Abstract
Transfusion-associated circulatory overload (TACO) is the leading cause of transfusion related morbidity and mortality. The only treatment is empirical use of furosemide. Our aim was to investigate if furosemide can prevent TACO. A randomized controlled trial was performed using a previously validated two-hit rat model for TACO. Volume incompliance was induced (first hit) in anemic, anesthetized Lewis rats. Rats were randomized to placebo, low-dose (5 mg kg−1) or high-dose (15 mg kg−1) furosemide-administered prior to transfusion (second-hit) and divided over two doses. Primary outcome was change in left-ventricular end-diastolic pressure (∆LVEDP) pre- compared to post-transfusion. Secondary outcomes included changes in preload, afterload, contractility and systemic vascular resistance, as well as pulmonary outcomes. Furosemide treated animals had a significantly lower ∆LVEDP compared to placebo (p = 0.041), a dose–response effect was observed. ∆LVEDP in placebo was median + 8.7 mmHg (IQR 5.9–11), + 3.9 (2.8–5.6) in the low-dose and 1.9 (− 0.6 to 5.6) in the high-dose group. The effect of furosemide became apparent after 15 min. While urine output was significantly higher in furosemide treated animals (p = 0.03), there were no significant changes in preload, afterload, contractility or systemic vascular resistance. Furosemide rapidly and dose-dependently decreases the rise in hydrostatic pulmonary pressure following transfusion, essential for preventing TACO.
Similar content being viewed by others
Introduction
Transfusion-associated circulatory overload (TACO), occurring in up to five percent of transfused patients in the ICU, is the leading cause of major morbidity and mortality following transfusion1,2. Furosemide, a loop diuretic, is currently the only treatment available and its use is at best empirical.
TACO is hallmarked by hydrostatic pulmonary edema following transfusion, analogous to acute heart failure (AHF). Considering the similarities, treatment for AHF has been extrapolated to TACO, including diuretics as first-line therapy. However, increasing evidence suggests that TACO has a different etiology compared to conventional volume overload. First, TACO incidence decreased following institution of universal leukoreduction3 and up to a third of cases develop fever4,5, suggesting an immunological component. Furthermore, the incidence of TACO varies per blood product transfused, suggesting more than pure volume overload6. Finally, our previous rat study showed that hydrostatic pulmonary capillary pressure (Pcap) increased after a red blood cell (RBC) transfusion and not crystalloids7. In the ICU, RBC transfusion is associated with an increased Pcap and an increased mortality8. It is unclear why blood transfusion increases Pcap, and through what mechanisms cardiac performance and hemodynamics are altered aside from the volume infused.
Prophylactic use of furosemide to prevent TACO warrants further investigation since a lack of evidence precluded the latest meta-analysis to provide any recommendations9. The few studies investigating furosemide in the context of transfusion, were performed over 35 years ago. Moreover, whole blood was transfused, and patients included were young with severe anemia due to tropical infections and malnutrition10,11. A recent pilot RCT included 80 patients randomized to receive either 20 mg of furosemide or placebo prior to transfusion, leading up to a larger trial12. One case of TACO was reported in each arm. There are currently no pre-clinical data on furosemide in the transfusion setting and translational research is essential to guide further clinical studies.
The goal of this study was to assess the effect of furosemide on hydrostatic pulmonary capillary pressure. We hypothesize that furosemide prophylaxis will rapidly decrease Pcap, and that this effect is dose dependent.
Results
A total of 18 animals were included in one of three groups (n = 6) randomized to receive low-dose furosemide (5.0 mg kg−1), high-dose furosemide (15.0 mg kg−1) or placebo. Two rats died prior to randomization: one due to a hemorrhage from the left-internal mammary artery, damaged during thoracotomy and one due to acute cardiac failure following LAD ligation—both were replaced. Additionally, one animal was excluded and replaced post-randomization after autopsy failed to show an MI, thereby lacking a first hit.
Anemia and volume incompliance
Following isovolemic anemia, hematocrit fell from 42.5 (IQR 39–43) to 31.0 (IQR 29–30.8; p = 2.04 × 10–4). Cardiac function decreased following MI: stroke work decreased by − 1462 (IQR − 2590 to 247.7; p = 0.038) and − dP/dt, diastolic relaxation rate, slowed by + 1313 (IQR 271–1827; p = 2.81 × 10–3). Ejection fraction was not a reliable variable due to conformational changes of the ventricle following LAD ligation. The MI volume, as surrogate measure of first hit severity, was comparable between groups (Table 1).
Effect of furosemide on hydrostatic pulmonary capillary pressure
Furosemide treatment resulted in a significantly lower ∆LVEDP compared to placebo following transfusion (p = 0.041, Fig. 1). Rats that received furosemide (any dose) had a lower ∆LVEDP after 15 min, following two units of RBCs (p = 0.024), as well as after four units transfused (p = 0.041). Directly following transfusion ΔLVEDP was increased by + 8.7 mmHg (IQR 5.9–11.0) in the placebo group, + 3.9 (IQR 2.8–5.6) in the low-dose group and by + 1.9 (IQR − 0.6 to 5.6) in the high-dose group. At 60 min post-transfusion the furosemide treated group still had a lower LVEDP, though this was not significant (p = 0.103, Fig. 1B).
Effect of furosemide on LVEDP. (A) The change of LVEDP over the course of the transfusion is given per animal. Animals receiving the placebo group show the greatest increase in ΔLVEDP compared to low and high-dose furosemide. The decrease in LVEDP is dose-dependent and is apparent within 15-min. (B) The change of LVEDP over the course of the experiment. Animals receiving placebo have a greater increase in LVEDP post-transfusion and this remains higher through-out the follow-up period. ΔLVEDP difference between LVEDP at timepoint compared to baseline, Trx transfusion.
Effect of furosemide on preload, afterload, contractility, SVR and electrolytes
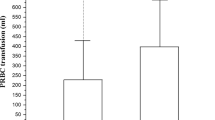
Preload was assessed by left-ventricular EDV, as well as surrogate markers including urine output, fluid balance, and CVP. Rats receiving furosemide had a significantly increased urine output (mL kg−1) compared to placebo (p = 9.70 × 10–4), with a dose–response relationship seen (Fig. 2A). Urine output between low-dose and high-dose furosemide was neither significantly different directly post-transfusion (p = 0.94), nor between groups comparing overall urine output (p = 0.59). While the volume of fluid infused was equal between groups (supplementary eTable 1), fluid balance was significantly lower due to a diuresis in rats receiving furosemide + 2.2 mL (IQR 1.2–3.0) versus + 5.2 mL (IQR 3.6–5.7, p = 0.013) in the placebo group. EDV did not differ significantly between placebo, low or high-dose furosemide post-transfusion (Table 2) or after 1-h follow-up (p = 0.372). Further post-hoc analyses of EDV when corrected for HR, LVEDP, SV or CO showed no significant difference. CVP was not different between groups (p = 0.738). There were no significant differences between group sodium and potassium concentrations. Only chloride concentrations were significantly lower in the furosemide treated groups (supplementary eTable 2, p < 0.01).
Afterload variables included MAP, LVPmax, systolic and diastolic blood pressure, all of which were not different between groups. SVR also did not differ between groups comparing pre- to post-transfusion and also not after a full hour of follow-up. Contractility reflected by RPP, stroke work, dP/dt and diastolic relaxation (− dP/dt) also did not differ between groups at any time-point.
Pulmonary outcomes
A higher P/F-ratio was seen in the high-dose group, though this did not reach significance (Fig. 2B). Wet-dry ratio did not differ between furosemide treatment and placebo groups 4.55 (IQR 4.54–4.79) versus 4.53 (IQR 4.42–4.73). Pathology scores were not significantly lower in the furosemide treated groups (p = 0.217).
Discussion
TACO is associated with severe morbidity and mortality and considering the number of transfusions, prevention of TACO is important. We evaluated prophylactic use of furosemide on Pcap in a rat transfusion model. The main findings of this study are (1) furosemide significantly reduces the Pcap increase caused by RBC transfusion; (2) there is a dose dependent, early non-diuretic effect of furosemide on LVEDP, apparent within 15 min following administration; (3) left-ventricular preload, afterload, contractility and SVR did not differ between groups.
Most knowledge concerning furosemide is based on AHF research. Since circulatory overload is triggered sooner after transfusion then following conventional fluids13, it is unclear whether furosemide would be comparably effective in TACO as in AHF. Furosemide’s actions are divided into an early non-diuretic effect and a natriuretic effect that persists for several hours. The early non-diuretic effect decreases Pcap in AHF prior to diuresis, as this effect persists in animal models when the ureters are ligated14,15. Supposedly this effect is the result of endothelial prostaglandin synthesis influencing vascular tone16, specifically vasodilation of the systemic circulation17. Prostaglandin synthesis inhibitors seem to abolish the early non-diuretic effect of furosemide18,19. The diuretic effect results from a blocking of the Na+-K+-2Cl− symporter (NKCC) in the kidney, leading to natriuresis and a decrease in circulating volume. However, NKCC is also located in the lungs on the membrane of alveolar type I and II cells, is involved in alveolar fluid secretion, and is sensitive to loop diuretics20. Blocking of the pulmonary NKCC may be an additional target to prevent additional pulmonary edema from forming.
The main finding of this study is that prophylactic use of furosemide significantly reduces the increase of ∆LVEDP following transfusion (Fig. 1). A low hydrostatic pressure by definition cannot result in hydrostatic pulmonary edema and TACO. Already at 15 min there was a dose-dependent LVEDP reduction, while there was no significant difference in urine output post-transfusion between low and high dose furosemide. This underlines that the early non-diuretic effect can blunt an increase in Pcap following transfusion, similar to the treatment of AHF17,21. This suggests that diuretic prophylaxis directly pre-transfusion may still be effective, while reducing circulating volume through diuresis requires time. Moreover, a lower dose of loop diuretics may already be sufficient in blunting a Pcap increase.
In a small survey, clinicians treatment goals in TACO differed from lowering circulating volume or decreasing preload to decreasing afterload22. Interestingly, there was no significant effect on preload (including CVP), afterload, contractility or systemic vascular resistance variables between groups. We hypothesize that an increased pulmonary venous capacitance explains why Pcap significantly decreases prior to a change in circulating volume. While Dikshit et al.17 demonstrated that furosemide increases systemic venous capacitance, our study specifically revealed no lowering of CVP in combination with a decreased EDV. The constant EDV could suggest a guaranteed preload by increased capacitance of the pulmonary capillary bed.
A mechanistic study in isolated dog lungs, showing a rapid increase of pulmonary blood flow following furosemide suggests a decreased pulmonary vascular resistance (PVR) which supports our hypothesis23. Unfortunately, PVR is difficult to measure in-vivo in rats, as it requires a pulmonary artery catheter. An increased pulmonary capillary capacitance would increase total pulmonary blood volume (PBV). Seemingly contradicting evidence includes a decrease in PBV shown measured by transpulmonary thermodilution24, however this method cannot specifically estimate volumes of different compartments. While our model measured lung wet-weight, this was after exsanguination and can therefore not be used to approximate PBV.
While our study has several strong points, there are a number of limitations. First, the total urine output was not significantly different, while the ΔLVEDP was different between low and high-dose furosemide. In our experiment the diuretic effect might already be near maximal at low-dose, explaining the lack of difference in urine output, while the early non-diuretic effects increase with increasing dose. Furthermore, while investigators were blinded to treatment groups, they could not be blinded for urine output. We minimized bias by not allowing any adjustments to fluid infusion, vasopressors or ventilatory parameters following randomization, which limited the possible follow-up duration of the experiment. Electrolyte fluctuations were not clinically relevant in this animal model however, due to the duration of follow-up might not have become clinically relevant yet. Baseline electrolyte disturbances in critically ill patients can potentially further derail and have deleterious consequences. Finally, the experiment included healthy rats with intact kidney function. Whether the early non-diuretic effect is equally effective in reducing Pcap when renal function is impaired, and if dosage changes are required, remains to be determined.
Our results should encourage human trials that assess the preventive effect of furosemide in the context of TACO. So far, prophylactic furosemide is employed in up to 30% of patients transfused2,25. If proven beneficial, then more widespread prophylaxis could curb the incidence of TACO. Considering the pharmacodynamics of furosemide, the prophylactic effects likely carry-over in the post-transfusion period. Aside from prevention, its role in the treatment of TACO should be investigated. Additional research is required as to how renal function impacts the effect of furosemide prophylaxis, since renal insufficiency is a major risk factor for TACO and influences furosemide’s effectiveness. Based on this study the low-dose already showed significant reduction in LVEDP, therefore high-dose furosemide might not be required in patients.
In conclusion, our randomized controlled rat study, the prophylactic use of furosemide successfully and rapidly limited the increase in Pcap following transfusion. The effect on Pcap showed a dose–response relationship to furosemide administration.
Methods
Animal experiments were approved by the Dutch national committee for animal experiments (Centrale Commissie Dierproeven-The Hague, The Netherlands) under license: AVD118002017814. Experiments were separately approved by the center’s animal ethical committee (Dier Ethische Commissie, Academisch Medische Centrum-Amsterdam, The Netherlands). Experiments were in accordance with The Guide for the Care and Use of Laboratory Animals26. Results are reported according to the ARRIVE 2.0 guidelines.
Animal protocol
A validated and previously published rat model for TACO was used7. Male adult Lewis rats (LEW/SsNHsd, Envigo-USA) weighing 300–360 g, were used after a 7-day minimum acclimatization period. General anesthesia was induced by placing animals in a container with 5% isoflurane. After loss of consciousness, a mixture of ketamine (9.0 mg/100 g), dexmedetomidine (12.5 mg/100 g) and atropine (5 mg/100 g) was administered intraperitoneally. A continuous infusion of ketamine (5 mg/100 g h−1) was used for maintenance anesthesia over a tail-vein cannula. Rats were mechanically ventilated through a surgically placed tracheal cannula (Babylog 3000, Dräger-Germany). Pressure-controlled ventilation was used with tidal volumes of 6 mL kg−1 at 60 breaths min−1 (guided by PaCO2), and 3cmH2O positive end-expiratory pressure set. An ultraminiature pressure–volume (PV)-catheter (SPR-838, Millar-USA) was retrogradely advanced through the right carotid artery into the left ventricle. The left carotid artery was cannulated to measure arterial blood pressure and for blood sampling with blood gas analyses performed (RapidLab 500, Siemens-Germany). A left internal jugular catheter was placed to measure central venous pressure (CVP), administer furosemide or placebo and transfuse RBCs.
Isovolemic anemia was induced through a slow blood draw with 1:1 substitution of colloid (Tetraspan 6%, B. Braun-Germany). Substitution was continued until a hematocrit (Htc) of 30% was achieved. Animals were allowed to stabilize for the following 15 min.
A norepinephrine infusion was started targeting a mean arterial pressure (MAP) of 65 mmHg and a left-anterior thoracotomy was performed between the fourth and fifth rib. An acute MI was induced by ligation the left-anterior descending (LAD) coronary artery ± 2 mm below the left-atrium using a 5-0 Prolene suture. The MI was visually confirmed by blanching of the dependent flow territory and ST-elevations on a 3-lead ECG. A 20G chest tube was placed one rib below the incision and the thorax was closed in two layers. Following wound closure, a recruitment maneuver of five breaths at an inspiratory pressure of 25 cmH2O was performed and simultaneously the chest tube removed under negative pressure to maximize pulmonary expansion. Rats were allowed to stabilize over 30 min following the MI.
Randomization, blinding, intervention and transfusion
Randomization was performed after 30 min stabilization using the sealed-envelope method containing the number corresponding to a randomized syringe. Syringes used were identical, prepared under sterile conditions, prefilled prior to the start of the experiments with a similar volume of 600 μL and stored under dark conditions at 20 °C. Placebo syringes contained NaCl 0.9%, high-dose syringes were filled with furosemide 10 mg mL−1 (Centrafarm BV-The Netherlands) and low-dose syringes were filled with 200 μL of furosemide (10 mg mL−1) and 400 μL of NaCl 0.9%. The syringes were randomized using a random number sequence generator (www.random.org/sequences/—accessed March 2018) and stored in ascending numeric sequence guaranteeing a random order.
After randomization, no further adjustments were allowed concerning anesthetic, fluid or vasopressor infusion rates and ventilatory settings to limit confounding of hemodynamic and pulmonary outcomes. Investigators were blinded to the intervention, which was revealed after the inclusion ceased. All rats that completed the protocol were included. Rats that died prior to randomization were replaced. Additional syringes were prepared, and replacement syringes could be requested without loss of blinding.
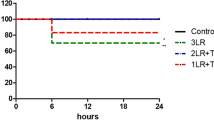
The furosemide doses were determined based on a previous rat studies, i.e. 5.0 mg kg−1 for low-dose and 15.0 mg kg−1 for high-dose27,28. Dosages correspond respectively to 40 mg and 120 mg (divided over two administrations) in an 80 kg human male. The total dose administered was calculated per animal based on baseline weight (150 μL/100 g). The total dose was spilt into two separate administrations (Fig. 3). At 30-min post-MI the first dose was given intravenously over two minutes, whereafter the transfusion was initiated. Two units were infused over fifteen minutes using a volumetric pump, subsequently hemodynamic measurements were recorded for one minute. The second dose was given over two minutes, and the remaining two RBC units transfused. The volume of one RBC unit was 1.0 mL and approximately 5% of circulating volume, analogous to humans assuming 6 L of blood and ± 300 mL of volume per RBC unit.
Experimental design. Rats under general anesthesia are made anemic. The first-hit is a myocardial infarction rendering rats volume incompliant. Randomization to placebo, low or high-dose furosemide is performed and prior to transfusion half of the product is administered. Subsequently two RBC units (2.0 mL) are transfused followed by a subsequent dose and transfusion of the remaining two units (2.0 mL). Rats are monitored up to 1 h post-transfusion. PV-catheter pressure–volume catheter, Art.line arterial line, CVC central venous cannula, Circ.vol circulating volume, LAD left-anterior descending coronary artery.
Following the transfusion phase, hemodynamic variables were collected for 60 min after which animals were terminated by exsanguination. Longer follow-up was not possible without changing ventilator settings or anesthetic, fluid and/or vasopressor infusion settings which would have induced bias.
Data and sample collection and processing
Hemodynamic measurements were averaged over one minute and PV-loop measurements were averaged from ten cardiac cycles. Measurements were performed at fixed-time points: at baseline, randomization (pre-transfusion), after the first half of transfusion (2 units of RBCs), immediately post-transfusion and after 60 min follow-up. Total urine output was calculated by weighing spontaneous diuresis, urine massaged from the bladder pre- and post-transfusion as well as to urine aspirated from the bladder during autopsy. Myocardial infarct volume was quantified according to previously published methods to confirm an MI and assess the severity of the first hit between groups7.
After termination the lungs were excised. The right upper lobe was examined by an experienced pathologist and rated on a 0 to 3-point scale of increasing pulmonary edema severity. The right lower lobe was weighed (wet-weight) and dried in a stove at 37 °C; dry-weight was determined when the weight no longer decreased after which the wet-dry weight ratio was calculated.
Preparation of transfusion products
Buffy coat reduced packed RBC units were prepared from whole blood, which was collected from animals outside of the experimental group. Whole blood was collected from healthy adult Lewis rats, anesthetized with isoflurane, through exsanguination via direct cardiac puncture. Whole blood from was collected in a 10:1 ratio with a citrate–phosphate-dextrose solution, pooled from multiple rats and centrifuged at 2000g for ten minutes. Under sterile conditions the plasma and buffy coat were removed. The red cell pellet was resuspended in a saline, adenine, glucose and mannitol solution (SAGM), where SAGM was added until a hematocrit of 60% was achieved. RBCs were used within 5 days and all rats in 1 week received a transfusion from this pooled product.
Outcomes and measurements
The primary outcome was the difference in ∆LVEDP (pre- to post-transfusion) between treatment groups. Secondary outcomes included ∆LVEDP comparing pre-transfusion to 60-min post-transfusion follow-up, urine output during and post-transfusion as well as electrolyte concentrations. Hemodynamic variables included HR, blood pressure, CVP and systemic vascular resistance (SVR). PV-variables included: left ventricular maximum pressure (LVPmax), end-diastolic volume (EDV), stroke volume (SV), cardiac output (CO), stroke work (calculated as area within the PV-loop) and rate-pressure product (beats/min LVPmax). Pulmonary outcomes included oxygenation capacity using PaO2/FiO2-ratio, wet-dry ratio to quantify pulmonary edema as well as a histopathology score.
Sample size calculation
The sample size was calculated to find a clinically relevant difference in Pcap between placebo and high-dose furosemide. A 4.0 mmHg decrease in LVEDP was deemed significant, similar to previous human studies29. Based on previously published results the placebo group was estimated to have a mean ∆LVEDP 8.0 ± 1.5 mmHg7. In order to detect a clinically relevant effect using a two-tailed alpha of 0.05 and 80% power, a group size of four was required. The group size was increased by 2 rats to correct for possible dropout.
Statistical analysis
Data were inspected for normality using histograms and was presented as mean ± SD or median (IQR) where appropriate. The Kruskal–Wallis test was used to compare ∆LVEDP between groups. The secondary outcomes including difference between furosemide treated groups versus placebo were compared using a Wilcox-signed rank test. Post-hoc analysis of EDVs were compared using a linear regression with step-wise correcting for the various covariates. Two-way testing was employed and results were considered significant with a p < 0.05, and in case of univariate linear regression with a p < 0.10.
Ethical approval
Animal experiments were approved by the Dutch national committee for animal experiments (license: AVD118002017814) and the center’s animal ethical committee. Experiments were in accordance with The Guide for the Care and Use of Laboratory Animals13, and reported according to the ARRIVE 2.0 guidelines.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AHF:
-
Acute heart failure
- BALF:
-
Bronchoalveolar lavage fluid
- CO:
-
Cardiac output
- CVP:
-
Central venous pressure
- dP/dt:
-
Maximum slope of left-ventricular pressure increase during systole
- − dP/dt:
-
Maximum slope of left-ventricular pressure decrease during diastole
- EDV:
-
(Left-ventricular) end-diastolic volume
- HR:
-
Heart rate
- LAD:
-
Left anterior descending (coronary artery)
- LVEDP:
-
Left-ventricular end-diastolic pressure
- LVPmax :
-
Maximum pressure generated by the left-ventricle
- MAP:
-
Mean arterial pressure
- MI:
-
Myocardial infarction
- PBV:
-
Pulmonary blood volume
- PVR:
-
Pulmonary vascular resistance
- P/F-ratio:
-
PaO2/FiO2 ratio
- RBC:
-
Red blood cells
- Pcap :
-
Hydrostatic pulmonary capillary pressure
- PV-(catheter):
-
Pressure–volume (catheter)
- RPP:
-
Rate pressure product (calculated as HR LVPmax)
- Stroke work:
-
Calculated as area with the pressure–volume loop (mmHg μL)
- SVR:
-
Systemic vascular resistance (calculated as (MAP-CVP) Cardiac index−1)
- TACO:
-
Transfusion-associated circulatory overload
- WD-ratio:
-
Pulmonary wet weight/dry weight ratio
References
Narick, C., Triulzi, D. J. & Yazer, M. H. Transfusion-associated circulatory overload after plasma transfusion. Transfusion 52(1), 160–165 (2012).
Roubinian, N. H. et al. Incidence and clinical characteristics of transfusion-associated circulatory overload using an active surveillance algorithm. Vox Sang. 112(1), 56–63 (2017).
Blumberg, N. et al. An association between decreased cardiopulmonary complications (transfusion-related acute lung injury and transfusion-associated circulatory overload) and implementation of universal leukoreduction of blood transfusions. Transfusion 50(12), 2738–2744 (2010).
Andrzejewski, C. Jr. et al. Hemotherapy bedside biovigilance involving vital sign values and characteristics of patients with suspected transfusion reactions associated with fluid challenges: Can some cases of transfusion-associated circulatory overload have proinflammatory aspects?. Transfusion 52(11), 2310–2320 (2012).
Parmar, N. et al. The association of fever with transfusion-associated circulatory overload. Vox Sang. 112(1), 70–78 (2017).
Bosboom, J. J. et al. Transfusion-associated circulatory overload: A clinical perspective. Transfus. Med. Rev. 33(2), 69–77 (2019).
Klanderman, R. et al. Both volume incompliance and transfusion are essential for transfusion-associated circulatory overload—a novel animal model. Transfusion 59(12), 3617–3627 (2019).
Cullison, M. et al. Blood transfusions, blood storage, and correlation with elevated pulmonary arterial pressures. Transfusion 59(4), 1259–1266 (2019).
Sarai, M. & Tejani, A. M. Loop diuretics for patients receiving blood transfusions. Cochrane Database Syst. Rev. 20, CD010138 (2015).
Gupta, S. P., Nand, N., Gupta, M. S. & Mohan, J. C. Haemodynamic changes following blood transfusion in cases of chronic severe anemia: Increased safety with simultaneous furosemide administration. Angiology 34(11), 699–704 (1983).
Nand, N., Gupta, S. P. & Gupta, M. S. Hemodynamic evaluation of blood transfusion in chronic severe anemia with special reference to speed of transfusion. Jpn. Hear. J. 26(5), 759–765 (1985).
Pendergrast, J. et al. Can furosemide prevent transfusion-associated circulatory overload? Results of a pilot, double-blind, randomized controlled trial. Transfusion 59, trf.15270 (2019).
Bosboom, J. J. et al. Incidence, risk factors, and outcome of transfusion-associated circulatory overload in a mixed intensive care unit population: A nested case–control study. Transfusion 58(2), 498–506 (2018).
Bourland, W., Day, D. & Williamson, H. The role of the kidney in the early nondiuretic action of furosemide to reduce elevated left atrial pressure in the hypervolemic dog. J. Pharmacol. Exp. Ther. 202(1), 221–229 (1977).
Sechi, L. A., Palomba, D. & Bartoli, E. Acute effects of furosemide on blood pressure in functionally anephric, volume-expanded rats. . Am. J. Nephrol. 13(2), 94–99 (1993).
Jhund, P. S., McMurray, J. J. V. & Davie, A. P. The acute vascular effects of frusemide in heart failure. Br. J. Clin. Pharmacol. 50, 9–13 (2000).
Dikshit, K. et al. Renal and extrarenal hemodynamic effects of furosemide in congestive heart failure after acute myocardial infarction. N. Engl. J. Med. 288(21), 1087–1090 (1973).
Patak, R. V. et al. Antagonism of the effects of furosemide by in domethacin in normal and hypertensive man. Prostaglandins 10(6), 649–659 (1975).
Pickkers, P. et al. Direct vascular effects of furosemide in humans. Circulation 96(6), 1847–1852 (1997).
Weidenfeld, S. & Kuebler, W. M. Cytokine-regulation of Na+-K+-Cl- cotransporter 1 and cystic fibrosis transmembrane conductance regulator-potential role in pulmonary inflammation and edema formation. Front. Immunol. 8, 393 (2017).
Biagi, R. W. & Bapat, B. N. Frusemide in acute pulmonary oedema. Lancet 1(7494), 849 (1967).
Klanderman, R. B. et al. Transfusion-associated circulatory overload: A survey among Dutch intensive care fellows. Transfus. Clin. Biol. 25(1), 19–25 (2018).
Ali, J., Unruh, H., Skoog, C. & Goldberg, H. S. The effect of lung edema on pulmonary vasoactivity of furosemide. J. Surg. Res. 35(5), 383–390 (1983).
Bhatia, M. L., Singh, I., Manchanda, S. C., Khanna, P. K. & Roy, S. B. Effect of frusemide on pulmonary blood volume. Br. Med. J. 2(5656), 551–552 (1969).
Lin, Y. et al. Transfusion-associated circulatory overload prevention: A retrospective observational study of diuretic use. Vox Sang. 113(4), 386–392 (2018).
National Research Council. Guide for the Care and Use of Laboratory Animals 8th edn. (The National Academies Press, 2011).
Leenen, F. H. Diuretic and cardiovascular effects of furosemide in rats. Can. J. Physiol. Pharmacol. 59, 1002–1007 (1981).
Hammarlund, M. M. & Paalzow, L. K. Dose-dependent pharmacokinetics of furosemide in the rat. Biopharm. Drug Dispos. 3(4), 345–359 (1982).
Nand, N., Gupta, M. S. & Sharma, M. Furosemide supplemented blood transfusion in cases of chronic severe anemia. Jpn. Hear. J. 27(2), 177–182 (1986).
Acknowledgements
The authors would like to thank Adrie Maas for his surgical expertise and key role in performing experiments.
Funding
Support was provided from departmental resources as well as support by a Landsteiner Foundation for Blood Research (LSBR) fellowship Grant to A.P.J. Vlaar, number 1931F. From the Landsteiner Foundation for Blood Transfusion Research, Haarlem—The Netherlands.
Author information
Authors and Affiliations
Contributions
R.K., M.H., B.G., L.V. and A.V. designed the study, R.K. and J.J. performed experiments. D.K., J.B. and R.B. contributed specialized knowledge and resources to the production and manufacturing of blood products. J.R. analyzed and interpreted histopathological data. The data was critically evaluated by R.K., D.P., M.H., M.V. and A.V. The manuscript was written by R.K., J.J., M.H., N.J., B.G. and A.V. and critically evaluated by all coauthors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Klanderman, R.B., Bosboom, J.J., Veelo, D.P. et al. Prophylactic furosemide to prevent transfusion-associated circulatory overload: a randomized controlled study in rats. Sci Rep 12, 12127 (2022). https://doi.org/10.1038/s41598-022-16465-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16465-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.