Abstract
It is unclear whether the dose–response relationship between lung function and all-cause and cardiovascular mortality in the Central and Eastern European populations differ from that reported in the Western European and American populations. We used the prospective population-based HAPIEE cohort that includes randomly selected people with a mean age of 59 ± 7.3 years from population registers in Czech, Polish, Russian and Lithuanian urban centres. The baseline survey in 2002–2005 included 36,106 persons of whom 24,944 met the inclusion criteria. Cox proportional hazards models were used to estimate the dose–response relationship between lung function defined as FEV1 divided by height cubed and all-cause and cardiovascular mortality over 11–16 years of follow-up. Mortality rate increased in a dose–response manner from highest to lower FEV1/height3 deciles. Adjusted hazard ratios (HR) of all-cause mortality for persons in the 8th best, the 5th and the worst deciles were 1.27 (95% CI 1.08‒1.49), 1.37 (1.18–1.60) and 2.15 (1.86‒2.48), respectively; for cardiovascular mortality, the respective HRs were 1.84 (1.29–2.63), 2.35 (1.67–3.28) and 3.46 (2.50‒4.78). Patterns were similar across countries, with some statistically insignificant variation. FEV1/height3 is a strong predictor of all-cause and cardiovascular mortality, across full distribution of values, including persons with preserved lung function.
Similar content being viewed by others
Introduction
The prognostic value of impaired lung function in association with mortality is well documented1,2,3,4,5,6. It has been shown that reduced levels of forced expiratory volume measured in one second (FEV1) are a better tool in predicting mortality than forced vital capacity (FVC)7,8. FEV1 was also an independent predictor of all-cause and cardiovascular mortality and morbidity in population-based studies9,10. Impaired FEV1 had a stronger relationship with mortality and cardiovascular events than other common risk factors even at modest range of decrease in FEV111 independent from smoking and chronic respiratory diseases (COPD)12,13. Evidence is limited on predictive properties of FEV1 among persons with preserved lung function, but earlier studies suggested possible associations between lung function and mortality among those without lung function impairment14,15,16.
The conventional approach of lung function evaluation as the percentage of predicted value compared with reference values from healthy population has been criticised17,18,19. It less accounts for age-specific height variability and more prone to false positive results19. Global Lung Function Initiative (GLI) equation20 based on standardised Z-score by taking into accounts age, sex, height and ethnicity are a more valid approach but it has some limitations in elderly population17,19. Some other methods of standardising spirometry indices including FEV1 divided by height squared and/or cubed have been found a better alternative to predict survival function and mortality in this age category17,21,22,23,24. The assessment of lung function impairment by these methods is not dependent on predictive values and it is a more informative way of describing a dose–response relationship between lung function and mortality.
Most of the existing evidence in terms of mortality and lung function comes from Western European and American populations. Patterns of exposures and risk factors may be different in other populations, including Central and Eastern Europe. These countries have had higher mortality rates due to socioeconomic inequalities25, lifestyle patterns (e.g., nutritional, physiological and physical activity) and a very high burden from tobacco and alcohol use26,27. In this study we assessed the country-specific pattern of lung function defined as FEV1 divided by height cubed in association with all-cause and cardiovascular mortality in four Central and Eastern European countries.
Results
Baseline characteristics of the study population
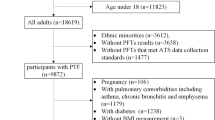
Altogether 36,106 individuals were recruited at baseline, of whom 24,944 met the inclusion criteria (Fig. 1). For logistic reasons, spirometry was conducted on 25,224 persons. For the same reasons, in the Polish cohort spirometry tests were performed only on random 50% of respondents in the 2nd year of baseline survey. Another reason for missing spirometry data was due to non-response in clinical examinations in Czech and Polish participants. Compared with the top tertile of FEV1/height3, persons in the lowest tertile were those at older ages with highest proportion of women and people with smoking history. The number of underlying chronic cardiovascular and lung diseases and diabetes was also greater for this group (Table 1). In comparison between countries, the prevalence of people in the lowest FEV1/height3 tertile was highest in Czech Republic and Lithuania, while a third of the Russian population were in the highest tertile group (Table 1).
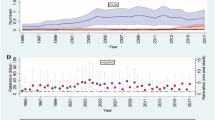
Association between lung function and all-cause and cardiovascular mortality
In total, 5069 persons died during a mean follow-up period of 13 years (Supplementary Table 1). More than a third of total deaths was due to cardiovascular causes. Mortality rate increased in a dose–response manner from the highest to lower FEV1/height3 deciles (mortality rate, 95% confidence interval (CI); 0.86, 0.76‒0.96 per 100 person-years among people in the highest and 3.10, 2.91‒3.31 per 100 person-years among people in the lowest FEV1/height3 decile (Table 2)). In the Cox proportional hazards regression model 1 that was adjusted for age, sex and country (Table 2, Supplementary Fig. 3), risk of death was already elevated in the group of people in the 8th decile (HR 1.39, 95% CI 1.19‒1.62) and it had a more than threefold increase in the lowest FEV1/height3 decile (HR 3.33, 95% CI 2.89‒3.82). In the model 2 that was adjusted for other baseline covariates (Table 2), being within the 8th decile of FEV1/height3 was still associated with increased mortality risk (HR 1.27, 95% CI 1.08‒1.49), and the risk was doubled in the lowest FEV1/height3 decile (HR 2.15, 95% CI 1.86‒2.48).
Cardiovascular mortality pattern was similar but with stronger association (Table 3, Supplementary Fig. 4). The strong association was observed even in the 9th decile compared to the 10th FEV1/height3 decile (Table 3, HR 1.62, 95% CI 1.12‒2.32) and it was approximately 3.5 times higher in the lowest FEV1/height3 decile (HR 3.46, 95% CI 2.50‒4.78) (Table 3).
Sensitivity analysis
Although the interactions between FEV1/height3 and country were not statistically significant, we also conducted analyses stratified by country. The excess risk of death in the lowest FEV1/height3 tertile was greater for people from Lithuania (HR 5.28, 95% CI 3.86‒7.24), whereas participants from the Czech Republic showed a two-times lower all-cause mortality (HR 2.46, 95% CI 1.82‒3.33) (Table 4, Supplementary Fig. 5). In terms of cardiovascular mortality, the highest increase in the risk of death was in Poland where people in the 9th decile of FEV1/height3 range had more than a threefold increased risk of mortality (Table 5, Supplementary Fig. 6, HR 3.38, 95% CI 1.25‒9.16) and it was more than 10-times higher in the lowest FEV1/height3 decile (HR 11.1, 95% CI 4.36‒28.23) (Table 5, Supplementary Fig. 6). The country-specific confidence intervals were wide and the differences in HRs between countries were not statistically significant (p for country heterogeneity = 0.31).
Discussion
Using data from the population-based cohort of people from four Central and Eastern European countries, we found a robust dose–response relationship between lung function (defined as FEV1/height3) and all-cause mortality with even stronger effects on cardiovascular mortality. The association was seen throughout all levels of lung function even in people with preserved function. The observed differences between countries were non-significant with higher all-cause mortality noticed in Lithuania and strongest association with cardiovascular mortality in Poland.
Many previous studies investigated the link between impaired lung function and mortality1,2,3,4,5,6. The predicting properties of lung function in terms of mortality have been evaluated applying different approaches, and the choice of the best one is not straightforward. Lung function prediction equations based on reference values from the general population (FEV1% percent predicted and z-score) have been largely used for categorisation of airway obstruction, however, both have some limitations for the use in the elderly population17,18,19,20. The major pitfalls of these approaches arise from the lack of sufficient data on this age group, possible survival bias of the selected people and impact of comorbidities on body size19. In our study, we explored the trend in mortality risk and lung function defined as FEV1 divided by height cubed. It has been shown that FEV1 standardised with height is a valid approach for predicting mortality risk in the elderly population17,23,24,28. Studies based on FEV1 standardised with height are scarce and the majority of them assessed the mortality risk through the commonly used comparison between healthy and people with the impaired lung function from the lowest tertile or quartile17,21,22,29.
We ranked FEV1/height3 into deciles in order to explore the risk of death across all levels of lung function including individuals with preserved lung function. The association was continuous, graded and considerably stronger for deaths from cardiovascular causes than for all-cause mortality. There is a paucity of studies evaluated the lung function across the whole spectrum in association with mortality. Ashley et al., using data on 2869 subjects from the Framingham Study, found a continuous association between FVC and all-cause mortality14. Analyses of data on 1195 people of the Buffalo Health Study and 1541 participants of the Rancho Bernardo Study also reported associations with mortality across FEV1 quantiles and quartiles, respectively15,16. More recently, Gupta et al. in the study of lifelong non-smokers has shown a consistent association with the risk of death per unit decrement in FEV1 and FVC z-scores as a measure of lung function but in more detailed assessment, the association across lung function quartiles was observed only with deaths from cardiovascular causes12. Moreover, the risk increase was more pronounced in groups corresponding to mild and mild to moderate decline in lung function compared to more severe impairment. Similar trend was also found in another study on mortality and cardiovascular adverse events in association with reduced lung function; which suggested that existing thresholds in defining lung function impairment might be misleading in terms of real impact of lung function on health risks11.
In line with previous studies, we also found a stronger association with cardiovascular mortality compared to deaths from all-causes. The exact mechanism underlying these associations remains unclear. Some epigenetic aging biomarkers may reflect lung function in elderly people30. Previous studies demonstrated that impaired lung function was associated with the severity of coronary atherosclerosis and vascular stiffness31,32. It was also an independent risk factor for predicting future cardiovascular disease and diabetes16,33,34. Lung function might act via similar mechanisms as other common risk factors (i.e., hypertension, obesity, level of physical activity and smoking) by triggering inflammatory processes that play a causal role in the development of chronic diseases leading to increased mortality22,35,36. In our study, the graded association with the risk of death remained strong after adjusting for potential confounders across all deciles suggesting the direct causal effect of lung function with mortality.
Most of the previous studies were performed in western populations, while studies investigating other populations are limited. In the large prospective international multi-ethnic (PURE) cohort study, the risk of death and cardiovascular events was elevated in persons with impaired lung function across all populations and it was highest in people from low- and middle-income countries11.
In our study, the association was similar across four countries with different socioeconomic status and health behaviour patterns, with non-significant variation between the countries. Compared to other populations from the Czech Republic and Russia, participants from Poland and Lithuania had higher number of pre-existing conditions that might partly explain the variation in results (Supplementary Table 2). Interestingly, the number of heavy smokers and people with COPD was the highest in Russia, where the effect of lung function was not particularly strong. Previous analyses have shown that lower socioeconomic status throughout a lifespan was associated with poorer lung function37 and that larger socioeconomic inequalities and higher mortality risk were in Russia25. Our study confirmed that lung function is a strong independent predictor of mortality risk, while its contribution to variation in mortality between countries remains unclear.
Strengths and limitations
Our study included people from urban communities of four Central and Eastern European countries. While the study cohort is in general representative for urban populations, it does not include rural areas, and the results are thus not generalizable to entire population of included countries. The response rate was comparable and follow-up time was balanced between countries. Although, some participants with less healthy status from Czech and Polish cohorts did not underwent the baseline clinical examination and that could lead to the underestimation of our results. Large sample size, standardised data collection across all populations, adjustment for a large number of investigating covariates in the association of lung function and mortality is the particular strength of this study. However, the self-report of information in the questionnaire may be a source of reporting bias.
Limited data is available on the use of FEV1/height3 in defining lung function and further studies needed to validate this approach. However, such an approach does not require reference values and considered as a better tool for predicting mortality risk in the elderly population17,23,24,28.
Finally, the nature of our design cannot entirely exclude reverse causation, although the longitudinal design, extensive covariate adjustment of models and long follow-up likely to minimize these limitations.
Conclusion
This study explored the association of lung function with all-cause and cardiovascular mortality in the Central and Eastern European populations. We showed a significant dose–response relationship of lung function with risk of death across the whole spectrum of FEV1/height3. The results emphasize the important contribution of lung function to cardiovascular and total mortality risk. If further research confirms the use of FEV1/height3 in assessing lung function in the elderly population, this measure may have a useful role in predicting future mortality risk in clinical practice.
Methods
Study design and participants
The prospective Health, Alcohol and Psychosocial factors in Eastern Europe (HAPIEE) cohort study has been designed to investigate risk factors for high rates of mortality and cardiovascular diseases in four Central and Eastern European countries (e.g., Czech Republic, Poland, Russia and Lithuania)38. It includes randomly selected people with a mean age of 59 ± 7.3 from population registers in seven towns in the Czech Republic and in big cities such as Novosibirsk in Russia, Krakow in Poland and Kaunas in Lithuania (N = 36,106). Data on age, sex, health status, medical examination, lifestyle, socioeconomic and psychosocial factors were collected during 2002–2005. The follow-up survey in the Czech Republic, Russia and Poland and baseline survey in Lithuania were conducted in 2005–2008 with the use of face-to-face computer assisted personal interviews combined with the clinical examination.
The follow-up time was estimated based on deaths occurring until the end of 2020 in the Czech Republic, until 31 July 2017 in Poland, until the end of 2017 in Russia and until 31 March 2019 in Lithuania. Persons with complete follow-up data were included in the study. Participants were censored on the date of death or the end of the study depending on data availability for each country.
Ethics approval
All participants provided written informed consent. The study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Joint UCL/UCLH Committees on the Ethics of Human Research (Committee Alpha), reference 99/0081; the Ethical Committee of the Institute of Internal Medicine, Siberian Branch of the Russian Academy of Medical Sciences, March 14, 2002 (Protocol No. 1); the Ethics Committee of the Kaunas Medical University (reference P1-09/2005); and Ethics Committee at the National Institute of Public Health, Prague (reference 2002-01-08/P1).
Spirometry
Lung function test was performed using a Micro-Medical Microplus spirometer. Participants with acute pulmonary infections and illnesses (e.g., vomiting and nausea), recent surgical procedures and cardiovascular conditions (e.g., myocardial infarction and stroke) were excluded from testing39. Two or more measurements of FEV1 within 150 ml variation considered for the study39. For each participant the highest value of FEV1 was selected. FEV1 was standardised by height and defined as FEV1 divided by height cubed (FEV1/height3). It was expressed at levels of tertiles and deciles of their distribution for further analyses.
Outcome
The primary outcome was all-cause mortality. Dates of death were obtained from the national or regional (Novosibirsk) death registers in each country. All registers have been shown a complete coverage of deaths38. In this study cause-specific mortality was based on underlying causes of death which are determined according to the selection and application rules of ICD-10 maintained by the World Health Organization (WHO).
Covariates
Data on covariates was obtained from questionnaires and medical examination. The selection of variables was based on their known association with mortality40,41. For the adjustment we considered age, sex, country, education (primary, secondary education, college or university degree), occupation (employed as entrepreneur or freelancer, housewife, farmer, retired or unemployed), deprivation scale (graded from 1 as a least deprived up to 12 as a most deprived), smoking status (never, current or past heavy smoker (> 30 cigarettes per day), moderate smoker (11–29 cigarettes per day), or light smoker (< 10 cigarettes per day))42, alcohol consumption (never, graduated frequency from 1 to 3 drinks monthly or 1–5 drinks weekly) and physical activity (as number of hours demanding physical activity per week). We also identified the following self-reported comorbidities: stroke, myocardial infarction, ischemic heart disease, hypertension (defined as measured blood pressure > 140/90 mm Hg and self-reported treated hypertension), diabetes (treated and/or untreated), asthma and COPD, any type of surgery (in last 3 months), cancer.
Information on pulmonary symptoms such as cough with or without phlegm (for 3 months) and chest pain were also included in the analyses as markers of respiratory diseases. Confounders obtained during medical examination were weight, height, body-mass index (BMI), blood pressure and cholesterol level.
Statistical analyses
All analyses were performed with Stata (Version 14; StataCorp). Descriptive statistics are presented as means with standard deviations (SD) or frequencies with proportions and were compared across FEV1/height3 tertiles.
The risk of death in association with FEV1/height3 was compared by Cox proportional hazards regression models. Deciles of FEV1/height3 were entered into the model as categorical variable accounting for level of lung function with highest category set as a reference. We used robust variance estimator to account for possible interactions between groups and multiple comparison. Proportional hazards assumptions were confirmed by exploring parallelism of log negative and log estimated survival curves for each covariate (Supplementary Figs. 1, 2). Hazard ratios (HR) with their corresponding 95% confidence intervals (CI) were estimated by crude (included age, sex and country) and confounder-adjusted models.
Dose–response relationship between FEV1/height3 and mortality was also assessed by entering FEV1/height3 as a continuous variable into the model. Linear trend was explored by adding quadratic terms and splines.
In addition to all-cause mortality, we investigated cardiovascular mortality. These analyses were restricted to diseases of circulatory system (ICD10 codes I00-I99).
We also conducted separate stratified sensitivity analysis for each country.
Data availability
The data that support the findings of this study are available from the register maintainers but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the register maintainers.
References
Weinmayr, G. et al. Association of lung function with overall mortality is independent of inflammatory, cardiac, and functional biomarkers in older adults: The ActiFE-study. Sci. Rep. https://doi.org/10.1038/s41598-020-68372-w (2020).
Baughman, P. et al. Combined effect of lung function level and decline increases morbidity and mortality risks. Eur. J. Epidemiol. 27, 933–943 (2012).
Leivseth, L., Nilsen, T. I. L., Mai, X. M., Johnsen, R. & Langhammer, A. Lung function and respiratory symptoms in association with mortality: The HUNT study. Copd-J. Chronic Obstruct. Pulm. Dis. 11, 59–80 (2014).
Yang, K., Wu, Y., Chen, D., Liu, S. & Chen, R. The impact of lung function on extra-pulmonary diseases and all-cause mortality in US adult population with and without COPD. Clin. Epidemiol. https://doi.org/10.2147/CLEP.S270599 (2020).
Vaz Fragoso, C. A., van Ness, P. H. & McAvay, G. J. FEV(1) as a standalone spirometric predictor and the attributable fraction for death in older persons. Respir. Care 65, 217–226 (2020).
Sircar, K., Hnizdo, E., Petsonk, E. & Atffield, M. Decline in lung function and mortality: Implications for medical monitoring. Occup. Environ. Med. 64, 461–466 (2007).
Bikov, A. et al. FEV 1 is a stronger mortality predictor than FVC in patients with moderate COPD and with an increased risk for cardiovascular disease. Int. J. Chronic Obstruct. Pulm. Dis. 15, 1135. https://doi.org/10.2147/COPD.S242809 (2020).
Menezes, A. M. B. et al. FEV 1 is a better predictor of mortality than FVC: The PLATINO cohort study. PLoS ONE 9, e109732. https://doi.org/10.1371/journal.pone.0109732 (2014).
Ching, S.-M. et al. FEV1 and total Cardiovascular mortality and morbidity over an 18 years follow-up population-based prospective EPIC-NORFOLK study. BMC Public Health https://doi.org/10.1186/s12889-019-6818-x (2019).
Sunyer, J. & Ulrik, C. S. Level of FEV1 as a predictor of all-cause and cardiovascular mortality: An effect beyond smoking and physical fitness? Eur. Respir. J. 25, 587. https://doi.org/10.1183/09031936.05.00011105 (2005).
Duong, M. et al. Mortality and cardiovascular and respiratory morbidity in individuals with impaired FEV1 (PURE): An international, community-based cohort study. Lancet Global Health 7, E613–E623 (2019).
Gupta, R. P. & Strachan, D. P. Ventilatory function as a predictor of mortality in lifelong non-smokers: Evidence from large British cohort studies. BMJ Open 7, e015381 (2017).
Loth, D. W. et al. Normal spirometry values in healthy elderly: The Rotterdam study. Eur. J. Epidemiol. 28, 329–334 (2013).
Ashley, F., Kannel, W. B., Sorlie, P. D. & Masson, R. Pulmonary function: Relation to aging, cigarette habit, and mortality: The Framingham study. Ann. Intern. Med. 82, 739–745 (1975).
Schünemann, H. J., Dorn, J., Grant, B. J. B., Winkelstein, W. & Trevisan, M. Pulmonary function is a long-term predictor of mortality in the general population: 29-year follow-up of the Buffalo Health Study. Chest 118, 656–664 (2000).
Lee, H. M., Liu, M. A., Barrett-Connor, E. & Wong, N. D. Association of lung function with coronary heart disease and cardiovascular disease outcomes in elderly: The Rancho Bernardo study. Respir. Med. 108, 1779–1785 (2014).
Pedone, C. et al. Alternative ways of expressing FEV1 and mortality in elderly people with and without COPD. Eur. Respir. J. 41, 800–805 (2013).
Sylvester, K. P. et al. ARTP statement on pulmonary function testing 2020. Bmj Open Respir. Res. 7, e000575 (2020).
Miller, M. R., Thinggaard, M., Christensen, K., Pedersen, O. F. & Sigsgaard, T. Best lung function equations for the very elderly selected by survival analysis. Eur. Respir. J. 43, 1338–1346 (2014).
Quanjer, P. H. et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 40, 1324–1343 (2012).
Turkeshi, E. et al. Short-term prognostic value of forced expiratory volume in 1 second divided by height cubed in a prospective cohort of people 80 years and older. BMC Geriatr. https://doi.org/10.1186/s12877-015-0013-4 (2015).
Sabia, S. et al. Why does lung function predict mortality? Results from the whitehall ii cohort study. Am. J. Epidemiol. 172, 1415–1423 (2010).
Miller, M. R. & Pedersen, O. F. New concepts for expressing forced expiratory volume in 1 s arising from survival analysis. Eur. Respir. J. 35, 873–882 (2010).
Chinn, S., Gislason, T., Aspelund, T. & Gudnason, V. Optimum expression of adult lung function based on all-cause mortality: Results from the Reykjavik study. Respir. Med. 101, 601–609 (2007).
Vandenheede, H. et al. Socioeconomic inequalities in all-cause mortality in the Czech Republic, Russia, Poland and Lithuania in the 2000s: Findings from the HAPIEE Study. J. Epidemiol. Community Health 68, 297–303 (2014).
Kolossváry, E., Björck, M. & Behrendt, C. A. A divide between the western European and the central and Eastern European countries in the peripheral vascular field: A narrative review of the literature. J. Clin. Med. 10, 3553 (2021).
Powles, J. W. et al. The contribution of leading diseases and risk factors to excess losses of healthy life in eastern Europe: Burden of disease study. BMC Public Health 5, 1–10 (2005).
Bhatta, L. et al. Spirometric classifications of COPD severity as predictive markers for clinical outcomes: The HUNT Study. MedRxiv. https://doi.org/10.1101/2020.11.03.20221432 (2020).
Hegendörfer, E., Vaes, B., Matheï, C., van Pottelbergh, G. & Degryse, J. M. Prognostic value of short-term decline of forced expiratory volume in 1 s over height cubed (FEV 1/Ht 3) in a cohort of adults aged 80 and over. Aging Clin. Exp. Res. 30, 507–516 (2018).
Wang, C. et al. Biomarkers of aging and lung function in the normative aging study. Aging 12, 11942 (2020).
Kim, J. J. et al. Relationship between airflow obstruction and coronary atherosclerosis in asymptomatic individuals: Evaluation by coronary CT angiography. Int. J. Cardiovasc. Imaging 34, 641–648 (2018).
Sheen, S. S. et al. Airflow limitation as a risk factor for vascular stiffness. Int. J. Tuberc. Lung Dis. 24, 577–584 (2020).
Min, K. B. & Min, J. Y. Reduced lung function, C-reactive protein, and increased risk of cardiovascular mortality. Circ. J. 78, 2309-U423 (2014).
Lin, W. Y., Yao, C. A., Wang, H. C. & Huang, K. C. Impaired lung function is associated with obesity and metabolic syndrome in adults. Obesity 14, 1654–1661 (2006).
Liu, G. Y. & Kalhan, R. Impaired respiratory health and life course transitions from health to chronic lung disease. Chest 160, 879–889 (2021).
Miller, J. et al. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir. Med. 107, 1376–1384 (2013).
Polak, M. et al. Socioeconomic status and pulmonary function, transition from childhood to adulthood: Cross-sectional results from the polish part of the HAPIEE study. BMJ Open 9, e022638 (2019).
Peasey, A. et al. Determinants of cardiovascular disease and other non-communicable diseases in Central and Eastern Europe: Rationale and design of the HAPIEE study. BMC Public Health 6, 255 (2006).
Graham, B. L. et al. Standardization of spirometry 2019 update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 200, e70 (2019).
Zhang, Y. B. et al. Combined lifestyle factors, all-cause mortality and cardiovascular disease: A systematic review and meta-analysis of prospective cohort studies. J. Epidemiol. Community Health 75, 92–99 (2021).
Ganna, A. & Ingelsson, E. 5 year mortality predictors in 498,103 UK Biobank participants: A prospective population-based study. The Lancet 386, 533–540 (2015).
Etter, J. F., le Houezec, J. & Perneger, T. V. A self-administered questionnaire to measure dependence on cigarettes: The cigarette dependence scale. Neuropsychopharmacology 28, 359–370 (2003).
Acknowledgements
The authors would like to thank all local collaborators in Prague, Havířov, Karviná, Jihlava, Ústí nad Labem, Liberec, Hradec Králové, Kroměříž, Novosibirsk, Krakow and Kaunas.
Funding
The authors have disclosed the receipt of the following financial support for the research, authorship and/or publication of this article: the HAPIEE study was funded by the Welcome Trust (Grant WT064947 and WT081081), the US National Institute of Aging (Grant R01 AG23522) and the MacArthur Foundation. Contribution of Polish authors was supported by the Grant of Polish National Science Centre (Grant 2018/29/B/NZ7/02118). Contribution of Russian authors was supported by Russian Academy of Science, State assignment (AAAA-A17-117112850280-2). The present analyses were supported by the European Union’s Horizon 2020 Research and Innovation Programme projects CETOCOEN Excellence (Grant Agreement 857560), R-Exposome Chair (Grant Agreement 857487) and the National Institute for Research of Metabolic and Cardiovascular Disease project (Programme EXCELES, ID Project LX22NPO5104) funded by the Next Generation EU.
Author information
Authors and Affiliations
Contributions
T.S., H.P. and M.B. (guarantors of the paper) codesigned the paper. T.S. and H.P. performed the statistical analyses. M.B., N.C., A.P., S.M. and A.T. jointly designed the HAPIEE study. T.S. wrote the first draft and finalised the paper. All co-authors provided comments.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sarycheva, T., Capkova, N., Pająk, A. et al. All-cause and cardiovascular mortality in relation to lung function in the full range of distribution across four Eastern European cohorts. Sci Rep 12, 12959 (2022). https://doi.org/10.1038/s41598-022-17261-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17261-5
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.