Abstract
The high global bacterial infection burden has created need to investigate the neglected potential drivers of pathogenic bacteria, to inform disease prevention. Kampala is facing a proliferation of herbalists, selling herbal medicine (HM), of largely unregulated microbiological quality. We evaluated the bacterial contamination burden in HM sold in Kampala, to support evidence-based redress. The total viable loads (TVL), total coliform counts (TCC), E. coli counts, and prevalence of selected bacterial strains in 140 HM were examined using conventional culture, following the guidelines of World Health Organization (WHO), and Uganda National Drug Authority (NDA). Data were analyzed using D'Agostino-Pearson test, frequencies, proportions, Chi-square, and Mann–Whitney U test with STATA version-15.0. Fifty (35.7%), fifty-nine (42.1%), and twelve (8.6%) HM were unsafe for human use because they exceeded WHO’s permissible limits for TVL, TCC, and E. coli counts respectively. Solids had significantly higher mean TVL than liquids. Violation of NDA’s guidelines was significantly associated with high TVL. Fifty-nine bacteria, viz., Klebsiella pneumoniae (n = 34; 57.6%), Escherichia. coli (12; 20.3%), Staphylococcus aureus (7; 11.9%), Klebsiella oxytoca (3; 5.1%), Bacillus cereus, Pseudomonas aeruginosa, and Enterobacter spp. (1; 1.7% each), were isolated from 45 (32.1%) samples. These bacteria can cause severe clinical diseases, and promote deterioration of HM potency.
Similar content being viewed by others
Introduction
Infectious diseases are among the major causes of death and hospitalization worldwide, and those caused by bacteria are more common in some parts of Africa including Uganda1. In Eastern Africa, the burden incurred by bacterial pathogens manifests more in form of diarrheal and/or respiratory diseases. For example, in Uganda and Tanzania, diarrheal and respiratory ailments of bacterial origin are ranked among the six major causes of both adult and childhood mortality2. Since the leading factors in escalating these infections may vary from one setting to another3, the establishment of community- or area specific research and/or other interventions is necessary for effective thwarting of the burden. In Uganda, like some other parts of the world, the interventions aimed at counteracting infectious disease spread are somewhat inclined towards the human-to-human and/or human-to-animal linkages4. Though neglected to some extent, the potential role some plant resources may play in the community spread of bacterial pathogens could be substantial. Such plant materials are not only limited to food but also herbal medicines (HM)1,5,6,7.
In Uganda, like most other parts of the world, HM trade has been increasing in a few past decades8. Of recent, the ratio of traditional medical practitioners (TMP) to the general population in Uganda was reported to be between 1:200 and 1:400, contrasting greatly with the ratio of formal health personnel to the general population which was ≤ 1:20,000 (WHO9,10). The herbalists also offer consultation services, and/or sell HM for managing common ailments. The evolution of microbial resistance to conventional drugs, and the affordability and accessibility of HM have been reported as some of the key factors promoting the ongoing increase in herbal medicine use, especially in the developing world9,10. Kampala being Uganda’s major capital and commercial center, has a greater number of herbal medicine business ventures compared to other cities in the country5. This could partly be attributed to the high demand, and the lucrative market offered by the large population of residents, travelers, and the business community in the city11. The resident population in Kampala city mostly comprises of low-income earners that live in the suburbs, and have high inclination to HM use5,12,13,14.
In the recent past, the population in Kampala city has been experiencing persistent outbreaks of bacterial diseases such as typhoid fever and E. coli infection among others15,16. In this city, HM are widely popularized by the herbalists as being absolutely safe for human use. However, the microbiological quality of these HM is not routinely monitored. Besides, adverse effects of HM have been reported to be potentially linked to bacterial contamination in some parts of the world1,6,7. Such bacteria may include Streptococcus pneumoniae, Salmonella spp., Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus, and Klebsiella pneumoniae, among others7,17. Several strains belonging to some of the species which may contaminate HM, such as E. coli, Salmonella spp., and Streptococcus pneumoniae have been implicated in severe diarrheal and/or respiratory diseases1. Further, some bacterial species, particularly members of the family Enterobacteriaceae (the coliforms), like E. coli have been specified by the World Health Organization (WHO), as indicators of fecal contamination18. Therefore, the existence of E. coli in HM does not only indicate gross violation of hygiene standards, but also the potential presence of other, more virulent, enteric pathogens such as Salmonella spp. and Shigella spp. among others5,19. Information about the degree of bacterial loading, and the profiles of bacteria that inhabit HM in particular settings is essential in improving the mitigation strategies.
The aim of this study therefore, was to isolate and characterize selected bacteria that could be associated with diarrhea and/or respiratory infections such as Salmonella spp., Shigella, B. cereus, K. pneumoniae, S. aureus and E. coli from commercial HM sold in Kampala city. The overall degree of bacterial contamination was also assessed by using standard microbiological parameters such as the Total Coliform Counts (TCC), Total Viable Counts (TVL), and E. coli counts. The findings could contribute to the attainment of evidence-informed public health policy and practice.
Results
Socio-demographic profile of participants
Majority (n = 36, 55.4%) of the respondents were men, hence females were 44.6% (n = 29). Most of the participants were in the youthful age category (n = 24, 36.9%), followed by the middle aged (n = 39, 60%), while only two (3.1%) were elderly. Most of the participants (n = 26, 40.0%) had attended secondary education, while very few (3, 4.6%) had attained tertiary education. The majority of the respondents had practiced commercial traditional medicine for a duration of 5–15 years, and these constituted 72.3% (n = 47). Most participants (39, 60.0%), earned a net monthly profit of UGX 730,000 ($ 200) ≤ 1,460,000 ($ 400), while the minority (5, 7.7%) earned above UGX 1,825,000 ($ 500) from HM sales (Table 1).
Characteristics of the herbal medicines from which bacterial contaminants were isolated
Out of the 140 herbal medicine (HM) samples, 114 were liquids while 26 were solids. In addition, two conventional antibiotic drugs were included as controls. The HM samples were availed on market in different packaging materials namely; bottles (116; 82.6%), polyethene (12; 8.6%), Tins (6; 4.3%), papers (5; 3.6%), and bare (unwrapped) (1; 0.9%). Figure 1 below shows some of the samples that were investigated in this research. Most of the HM (87; 62.1%), were packaged in original material (without evidence of package recycling), the re-used packages were (53; 37.83%), while the bare/unwrapped was (1, 0.07%). One hundred and one (101, 72.1%) samples were visibly clean, while 39 (27.9%) appeared dusty. Though most (77, 55.0%) samples satisfied at least (4 of the10) conditions enshrined in herbal medicine packaging and branding guidelines provided by Uganda National Drug Authority (NDA)20, 63 samples (63, 45.0%) were in absolute disconformity (did not satisfy any of the 10 conditions), while none of the samples (0, 0%) conformed to all the 10 conditions. The ailments suggested to be treated by these HM belonged to 12 disease categories; gastro-intestinal tract infections being the largest category (constituting 14 diseases), followed by respiratory infections (10 diseases), and urinogenital and reproductive disorders (8 diseases); the smallest categories were the metabolic disorders and bone diseases with one ailment each (Table 2).
Total viable loads (TVL) of bacteria isolated from selected herbal medicines sold in Kampala City
Out of the 140 samples screened, 50 (35.7%) possessed total viable loads (TVL) of bacteria that exceeded the maximum acceptable levels (105 CFU/ml for liquids and 107 CFU/g for solids), that are recommended by the World Health Organization (WHO)18,19. However, the samples that exceeded permissible limits were significantly fewer than those that passed (χ2, p = 0.0012). Though most (15 out of 50), samples which did not conform to the WHO standards were found in Rubaga, a Chi-square test revealed that such HM did not significantly differ from those traded in the other divisions of the city (p ≤ 0.05) (Fig. 2).
Conformity of the herbal medicines sold in Kampala to the permissible bacterial Total Viable Loads (TVL), that are recommended by World Health Organization (WHO)18. The p values show the significancy of differences in the proportions of samples that possessed unacceptable TVL.
The mean TVL from all the 140 samples (solids and liquids) was 126.407 × 104 CFU/ml or g, and it exceeded the WHO’s permissible levels. The mean TVL values were (286.334, 125.919, 77.351, 52.789, and 35.821) × 104 CFU/ml or g for Rubaga, Kampala central, Nakawa, Makindye, and Kawempe divisions, respectively. There were no significant variations in the mean TVL of the five divisions, as well as the overall mean, except for Nakawa and Makindye (Mann–Whitney U; Z = 2.467, p = 0.0136) (Fig. 3).
For the liquid HM, the lowest TVL was 0.000 × 104 CFU/ml (recorded in 14 samples), while the highest was 1420.000 × 104 CFU/ml. For the solid HM, the highest was TVL was 1670.000 × 104 CFU/g and the least was 0.180 × 104 CFU/g. (Table 3). Overall, the highest TVL was 1670.000 × 104 CFU/g (observed in one solid sample), while the lowest was 0.000 × 104 CFU/ml (recorded in 14 liquid samples). Consequently, the mean TVL of the solid samples (215.660 × 104 CFU/g) was significantly higher than that (106.051 × 104 CFU/ml) in liquids (Mann–Whitney U; Z = − 2.136, p = 0.0326). Similarly, the mean TVL was significantly higher in solids than liquids in Makindye (Z = − 2.135, p = 0.0327). On the contrary, the mean TVL was significantly higher in liquids than the solid samples in Rubaga division (Z = − 2.673, p = 0.0075), while there was no significant variation in the mean TVL of solids and liquids in Kawempe, Kampala central, and Nakawa divisions (Table 3).
The samples that were sold in recycled packaging materials possessed significantly higher mean TVL than those packed in nonrecycled packages except in Kawempe (Z = 0.343, p = 0.7313), and Rubaga divisions (Z = 0.1267, p = 0.1267). Both the Mann–Whitney U test and the t-test revealed no significant differences in the mean TVL values among the types of establishments where they were procured (market stalls, herbal shops, roadside and/or mobile stalls) (p < 0.05). The herbal medicines that scored ≤ 5 out of 10 (≤ 50%) in regard to conformity to NDA’s herbal medicine packaging and labeling guidelines possessed significantly higher TVL than those with > 50% (Table 3). Herbal medicines sold at the lower prices (UGX 1000 ≤ 5000) contained greater mean TVL compared to those with high prices (> UGX 5000) but the differences were not significant (Table 3).
Total coliform counts (TCC), and E. coli counts
Fifty nine samples (42.1%) harbored total coliform counts that exceeded the World Health Organization’s maximum permissible limit of ≤ 103 CFU/ml or g18,19. Although the majority if these unsuitable samples originated from Kampala central division (n = 17), the proportions were not significantly different from those procured from the rest of the city divisions, as well as the overall TCC (χ2, p < 0.05) (Table 4). The mean TCC was 35.5651 × 104 CFU/ml or g (95% CI = 18.7993 × 104 to 52.3308 × 104 CFU/ml or g), while the range was 624.0000 × 104 CFU/ml or g. The maximum TCC was 624.0000 × 104 CFU/ml. The minimum value was 0.0000 × 104 CFU/ml or g, observed in 64 (45.7%), samples (5 solids and 59 solids). Twelve (8.6%) out of all the sample (N = 140), possessed E. coli counts which exceeded the World Health Organization’s maximum permissible limit of ≤ 10 CFU/ml or g18,19. Rubaga and Kawempe harbored the greatest number of samples with unacceptable loads of E. coli and these were not significantly different from the other divisions of the city except Rubaga (χ2, p < 0.05), which did not exhibit any positive growth of E. coli (Table 4).
Prevalence of K. pneumoniae, E. coli, S. aureus, P. aeruginosa, K. oxytoca, Enterobacter spp., Bacillus cereus, Salmonella spp., and Shigella spp. in selected herbal medicines sold in Kampala city
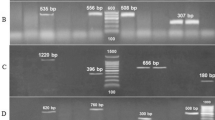
Representative cultures for some of the bacteria that grew are shown in Fig. 4. Pseudomonas aeruginosa, on Kings’ agar, demonstrated small to medium sized, spindle/irregularly shaped, flat, greenish colonies. Staphylococcus aureus on MSA manifested as small, round, raised, smooth, yellow colonies (Fig. 4). On BCA media, Bacillus cereus showed medium to large sized, bluish (peacock blue), flat colonies with serrated margins. E. coli on VRBA demonstrated hot pink, dry, flat/umbonate colonies, while Enterobacter spp. showed mucoid pink to pinkish red colonies, and Klebsiella spp., mucoid, golden- or dull-yellow colonies. K. pneumoniae presented as mucoid pink colonies on MacConkey agar (Fig. 4). On XLD agar, the characteristic slightly rough/dimpled, red colonies with or without black centers were absent for all the samples, indicating the absence of Salmonella spp. or Shigella spp. respectively.
Schematic diagram for isolation of selected bacteria from herbal medicines sold in Kampala city. (a) The panel of bacterial culture media used, (b) culture media weighed (according to the manufacturer’s instructions) using an electric balance and (c), dispensed in conical flasks, then (d), dissolved in distilled water followed by autoclaving (e). (f) Media casted in petri dishes, and (f) incubated at 37 °C for 24 h (quality control). (h) Media plates that passed the quality test. (i) Representative herbal medicine (HM) samples. 1: Inoculation of culture plates with serially diluted HM samples. 2: Incubation of the inoculated culture plates, and 3: Appearance of pure colonies of bacteria on some different media, viz; E. coli (hot pink colonies on VRBA), B. cereus (bluish colonies on B. cereus agar), S. aureus (yellow and golden yellow colonies on Mannitol Salt Agar), K. pneumoniae (Mucoid pink colonies on MacConkey agar).
The bacteria that grew were further characterized basing on their gram-staining properties and biochemical traits, under the guidance of the Bergey’s Manual of Systematic Bacteriology21 (Fig. 5, Table 5).
Representative plates for the biochemical phenotypes observed during characterization of bacteria isolated from commercial herbal medicines in Kampala city. (a) Panel for K. pneumoniae: 1: TSI(A/A), 2: urease (positive reaction)., 3: citrate utilization test (positive reaction), 4: peptone water for Indole (negative reaction), 5: methyl red test (negative reaction). (b) Panel for E. coli: TSI(A/A), 2: urease (negative reaction), 3: citrate utilization test (negative reaction), 4: peptone water for Indole (positive reaction), 5: methyl red test (positive reaction).
Bacterial species isolated from selected herbal medicines sold in Kampala city
A total of 59 bacterial strains were recovered from 45 (32.1%), of the 140 HM samples screened. The majority were K. pneumoniae (34; 57.6%), followed by E. coli (12; 20.3%), while the minority were Salmonella spp. (0; 0.0%) and Shigella spp. (0; 0.0%) (Table 6). The microbes were isolated from 35 out of 115 liquid samples (30.4%), with the exception of 11 isolates, viz; K. pneumoniae (5; 8.5%), E. coli (3; 5.1%), S. aureus (2; 3.4%), and K. oxytoca (1; 1.7%), which were got from 10 (40.0%), out of the 25 solids screened.
Discussion
Socio-demographic profiles of participants
The majority of the participants recruited in this study were men. The predominance of men in HM trade was reported earlier in some parts South Africa22, Tanzania23, and Malawi24. However, in some provinces of South Africa such as KwaZulu-Natal, and Mpumalanga25, the majority of commercial herbalists were reported to be women, and this aligned with findings of most studies that were conducted in the rural herbalist communities in several parts of Uganda26,27,28,29. Though men’s predominance as commercial herbalists in urban settings, as opposed to the rural areas, has been well documented, the factors that underpin this gender disproportion remain largely unexplained. Partly, this gender disparity may be attributed to societal norms28, and also to the fact that females are commonly responsible for their families’ primary health care. Hence treating people becomes a responsibility of mainly the female gender most evidently in the rural settings28.
Our observation, that over 90% of the participants in the current study had attained a certain level of formal education is of great significance, since basic education is believed to be a critical component of the health30. The high profits gained from HM sales, as observed in this study, highlight the potential role herbal medicines play towards Uganda’s national economy, as well as supporting the attainment of community livelihood needs, primary health care, and cultural heritage. Consequently, medicinal plants have been acknowledged as an important feature of the cultural, economic, medicinal, and ecological components of all cities in the world31.
Characteristics of the herbal medicines from which bacterial contaminants were isolated
Both the solid and liquid HM were included in this study and were procured from herbal shops, market stalls, as well as roadside and/or mobile stalls. Likewise, such types of commercial HM establishments were reported in urban settings in other parts of Africa and beyond6,32,33,34,35. The abundant presence of roadside and/or mobile commercial herbal medicines might pose herbal quality challenges since adequate regulation and monitoring of such establishments can be complicated36. Also, our observation that some HM were placed in recycled packaging materials (previously discarded as wastes) points to further potential threats to herbal safety since the re-use of these packages has been linked to the introduction of pathogenic microbial contaminants into the drugs elsewhere33,34,36,37. Even though the proportion of HM that absolutely violated the Uganda National Drug Authority (NDA)’s herbal packaging and labeling guidelines was generally high, it demonstrated a twofold decrease in the percentage that was reported in Makindye division of Kampala over a decade ago5. The NDA-guidelines provide for ten conditions that should be fulfilled to attain the desired herbal packaging and labelling standards, viz; (1) tight packaging (absence of leakage), (2) presence of a brand name, (3) active ingredients (contents), (4) indications (diseases/therapeutic claims), and contraindications (warnings and precautions), (5) name of manufacturer, (6) full address of manufacturer with physical location, (7) batch number, (8) date of manufacture and expiry, (9) dosage (for adults and children), and (10) directions for use and storage38. The factors that could explain this improvement in conformity of the HM sold in Kampala to the NDA-guidelines remain unclear. However, it might potentially be partly attributed to the rising competition which has stimulated innovations not only in the marketing/advertisement but also improvement in packaging and branding, nearly comparable to the standards that are acceptable in pharmacies39. Nonetheless, some hinderances to the standard labelling of herbal medicines have been reported in some parts of the world; for example, most herbalists decline to specify the active ingredients/contents present in their herbal products because they wish to keep their traditional medicinal knowledge confidential5,40. Unfortunately, this may lead to in adverse drug reactions if members of the community use HM having ingredients to which they are allergic.
Much as our inclusion criteria sought a random sample of 140 herbal medicines used for cough, diabetes, Ulcers, and/or diarrhea treatment, the same remedies were found to be used in the management of 62 health complications, including HIV/AIDS, different types of cancers, and reproductive disorders among others. On average therefore, each remedy was suggested to treat over 15 ailments. Though the “one drug for many diseases” approach may not only reduce the cost of treatment of multiple infections41, it can also increase the number of individuals (suffering from different ailments) who may consume the same drug, and hence get exposed to its associated risks such as pathogenic microbial contaminants.
Total viable loads (TVL) of bacteria isolated from selected herbal medicines sold in Kampala City
According to the quality control guidelines set by World Health Organization, herbal medicines with total viable loads of bacteria that exceed the maximum permissible limits (105 CFU/ml for liquids and 107 CFU/g for solids) should be considered unsuitable for human consumption and hence rejected18,19. The guidelines provided by other establishments such as the European pharmacopeia generally align with the standards set by the WHO42,43. In the current study, 35.7% of the HM possessed bacterial TVL that exceeded the maximum acceptable levels in reference to the WHO standards18,19. Even though most of these unsuitable samples were found in Rubaga division, the mounts did not significantly differ from those found in the other parts of the city (χ2, p < 0.05). The proportion of HM which exceeded the permissible TVL of bacteria in Kampala that were revealed in this study is over threefold higher than that (11.7%), reported by another study in 20095. The difference might partly be explained by the fact that the latter5, was less comprehensive since the sampling was limited to liquid HM for cough in Makindye division alone. Other few previous studies that assessed the bacterial contamination of herbal medicines in Kampala did not examine this parameter (the total viable loads of bacteria)14,44,45.
Our findings revealed that HM with ≤ 50% level of conformity to Uganda National Drug Authority’s packaging and labeling guidelines contained significantly higher TVL values than those with > 50%, and that there were no significant differences in the contamination levels between the highly priced and the low-cost HM. This implies that irrespective of the price, some of the commercial HM in Kampala may disseminate viable bacteria in the community, but conformity to the Uganda National Drug Authority guidelines can play a considerable role in resolving this burden. Most bacteria have the potential not only to impair human health but also spoil and reduce the potency of the herbal medicines they contaminate46.
Total Coliform Counts (TCC), and E. coli counts
In the present study, the proportion of HM (42.1%), which were found to exceed the permissible level of total coliform counts was high give the perceived public health importance of most coliform bacteria5,46,47. The term “total coliforms” represents a group of non-spore-forming, gram-negative, facultatively anaerobic, bacillus bacteria that strongly ferment lactose to acid and gas following 42–48 h incubation at 35 ± 2 °C48. They mainly belong to two groups. The 1st group includes bacteria that often form part of the natural flora of most vegetation, such as some strains of Enterobacter spp., Serratia spp., and Erwinia spp. among others. The bacteria belonging to this group do not have any historicaly linkages to feces and are commonly prevalent in environmental reservoirs such as water and soil. The presence of these strains in consumable products like HM may not necessarily infer fecal contamination, hence they do not necessarily indicate a substantial public health threat49. The 2nd group constitutes thermotolerant (fecal) coliforms, which are commonly found in the intestines of man and other warm-blooded animals48. These include some strains of Escherichia spp, Klebsiella spp, and Citrobacter spp. among others. The strains belonging to this group largely constitute the intestinal flora of man and other warm-blooded animals, hence they signify potential contamination by fecal matter and its associated human pathogens, threatening public health16. Escherichia coli is believed to be one of commonest flora that inhabit the intestinal tract of vertebrates50. Therefore, the presence of this coliform is widely used as a reliable basis to infer the degree of fecal contamination.
In the current study, over eight in very one hundred herbal medicines were found to possess higher loads of E. coli than the permissible level (10 CFU/ml or g), as per the guidelines of WHO18. From the public health point of view, over 8% of the samples screened in the current study were therefore unsafe for human use on the basis of this parameter. A chi-square test revealed that the overall number of samples with unacceptable total coliform counts were significantly higher than those harboring undesirable E. coli loads (p = 0.0291). Consequently, it was surprising to note that Rubaga division did not possess any samples with unacceptable levels of E. coli even though over 35% harbored high total coliform counts. These observations demonstrate the potential role other coliform bacteria (most likely nonfecal coliforms that are commonly prevalent on plants, and in environmental resources like soil and water), play in contaminating herbal remedies, hence the need to observe both the good manufacturing practices as well as the good agricultural practices by the herbalists.
Specific bacterial strains isolated from selected herbal medicines sold in Kampala city
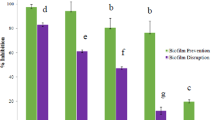
We report a 32.1% proportion of HM that were contaminated with at least one bacterial species of potential medical importance. Since the beginning of the 21st century, the percentages of bacterially contaminated HM in Kampala city have demonstrated an oscillating pattern, with some studies revealing less and others higher values than the 32.1% as well as the 62.1% reported by the current study and the East African regionwide survey respectively (Fig. 6)1,5,14,44. This creates uncertainties about the likely trend which the HM bacterial contamination burden in Kampala might ensue subsequent to the present study.
The failure to attain a stable level of microbiological safety in the herbal medicines sold in Kampala city, and/or some other similar settings (Fig. 4), reflects intervention gaps which could be associated with the policy and/or regulatory environment, hygiene, and sociographic factors of herbalists among others. In the present study, it was outrageous to observe the concurrence of three bacterial strains of potential medical importance in two of the herbal liquids (packed in dusty, re-used mineral water bottles), one for cough and the other for diarrhea treatment. The former was grossly adulterated with P. aeruginosa and the latter harbored S. aureus, while both were positive for E. coli and K. pneumoniae. Such HM might promote the community spread of mixed bacterial infections which can be complicated to treat. It was commendable to note that in this study, many of the primary pathogens such as Salmonella spp. and Shigella spp., some of which have been associated with persistent outbreaks of diarrheal diseases like typhoid fever in Kampala city were absent in all the samples screened15. Nonetheless, the strains that have been revealed by the current study to be highly prevalent in HM in Kampala, particularly K. pneumoniae, E. coli and S. aureus have the potential to impair human health in several ways. For example, S. aureus, and several pathotypes of E. coli are involved in severe diarrhea and/or urinogenital infections16,52,53. Besides, these pathogens are on the global list of critical multi-drug-resistant bacteria which require urgent redress54. Although bacterial contaminants have been reported in some conventional pharmaceutical drugs elsewhere55, the modern drugs included as controls in the present study where safe in reference to all the microbiological parameters examined. This implies that the modern drugs sold in pharmacies in Kampala might be of suitable microbiological quality but this can only be confirmed following a comprehensive investigation.
Conclusions
The prevalence of commercial herbal medicines that are bacterially contaminated in Kampala city remains relatively high. Some strains belonging to the bacterial species involved in this contamination, particularly, E. coli, K. pneumoniae, P. aeruginosa and S. aureus have the potential to cause severe clinical diseases, spoilage of HM, and deterrence of therapeutic potency. Also, these strains have been implicated in the community spread of antibiotic resistance. There is need to conduct further research on bacteria isolated from HM in Uganda, especially to examine their antibiotic resistance traits, to fully elucidate the risk incurred. Quality assurance should be enhanced to promote public health and to harness herbal medicine sector development.
Methods
Study area
The study was conducted in the five administrative divisions of Kampala city, located in the central region of Uganda, stretching over an area between DMS Latitude: 0° 12′ 46.755″ N, Longitude: 32° 30′ 32.567″ E and DMS Latitude: 0° 12′ 20.692″ N, Longitude: 32° 40′ 14.054″ E. It is bordered by Mukono district to the East; Lake Victoria to the South East; and Wakiso district to the West, South, and North (Fig. 7). Its five administrative divisions are; Kampala central, Kawempe, Nakawa, Makindye and Rubaga divisions. According to the recent Uganda national population census, the city is populated by about 1,680,601–2,915,200 residential occupants56, plus large numbers of individuals that enter and leave the city on a daily basis11.
Study design
A cross sectional survey was conducted on 65 traditional herbalists that sell herbal medicines in Kampala, between April and September 2021. Pre-tested, semi-structured questionnaires were used to record the socio-demographic profiles of respondents, and the attributes of herbal medicines which were procured from the participants. Such attributes included, prices, quantity and label information among others. In addition, HM packaging properties, categories of traditional HM outlets, cleanliness, and pharmaceutical forms of the HM were examined through field observations which were supplemented using photography, with a high-resolution digital camera inbuilt in a Phantom-9 Mobile Phone, model AB7/2019, Techno Mobile Limited57. The laboratory experiments were aimed at assessing the Total Viable Loads (TVL), Total Coliform Counts (TCC), as well as the isolation and characterization of selected diarrheal and/or respiratory bacterial pathogens from the herbal medicine samples. The targeted bacterial species were those that had been commonly implicated in disease causation in Kampala city and/or Uganda at large, such as; Salmonella spp., E. coli and K. pneumoniae among others15,16,58.
Study population
The study units of interest in this research were the herbal medicines for diarrhea, cough, diabetes, and high blood pressure, sold by herbalists in herbal shops, market stalls, and roadside/mobile stalls in Kampala city. These herbal medicines were selected because of their perceived high frequency of use, and the likely carriage of bacterial contaminants of mostly unidentified profiles5,14.
Sample size
Due to high number of largely unregulated HM marketed with various therapeutic claims in Kampala, a representative sample (N), was determined using the formula for unknown population size at 95% confidence interval; N = Z21−α [P (1 − P)] ÷ D259.
Where; N = The desired sample size, Z1−α = Standard error of the mean = 1.96 at 95% confidence level, P = Estimated prevalence of bacterial contamination in HM above the WHO permissible levels = 90%14, and D = Tolerable sampling error = 0.05 at 5% significance level.
Hence, sample size = 1.962 [0.9 (1 − 0.9)] ÷ 0.052 = 138.3 ≃ 138.
Therefore, the minimum sample size required was 138. However, since the current study was conducted in five administrative divisions of Kampala, a sample size of 140 herbal medicines was adopted, and was divided into strata (of 28 samples each), that were obtained from each division. In addition, two conventional pharmaceutical drugs (one powder for diarrhea, and one liquid for cough), from pharmacies were included as controls; hence the total of medicines processed for bacteriological analysis was 142.
Sampling technique
Prior informed consent was obtained from all the herbalists that offered their herbal medicine samples to be used in this study. Ethical approval for the study was obtained from the School of Health Sciences Research and Ethics Committee of Makerere University. The sampling frame exclusively involved herbalists that were engaged not only in trade, but also in harvesting, and/or preparation of the HM. The stratified sampling technique was adopted; viz, each administrative division of Kampala constituted a stratum 28 samples which were procured from herbal shops, market stalls, roadside stalls, and mobile stalls. Then, the random selection of individual herbal medicine samples from each stratum was done following the guidelines for research on HM products, established by the Uganda National Drug Authority (NDA) and the World Health organization38,60.
Specimen collection and transportation
We randomly selected some of the HM (ready for consumption), that had been proposed to potentially possess largely unknown species of bacterial contaminants in earlier studies, particularly those for diarrhea, cough, diabetes, and high blood pressure5,14. Upon procurement, the samples were aseptically wrapped in sterile zipped specimen bags, and transported on a cold chain for bacteriological analysis, in the microbiology laboratory at Makerere University, School of Veterinary Medicine. Since microbial loads may depend on temperature and humidity47; the samples were collected during dryness as well as frequent rains, from April to September 2021.
Media preparation, and bacteriological analysis
Three types of bacteriological analyses were performed, viz: (1) determination of bacterial total viable counts and total coliform counts, and (2) determination of total Escherichia coli counts, and (3) isolation and biochemical characterization of Klebsiella pneumoniae, Escherichia coli, Klebsiella oxytoca, Pseudomonas aeruginosa, Enterobacter spp., Staphylococcus aureus, Salmonella spp., Shigella spp., and Bacillus cereus.
Media preparation
All the media used in this study were prepared and casted into sterile bacterial culture plates by following the manufactures instructions. The bacterial total viable count was determined using Total Plate Count Agar (PCA), Batch Number 805161; while total coliform count was determined using Violet Red Bile Agar (VRBA), Batch Number: 605181. Both media were procured from Conda Pronadisa (Laboratorion Conda S.A.), in Spain (www.condalab.com). Pseudomonas aeruginosa was isolated using Kings Agar medium (KMA); Lot Number: 213075, manufactured by Techno Phermchem, Bahadurgarh, India. Staphylococcus aureus was isolated using Mannitol Salt Agar (MSA); Lot Number: 3213811, procured from Oxoid Ltd, Basingstoke, United Kingdom. Bacillus cereus was isolated using Bacillus cereus agar (BCA), Lot Number: 0000132719, manufactured by HiMedia Laboratories Pvt. Ltd, Mumbai, India. Salmonella spp. and Shigella spp. were isolated using Xylose Lysine Deoxycholate (XLD) agar; Lot Number: 2875014, manufactured by Oxoid Ltd, United Kingdom. Prior to culturing on XLD, the samples were first pre-enriched in peptone water; Batch Number: 602041, manufactured by Conda Pronadisa, Spain, followed by enrichment in Rappaport-Vassiliadis Soya Peptone (RVS) broth; Lot number: 2896635, manufactured by Oxoid Ltd, United Kingdom. All other coliform bacteria, such as E. coli, Klebsiella spp., and Enterobacter spp. were recovered from the colonies that grew on VRBA, during determination of TCC. Screening for Enterohaemorrhagic E. coli (017H7) was done using Sorbitol MacConkey; Lot number; 461684 procured from Oxoid Ltd, Basingstoke, United Kingdom. All the media was quality controlled through overnight incubation at 37 °C prior to inoculation, to rule out contamination.
Preparation of serial dilutions of herbal medicine samples
For the liquid samples (10° dilution), five test tubes (labeled 1–5) were arranged and 9.0 mls of sterile peptone water introduced into each tube. Then 1.0 ml of a sample was pipetted into test tube number 1 followed by thorough mixing, hence constituting the 10–1 dilution. 1.0 ml of the 10–1 dilution (in test tube 1), was pipetted into test tube 2 using a fresh pipette tip, followed by thorough mixing, hence constituting the 10–2 dilution, and the procedure was repeated up to test tube number 5, thus constituting the dilutions 10–3, 10–4 and 10–5, respectively. For the case of solid samples, 10 g of each sample were introduced into a stomach bag containing 90 mls of peptone water. The mixture was homogenized using a Pulsifier (Serial No: 30660282, Manufactured by Kalyx Biosciences Inc, Canada), and this constituted the 100 dilution which was then serially diluted up to the 10–5 through the same procedure applied above on liquid samples.
Determination of total viable counts (TVC)
0.1 ml of each serial dilution of the herbal medicine samples were pipetted onto PCA media plates, spread using a glass spreader, and incubated for 24 h at 37 °C. Colonies that grew were counted using a colony counter (CAT No: SC6+, Serial number: R570003270, made in United Kingdom, www.staurt.equipment.com), and expressed as Colony Forming Units per gram (CFU/g) for solid samples, or per milliliter (CFU/ml) for liquids. To convert the counted colonies into CFU, a standard formula (below), was used61.
The CFU of the different dilutions were computed and the mean was evaluated and recorded as the TVC of that sample. The mean TVC for each sample was compared with the permissible limits recommended by the World Health Organization18,19, to assess whether the samples were of good quality and safe for human consumption.
Determination of Total Coliform count (TCC)
0.1 ml of each dilution was pipetted onto VRBA media plates, spread using a glass spreader, and incubated for 24 h at 37 °C. Colonies that grew were counted using a colony counter (CAT No: SC6+, Serial number: R570003270, made in United Kingdom, www.staurt.equipment.com) and expressed as Colony Forming Units per gram (CFU/g) for solid samples, or per milliliter (CFU/ml) for liquids. The coliforms were considered as pale pink, moist/mucoid colonies that grew on VRBA media, except for E. coli which presented as hot pink, dry, flat/umbonate colonies. The CFU of the different dilutions were computed and the mean was evaluated and recorded as the TCC of the sample. The mean TCC for each sample was compared with the permissible limits recommended by the World Health Organization18, to assess whether the samples were of good quality and safe for human consumption. All samples with a mean TCC > 0.0 CFU/ml, or > 0.0 CFU/g were classified as unsafe for human consumption (WHO, 2007).
Isolation and identification of the targeted bacteria P. aeruginosa, S. aureus, B. cereus, E. coli, Klebsiella spp., Enterobacter spp., Salmonella spp. and Shigella spp.
To isolate the targeted bacterial species, 0.1 ml of the 10–1 dilution of each sample was spread plated on the appropriate culture media, viz; Pseudomonas aeruginosa (on Kings agar), Staphylococcus aureus (MSA), Bacillus cereus (BCA), E. coli, Klebsiella spp., and Enterobacter spp. (VRBA). For the case of Salmonella spp. and Shigella spp., prior to culturing on XLD agar, the samples were first taken through a pre-enrichment stage, followed by an enrichment process. Pre-enrichment was done by incubating the 10–1 dilution of each sample at 37 °C for 24 h. The enrichment culture procedure was then done by introducing 1.0 ml of the 24-h old pre-enriched culture into 9.0 mls of Rappaport–Vassiliadis Soya Peptone broth, followed by incubated for 24 h at 42 °C. One loopful of the enriched cultures were then streak plated on XLD.
All the inoculated agar plates were incubated at 37°C for 24 h. In the case of E. coli, the pink colonies that grew on VRBA were sub-cultured on sorbitol MacConkey and incubated at 37 °C for 24 h to screen for the potential presence of translucent colonies of Enterohaemorrhagic E. coli (E. coli: 017H7). The observed bacterial species in each sample were compared with the guidelines of the World Health Organization to assess if the samples were safe for human consumption (WHO10,18).
The bacterial colonies that grow were identified based on their cultural characteristics (growth and colony morphotypes on various forms of media), gram staining, and biochemical traits62. The biochemical experiments used for bacterial characterization in this study were as follows;
-
(a)
The catalase test: The catalase enzyme catalyzes the dissociation of hydrogen peroxide (a cytotoxic metabolite) to nontoxic products (water and oxygen), i.e., \({\text{2H}}_{{\text{2}}} {\text{O}}_{{\text{2}}} \left( {\text{l}} \right) \to {\text{2H}}_{{\text{2}}} {\text{O }}\left( {\text{l}} \right) + {\text{O}}_{{\text{2}}} \left( {\text{g}} \right)\). A loopful of 24 h-old bacterial colonies was introduced onto the inner walls of a screw-cap test tube containing 0.5 ml of H2O2 solution. The test tube was then capped (to prevent the escape of aerosols), and slanted in order for the H2O2 solution cover the bacterial colonies. Effervescence in about 30 s was indicative of a positive reaction63.
-
(b)
Urease test: The urease test examines the ability of the bacterial species to produce urease enzyme. This enzyme catalyzes the hydrolysis of urea into ammonia and carbondioxide, i.e. \({\text{(NH}}_{{\text{2}}} )_{{\text{2}}} {\text{CO}}\left( {{\text{aq}}} \right)_{~} + {\text{ H}}_{{\text{2}}} {\text{O}}\left( {\text{l}} \right) \to {\text{2NH}}_{{\text{3}}} \left( {\text{g}} \right)~~ + {\text{CO}}_{{\text{2}}} \left( {\text{g}} \right).\). The ammonia formed ionizes, resulting in an alkaline medium, viz; \({\text{NH}}_{{\text{3}}} \left( {\text{g}} \right)~~ + {\text{H}}_{{\text{2}}} {\text{O}}\left( {\text{l}} \right)~ \to {\text{NH}}_{{\text{4}}} ^{ + } \left( {{\text{aq}}} \right)~~ + {\text{ OH}}^{ - } \left( {{\text{aq}}} \right)\). The alkalinity is detected using a suitable Ph-indicator63,64. The butt and surface of a slant of 3.0 ml of urea agar base (containing phenol red indicator) supplemented with 5% v/v of 40% w/v urea solution, in a screw-cap test tube, was inoculated with 24 h-old bacterial colonies, and incubated at 37 °C for 24 h. The development of a red color in the urea agar was indicative of a positive urease reaction.
-
(c)
Indole production/tryptophan decomposition test: This test demonstrates the presence of tryptophanase enzyme in bacterial isolates, which enables them to metabolize the amino acid tryptophan. This enzyme catalyzes the breakdown of l-tryptophan into indole, pyruvic acid and ammonia. The indole is detected when it reacts with p-dimethylaminobenzaldehyde to form a quinoidal red-violet (red or pink) compound65. 2.0 mls of peptone broth in a screw-cap test tube were inoculated with a loopful of 24-h old bacterial colonies and incubated at 37 °C for 24 h. Then 3 drops of Kovac’s reagent were added to this broth culture. Formation of a red or pink ring on top of the broth culture was indicative of indole positive isolates.
-
(d)
Methyl red (MR) test: Both the MR test and the Voges–Proskauer (V–P) test are used to identify the fermentation pathways of bacterial isolates for acids and carbohydrates, respectively66. The MR test examines the ability of bacterial strains to catabolize glucose in a buffered media hence yielding ethanol, CO2, H2, and a mixture of organic acids such as succinic acid, lactic acid, formic acid, and acetic acid. The acids cause a drop in the pH of the culture below 4.2, and this is detected using a suitable indicator65,66. 2.0 mls of sterile methyl red-Voges–Proskauer (V–P) medium (glucose-phosphate) base in screw-cap test tubes were inoculated with a loopful of 24-h old bacterial colonies and incubated at 37 °C for 4 days, and then a drop of methyl red reagent (0.25 g of methyl red in 100 mls of ethanol) was added. The results were interpreted basing on the emergent colour changes, i.e., red colour (MR positive), any shade of orange or yellow was taken as a negative reaction.
-
(e)
V–P test (Voges–Proskauer test): This test is used to identify fermentative microbes that catabolize glucose via the butanediol pathway. During the glucose fermentation, acetoin (acetylmethylcarbinol) exists as an intermediate in the formation of 2,3-butanediol, which gets oxidized (in the presence of KOH and O2) to a diacetyl. The diacetyl reacts with a guanidine group present in amino acids such as arginine (contributed by peptone in the V–P media), to form a pink- to red-colored product and this colour may be intensified by α-naphthol63,65. 1.0 ml of MR-VP reagent in a screw-cap test tubes were inoculated with a loopful of 24-h old bacterial colonies and incubated at 37 °C for 4 days. 3 drops of reagent A (5.0 g of α-naphthol in 100 mls of absolute ethanol) were added and followed by 3 drops B (40.0 g of KOH in 100 mls of distilled water). Development of strong cherry red color on the surface of the media was indicative of a positive V–P test while a copper or lack of colouration showed a negative result.
-
(f)
Hydrogen sulfide (H2S) test: This examines the ability of microbes to produce hydrogen sulfide (H2S), through the anaerobic reduction of thiosulfate molecules (S2O32−). The detection of H2S is achieved through its reaction with Iron salts (present in the culture media), which yields black precipitates of either Iron(ii) Sulfide (FeS) or Iron(iii) Sulfides (Fe2S3)63,67. Using a stabbing wire, a 24-h old culture was stabbed into SIM (Sulfite Indole Motility) media in screw-cap test tubes and incubated at 37 °C for 24 h. The formation of black coloration in the media indicated positive results. This same test was used to assess the motility and indole production. Motile organisms were identified based on their observable growth away from the stabbing line, while indole production was deduced by adding a drop of Kovac’s reagent and observing the formation of pink colouration.
-
(g)
Triple Sugar Iron test (TSI): This test identifies bacterial strains basing on their differences in the carbohydrate fermentation patterns and hydrogen sulfide production ability66. The TSI agar contains sodium thiosulfate, peptone, three fermentative carbohydrates [lactose (1%), sucrose (1%) and glucose (0.1%)], and the phenol red acid base indicator. The accumulation of acids associated with carbohydrate fermentation, lowers the pH hance the phenol red indicator turns from orange-red to yellow, while the oxidative decarboxylation of peptone yields alkaline products hence the indicator turns deep red. The production of H2S is indicated by the black colour of the butt66. The TSI agar in the screw-cap test tubes was inoculated with 24-h old bacterial colonies, first by stabbing through the center of the media up to the bottom of the butt, followed by streaking on the surface of the slant. The tube was loosely capped and incubated at 37 °C for 24 h. Alkaline/acid (red slant/yellow butt) was interpreted as glucose fermentation only; acid/acid (yellow slant/yellow butt) as metabolization of glucose, lactose and/or sucrose; alkaline/alkaline (red slant/red butt) as absence of any carbohydrate fermentation; blackening of the media as H2S production, while bubbles or cracks in the agar were interpreted as gas (CO2 and H2) production.
Data analysis
Data were entered in MS-Excel and exported to STATA version 15.0 software. The data were tested for normality by using D'Agostino–Pearson test and normal distribution was accepted at (p > 0.05). Data were then analyzed using descriptive statistics (frequencies and percentages), and inferential statistics [Pearson’s Chi-square (in case of normality), or Mann–Whitney U test (for nonparametric data)], at 0.05 significancy level.
Ethical approval and consent to participate
The study sought ethical approval from the Makerere University School of Health Sciences Research Ethics Committee (Ref: MAKSHSREC-2020-72), Uganda National Council for Science and Technology (Ref: HS1278ES), and Kampala Capital City Authority (Ref: DPHE/KCCA/1301). The research was conducted in conformity to the national guidelines for the conduct of research in the COVID-19 era established by the Uganda National Council for Science and Technology (UNCST)68. Informed consent to participate in this study was obtained in writing from the study participants. Respondents’ identifiers were recorded in form of assigned codes instead of names to ensure anonymity.
Data availability
All data generated and analyzed during this study are available on request from the corresponding author.
Abbreviations
- HM:
-
Herbal medicine
- TMP:
-
Traditional Medical Practitioners
- WHO:
-
World Health Organization
- KCCA:
-
Kampala Capital City Authority
References
Walusansa, A. et al. Prevalence and dynamics of clinically significant bacterial contaminants in herbal medicines sold in East Africa from 2000 to 2020: A systematic review and meta-analysis. Trop. Med. Health 49(1), 1–14 (2021).
Centers for Disease Control and Prevention (CDC). Uganda Top 10 Causes of Death. Published online 2020. https://www.cdc.gov/globalhealth/countries/uganda/default.htm.
Walker, C. L. F. et al. Global burden of childhood pneumonia and diarrhoea. Lancet 381(9875), 1405–1416 (2013).
Iramiot, J. S., Kajumbula, H., Bazira, J., Kansiime, C. & Asiimwe, B. B. Antimicrobial resistance at a humans-animals interface in pastoralist communities of Kasese District: Why we must bring farmers into the picture. AAS Open Res. 2, 25 (2019).
Nanyanzi, J. Evaluation of bacterial contamination and label information of oral-liquid herbal medicinal products for cough in Makindye Division, Kampala District. Published online 2009.
Kira, J. D., Mkupasi, E. M., Katakweba, A. A. S. & Ngowi, H. A. Assessment of bacterial contamination in herbal medicine products vended in Morogoro Municipality, Tanzania. East Cent. Afr. J. Pharm. Sci. 24(1), 21–28 (2021).
Keter, L. et al. Bacteria contaminants and their antibiotic sensitivity from selected herbal medicinal products from Eldoret and Mombasa, Kenya. Am. J. Microbiol. 7(1), 18–28 (2016).
Kamatenesi-Mugisha, M. & Oryem-Origa, H. Medicinal plants used to induce labour during childbirth in western Uganda. J. Ethnopharmacol. 109(1), 1–9 (2007).
World Health Organization (WHO). WHO Traditional Medicine Strategy: 2014–2023. World Health Organization; 2013. https://apps.who.int/iris/handle/10665/92455.
World Health Organization (WHO). WHO Traditional Medicine Strategy 2002–2005; 2002.
Nordqvist, P. System order and function in urban sanitation governance: Exploring the concept of polycentric systems in the city of Kampala, Uganda. Published online 2013.
Campbell, M. R. Low-income housing in Kampala, Uganda: A strategy package to overcome barriers for delivering housing opportunities affordable to the urban poor. Published online 2011. https://dspace.mit.edu/bitstream/handle/1721.1/67233/759121706-MIT.pdf;sequence=2.
Uganda Bureau of Statistics (UBOS). Uganda National Household Survey 2016/17; 2018.
Musoke, W. Microbial and heavy metal contamination in herbal medicines in Uganda. Published online 2019.
Kabwama, S. N. et al. A large and persistent outbreak of typhoid fever caused by consuming contaminated water and street-vended beverages: Kampala, Uganda, January–June 2015. BMC Public Health 17(1), 23 (2017).
Najjuka, C. F., Kateete, D. P., Kajumbula, H. M., Joloba, M. L. & Essack, S. Y. Antimicrobial susceptibility profiles of Escherichia coli and Klebsiella pneumoniae isolated from outpatients in urban and rural districts of Uganda. BMC Res. Notes 9(1), 235 (2016).
Hassan, K. M., Njogu, P. M., Njuguna, N. M. & Ndwigah, S. N. Microbiological contamination of herbal medicinal products marketed in Kenya for chronic diseases: A case study of Nairobi metropolis. J. Herb. Med. 29, 100475 (2021).
World Health Organization (WHO). Guidelines for assessing quality of herbal medicines with reference to contaminants and residues. Geneva: World Health Organization; 2007. Published online 2007.
World Health Organization (WHO). Quality Control Methods for Herbal Materials. World Health Organization; 2011. https://apps.who.int/iris/handle/10665/44479.
Uganda National Drug Authority (NDA). Herbal Medicine Guidelines; 2021.
Vos, P. et al. Bergey’s Manual of Systematic Bacteriology: Volume 3: The Firmicutes, Vol ***3 (Springer, 2011).
Botha, J., Witkowski, E. T. F. & Shackleton, C. M. Market profiles and trade in medicinal plants in the Lowveld, South Africa. Environ. Conserv. 31(1), 38–46 (2004).
Posthouwer, C. Medicinal plants of kariakoo market, dar es salaam, Tanzania. MsC Res Proj Report, Leiden Univ Netherlands. Published online 2015.
Meke, G. S., Mumba, R. F. E., Bwanali, R. J. & Williams, V. L. The trade and marketing of traditional medicines in southern and central Malawi. Int. J. Sustain. Dev. World Ecol. 24(1), 73–87 (2017).
Mander, M., Ntuli, L., Diederichs, N. & Mavundla, K. Economics of the traditional medicine trade in South Africa care delivery. South Afr. Health Rev. 2007(1), 189–196 (2007).
Okot, D. F., Anywar, G., Namukobe, J. & Byamukama, R. Medicinal plants species used by herbalists in the treatment of snakebite envenomation in Uganda. Trop. Med. Health 48, 1–14 (2020).
Schultz, F., Anywar, G., Wack, B., Quave, C. L. & Garbe, L. A. Ethnobotanical study of selected medicinal plants traditionally used in the rural Greater Mpigi region of Uganda. J. Ethnopharmacol. 256, 112742 (2020).
Adia, M. M. et al. Medicinal plants used in malaria treatment by Prometra herbalists in Uganda. J. Ethnopharmacol. 155(1), 580–588. https://doi.org/10.1016/j.jep.2014.05.060 (2014).
Mugisha, M. K., Asiimwe, S., Namutebi, A., Borg-Karlson, A. K. & Kakudidi, E. K. Ethnobotanical study of indigenous knowledge on medicinal and nutritious plants used to manage opportunistic infections associated with HIV/AIDS in western Uganda. J. Ethnopharmacol. 155(1), 194–202. https://doi.org/10.1016/j.jep.2014.05.012 (2014).
Hahn, R. A. & Truman, B. I. Education improves public health and promotes health equity. Int. J. Health Serv. 45(4), 657–678. https://doi.org/10.1177/0020731415585986 (2015).
Cunningham, A. B. African medicinal plants. United Nations Educ. Sci. Cult. Organ. Paris 20, 20 (1993).
Ahmad, F., Zaidi, M. A. S., Sulaiman, N., & Majid, F. A. A. Issues and challenges in the development of the herbal industry in Malaysia. Pros Perkem. 10(1):227–238 (2015). https://www.ukm.my/fep/perkem/pdf/perkem2015/PERKEM_2015_3A1.pdf.
Han, J. et al. An authenticity survey of herbal medicines from markets in China using DNA barcoding. Sci. Rep. 6(1), 1–9 (2016).
Korir, R., Anzala, O., Jaoko, W., Bii, C. & Ketera, L. Multidrug-resistant bacterial isolates recovered from herbal medicinal products sold in Nairobi, Kenya. Health Res. J. 40, 55 (2017).
Rasethe, M. T., Semenya, S. S., & Maroyi, A. Medicinal plants traded in informal herbal medicine markets of the Limpopo Province, South Africa. Evid. Based Complement Altern. Med. 2019;2019. https://www.hindawi.com/journals/ecam/2019/2609532/.
Choi, S., Chung, Y. L. J., et al. Challenges of regulatory theory and practice: A study of hawker control in Hong Kong. Published online 2015. https://core.ac.uk/download/pdf/45604192.pdf.
Ngemenya, M. N. et al. Microbial, phytochemical, toxicity analyses and antibacterial activity against multidrug resistant bacteria of some traditional remedies sold in Buea Southwest Cameroon. BMC Complement Altern. Med. 19(1), 1–11 (2019).
Uganda National Drug Authority (NDA). Guidelines on Registration and Importation of Herbal Medicine Products for Human and Veterinary Use in Uganda; 2021. https://www.nda.or.ug/human-medicine-guidelines/.
Walusansa, A. et al. Herbal Medicine used for the treatment of diarrhea and cough in Kampala city, Uganda. Trop. Med. Health https://doi.org/10.21203/rs.3.rs-937360/v1 (2021).
Okunlola, A., Adewoyin, B. A. & Odeku, O. A. Evaluation of pharmaceutical and microbial qualities of some herbal medicinal products in south western Nigeria. Trop. J. Pharm. Res. 6(1), 661–670. https://doi.org/10.4314/tjpr.v6i1.14644 (2007).
Pierzynowska, K., Kamińska, T. & Węgrzyn, G. One drug to treat many diseases: Unlocking the economic trap of rare diseases. Metab. Brain Dis. 35(8), 1237–1240. https://doi.org/10.1007/s11011-020-00617-z (2020).
Yapar, E. A. & Özdemirhan, M. E. An overview on pharmacopoeias in the world and monograph elaboration techniques. Univ. J. Pharm. Res. 5, 57–64 (2020).
Wiggins, J. M., & Joseph, A. A. A brief history of pharmacopoeias: A global perspective. Published online 2020.
Gonsha, R. An Assessment of Bacterial Contamination of Locally Prepared Herbal/Traditional Oral Liquid Medicines Sold in Owino Market. Published online 2012. https://wfpha.confex.com/wfpha/2012/webprogram/Paper8962.html.
Niyonshima, D. “Staphylococcus aureus” Contamination Levels in Selected Local Herbal Medicines Sold in Kampala (GRIN Verlag, 2018).
Nakajima, K. et al. Rapid monitoring of microbial contamination on herbal medicines by fluorescent staining method. Lett. Appl. Microbiol. 40(2), 128–132. https://doi.org/10.1111/j.1472-765X.2004.01643.x (2005).
Abdolghani, A., Maryam, E. & Sara, S. Microbial indices of industrial and traditional medicinal herbs in Ahvaz, Iran. Foods Raw Mater. 8, 1 (2020).
Halkman, H. B., & Halkman, A. K. Coliform Bacteria. Sci. Direct. Published online 2014.
Bartram, J. & Ballance, R. Water Quality Monitoring: A Practical Guide to the Design and Implementation of Freshwater Quality Studies and Monitoring Programmes (CRC Press, 1996).
Jarzembowski, T. Commensal aerobic bacterial flora of the gastrointestinal tract of Pipistrellus nathusii (Chiroptera: Vespertilionidae): lack of Escherichia coli in fecal samples. Acta Chiropterol. 4(1), 99–106. https://doi.org/10.1016/j.genrep.2020.100709 (2002).
Walker, G., Musinguzi, B., Musa, K., et al. Assessment of Pathogenic Contamination and Antimicrobial Activity of Selected Herbal Medicinal Remedies in Mbarara City, South Western Uganda. Published online 2021.
Walusansa, A. et al. High prevalence of antibiotic resistant Escherichia coli serotype O157: H7 among pastoral communities in rural Uganda. Microbiol. Res. J. Int. 25, 36–43 (2020).
Nalwoga, J. et al. Drug resistant Staphylococcus aureus in clinical samples at Kampala International University-teaching Hospital, Bushenyi District, Uganda. Am. J. Biomed. Res. 4(4), 94–98 (2016).
World Health Organization (WHO). Global Priority List of Antibiotic Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics; 2018.
Esraa, K. M. Detection of objectionable and non-objectionable microorganisms in contaminated paracetamol dosage forms. Editor BOARD-2021 16(2–3), 3 (2021).
The Uganda Bureau of Statistics (UBOS). Uganda Demographic and Health Survey; 2020. http://library.health.go.ug/sites/default/files/resources/UBOSStatisticalAbstract2020.pdf.
Techno Mobile Limited. Tecno Phantom 9. Published 2019. https://www.tecno-mobile.com/ug/phones/product-list/.
Berendonk, T. U. et al. Tackling antibiotic resistance: The environmental framework. Nat. Rev. Microbiol. 13(5), 310–317 (2015).
Fischer AA, Laing JE, Townsend JW. Hand Book of Family Planning Operations Research Design, Population Council. New York. 1998:1–45.
World Health Organization (WHO). Guidelines for registration of traditional medicines in the WHO African Region. Published online 2014. https://apps.who.int/iris/bitstream/handle/10665/336176/9789290231479-eng.pdf.
International Standards Organisation (ISO). 4833-1 (2013): Microbiology of the food chain-Horizontal method for the enumeration of microorganisms-Part 1: Colony count at 30 degrees C by the pour plate technique. Int Organ Stand Geneva, Switz. Published online 2013.
Cheesbrough, M. District Laboratory Practice in Tropical Countries, Part 2 (Cambridge University Press, 2006).
Li, Q., Chen, X., Jiang, Y. & Jiang, C. Cultural, physiological, and biochemical identification of actinobacteria. Actinobacteria Basics Biotechnol. Appl. 2016, 87–111. https://doi.org/10.5772/61462 (2016).
Christensen, W. B. Urea decomposition as a means of differentiating Proteus and paracolon cultures from each other and from Salmonella and Shigella types. J. Bacteriol. 52(4), 461–466. https://doi.org/10.1128/jb.52.4.461-466.1946 (1946).
Lanyi, B. 1 Classical and rapid identification methods for medically important bacteria. In Methods in Microbiology, Vol ***19 (ed. Sad, D.) 1–67 (Elsevier, 1988). https://doi.org/10.1016/S0580-9517(08)70407-0.
Lesny, J. E., Mohan, A. P. & Vijaya, J. A. Bioremediation of petroleum-polluted soil using biosurfactant producing bacteria, Pseudomonas sp.. J. Sci. Res. 66, 1. https://doi.org/10.37398/JSR.2022.660124 (2022).
Levine, M., Epstein, S. S. & Vaughn, R. H. Differential reactions in the colon group of bacteria. Am. J. Public Health Nat. Health 24(5), 505–510 (1934).
Uganda National Council for Science and Technology (UNCST). National Guidelines for Conduct of Research During Coronavirus Disease 2019 (Covid-19) Pandemic; 2020. www.uncst.go.ug.
Acknowledgements
We wish to thank the directorate of public health of Kampala Capital City Authority (KCCA), and the Resident City Commissioner (RCC), who authorized conducting of this study. We also thank the herbalists in Kampala city who provided the HM samples. We gladly acknowledge the assistance in form of laboratory services rendered to us by Dr. Nathan Lubowa Musisi of Makerere University, college of veterinary medicine.
Funding
This study was funded by the Islamic Development Bank (IsDB), through a research and capacity development Grant phase two, awarded to Islamic University in Uganda (IUIU).
Author information
Authors and Affiliations
Contributions
A.W., and J.L.N., and S.A. conceived the research idea, and were involved in field data collection and manuscript writing. J.E.S., G.A., D.A., T.S. and H.M.K. were involved in data analysis and manuscript writing. T.S., E.K., and A.N. and N.L.M. were involved in data collection and manuscript writing. A.K.T., J.L.N. and E.K.K. were the overall supervisors and were involved in manuscript writing. All the authors proofread and approved the final draft of the manuscript. Consent to publish the findings of this study was obtained in writing from the study participants.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Walusansa, A., Nakavuma, J.L., Asiimwe, S. et al. Medically important bacteria isolated from commercial herbal medicines in Kampala city indicate the need to enhance safety frameworks. Sci Rep 12, 16647 (2022). https://doi.org/10.1038/s41598-022-21065-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21065-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.