Abstract
The spread of SARS-CoV-2 infections and the severity of the coronavirus disease of 2019 (COVID-19) pandemic have resulted in the rapid development of medications, vaccines, and countermeasures to reduce viral transmission. Although new treatment strategies for preventing SARS-CoV-2 infection are available, viral mutations remain a serious threat to the healthcare community. Hence, medical devices equipped with virus-eradication features are needed to prevent viral transmission. UV-LEDs are gaining popularity in the medical field, utilizing the most germicidal UVC spectrum, which acts through photoproduct formation. Herein, we developed a portable and rechargeable medical device that can disinfect SARS-CoV-2 in less than 10 s by 99.9%, lasting 6 h. Using this device, we investigated the antiviral effect of UVC-LED (275 nm) against SARS-CoV-2 as a function of irradiation distance and exposure time. Irradiation distance of 10–20 cm, < 10 s exposure time, and UV doses of > 10 mJ/cm2 were determined optimal for SARS-CoV-2 elimination (≥ 99.99% viral reduction). The UVC-LED systems have advantages such as fast-stabilizing intensity and insensitivity to temperature, and may contribute to developing medical devices capable of containing SARS-CoV-2 infection. By demonstrating SARS-CoV-2 inactivation with very short-term UVC-LED irradiation, our study may suggest guidelines for securing a safer medical environment.
Similar content being viewed by others
Introduction
The coronavirus disease of 2019 (COVID-19) pandemic has spread worldwide since its initial outbreak in 2019, causing serious morbidity and mortality. It is caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), a highly contagious virus, detected mainly in specimens from the respiratory tract and nasopharyngeal sites in COVID-19 patients1. Reports indicate transmission between humans within 2–10 days, showing that the virus spreads through direct contact, such as contaminated hands and surfaces, and via airborne routes2. Under environmental conditions, SARS-CoV-2 remains viable in aerosols for up to 3 h and is more stable on plastic and stainless steel (up to 72 h) than on copper (4 h) and cardboard (24 h)3. Exposure to contaminated environmental materials can be prevented by many control techniques, including heat sterilization, chemical disinfection, filtration disinfecting surfaces, and ultraviolet (UV) irradiation4. The possible material damage caused by heat sterilization and toxicity of chemical disinfectants, and the shortage of filters in the market pose a major challenge throughout the pandemic, generating an alarming demand of more sustainable disinfection systems4. Given the rapid transmission of the virus, it is important to develop sustainable measures and technologies that can inactivate the virus and limit transmission.
The global UVC (ultraviolet-C) market growth has been positively impacted by the COVID-19 outbreak. During the pandemic, UV air and surface disinfection has attracted attention to UV devices and many products became available on the market4. Various public places with different levels of contaminated air and environmental materials started using UV surface disinfection systems4. UV rays are classified into three basic types according to wavelength: UVA (320–400 nm), UVB (280–320 nm), and UVC (100–280 nm)5. Various research centers and laboratories are developing UVC-based products to prevent the spread of infection. UV light-emitting diodes (UV-LEDs) are mercury-free devices that can be used for on-demand operations6. While mercury lamps emit light only at a particular wavelength, UV-LEDs are capable of emitting light at multiple individual wavelengths5. As a public health and environmental safety measure, the United Nations Environment Programme (UNEP) banned mercury-containing products in 2013 and beginning in 2020, low-pressure mercury lamps were to be replaced with new UV-emitting sources7. UV irradiation is an emerging antimicrobial approach owing to its flexibility, availability, and easy control of radiation patterns8. Medical devices equipped with UV-LEDs are now gaining popularity in medical fields, with UVC, which acts through the formation of photoproducts, considered the most effective germicidal region within the UV spectrum9. Additionally, a recent study reported that the UVC-LED intensity was not affected by temperature changes or warm-up time10. Further, UVC-LED inactivates pathogens through several mechanisms, including nucleic acid or protein damage and producing oxygen radicals11,12. A recent study reported that irradiation with UVC-LED at a wavelength of 280 ± 5 nm rapidly inactivated SARS-COV-2 isolated from a COVID-19 patient9. Furthermore, another study reported the elimination of SARS-COV-2 upon treatment with high temperature (> 56 °C) and UVC irradiation (100–280 nm)13. Various technologies to disinfect COVID-19 employing UV include photoelectrochemical oxidation (PECO) technology used in developing an air purifier, wherein UV-A light was utilized to activate a catalyst in the nanoparticle-covered filter to oxidize air contaminants14. In accordance with these findings, we developed a portable and rechargeable medical device for SARS-CoV-2 disinfection, which can be utilized to sterilize hard-to-reach areas or surfaces that will stain or otherwise react upon contact with cleaning chemicals. In the current study, we demonstrate exposure time- and distance-dependent reductions in SARS-COV-2 by UVC and aim to optimize and validate the performance of the developed UVC-LED device.
Methods
UVC-LED irradiation system
A portable UVC device, manufactured by the Korea Railway Research Institute (KRRI), containing a 1000 mW LED module was used in the current study. The module also contained a cooling system and a human detection sensor, which were discarded after use to prevent contamination risks. UVC-exposure experiments were conducted using a UV-LED system with selected LEDs obtained from the Korea Institute of Lighting and ICT (Bucheon, Korea). The UV spectra of the UV-LED wavelengths used in this study were measured using an IDR300 Photobiological Safety Spectroradiometer (Bentham, Reading, UK).
Virus irradiation with UVC-LED
The SARS-CoV-2 resource (NCCP43326) utilized in this study was procured from the National Culture Collection for Pathogens of the Korea Center for Disease Control and Prevention. VeroE6 cells (African green monkey kidney cell line) were purchased from the Korean Cell Line Bank (Seoul, Korea). For these experiments, 100 μL of the viral suspension with a titer of 3.16 × 106 TCID50 (50% tissue culture infective dose)/mL was placed in a petri dish and covered with a quartz coverslip. The UVC-LED irradiance produced for the virus eradication was measured at different heights (10, 20, 30, and 50 cm) for different times (2–60 s). After UV exposure, the virus was collected and serially diluted tenfold and infected into the Vero-E6 cells. Infected cells were incubated for 3 d at 37 °C in a humidified 5% CO2 incubator, following which the cytotoxic effects were evaluated by staining with a crystal violet solution.
Verification of viral titer reduction as a function of UV exposure time and distance
The Vero E6 cells infected with the post-irradiated virus were stained, and the TCID50 was calculated using the Spearman–Karber method. The viral titers and reduction rates were determined according to the exposure time and distance between the UV radiation device and virus-infected cells. Virus reduction was calculated according to the following equation:
Verification of viral titer reduction according to UVC radiation dose
The UV dose was estimated by calculating UV irradiance based on exposure time (s) and distance (cm) between the UV-LED and virus surface. In this study, a device with a luminous intensity of 1000 mW was used, but considering the experimental loss, a value of 800 mW was used to calculate the UV dose according to Eq. (2):
The distance between the UVC-LED device and the plated virus was set at 10, 20, 30, and 50 cm, and exposure times of 2, 4, 5, 10, 20, 30, 40, 50, and 60 s were used. The plated virus was covered with a quartz coverslip for even UV exposure. Following exposure, the virus was harvested by washing the quartz coverslip with complete media, then serially diluted tenfold, and used to infect Vero-E6 cells. After incubating for 3 days, viral titer reduction was measured by staining cells with a crystal violet solution.
Statistical analysis
All measures of variance are presented as the standard error of the mean (SEM). Correlations of efficacy with irradiation distance and time and relationship to UV dose were analyzed using two-way analysis of variance (ANOVA) with a Tukey’s post-hoc test using Prism8 (GraphPad Software, San Diego, CA, USA).
Results
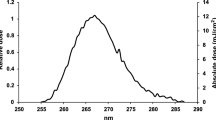
UVC-LED irradiance as a function of wavelength
The UVC-LED irradiance generated for virus eradication was measured at heights of 10, 20, 30, and 50 cm. We measured irradiance at a wavelength of 275 nm and confirmed that the intensity of the 275 nm peak gradually decreased at the sample as the distance from the source increased (Fig. 1). Accordingly, we assessed viral eradication at various irradiation time points and distances.
Viral reduction as a function of UVC exposure time and distance
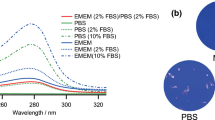
The distance between UVC-LED and plated virus (3.16 × 104 TCID50/mL, 100 µL) was fixed, and the exposure time was varied. The virus was covered and exposed to UVC, after which the virus was harvested for infection into the Vero-E6 cells (Fig. 2).
Post-irradiation, the viral reduction was measured as a function of varying UVC exposure time and distance by determining the viral titer (Fig. 3). After incubating for 3 days, cell death induced by virus infection was assessed by staining cells with a crystal violet solution. We observed that the viability of cells infected with UVC-irradiated virus gradually decreased with increasing UVC exposure time and a shorter distance between the virus and UVC-LED.
After staining the infected Vero E6 cells, TCID50 was calculated using the Spearman-Karber method (Fig. 4.). At 50 cm, the viral titers were calculated to be 3.2 × 103, 2.0 × 103, 6.8 × 102, 9.3 × 101, 7.8 × 101, 7.8 × 101, and 6.3 × 101 TCID50/mL at irradiation times of 5, 10, 20, 30, 40, 50, and 60 s, respectively, yielding the corresponding log TCID50/mL values of 3.468, 3.301, 2.801, 1.968, 1.884, 1.884, and 1.801. From these values, a viral reduction of ≥ 99.99% was calculated compared with the unirradiated viral samples (3.16 × 106 TCID50/mL, 6.500 log TCID50/mL) at irradiation times of > 30 s and a distance of 50 cm. At 30 cm, the viral titers were calculated to be 1.1 × 103 TCID50/mL (3.031 log TCID50/mL), 2.2 × 102 TCID50/mL (2.301 log TCID50/mL), and 6.3 × 101 TCID50/mL (1.801 log TCID50/mL) at irradiation times of 5, 10, and 20 s, respectively. At 20 cm, viral titers were calculated as 8.96 × 102 TCID50/mL (2.884 log TCID50/mL), 6.32 × 101 TCID50/mL (1.801 log TCID50/mL), and 6.32 × 101 TCID50/mL (1.801 log TCID50/mL) at irradiation times of 5, 10, and 20 s, respectively. Collectively, these data confirm a viral reduction rate of > 99.99% at 30 cm/20 s, 20 cm/10 s, and 20 cm/20 s. At 10 cm, viral titers were 7.80 × 101 TCID50/mL (1.884 log TCID50/mL) and 6.32 × 101 TCID50/mL (1.801 log TCID50/mL) at irradiation times of 2 and 4 s, both translating to a viral reduction rate of > 99.99%.
Verification of SARS-CoV-2 reduction as a function of ultraviolet C (UVC) exposure time and distance. After staining Vero E6 cells with crystal violet, 50% tissue culture infective dose (TCID50) was calculated using the Spearman–Karber method. (A) Determination of viral titer at variable radiation exposure time and distance between the UV light-emitting diode (UV-LED) and plated virus. (B) Determination of viral reduction rate over time at varying UV irradiation distance (*p ≤ 0.05, **p ≤ 0.005, ***p ≤ 0.0005 vs. 50 cm condition).
SARS-CoV-2 titer reduction as a function of UVC irradiation strength
UV doses at different distances and exposure times were calculated using Eq. (2) and a power of 800 mW rather than the actual 1000 mW to account for the experimental loss (Table 1). Four conditions (red font) resulted in a ≥ 99.99% viral reduction: 30 s UV at 50 cm, 20 s UV at 30 cm, 10 s UV at 20 cm, and 2 s UV at 10 cm.
Further, we verified the titer and viral reduction of SARS-CoV-2 as a function of UVC radiation (Fig. 5, Table 2). Interestingly, a common feature gleaned from these experiments is that the UV doses > 10 mJ/cm2 produced a 99.99% viral reduction. In case of the 20 cm/5 s condition, the calculated dose of 10 mJ/cm2, which is the same as determined for the 50 cm/30 s condition, showed ≥ 99.96% viral reduction, which is slightly lower than the 99.99% standard reduction. Therefore, we conclude that a UV dose of > 10 mJ/cm2 is required for a stable viral reduction of > 99.99%.
Verification of the SARS-CoV-2 titer reduction at different ultraviolet C (UVC) radiation doses. UV irradiance was deduced based on exposure time and distance between the UV light-emitting diode (UV-LED) and virus. (A) The variance of viral titer due to UV irradiation. (B) Evaluation of virus reduction rate by UV irradiation. The titer of non-irradiated virus was used as a negative control. ***p ≤ 0.0005.
Discussion
The spread of SARS-CoV-2 infection and the severity of the COVID-19 pandemic has raised worldwide concerns and has empowered the rapid development of medications, vaccines, and countermeasures to contain viral transmission. In this study, we investigated the antiviral effects of UVC-LED against SARS-CoV-2 at a wavelength of 275 nm at different distances and exposure times. The novelty of our study is that it presents the optimized SARS-CoV-2 deactivating conditions employing UVC-LED at a wavelength of 275 nm. We confirmed a viral reduction rate of ≥ 99.99% at 50 cm with irradiation for > 30 s, 30 cm with 20 s irradiation, 20 cm with 10 s irradiation, and 10 cm with 2 s irradiation. Collectively, these results reveal that a distance of 10–20 cm is ideal for rapid (< 10 s) viral eradication. According to our calculations, a UV dose of > 10 mJ/cm2 resulted in 99.99% reduction of the virus. Overall, we conclude that the distance of 10–20 cm between the UVC source and the virus contaminated surface, an exposure time of < 10 s, and a UV dose of > 10 mJ/cm2 are the ideal conditions for effective SARS-CoV-2 eradication.
Both community and healthcare settings are vulnerable to the spread of SARS-CoV-2, and the stability of SARS-CoV-2 will likely be a threat in both environments3. Although various clinical trials and vaccines are currently available for the treatment and prevention of SARS-CoV-2, viral mutations remain a serious threat to our healthcare community. Hence, medical devices equipped with virus-eradication features are required to prevent viral transmission in healthcare environments.
Devices equipped with UV-LEDs are now gaining popularity in the medical fields9. Within the UV spectrum, UVC is considered to have the most powerful germicidal effects, inactivating various microorganisms such as viruses, bacteria, protozoa, and fungi, among others, via formation of the pyrimidine dimers in DNA and RNA9,15. Consecutively, pyrimidine dimers are considered to be photoproducts that disrupt DNA replication and transcription, leading to cell death16. Shin et al. reported effective inactivation of Escherichia coli O157:H7, Salmonella typhimurium, and Listeria monocytogenes on medium surfaces using UVC-LED at a wavelength of 275 nm, and in water systems at 278 nm under various conditions10. Additionally, another study comparing different spectra of UVA, UVB, and UVC against influenza virus revealed that UVB- and UVC-LED irradiation were highly effective in inactivating the virus5. By demonstrating SARS-CoV-2 inactivation with very short-term UVC-LED irradiation and determining the optimal irradiation distances and exposure times, our study suggests guidelines for securing a safer medical environment. Considering the advantages of UVC-LED, such as rapidly stabilizing intensity and insensitivity to temperature10, this system may contribute to the development of medical devices capable of preventing SARS-CoV-2 infection.
Data availability
The datasets generated during the current study are available from the corresponding author (kimera@konkuk.ac.kr) on reasonable request.
References
Wölfel, R. et al. Virological assessment of hospitalized patients with COVID-2019. Nature 581, 465–469. https://doi.org/10.1038/s41586-020-2196-x (2020).
Kampf, G. et al. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 104, 246–251. https://doi.org/10.1016/j.jhin.2020.01.022 (2020).
van Doremalen, N. et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 382, 1564–1567. https://doi.org/10.1056/NEJMc2004973 (2020).
Raeiszadeh, M. & Adeli, B. A critical review on ultraviolet disinfection systems against COVID-19 outbreak: applicability, validation, and safety considerations. ACS Photon. 7, 2941–2951. https://doi.org/10.1021/acsphotonics.0c01245 (2020).
Nishisaka-Nonaka, R. et al. Irradiation by ultraviolet light-emitting diodes inactivates influenza a viruses by inhibiting replication and transcription of viral RNA in host cells. J. Photochem. Photobiol. B Biol. 189, 193–200. https://doi.org/10.1016/j.jphotobiol.2018.10.017 (2018).
Rattanakul, S. & Oguma, K. Inactivation kinetics and efficiencies of UV-LEDs against Pseudomonas aeruginosa, Legionella pneumophila, and surrogate microorganisms. Water Res. 130, 31–37. https://doi.org/10.1016/j.watres.2017.11.047 (2018).
Kim, D.-K. & Kang, D.-H. UVC LED irradiation effectively inactivates aerosolized viruses, bacteria, and fungi in a chamber-type air disinfection system. Appl. Environ. Microbiol. 84, e00944-e1918. https://doi.org/10.1128/aem.00944-18 (2018).
Gerchman, Y. et al. UV-LED disinfection of Coronavirus: Wavelength effect. J. Photochem. Photobiol. B Biol. 212, 112044. https://doi.org/10.1016/j.jphotobiol.2020.112044 (2020).
Inagaki, H. et al. Rapid inactivation of SARS-CoV-2 with deep-UV LED irradiation. Emerg. Microbes Infect. 9, 1744–1747. https://doi.org/10.1080/22221751.2020.1796529 (2020).
Shin, J. et al. Fundamental characteristics of deep-UV light-emitting diodes and their application to control foodborne pathogens. Appl. Environ. Microbiol. 82, 2–10. https://doi.org/10.1128/aem.01186-15 (2016).
Gerchman, Y. et al. The involvement of superoxide radicals in medium pressure UV derived inactivation. Water Res. 161, 119–125. https://doi.org/10.1016/j.watres.2019.05.084 (2019).
Rastogi, R. P. et al. Molecular mechanisms of ultraviolet radiation-induced DNA damage and repair. J. Nucl. Acids 2010, 592980. https://doi.org/10.4061/2010/592980 (2010).
Parsa, S. M. et al. Effectiveness of solar water disinfection in the era of COVID-19 (SARS-CoV-2) pandemic for contaminated water/wastewater treatment considering UV effect and temperature. J. Water Process Eng. 43, 17 (2021).
Chaudhary, V. et al. Advancements in research and development to combat COVID-19 using nanotechnology. Nanotechnol. Environ. Eng. 6, 8. https://doi.org/10.1007/s41204-021-00102-7 (2021).
Yaun, B. R. et al. Inhibition of pathogens on fresh produce by ultraviolet energy. Int. J. Food Microbiol. 90, 1–8. https://doi.org/10.1016/S0168-1605(03)00158-2 (2004).
Franz, C. M. et al. UV-C-inactivation of microorganisms in naturally cloudy apple juice using novel inactivation equipment based on Dean vortex technology. Food Control 20, 1103–1107. https://doi.org/10.1016/j.foodcont.2009.02.010 (2009).
Acknowledgements
This research was supported by the Korea Railroad Research Institute and the Ministry of Health & Welfare (grant No. HQ21C0264), the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (grant No. HQ21C0264, HV22C0263), and Ministry of Food and Drug Safety (grant No. 22183MFDS443) in 2022.
Author information
Authors and Affiliations
Contributions
Conceptualization, C.L.; methodology and validation, K.P.; validation and data curation, C.L and K.P.; original draft preparation and supervision, M.K.; manuscript writing, reviewing, and editing, and funding acquisition, Y.B.K. All authors have read and agreed to the published version of the manuscript. C.L. and K.P. are the co-first authors and M.K. and Y.B.K. are the co-corresponding authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, C., Park, K.H., Kim, M. et al. Optimized parameters for effective SARS-CoV-2 inactivation using UVC-LED at 275 nm. Sci Rep 12, 16664 (2022). https://doi.org/10.1038/s41598-022-20813-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20813-4
This article is cited by
-
Germicidal efficacy of continuous and pulsed ultraviolet-C radiation on pathogen models and SARS-CoV-2
Photochemical & Photobiological Sciences (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.