saharan Africa is still the highest in the global region2,3,4,5. Ethiopia has one of the highest infant mortality rates in the world5,6. In rural Ethiopia, the infant mortality rate is 62 deaths per 1000 live births. This infant mortality is substantially higher than the SDG targets of 12 deaths per 1000 live births5,7,8.
The Ethiopian government is working to reduce child deaths and reforms have been made in recent years. In the rural part of Ethiopia, maternal complications during childbirth, immediate exclusive breast-feeding, birth interval, maternal socioeconomic characteristics, and health service seeking actions, etc., are still major challenges9,10. In order to prepare and enforce an initiative and take steps to address the burden of newborn deaths in the rural areas of Ethiopia, identification of the enumeration area specific factors on infant mortality is therefore necessary4,11.
Previous studies have concluded that infants born in rural areas are more at risk of death than infants born in urban areas12,13,14,15,16,17. In Ethiopia, infant mortality in rural areas is a major challenge7,9. Understanding the causes of infant mortality in rural regions is crucial if we are to reduce Ethiopia's high infant mortality rate. Furthermore, the estimated infant mortality rate in this country was greater in rural areas (62 per 1000 live births) than in urban areas (54 per 1000 live births) and compared to the national average (48 per 1000 live births)7,18. Although various studies have been undertaken in Ethiopia to investigate infant death rates and risk factors16,17,19,20, little study has been conducted in rural Ethiopia. This lack of epidemiologic study limits our understanding of the determinant to prioritize for evidence-based programming in this high-risk region of infant mortality. Previous studies in Ethiopia on the risk factors for infant mortality were also institutionally focused21,22, and only looked at individual-level factors19,21,22. However, community-level variables such as the source of drinking water23, type of toilet facilities23, cluster (enumeration area)23,24, and region23,24 may all have an effect on infant mortality.
Furthermore, the Ethiopian Demographic and Health Survey (EDHS) used a multistage cluster sampling procedure in which individuals were nested in clusters and infant mortality was correlated with these clusters7,18. This violates the assumption of independence, which may introduce a significant bias in programmatic implementation by implying that contextual variables are not taken into account in the study. For example, researchers discovered that geographic access to health care has an impact on infant mortality. Contextual variables, such as the region of respondents, enable researchers to investigate how a wide range of environmental factors may influence health and well-being25. To address this, we used a multilevel logistic regression model to examine variables associated with infant mortality at individual and community levels25,26. This study aimed to identify individual- and community-level factors associated with infant death in the rural parts of Ethiopia.
Methods
Study design and setting
This study was conducted in Ethiopia, which is the second-most populated country in Africa, after Nigeria, and is located in the Horn of Africa. Ethiopia has nine regional states (Tigray, Afar, Amhara, Oromiya, Somali, BenishangulGumuz, Southern Nations Nationalities and People (SNNP), Gambela, and Harari) as well as two city administrations (Addis Ababa and Dire Dawa). We used secondary data from the 2016 EDHS.
Sampling and data measurements
The 2016 EDHS employed stratified and cluster multistage sampling, with the goal of being representative at the regional and national levels in terms of appropriate demographic and health indicators. In the first stage, 645 clusters (202 in urban areas and 443 in rural areas) were selected using a probability proportional to cluster size and independent selection in each sampling stratum. In the second stage, random samples of 18,008 households were drawn from all identified EAs. A total of 15,683 women aged 15–49 were interviewed. Data was collected from 18 January to 27 June 2016. The sample size for EDHS was determined using a multistage sampling procedure that took into account sampling variation7.
Study variables
Outcome variables
The response variable of this study was the status of infant mortality. Infant mortality is defined as the risk of a child dying between birth and their first birthday. This takes a binary outcome; so infant death is classified as either death (1 = if the infant died between birth and their first birthday) or alive (0 = if the infant was alive between birth and their first birthday).
Independent Variables
The possible predictor variables associated with infant mortality will be categorized as individual-level factors and community-level factors. These variables were chosen based on previous knowledge and existing literature12,13,14,15,16,19 (Table 1).
Data management and analysis
The variables were extracted from the BR dataset using SPSS software version 21, and then exported to the statistical software R version 3.5.3 for further analysis. Data were weighted after extraction using sampling weight (v005), main sampling unit (v023), and strata (v021) to account for unequal probability of selection and non-response. Descriptive analysis was done and sample characteristics were presented in frequency and percentages to show the distribution of respondents by the selected variables. The data in EDHS were not flat and were collected using multistage stratified cluster sampling techniques. To draw valid inferences and conclusions, advanced statistical models such as hierarchical modelling, which consider independent variables measured at the individual and community levels, should be used to account for the clustering effect/dependency. A two-level multilevel logistic regression analysis was used to examine the effects of individual- and community-level characteristics on infant death and to determine the extent to which characteristics at the individual and community levels explain enumeration area variations in infant death in rural Ethiopia. The reason for using multilevel logistic regression model was to account for the hierarchical (correlated) structure of the data. The assumption is that infant and their households are nested within enumeration area (communities). This suggests that infant in households with similar characteristics can have different health outcomes when residing in different communities with different characteristics. The log of the probability of infant death was modeled using a two-level multilevel model as follows:
where, \(i\) and \(j\) are the level 1 (individual) and level 2 (community) units, respectively; \(X\) and \(Z\) refer to individual and community-level variables, respectively; \(\pi_{ij}\) is the probability of infant death for the ith women in the jth community; the \(\beta\) indicates the fixed coefficients. Whereas, \(\beta_{0}\) is the intercept-the effect on the probability of infant death in the absence of influence of predictors; and \(u_{j}\) showed the random effect (effect of the community on infant death for the jth community and \(e_{ij}\) showed random errors at the individual levels. By assuming each community had different intercept (\(\beta_{0}\)) and fixed coefficient (\(\beta\)), the hierarchical (clustered) data nature and the within and between community variations were taken into account. Four models were fitted to identify community and individual level factors associated with infant death. The first model (Model 1 or empty model) contained no explanatory variables, but was fitted to decompose the total variance into its individual- and community-level components. The second model (Model 2) considered only the individual-level variables in order to examine the individual-level effect. The third model (Model 3) considered only the community-level variables in order to examine the effect of community-level factors on infant death, independent of other factors. The fourth model (Model 4) is the full model that incorporated all the individual and community-level variables into the multilevel analysis. Fitting the final model involved two steps. First, stepwise logistic regression analysis was done to identify the key variables associated with infant death. Second, all the variables selected from the stepwise logistic regression models were incorporated into the multilevel modeling. For the result of fixed effect, odds ratio (ORs) with 95% confidence intervals (CIs) was used to declare statistical significance. The P-value ≤ 0.05 has been considered as statistically significant. The measures of variation (random-effects) were summarized using ICC, Median Odds Ratio (MOR) and proportional change in variance (PCV) to measure the variation between enumeration areas (clusters). ICC is a measure of within-cluster variation, the variation between individuals within the same cluster, and it was calculated using the formula: \( ICC = ~\frac{{V_{A} }}{{V_{A} + {\raise0.7ex\hbox{${\pi ^{2} }$} \!\mathord{\left/ {\vphantom {{\pi ^{2} } 3}}\right.\kern-\nulldelimiterspace} \!\lower0.7ex\hbox{$3$}}}} = ~\frac{{V_{A} }}{{V_{A} + 3.29}} \) , where \({V}_{A}\) is the estimated variance in each model, which has been described elsewhere27. The total variation attributed to individual or/and community level factors at each model was measured by the proportional change in variance (PCV), which was calculated as: \(CV= \frac{{V}_{A}-{V}_{B}}{{V}_{A}}\) , where \({V}_{A}\) = variance of the initial model, and \({V}_{B}\) = variance of the model with more terms25. The MOR is the median odds ratio between the individual of higher propensity and the individual of lower propensity when comparing two individuals from two different randomly chosen clusters and it measures the unexplained cluster heterogeneity, the variation between clusters by comparing two persons from two randomly chosen different clusters. It was computed using the formula:
\(MOR=\mathrm{exp}(\sqrt{2*{V}_{A}*0.6745} )\approx \mathrm{exp}(0.95\sqrt{{V}_{A}} )\), where \({V}_{A}\) is the cluster level variance25,27. The MOR measure is always greater than or equal to 1. If the \(MOR\) is 1, there is no variation between clusters 27. The generalized variance-inflation factor (GVIF) test was used to check for multicollinearity; the findings showed that there no multicollinearity because the GVIF for each variable was less than 5. Model comparison was done using Deviance Information Criteria (DIC), Akaike’s Information Criterion (AIC) and Bayesian’s Information Criterion (BIC). The model with the smallest value of the information criterion was selected as the final model of the analysis27.
Ethical Issues.
Publicly available EDHS 2016 data was used for this study. Informed consent was taken from each participant, and all identifiers were removed.
Confirmation of methods
Author(s) confirm that all methods were carried out in accordance with relevant guidelines and regulations in the manuscript.
Results
Socio-demographic and obstetric characteristics of the study respondents
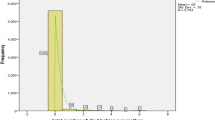
The total number of infants participated in this study was 8667. 6568 (73.8%) of them were born at home, and 4467 (51.1%) of them were males. 6509 (75.1%) of mothers were housewives and 6267 (72.3%) had no formal education. About 8439 (97.4%) infants were born as singletons and 5625 (64.9%) infants were born into low-income household. The majority; 7129 (82.3%) of mothers have used improved sources of drinking water. About 5350 (61.7%) of mothers did not have visits during pregnancy and 5857 (67.6%) of women did not receive tetanus injection during pregnancy. 4675 (53.9%) of mothers had 3 or above ever-born children and only 458 (5.3%) infants were not breastfeeding at all (Table 2).
Factors associated with the infant death
The result of the multilevel logistic regression model was summarized in Table 2. The model selection result indicated that model IV was a better fit to the data as compared to other reduced models, since it has the smallest AIC, BIC, and deviance statistic. The final selected model (model IV) showed that antenatal care visit, preceding birth interval, number of TT injections, education level of the mother, family size, vaccination of the child, contraceptive use, child twin, place of delivery, diarrhea status, size of child at birth, marital status, number of living children, breastfeeding, region, water source, and latrine facility type were found to have a statistically significant association with infant mortality (Table 3 and Table 4).
Individual-level factor
The odds of infant death among mothers who had four or more ANC visits during their pregnancy was 0.787 (AOR = 0.787, 95%CI: 0.645, 0.961) times lower as compared to mothers who had no ANC visits during their pregnancy. The odds of infant death for infants with preceding birth interval less than 2 years were increased by 27% (AOR = 0.724, 95%CI: 0.624, 0.839) compared to infants with preceding birth interval more than 2 years. The odds of infant death among multiple birth were 4.35 (AOR = 4.350; 95% CI, 2.179, 8.685) times higher as compared to singletons. Infants born to mother who attained primary education had 0.859 (AOR = 0.859; 95% CI: 0.739, 0.998) times lower likelihood of infant death than infants whose mother did not have formal education. The odds of infant death who are born at the health facility were 0.249 (AOR = 0.249; 95% CI, 0.193, 0.321) times lower as compared to children who are born at home. Infants who had not received vaccination had a 2.033 (AOR = 2.033; 95% CI, 1.745, 2.370) times higher risk of death than infants who had received vaccination. The odds of infant death were 1.29 (AOR = 1.290; 95% CI, 1.096, 1.519) times higher in infants born with a small birth size compared to infants born with a large birth size. As compared to separated mothers, married mothers had 0.670 (AOR = 0.670; 95% CI, 0.485, 0.925) times lower odds of infant death. The odds of infant death among mothers who received TT injections 4 and above times during pregnancy was 0.043 (AOR = 0.043, 95%CI: 0.026, 0.071) times lower as compared to mothers who did not receive TT injection during pregnancy. Families with five or more members were 1.623 times (AOR = 1.623; 95% CI: 1.193, 2.206) more likely to lose an infant than families with four or fewer members. The risk of infant death was reduced by 67.1% (AOR = 0.329; 95%CI: 0.260, 0.418) in mothers who breastfed compared to mothers who did not breastfeed (Table 2).
Community level factor
Infants living in Afar (AOR = 2.564: 95%CI: 1.466, 4.487), Amhara (AOR = 3.326; 95%CI: 2.064, 5.361), Oromia(AOR = 12.070; 95% CI: 7.584, 19.21), Somali(AOR = 4.171; 95% CI: 2.501, 6.955), SNNPR (AOR = 4.083; 95%CI: 2.561, 6.509) and Harari (AOR = 7.067; 95%CI: 3.679, 13.575) regional state were more likely die as compared to infants living in Tigray regional state. Infants from households without access to a latrine had 62.1% (AOR = 1.621; 95%CI: 1.201, 2.187) higher odds of death compared with infants from households that had an improved latrine facility. The probability of infant death for women those use unprotected source of water was increased by 40% (AOR = 1.400; 95%CI: 1.087, 1.802) as to women use protected water sources (Table 3).
Random effect (a measure of variation)
In Table 4, the results of the random-effects model are given. There were varying infant mortality rates across clusters (communities). Significant variations in infant mortality at the community level were seen in the results of the null model (Model I). The findings show that 32.93% of intra-class correlations (ICCs) were correlated with infant mortality at the community level. After adding both the individual-level and community-level factors in the model (Model IV), there is a significant variation of infant mortality across communities or clusters. About 87.68% of infant mortality in clusters was explained in the full model. Moreover, the MOR confirmed that infant mortality was attributed to community-level factors. In the null model, the MOR for infant mortality was 3.344; this showed that the difference between communities (clustering) was 3.344 times greater than the reference (MOR = 1). When all variables were included in the model, the unexplained community variation in infant deaths was reduced to an MOR of 2.04. This indicated that when all factors are considered, the effects of clustering are still statistically significant in the full models (Table 4).
Discussion
This study aimed to investigate modifiable risk factors in rural Ethiopia for infant mortality. In addition, it explored the variation of rural infant mortality in the enumeration area that has not been studied so far. From the 2016 EDHS data, 8667 rural infants nested in 443 clusters were included in the analysis. The infant mortality rate in rural Ethiopia in 2016 was 62 deaths per 1000 live births7. This death rate is higher than 54 deaths per 1000 live births in urban Ethiopia7. This may be due to the prevalence in rural settings of weak infrastructure, low-economic classes, and restricted flow of information, where the level of risk is estimated to be high. The random effect model showed that both individual and community-level factors accounted for about 87.68% of the variation observed for infant mortality. This finding was in line with the study conducted in Ethiopia24.
A lower risk of infant death has been associated to having a wealthy household. Previous studies in Ethiopia20, Bangladesh15, rural district in Indonesia28 and Nigeria29 showed that infant mortality was negatively associated with household income. Infants from high-income families would be able to meet basic needs and services including health care, quality of life, water quality, and sanitation25. Compared to short birth intervals, long birth intervals were associated with a lower risk of infant death, and the risk of infant death decreased as the previous birth interval increased. This was supported by the study findings in Bangladesh15, Ethiopia19,20,30 and Tanzania31. The reason behind this could be shorter preceding birth intervals are linked to an increased risk of preterm birth, low birth weight, and IUGR for subsequent births. Furthermore, women had less time to recover from previous births and were less able to provide sustenance for their children, potentially increasing the risk of infant mortality.
The study result showed that; the odds of infant death among mothers who received TT injections during pregnancy was lower as compared to mothers who did not receive TT injection during pregnancy This finding was in agreement with a study done in Ethiopia11,17,25 and rural district in Indonesia28 . This could be due to the fact that TT injection produces protective antibodies against infant tetanus11.
The women’s education level was an important socio-economic predictor of infant death. Educated mothers had lower infant mortality than uneducated mothers. This is similar to studies done in Bangladesh15, Ethiopia19,32, Nigeria29,33 and Brazilian34, which found the infant death rate decreased with an increase in the level of education of the mother. Educated mothers are more likely to be conscious of nutrition, use of contraceptives to space births, and awareness of childhood diseases and care.
This study found that ANC visit was a significant predictor of infant mortality. Women who did not have an ANC visit during pregnancy had a greater risk of infant death than those who did. This finding is consistent with the study conducted in Ethiopia11, rural district in Indonesia28, Nepal35 and Pakistan36. This could be because antenatal care visits provide health benefits such as iron, folic acid, and tetanus vaccines, which may reduce the risk of infant mortality. Furthermore, ANC provides mothers and newborns with the opportunity to undergo various interventions like as anti-D, childhood vaccines, and nutritional supplementation37.
Infant mortality was positively associated with multiple births among infants. The odds of infant death among multiple births were higher as compared to singletons. This finding is in agreement with a study from Ethiopia19,20,24 showed that the risk of infant deaths due to multiple births is very high. Infants born at the health center were at lower risk than infants born at home. Multiple births are regarded to put a strain on a family's finances, affecting the infant's nutrition and health care. Multiple births have been related to a higher rate of negative prenatal outcomes, such as premature birth and low birth weight.
Place of delivery was a significant predictor of infant mortality. Infants born health facilities had a lower risk of death when compared to those born at home. This finding was in agreement with a study done in Ethiopia4 rural district in Indonesia28and Nigeria29. This outcome could be explained by the fact that the place of delivery is required to promote the health of women and fetuses by lowering birth complications.
Child vaccination was significantly correlated with infant mortality. Non-vaccinated infant had a greater risk of death than those who had been vaccinated. It is supported by other findings in Ethiopia17,38. The possible reason could be that vaccines can prevent infectious diseases that once killed or harmed many infants. Breastfeeding was found to be significantly associated with infant death. Currently breastfeeding infants have fewer chances of dying with infants than non-breastfed infants. This is also consistent with previous research conducted in Ethiopia17,20 and Nepal39. This may be because breastfeeding may protect babies from infectious diseases since the fluids from the breast are high in antibodies and white cells.
The results of this study also indicated that infant deaths are significantly impacted by family size. The likelihood of infant death increased significantly as family size increased. Similar findings were also found in Ethiopia20. The potential explanation for this may be that there are too many siblings residing at home, which may result in baby care that is insufficient and inappropriate. The study also revealed that number of living children in the household is an important variable affecting infant mortality. As the number of living children in the household increased the risk of infant mortality increased significantly. A study from Ethiopia17, Bangladesh15 and rural district in Indonesia28 consistently reported that infant mortality increase with increase in the number of living children.
Separated women had a higher risk of infant mortality than married women. This finding is in agreement with a study from Rwanda40 and United States41 .This could be due to socioeconomic issues, cultural norms, and the lifestyle consequences of single women. Similarly, infants born with a small birth size had a higher risk of infant mortality than infants born with a large birth size. This result is in line with the previous findings in Ethiopia19,20, Bangladesh14,42 and Indonesia43. Poor nutritional status may have an impact on size at birth, which may have an impact on the risk of newborn mortality19.
The studies also revealed that infant mortality was influenced by geographic location. Infants born in the regional states of Afar, Amhara, Oromia, Somalia, SNNPR, Benishangul-gumz, Gambela, Dire Dawa, and Harari were more likely to die than those born in Tigray. It is supported by other findings in Ethiopia24, Bangladesh13 and Nigeria29,33. The potential explanation for this may be the regional disparities in socioeconomic status, health-care coverage, and other amenities.
Women who drank from an unimproved source had a greater risk of infant death than women who drank from a safe and protected source. This finding is in line with studies done in Bangladesh15, Pakistan44 and Nigeria45. This could be because protected sources of drinking water are less likely to be polluted and less likely to prevent the spread of water-borne diseases like infections and cholera. Infants born into families without access to a latrine died at a higher rate than those born into families with superior latrine facilities. It is supported by other findings in Pakistan44 and Nigeria45 . This may be because access to modern sanitation facilities such as flush toilets is reducing diarrhea prevalence and ultimately decreasing the infant deaths23.
Strengths and limitation
EDHS are a national representative household survey with a high response rate and the findings are generalized to the national populations. The study focused on national survey data that provides policy makers and program managers insight into the implementation of effective intervention strategies both at national as well regional level. In addition, this study applied multilevel modeling to accommodate the EDHS data hierarchical nature. Because of the cross-sectional nature of the data, it is difficult to measure the causal effect and it is not possible to know if the data depends on time or not.
Conclusion
Infant mortality in rural Ethiopia is higher than the national average. This study has demonstrated the importance of both individual and community level factors in explaining enumeration area variations in infant death. This study indicated that antenatal visit, preceding birth interval, number of TT injections, education level of the mother, family size, vaccination of child, contraceptive use, child twin, place of delivery, diarrhea status, size of child at birth, marital status, number of living children, breastfeeding, region, water source, and latrine facility type were found to have a statistically significant association with infant death. The findings suggest that the government and other stakeholders should mainly focus on multiple births, unimproved breastfeeding culture, and the spacing between the orders of birth to reduce infant mortality. Community-based outreach activities and public health interventions focused on improving the latrine facility and source of drinking water as well as the importance of health facility delivery and received TT injections during the pregnancy. The findings of this study may provide a national perspective on the factors that contribute to infant mortality in rural Ethiopia. Finally, we advised policymakers and governments to prioritize community-level factors over individual factors in order to meet the SDG goals and targets by the end of 2030.
Data availability
This study used EDHS 2016 child data set and extracted the outcome and explanatory variables. Data is publicly available online from (https://dhsprogram.com/Data/). Correspondence and requests for data and materials should be addressed to S.M.
Abbreviations
- AIC:
-
Akaike’s information criterion
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence intervals
- CSA:
-
Central Statistical Agency
- DIC:
-
Deviance information criterion
- EAs:
-
Enumeration areas
- EDHS:
-
Ethiopian demographic and health survey
- ICC:
-
Intra-cluster correlation
- MOR:
-
Median odds ratio
- PCV:
-
Proportional change in variance
- SNNPR:
-
Southern Nations, Nationalities, and People Region
- TT:
-
Tetanus Toxoid
- WHO:
-
World Health Organization
References
Estimation, U.N.I.G.f.C.M., Levels & trends in child mortality: report 2017: estimates developed by the UN Inter-Agency Group for Child Mortality Estimation. 2017: United Nations Children's Fund.
Estimation, U.N.I.-a.G.f.C.M., et al., Levels & Trends in Child Mortality: Report 2018, Estimates Developed by the. 2018: United Nations Children's Fund.
Organization, W.H., World health statistics overview 2019: monitoring health for the SDGs, sustainable development goals. 2019, World Health Organization.
Fenta, S. M., Fenta, H. M. & Ayenew, G. M. The best statistical model to estimate predictors of under-five mortality in Ethiopia. J. Big Data 7(1), 1–14 (2020).
IGME, U., Levels & Trends in Child Mortality: Report,. Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation 2017 (United Nations Children’s Fund, 2017).
Zimmerman, L. A. et al. Evaluating consistency of recall of maternal and newborn care complications and intervention coverage using PMA panel data in SNNPR, Ethiopia. PLoS ONE 14(5), e0216612 (2019).
EDHS, Central Statistical Agency: Ethiopia Demographic and Health Survey https://dhsprogram.com/publications/publication-fr328-dhs-final-reports.cfm. 2016.
Ruducha, J. et al. How Ethiopia achieved millennium development goal 4 through multisectoral interventions: a countdown to 2015 case study. Lancet Glob. Health 5(11), e1142–e1151 (2017).
Gebresilassie, Y., Nyatanga, P. & Gebreselassie, M. Determinants of rural–urban differentials in under-five child mortality in ethiopia. Eur. J. Dev. Res. 33(3), 710–734 (2021).
Yalew, M. et al. Time to under-five mortality and its predictors in rural Ethiopia: Cox-gamma shared frailty model. PLoS ONE 17(4), e0266595 (2022).
Fenta, S. M. & Fenta, H. M. Risk factors of child mortality in Ethiopia: application of multilevel two-part model. PLoS ONE 15(8), e0237640 (2020).
Naz, L. and K.K. Patel, Determinants of infant mortality in Sierra Leone: applying Cox proportional hazards model. Int. J. Soc. Econ. (2020).
Nilima, S., Sultana, R. & Ireen, S. Neonatal, infant and under-five mortality: An application of cox proportional Hazard model to BDHS data. J. Asiat. Soc. Bangladesh, Sci. 44(1), 7–14 (2018).
Vijay, J. & Patel, K. K. Risk factors of infant mortality in Bangladesh. Clin. Epidemiol. Glob. Health 8(1), 211–214 (2020).
Rahman, A., et al. Machine Learning Algorithm for Analysing Infant Mortality in Bangladesh. In International Conference on Health Information Science. 2021. Springer.
Baraki, A. G. et al. Factors affecting infant mortality in the general population: Evidence from the 2016 Ethiopian demographic and health survey (EDHS); a multilevel analysis. BMC Pregnancy Childbirth 20(1), 1–8 (2020).
Fentaw, K. D. et al. Factors associated with post-neonatal mortality in Ethiopia: Using the 2019 Ethiopia mini demographic and health survey. PLoS ONE 17(7), e0272016 (2022).
Aalemi, A. K., Shahpar, K. & Mubarak, M. Y. Factors influencing vaccination coverage among children age 12–23 months in Afghanistan: Analysis of the 2015 demographic and health survey. PLoS ONE 15(8), e0236955 (2020).
Abate, M. G., Angaw, D. A. & Shaweno, T. Proximate determinants of infant mortality in Ethiopia, 2016 Ethiopian demographic and health surveys: results from a survival analysis. Arch. Public Health 78(1), 1–10 (2020).
Mulugeta, S. S. et al. Multilevel log linear model to estimate the risk factors associated with infant mortality in Ethiopia: Further analysis of 2016 EDHS. BMC Pregnancy Childbirth 22(1), 1–11 (2022).
Eyeberu, A. et al. Neonatal mortality among neonates admitted to NICU of Hiwot Fana specialized university hospital, eastern Ethiopia, 2020: a cross-sectional study design. BMC Pediatr. 21(1), 1–9 (2021).
Hadgu, F. B. et al. Prevalence and factors associated with neonatal mortality at ayder comprehensive specialized hospital, Northern Ethiopia: A cross-sectional study. Pediatric health, med. therapeutics 11, 29 (2020).
Fenta, S. M., Biresaw, H. B. & Fentaw, K. D. Risk factor of neonatal mortality in Ethiopia: Multilevel analysis of 2016 demographic and health survey. Trop. Med. Health 49(1), 1–11 (2021).
Baraki, A. G. et al. Factors affecting infant mortality in the general population: evidence from the 2016 Ethiopian demographic and health survey (EDHS): A multilevel analysis. BMC Pregnancy Childbirth 20, 1–8 (2020).
Kiross, G. T. et al. Individual-, household-and community-level determinants of infant mortality in Ethiopia. PLoS ONE 16(3), e0248501 (2021).
Tesema, G. A. & Worku, M. G. Individual-and community-level determinants of neonatal mortality in the emerging regions of Ethiopia: A multilevel mixed-effect analysis. BMC Pregnancy Childbirth 21(1), 1–11 (2021).
Austin, P. C. et al. Measures of clustering and heterogeneity in multilevel P oisson regression analyses of rates/count data. Stat. Med. 37(4), 572–589 (2018).
Rahayu, S. & Muhaimin, T. inadequate antenatal care visits and risks of infant mortality in rural district. Media Publ. Promosi Kesehat. Indones. (MPPKI) 5(7), 819–823 (2022).
Kunnuji, M. et al. Background predictors of time to death in infancy: evidence from a survival analysis of the 2018 Nigeria DHS data. BMC Public Health 22(1), 1–8 (2022).
Tesema, G. A. et al. Trends of infant mortality and its determinants in Ethiopia: mixed-effect binary logistic regression and multivariate decomposition analysis. BMC Pregnancy Childbirth 21(1), 1–16 (2021).
Ogbo, F. A. et al. Determinants of trends in neonatal, post-neonatal, infant, child and under-five mortalities in Tanzania from 2004 to 2016. BMC Public Health 19(1), 1–12 (2019).
Kiross, G. T. et al. The effect of maternal education on infant mortality in Ethiopia: A systematic review and meta-analysis. PLoS ONE 14(7), e0220076 (2019).
Yaya, S. et al. Prevalence and determinants of childhood mortality in Nigeria. BMC Public Health 17(1), 1–7 (2017).
Anele, C. R. et al. The influence of the municipal human development index and maternal education on infant mortality: An investigation in a retrospective cohort study in the extreme south of Brazil. BMC Public Health 21(1), 1–12 (2021).
Lamichhane, R. et al. Factors associated with infant mortality in Nepal: A comparative analysis of Nepal demographic and health surveys (NDHS) 2006 and 2011. BMC Public Health 17(1), 1–18 (2017).
Patel, K. K., Rai, R. & Rai, A. K. Determinants of infant mortality in Pakistan: Evidence from Pakistan demographic and health survey 2017–18. J. Public Health 29(3), 693–701 (2021).
Antehunegn, G. & Worku, M. G. Individual-and community-level determinants of neonatal mortality in the emerging regions of Ethiopia: A multilevel mixed-effect analysis. BMC Pregnancy Childbirth 21(1), 1–11 (2021).
Gebremichael, S.G. and S.M. Fenta, Factors associated with U5M in the afar region of Ethiopia. Adv. Public Health (2020).
Lamichhane, R. et al. Factors associated with infant mortality in Nepal: A comparative analysis of Nepal demographic and health surveys (NDHS) 2006 and 2011. BMC Public Health 17(1), 53 (2017).
Mfateneza, E. et al. Application of machine learning methods for predicting infant mortality in Rwanda: Analysis of rwanda demographic health survey 2014–15 dataset. BMC Pregnancy Childbirth 22(1), 1–13 (2022).
Orischak, M. et al. Social determinants of infant mortality amongst births to non-hispanic black women. Am. J. Obstet. Gynecol. 226(1), S706 (2022).
Razzaque, A. et al. Levels, trends and socio-demographic determinants of infant and under-five mortalities in and around slum areas of Dhaka city Bangladesh. SSM-popul. health 17, 101033 (2022).
Wardani, Y., Huang, Y.-L. & Chuang, Y.-C. Factors associated with infant deaths in Indonesia: An analysis of the 2012 and 2017 Indonesia demographic and health surveys. J. Trop. Pediatr. 68(5), p.fmac065 (2022).
Asif, M. F. et al. Socio-economic determinants of child mortality in Pakistan and the moderating role of household’s wealth index. BMC Pediatr. 22(1), 1–8 (2022).
Eke, D. O. & Ewere, F. Levels, trends and determinants of infant mortality in Nigeria: An analysis using the logistic regression model. Earthline J. Math. Sci. 8(1), 17–40 (2022).
Acknowledgements
The authors acknowledge the ICF international for granting access to use the 2016 EDHS data set for this study.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
S.M. had substantial contributions to the conception and design of this research, involved in the analysis and interpretation of data, and drafted the article. G.M., H.M., H.B. and K.D. designed the study and revised the article. All authors read and approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fenta, S.M., Ayenew, G.M., Fenta, H.M. et al. Community and individual level determinants of infant mortality in rural Ethiopia using data from 2016 Ethiopian demographic and health survey. Sci Rep 12, 16879 (2022). https://doi.org/10.1038/s41598-022-21438-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21438-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.