Abstract
Low birth weight is an indicator of maternal-related multifactorial problems such as malnutrition, illness, and work overload. As a result, low birth weight is associated with maternal anaemia, and both of them were significant public health issues in developing nations. Low birth weight and anaemia are caused by insufficient nutrient intake, which is especially severe during pregnancy. So, this study aimed to assess the effect of maternal anaemia during the late trimester on low birth weight among newborns in Northwest Ethiopia. A systematic random sampling technique was used to select 211 participants for the primary data collection. Face-to-face interviews were used to collect data, while blood samples were collected using standard operating procedures. For further analysis, the data file was imported into Stata version 16 (MP) software. The binary logistic regression model was used to investigate significant factors related to low birth weight. Finally, the statistical significance of the variables was determined using a p value of ≤ 0.05. The prevalence of anaemia among pregnant women in the late trimester and newborns was 34 (16.11%, 95% CI: 11.42, 21.78) and 64 (30.33%, 95% CI: 24.20, 37.01), respectively. The mean ± standard deviation of the newborn babies' weight was 3.19 ± 0.49 kg. The proportion of low birth weight among newborns was 26 (12.32%, 95% CI: 8.20, 17.53%). The independent effect of anaemia on low birth weight was 4.19 times while all other factors were constant (COR = 4.19, 95% CI: 1.70, 10.30). Maternal educational status [unable to read and write (AOR = 10.94, 95% CI: 1.74, 68.58) and attained secondary education (AOR = 8.06, 95% CI: 1.53, 42.36)], and maternal anaemia (AOR = 3.51, 95% CI: 1.29, 9.55) were associated with low birth weight after adjusting with all other variables. In this study, the proportion of low birth weight was high. Here, maternal anaemia alone had a significant independent role in the development of low birth weight. Maternal education status and anaemic conditions were associated with low birth weight among newborns. Early detection and treatment of maternal anaemia during pregnancy is crucial with the usual nutritional-related care.
Similar content being viewed by others
Introduction
Anaemia is hematological abnormality and has a significant public health problem globally. World Health Organization (WHO) reports that more than 1.62 billion people are affected globally. Of these, 56 million pregnant women (41.8%) were suffering from varying degrees of anaemia1. Despite anaemia being found worldwide, it's more prevalent in developing countries2. In Ethiopia, the prevalence of anaemia among pregnant women ranges from 11.6 to 45.4%3,4.
Anaemia is one of the complications during pregnancy, and it also has adverse effects on neonatal outcomes like5 fetal anaemia, stillbirth, and low and very low birth weight (LBW)6,7. A study conducted in Nepal showed that the risk of LBW was 6.8 times higher among anaemic mothers8. Another study reveals that anaemia during pregnancy increases the risk of LBW among newborns9.
Maternal nutritional deficiency during pregnancy affects the developmental process of the fetus, which subsequently influences the birth weight of the newborn10. The fetus is highly dependent on maternal nutritional intake since malnutrition during pregnancy leads to different adverse birth outcomes like LBW. During pregnancy, insufficient storage or inadequate intake of essential nutrients can cause harmful effects on both the mothers and newborn babies11,12,13.
Birth weight is a good indicator to measure multi-layered pubic-related health problems like long-term maternal malnutrition, health status, and poor health care delivery system. The LBW is one of the most basic and common health indicators used to assess the status of infants. It is still the major determinant of mortality, morbidity, and disability in infancy and childhood to a long-term impact on health outcomes in adult life. Also, it affects the health sector economy, has a higher risk of death and illness shortly after birth and non-communicable disease, and is a significant burden on society as a whole14,15.
According to the WHO, we can say LBW if the weight of the newborn is < 2500 gm16. The prevalence of LBW ranges from 15 to 20% (over 20 million births annually) globally, and a majority (90%) of them are found in low-and-middle-income countries17,18. According to the Ethiopian demographic health survey (EDHS) report, the magnitude of LBW increased from 11 to 13%19,20. Also, this prevalence is high (18%) in Southern Ethiopia21. Based on the 2011 EDHS finding, the magnitude of the LBW report varies from region to region, 30% in Afar, 28% in Amhara, 26% in Somali, and 27% in the Gambela region19.
As corresponded to normal, LBW infants were 20 times more likely to develop complications and die22. It is the potential risk of cognitive deficits23, motor delays24, cerebral palsy25, other behaviour26, and psychological-related problem27.
Birth weight is one of the predictive factors of newborn death in the first few months of life28. In Ethiopia, in 2014, there were 27,243 deaths, of which LBW accounted for 4.53% of the total deaths29. Globally, LBW is still a significant determinant factor for infant mortality, and morbidity, which causes short- and long-term consequences in later life.
LBW is an adverse health outcome that continues to later life and seriously impairs the normal functioning of an individual. LBW comes with numerous social and economic problems for a country30. Therefore, this study aimed to assess the effect of maternal anaemia on the birth weight of newborn babies.
Materials and methods
Study design, period, and setting
The primary data were collected cross-sectionally from February 1 to April 30, 2019. The initial study was conducted at the Gynecology and Obstetrics Department, University of Gondar Comprehensive Specialized Hospital in Gondar Town, Northwest Ethiopia. The Town is located in the Amhara region, 180 km far from Bahir Dar, the capital city of the Amhara regional state, and 727 km from Addis Ababa, the capital city of Ethiopia. Gondar Town is found 2133 m above sea level. The hospital delivers several primary services in paediatrics, surgery, gynaecology and obstetrics, and Internal medicines departments with teaching–learning activities.
Study population
All full-term newborn babies (39–42 weeks of gestational age) were the study population for this secondary data analysis.
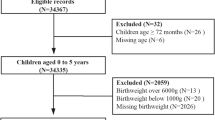
Sample size determination
For the primary objective (i.e. prevalence and associated factors of anemia among full-term newborn babies), the sample was determined using a single population proportion formula. But, this is a secondary data analysis beyond the primary objective. So, this secondary data analysis includes 211 full-term newborn babies data31.
Eligibility criteria
For this study, 211 study participants' data were included (full-term newborn babies paired with their mothers). During primary data collection, mothers who had twin newborns, complications during pregnancy, and known chronic illnesses (diabetes, preeclampsia/hypertension, HIV/AIDS, chronic kidney, liver disease, malaria, and any malignancy) were excluded from this study. If the clinician had already confirmed the diagnosis, then the presence of co-morbidities was taken into account (subclinical conditions were not investigated). Moreover, individuals with any hemoglobinopathy conditions were excluded from the study.
Sampling procedure
This secondary data was collected by applying a systematic random sampling technique was employed to select study participants. At this time, every 4th pregnant woman during the delivery time from February 1 to April 30, 2019. The first study participant was selected randomly by lottery methods every day, and excluded study participants were substituted by the succeeding participants (subsequent consecutive study participants).
Data collection methods and tools
At the time of primary data collection, the pre-tested Amharic version questionnaires were employed. The questionnaire consists of socioeconomic, dietary intake (iron-rich foods), antenatal care (ANC) follow-up, supplementation, complication during birth, and previous pregnancy-related characteristics. The weights were measured using the Seca scale, and results were recorded to the nearest 0.1 kg. About 3 ml cord blood sample was drawn from the umbilical vein of the cord by midwives professional, and from each selected mother, 3 ml of blood was drawn from each mother. Then, a complete blood count was done by laboratory professionals. The dietary data were collected using a meal frequency questionnaire with five options (once a week, twice a week, more than twice a week, once per month, and less than one time per month). Finally, we reduced it into three categories due to small frequency (twice and above a week, once a week, and no/never/not at all).
Data quality
Initially, a pre-test was done on 5% of the total sample size outside the study area (at Debre Tabor Referral Hospital) after training the data collectors. In addition, the questionnaire was collected using the Amharic language (local). At all times during the primary data collection, cross-checking of collected questionnaires was done daily. The collected data were checked for completeness and consistency by investigators and supervisors.
To ensure the quality of the laboratory test, a standard operating procedure was followed during specimen collection, and daily cleaning and background runs were done to ensure the laboratory results. Also, to avoid hemolysis and mix-up of sample, appropriate sample transportation using a test tube and labelling was done on the sample with the same identification number. All materials and reagents were checked for the expired date before sample processing.
Operational definitions
-
Anaemia among newborns: If the newborn Hb level was < 14 mg/dl from newborn cord blood.
-
Anaemia among pregnant women: If a Hb level of a pregnant woman was < 11 mg/dl after adjusting for altitude. The magnitude is further categorized as mild, moderate and severe anaemia if the haemoglobin count (g/dl) is between 10.0 and 10.9, 7.0 and 9.9 and < less than 7.0, respectively.
-
Low birth weight: If the birth weight of a newborn was < 2500 gr.
Data processing and analysis
This secondary data was imported to the Stata. Then, by using the Stata 16.0/MP version for windows, data cleaning, recategorizing, and tabulation were done. Then, both descriptive and analytical analysis of variables was employed. Binary and multivariable binary logistic regression analysis was hired to assess the independent and multiple effects of each variable on the LBW. During bivariable binary logistic regression, candidate variables for multivariable analysis were chosen if the p value was ≤ 0.25. Finally, a p value ≤ 0.05 was used to declare statistical significance during multivariable analysis. For each odd ratio (ORs; adjusted and crude), 95% CI was computed. The model fitness was tested using Hosmer and Lemeshow tests (p value = 0.9711) during the final model.
Ethical approval and consent from participants
For this secondary data analysis, the ethical clearance letter was obtained from the Ethical Review Committee of Debre Tabor University. Also, written informed consent was obtained from each selected mother after explaining the study. The data was collected without personal identifiers, and for anaemic and low-birth newborn babies, immediate consultation took place in addition to information dissemination by data collectors.
Results
Sociodemographic results of study participants
In this study, 211 participants' data were analyzed. The mean ± SD of the pregnant women’s age was 27.36 ± 5.19 years, which ranges from 18 to 44 years. All of the participants were from Amhara ethnic. Of all, 178 (84.36%) pregnant women were from urban areas. Only one-third of the pregnant women attended more than secondary school and above (Table 1).
Maternal reproductive health and newborn-related characteristics
Almost all pregnant women [198 (93.84%)] had ANC follow-up for their respective pregnancies. Also, all of the mothers had an intake history of Iron with folic acid supplementation for this pregnancy. More than half of the pregnant women [118 (55.92%)] were multigravida, while others were primigravida [93 (44.08%)]. From all, 171 (81.04%) the index children were delivered vaginally, but the rest of the pregnant women were delivered via cesarean section. Of all pregnant women, only [18 (8.53%)] have had a history of vaginal bleeding during their pregnancy.
Dietary intake-related characteristics of the pregnant women
Among study participants, the consumption of iron reach foods at least once per week was 50%. The consumption of vegetables, fruits, and red meat once per week was 93 (44.08%), 110 (52.13%), and 133 (63.03%), correspondingly (Table 2).
The magnitude of anaemia and low birth weight
The mean ± SD of the pregnant women's Hb after adjusting for altitude and hematocrit was 13.23 ± 1.81 g/dl and 39.66 ± 5.30, correspondingly. The prevalence of anaemia among the delivered women using the adjusted Hb for altitude was 34 (16.11%, 95% CI: 11.42, 21.78). Among anaemic pregnant women, the magnitude of moderate and mild anaemia was 11 (5.21%) and 23 (10.90%), respectively.
The mean ± SD of the newborn babies' Hb and hematocrits was 15.70 ± 2.11 g/dl and 47.81 ± 6.06, correspondingly. The prevalence of anaemia among the newborn was 64 (30.33%, 95% C:I 24.20, 37.01) using the cord blood adjusted Hb for altitude. The mean ± SD of the newborn babies’ weight was 3.19 ± 0.49 kg, which ranges from 1.60 to 4.2kgs. The proportion of LBW among newborns was 26 (12.32%, 95% CI: 8.20, 17.53%). The prevalence of LBW among anaemia and non-anaemic women was 10 (29.41%, 95% CI: 15.09–47.7%) and 16 (9.04%, 95% CI: 5.25 - 14.26%), respectively.
Factors associated with low birth weight among newborn
While all other factors were assumed constant, pregnant women who had anaemia during late pregnancy were 4.19 (COR = 4.19, 95% CI: 1.70, 10.30) times more likely to have a newborn with LBW as compared to those who had no anaemia. This finding shows that the prevention of anaemia is vital to decreasing the occurrence of LBW.
Also, the adjusted effects were assessed using bi-variable binary logistic regression. At this time, maternal anaemia status, maternal educational status, maternal occupation, consumption habit of vegetables, and consumption habit of red meat were the significantly associated variables for LBW. Finally, these significant variables were fitted into multivariable binary logistic regression. During multivariable analysis, maternal anaemia status and maternal educational status were the associated factors for the occurrence of LBW among newborns as shown in the table below (Table 3).
In this study, newborn babies from unable to read and write pregnant women were 10.94 times more likely (AOR = 10.94, 95% CI: 1.74, 68.58) to have LBW babies as compared to those who attend above high school. Also, these mothers who attended secondary education were 8.06 times (AOR = 8.06, 95% CI: 1.53, 42.36) more likely to give LBW newborn.
Likewise, the independent effect above, newborn children from anaemic pregnant women were 3.51 times (AOR = 3.51, 95% CI: 1.29, 9.55) more likely to have a low-birth-weight baby as compared to non-anaemic pregnant women.
Discussion
LBW is a leading public health problem that is mainly associated with an increased risk of newborn morbidity and mortality. Among different causes of LBW, anaemia during pregnancy is the one, which is occurred in each trimester of pregnancy worldwide32,33,34,35,36,37.
The prevalence of anaemia among the delivered women was 16.11% (95% CI: 11.42, 21.78). The result in this study is low while we compared with a study done in Jimma, Ethiopia (27.4%)38, Northwest Ethiopia (25.2%)39, India (78.45%)40, Egypt (72%)41, and Turkey (27%)42. This variation might be due to eligibility criteria like pregnancy complicated with diabetics, preeclampsia, hypertension, HIV/AIDS, and malaria were considered in these studies but excluded in our study. In addition, participants' habits of consumption of vegetables (80.1%), fruit (78%)43, and red meat (63%) were high. Besides, the regular antenatal follow-up with Iron and Folic Acid supplementation during pregnancy is also an asset44,45. All these factors were essential to prevent the occurrence of anaemia during pregnancy.
In this study, the prevalence of anaemia among newborns was 30.33% (95% CI: 24.20, 37.01) which was comparable to a study conducted in Brazil (32.6%)46. The possible reasons might be a similarity in socioeconomic status, dietary habits, lack of supplementation during pregnancy, and poor preconception and conception care.
The proportion of the LBW in the current study was 12.32%, (95% CI: 8.20, 17.53%). The finding of this study was comparable to the study done in Northern Ethiopia (10%)37, Pakistan (10.6%)47, Iran (9.5%)48, Northwest Ethiopia (14.9%)49, and Dessie, Ethiopia (15.6%)50. However, in this study, the prevalence of LBW was higher than in the study conducted in Northwestern Iran (6.8%)51. This might be due to the presence of maternal morbidity like anaemia secondary to inadequate intake of micro and macronutrients during pregnancy. In addition, maternal weight gain during pre-pregnancy is also the most crucial factor. Mothers' nutritional status is the most significant determinant of newborn children's birth weight. In this study, anaemic mothers were more likely to deliver LBW than those who had no anaemia, which was consistent with a study finding in India52.
The prevalence of LBW was lower as compared to a study conducted in Dilla Town, Southern Ethiopia (34.1%), Eastern Ethiopia (21%)53, India (22%)52, and Nigeria (20.3%)54. These might be due to sample size, dietary behaviours, and access to maternal health services on time, early ANC follow-up, preconception level of awareness, conception care, and household's asset or wealth status.
Here, being a newborn from a mother with anaemia alone will increase the risk of LBW by four times (COR = 4.19 (95% C:I 1.71, 10.30) as compared to their counterparts. Even this risk will increase more than 3-folds (AOR = 3.51 (95% CI: 1.29, 9.55) with all other contributing factors. The result indicates that prevention and controlling of anaemia alone will play a significant role to prevent the occurrence of LBW among newborns. The finding of this study is in line with the study conducted in Nigeria54, Indonesia55, Northern Ethiopia56, Southern Ethiopia57, and Dessie town, Ethiopia58. Another study in India also showed that maternal anaemia increases the incidence of LBW babies by 6.5%59. These might be due to the occurrence of anaemia secondary to hemodilution physiologically. Moreover, anaemia during pregnancy might be happening due to inadequate intake of nutrients, unable to take the recommended dose of Iron with folic acid supplementation during pregnancy, poor preconception and conception care, morbidity during pregnancy like helminthiasis, and poor diet quality. All these factors will directly or indirectly cause LBW.
In our study, newborn babies born from mothers who were unable to read and write were 10.94 times more likely (AOR = 10.94, 95% C:I 1.74, 68.58) to have LBW babies compared to those who attend above high school. Additionally, these mothers who attended secondary education were 8.06 times (AOR = 8.06, 95% CI: 1.53, 42.36) more likely to give LBW newborn. This finding is consistent with a study conducted in Ethiopia60. But maternal education was not statistically significant in the other studies conducted in two different parts of Ethiopia49,53. The possible reasons might be the level of awareness related to preconception care, residence, and the socioeconomic status of being unable to read and write might not be different.
Finally, maternal anaemia had significant effects of on the newborn birth weight. This study’s findings are similar to those study reported in China61, India40, Brazil62, Nepal63 Colombia64, Eastern Ethiopia65, and Southern Punjab, Asia66. This could be because of intrauterine growth restriction. In a low oxygen environment, the placenta proliferates and grows. When the maternal hemoglobin level falls, oxygen circulation in the fetal body is restricted. The fetal placenta is thus exposed to an oxidative stress environment (chronic hypoxia). As, a result Intrauterine fetal hypoxia impairs the transfer of oxygen/nutrient supply, resulting in fetal growth restriction and low birth weight67,68 due to placental angiogenesis.
Limitation of the study
Since this is secondary data analysis, all determinant variables were not fully considered in this study. This study might not link specific macro and micro-nutrient deficiencies as a cause of anaemia, a particular type of anaemia, and difficult to establish a possible causality with LBW. Furthermore, this study did not include the assessment of subclinical conditions at the time of the primary data collection, and some essential laboratory tests (like stool exams) were not done.
Conclusion
The prevalence of anaemia among pregnant women was a moderate public health problem. The magnitude of LBW among newborns was relatively high. Anaemia during pregnancy is the most significant predictor of LBW alone. Also, maternal educational status is one of the factors affecting LBW.
According to this study, during routine care, treatment of anaemia is highly recommended with regular Iron Folic Acid supplementation. Also, regular nutrition education and counselling are essential based on the maternal educational status. The involvement of stakeholders in the treatment of anaemia is warranted to decrease the rate of LBW and its late consequence.
Data availability
All the important data is found within the manuscript.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
Adjusted odds ratio
- COR:
-
Crude odds ratio
- Hb:
-
Haemoglobin
- LBW:
-
Low birth weight
- SD:
-
Standard deviation
- WHO:
-
World Health Organization
References
McLean, E., Cogswell, M., Egli, I., Wojdyla, D. & De Benoist, B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr. 12(4), 444–454 (2009).
Parks, S. et al. Maternal anaemia and maternal, fetal, and neonatal outcomes in a prospective cohort study in India and Pakistan. BJOG Int. J. Obstet. Gynaecol. 126(6), 737–743 (2019).
Gebreweld, A. & Tsegaye, A. Prevalence and factors associated with anemia among pregnant women attending antenatal clinic at St Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. Adv. Hematol. 2018, 1–8 (2018).
Melku M, Agmas A. Maternal anemia during pregnancy in Bahirdar Town, Northwestern Ethiopia: A facility-based retrospective study. Appl Med Res. 1(1), 2–7 https://doi.org/10.5455/amr.20150129110510 (2015).
Mahmood, T. et al. The association between iron-deficiency anemia and adverse pregnancy outcomes: A retrospective report from Pakistan. Cureus 11(10), e5854 (2019).
Nair, M., Gireesh, S., Yakoob, R. & Cherian, N. Effect of maternal anaemia on birth weight of term babies. Int. J. Contemp. Pediatr. 5(3), 1019–1022 (2018).
Baig, J. A. R., Jamal, M. M., Jamal, J. & Musarrat, M. To determine the association of maternal anemia with perinatal outcome in tertiary care hospital. Pak. Armed Forces Med. J. 70(2), 302–307 (2020).
Rana, S. S., Sharma, S., Chand, A. & Malla, R. Relationship between maternal Haemoglobin and fetal weight. Nepal J. Obstetr. Gynaecol. 8(1), 37–40 (2013).
Dane, B., Arslan, N., Batmaz, G. & Dane, C. Does maternal anemia affect the newborn. Özgün Araştırma. 5, 195–199 https://doi.org/10.4274/tpa.1068 (2013).
Roland, M. C. P. et al. Maternal factors associated with fetal growth and birthweight are independent determinants of placental weight and exhibit differential effects by fetal sex. PLoS ONE 9(2), e87303 (2014).
Esmaillzadeh, A., Samareh, S. & Azadbakht, L. Dietary patterns among pregnant women in the west-north of Iran. Pak. J. Biol. Sci. PJBS 11(5), 793 (2008).
Abedini, Z. & Gaini, M. Dietary food intake of pregnant women based on food guide pyramid and its related factors. Iran J. Nurs. 24(73), 36–46 (2011).
Woldeamanuel, G. G., Geta, T. G., Mohammed, T. P., Shuba, M. B. & Bafa, T. A. Effect of nutritional status of pregnant women on birth weight of newborns at Butajira Referral Hospital, Butajira, Ethiopia. SAGE Open Med. 7, 2050312119827096 (2019).
Gholamzadeh Baeis, M., Miladi Nia, M., Mosavi Nori, E., Sharifirad, G. R. & Mohebi, S. An overview of the role of effective maternal indicators on birth weight. Arch. Hyg. Sci. 3(2), 70–84 (2014).
Ahmad, M. O., Kalsoom, U., Sughra, U., Hadi, U. & Imran, M. Effect of maternal anaemia on birth weight. J. Ayub Med. Coll. Abbottabad 23(1), 77–79 (2011).
Organization, W. H. WHO handbook for guideline development Geneva (World Health Organization, 2014).
Organization WH. Global Nutrition Targets 2025: Low birth weight policy brief. World Health Organization, 2014.
Blencowe, H. et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: a systematic analysis. Lancet Glob. Health 7(7), e849–e860 (2019).
Demographic E. Health survey 2011 central statistical agency Addis Ababa. Ethiopia ICF International Calverton, Maryland, USA. 2012:135-9.
Demographic E. Health survey 2016 central statistical agency Addis Ababa. Ethiopia ICF International Calverton, Maryland, USA. 2017:158-63.
Alemu, A., Abageda, M., Assefa, B. & Melaku, G. Low birth weight: prevalence and associated factors among newborns at hospitals in Kambata-Tembaro zone, southern Ethiopia 2018. Pan Afr. Med. J. 34, 68. https://doi.org/10.11604/pamj.2019.34.68.18234 (2019).
WHO U. Low birth weight: Country. Regional and Global Estimates (UNICEF, New York). 2004.
Mathewson, K. J. et al. Mental health of extremely low birth weight survivors: a systematic review and meta-analysis. Psychol. Bull. 143(4), 347 (2017).
Al Hazzani, F., Al-Alaiyan, S., Hassanein, J. & Khadawardi, E. Short-term outcome of very low-birth-weight infants in a tertiary care hospital in Saudi Arabia. Ann. Saudi Med. 31(6), 581–585 (2011).
Chang, H.-Y. et al. Short-and long-term outcomes in very low birth weight infants with admission hypothermia. PLoS ONE 10(7), e0131976 (2015).
Fitzgibbons, S. C. et al. Mortality of necrotizing enterocolitis expressed by birth weight categories. J. Pediatr. Surg. 44(6), 1072–1076 (2009).
Fan, R. G., Portuguez, M. W. & Nunes, M. L. Cognition, behavior and social competence of preterm low birth weight children at school age. Clinics 68(7), 915–921 (2013).
Amosu, A. & Degun, A. Impact of maternal nutrition on birth weight of babies. Biomed Res India. 25(1), 75–77 (2014).
Amhara, E. A review of low birth weight in Ethiopia: socio-demographic and obstetric risk factors. Global J. Res. Rev. 5(1), 4 (2018).
Cavallo, M. C. et al. Cost of care and social consequences of very low birth weight infants without premature-related morbidities in Italy. Ital. J. Pediatr. 41(1), 1–12 (2015).
Tiruneh, T., Shiferaw, E. & Enawgaw, B. Prevalence and associated factors of anemia among full-term newborn babies at University of Gondar comprehensive specialized hospital, Northwest Ethiopia: a cross-sectional study. Ital. J. Pediatr. 46(1), 1–7 (2020).
Uche-Nwachi, E. et al. Anaemia in pregnancy: associations with parity, abortions and child spacing in primary healthcare clinic attendees in Trinidad and Tobago. Afr. Health Sci. 10(1), 66 (2010).
Murphy J. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva, World Health Organization, 2011 (WHO/NMH/NHD/MNM/11.1; http://www.who.int/vmnis/indicators/haemoglobin.pdf, accessed 1 December 2012).
Melku, M., Addis, Z., Alem, M. & Enawgaw, B. Prevalence and predictors of maternal anemia during pregnancy in Gondar, Northwest Ethiopia: an institutional based cross-sectional study. Anemia 2014, 20 https://doi.org/10.1155/2014/108593 (2014).
Bodeau-Livinec, F. et al. Maternal anemia in Benin: prevalence, risk factors, and association with low birth weight. Am. J. Trop. Med. Hyg. 85(3), 414–420 (2011).
Al-Mehaisen, L., Khader, Y., Al-Kuran, O., Abu Issa, F. & Amarin, Z. Maternal anemia in rural Jordan: room for improvement. Anemia 2011, 15 (2011).
Gebregzabiherher, Y., Haftu, A., Weldemariam, S. & Gebrehiwet, H. The prevalence and risk factors for low birth weight among term newborns in Adwa General Hospital, Northern Ethiopia. Obstetr. Gynecol. Int. 2017, 20 https://doi.org/10.1155/2017/2149156 (2017).
Berhane, M., Workneh, N. & Admassu, B. Incidence of low birth weight and its associated factors in Jimma University specialized hospital. Ethiop. J. Pediatr. Child Health 11(1), 45–53 (2015).
Asrie, F. Prevalence of anemia and its associated factors among pregnant women receiving antenatal care at Aymiba Health Center, northwest Ethiopia. J. Blood Med. 8, 35 (2017).
Kumari, S. et al. Maternal and severe anaemia in delivering women is associated with risk of preterm and low birth weight: A cross sectional study from Jharkhand, India. One Health 8, 100098 (2019).
Eweis, M. et al. Prevalence and determinants of anemia during the third trimester of pregnancy. Clin. Nutr. ESPEN 44, 194–199 (2021).
Tekgül, N. & Yamazhan, M. The effects of maternal anemia in pregnant women with respect to the newborn weight and the placental weight in the delivery room. J. Pediatric Res. 6(4), 342–346 (2019).
Egbi, G., Gbogbo, S., Mensah, G. E., Glover-Amengor, M. & Steiner-Asiedu, M. Effect of green leafy vegetables powder on anaemia and vitamin-A status of Ghanaian school children. BMC Nutr. 4(1), 1–10 (2018).
Zhao, D. et al. Risk factors for iron deficiency and iron deficiency anemia in pregnant women from plateau region and their impact on pregnancy outcome. Am. J. Transl. Res. 14(6), 4146 (2022).
Knijff, M., Roshita, A., Suryantan, J., Izwardy, D. & Rah, J. H. Frequent consumption of Micronutrient-Rich foods is associated with reduced risk of anemia among adolescent girls and boys in Indonesia: A Cross-Sectional study. Food Nutr. Bull. 42(1_suppl), S59–S71 (2021).
de Sá, S. A. et al. Anemia in pregnancy: impact on weight and in the development of anemia in newborn. Nutr. Hosp. 32(5), 2071–2079 (2015).
Khan, A., Nasrullah, F. D. & Jaleel, R. Frequency and risk factors of low birth weight in term pregnancy. Pak. J. Med. Sci. 32(1), 138 (2016).
Monjezi, M., Rostami, S., Moradi-Kal-Boland, M. & Cheraghian, B. Survey of the relationship between mother’s chronic diseases and low birth weight in infants, Ahvaz, South of Iran, 2014. Jundishapur J. Chronic Disease Care 6(2), e38259 (2017).
Kumlachew, W., Tezera, N. & Endalamaw, A. Below normal birth weight in the Northwest part of Ethiopia. BMC. Res. Notes 11(1), 1–7 (2018).
Jember, D. A., Menji, Z. A. & Yitayew, Y. A. Low birth weight and associated factors among newborn babies in health institutions in Dessie, Amhara, Ethiopia. J. Multidiscipl. Healthcare 13, 1839 (2020).
Fallah, R., Kazemnejad, A., Zayeri, F. & Shoghli, A. Birthweight related factors in northwestern Iran: using Quantile regression method. Global J. Health Sci. 8(7), 116 (2016).
Dubey, D. K. & Nath, D. C. An epidemiological model investigating the association between mothers nutritional status and low birth weight in India. Health 8(3), 251–261 (2016).
Sema, A. et al. Associated factors with low birth weight in Dire Dawa City, Eastern Ethiopia: A cross-sectional study. BioMed Res. Int. 2019, 5 https://doi.org/10.1155/2019/2965094 (2019).
Temidayo, A. L. & Amosu Ademola M. Maternal factors associated with low birth weight babies delivered in selected primary health care centres in abuja municipal area council, FCT, Nigeria. 2020.
Widiyanto, J. & Lismawati, G. Maternal age and anemia are risk factors of low birthweight of newborn. Enfermeria Clinica 29, 94–97 (2019).
Aboye, W., Berhe, T., Birhane, T. & Gerensea, H. Prevalence and associated factors of low birth weight in Axum town, Tigray, North Ethiopia. BMC. Res. Notes 11(1), 1–6 (2018).
Lake, E. A. & Fite, R. O. Low birth weight and its associated factors among newborns delivered at wolaita sodo university teaching and referral hospital, southern Ethiopia, 2018. Int. J. Pediatr. 2019, 5 https://doi.org/10.1155/2019/4628301 (2019).
Ahmed, S., Hassen, K. & Wakayo, T. A health facility based case-control study on determinants of low birth weight in Dassie town, Northeast Ethiopia: the role of nutritional factors. Nutr. J. 17(1), 1–10 (2018).
Kumar, K. J., Asha, N., Murthy, D. S., Sujatha, M. & Manjunath, V. Maternal anemia in various trimesters and its effect on newborn weight and maturity: an observational study. Int. J. Prev. Med. 4(2), 193 (2013).
Kassaw, M. W., Abebe, A. M., Kassie, A. M., Abate, B. B. & Masresha, S. A. Trends of proximate low birth weight and associations among children under-five years of age: Evidence from the 2016 Ethiopian demographic and health survey data. PLoS ONE 16(2), e0246587 (2021).
Liu, D. et al. Maternal hemoglobin concentrations and birth weight, low birth weight (LBW), and small for gestational age (SGA): Findings from a Prospective Study in Northwest China. Nutrients 14(4), 858 (2022).
Figueiredo, A. C. et al. Maternal anemia and low birth weight: a systematic review and meta-analysis. Nutrients 10(5), 601 (2018).
Shrestha, A. & Shrestha, S. A correlative study between maternal hemoglobin concentration during third trimester and fetal birth weight of babies born at Kathmandu Medical College and Teaching Hospital. J. Pathol. Nepal 10(2), 1756–1759 (2020).
Puerto, A. et al. Iron status in late pregnancy is inversely associated with birth weight in Colombia. Public Health Nutr. 24(15), 5090–5100 (2021).
Negera A, Sento M. The maternal anthropometry and hemoglobin status in relations to newborn birth weight among primiparous mothers at Adama Hospital Medical College, Eastern Ethiopia: a cross-sectional study. medRxiv. 2022.
Mukhtar, H., Batool, H. & Arish, M. Maternal anemia as a predictor of low birth weight babies in underdeveloped rural area of Southern Punjab. J. Med. Physiol. Biophys. 37, 58–62 (2017).
Ganju, S. Maternal anaemia, intra uterine growth restriction and neonatal outcomes. Int J Clin Obstet Gynaecol. 4(4), 152–155 https://doi.org/10.33545/gynae.2020.v4.i4c.638 (2020).
Thompson, L. P., Crimmins, S., Telugu, B. & Turan, S. Intrauterine hypoxia: Clinical consequences and therapeutic perspectives. Res Rep Neonatol. 5, 79–89 (2015).
Acknowledgements
We deeply acknowledge all the study participants and data collectors for their cooperation and commitment during this study.
Funding
We did not receive any funds for this project except support from Debre Tabor University.
Author information
Authors and Affiliations
Contributions
M.T.E.: made the draft of the proposal, and acquisition, analysis of data, and the interpretation or discussion, results of the manuscript; T.T.: worked on drafting the proposal, data analysis, interpretation, results, discussion, and draft and revise the final manuscript. T.E.: Edited the final manuscript. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Engidaw, M.T., Eyayu, T. & Tiruneh, T. The effect of maternal anaemia on low birth weight among newborns in Northwest Ethiopia. Sci Rep 12, 15280 (2022). https://doi.org/10.1038/s41598-022-19726-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19726-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.