Abstract
This study aimed to review the clinical significance of BRAFV600E mutations in pediatric papillary thyroid carcinoma (PTC). From 2018 to 2021, 392 pediatric thyroid operations were performed in the first affiliated Hospital of Zhengzhou University. Of these, 169 patients underwent their first operation in our hospital and were histopathologically diagnosed as papillary thyroid carcinoma. BRAFV600E gene mutation detection was performed in these 169 pediatric patients to investigate the correlation between BRAF gene mutations and clinicopathological features. Ninety-seven of our 169 patients had a BRAFV600E mutation, with a mutation rate of 57.4%. The incidence of BRAFV600E was higher in boys than in girls, and in the 13–18-year age group as compared with the 6–12-year age group (P < 0.05). The positivity rate of BRAFV600E in unilateral PTC (67.7%) was significantly higher than the ones in bilateral PTC (28.9%). The occurrence of diffuse microcalcification of the thyroid negatively correlated with the presence of BRAFV600E mutations. BRAFV600E mutations were found more frequently in patients with smaller tumor size, a lack of multifocality, lower TSH levels and central lymph node metastasis. During the follow-up time, 70 patients were treated with iodine-131. Eight patients required a second surgery (All had cervical lymph node recurrence). BRAFV600E mutations do not suggest a more aggressive course in papillary thyroid carcinoma in pediatric patients in the short term.
Similar content being viewed by others
Introduction
The incidence of thyroid cancer in pediatric patients is significantly lower compare to adults, and there are significant differences between pediatric patients and adults in molecular pathology as well as in clinical manifestations1. Pediatric differentiated thyroid carcinomas include papillary thyroid carcinoma (PTC) and follicular thyroid carcinoma (FTC), of which PTC is the more common type. Unlike adult patients, PTC in pediatric patients is often asymptomatic, has a slow rate of growth and is hence more likely to present with advanced disease2. Children with PTC who present with multifocal, aggressive disease with invasion of blood vessels, the recurrent laryngeal nerve, trachea and esophagus have a poor prognosis3. Statistics show that the annual incidence of thyroid cancer in children and adolescents in China is approximately 0.44/100,000, and the mortality rate is 0.02/100,0004. Globally it has been found that the annual prevalence of thyroid cancer in adolescents is increasing5,6. Therefore, early diagnosis of PTC is the key to improving its prognosis. It is well known that BRAFV600E mutation rates are high in adult thyroid cancer7,8. However, the use of BRAFV600E as a molecular marker in adolescent thyroid cancer remains controversial9,10,11. This might be due to the limited number of reported cases. In this study, we aimed to evaluate the correlation between BRAFV600E mutations and their clinicopathological significance in pediatric PTC cases.169 cases of pediatric PTC in which we studied is the largest number of cases reported so far. This study would be an interest to all whom dealing with pediatric thyroid cancer.
Patients and methods
Patients
The study protocol was approved by the first affiliated Hospital of Zhengzhou University ethics and scientific review board (2019-KY-0202). Written informed consent were obtained from all the childre’s legal guardians, and the participants of age 16 to 18 provided their own informed consent to participate in the study. We confirm that all methods were performed in accordance with the relevant guidelines and regulations. We included 169 children (40 males and 129 females), ranging in age from 6 to 18 years, who had received their first surgical treatment in our hospital and in whom postoperative histopathology showed papillary thyroid carcinoma. There was no history of radiation exposure in these patients. The following data were recorded in each patient: age, sex, tumor size, unilateral/bilateral involvement, presence/absence of diffuse microcalcification and multifocal, extrathyroidal extension, Tumor Nodes Metastasis (TNM) stage, Thyroid-Stimulating Hormone (TSH) level, treatment received, and findings on follow-up. All cases were diagnosed and managed in accordance with the 2015 American Thyroid Association (ATA) guidelines for the diagnosis and treatment of pediatric thyroid nodules and differentiated thyroid cancer12. All histologic slides were reviewed by two independent pathologists according to the 2010 American Joint Committee on Cancer (AJCC) Guidelines, Edition 7.
DNA extraction
The mutational analysis was performed on formalin-fixed, paraffin-embedded tumor tissue from the thyroid resection specimens. Three to six pieces of unstained section (10 μm thick) from the tumor were deparaffinized and macro-dissected. DNA was extracted using a Qiagen tissue DNA extraction kit according to the manufacturer’s protocol (QIAamp DNA FFPE Tissue Kit, QIAGEN, Germany).
Gene detection
BRAF exon 15 was amplified using a BRAF mutation detection kit. Briefly, 5 μL DNA was added to 35 μL of the amplification system. The upstream primer sequence of BRAF was 5′-ATGCTTGCTCTGATAGGAA-3′ while the downstream primer sequence was 5′-GCATCTCAGGGCCAAA-3′. Polymerase Chain Reaction (PCR) amplification was then performed. The amplification conditions were as follows: pre-denaturation at 95 °C for 15 min; then denaturation at 94 °C for 30 s; annealing at 54 °C for 20 s; extension at 72 °C for 30 s for 35 cycles, the last 72 °C extension being for 10 min. BRAF amplification products were purified and sequenced by the BigDye® Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems, USA). Each sample was tested at least three times to ensure the repeatability of sequencing results.
Statistical analysis
The Chi-square test was used to assess whether BRAFV600E mutations were associated with age, sex, unilateral/bilateral involvement, presence/absence of diffuse microcalcification and extrathyroidal extension, multifocal/unifocal involvement, TNM stage, TSH level, treatment, and findings on short-term follow-up. Student’s t test and Mann–Whitney test were used appropriately for continuous numerical data, after applying the Shapiro–Wilk test for normality. Continuous data were summarized as median and range or mean ± standard deviation. All statistical calculations were performed using the SPSS Statistics 22.0 (IBM Inc., Armonk, New York, USA). A P value of < 0.05 was considered statistically significant.
Results
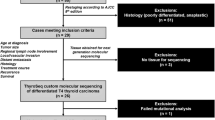
From 2018 to 2021, 40,799 thyroid operations were performed in the First Affiliated Hospital of Zhengzhou University. Of these, there were 392 patients aged 0–18 years of which 169 patients were diagnosed as PTC and underwent their first surgery at our hospital. The flow diagram for the inclusion of patients in this study is given in Fig. 1.
In the Table 1, 97 of our 169 patients had a BRAFV600E mutation, with a mutation rate of 57.4%. The rate of BRAFV600E mutation in males (72.5%) was higher than that in females (52.7%) and this difference was statistically significant (P = 0.027). The BRAFV600E mutation rate was higher in children aged 13–18 years as compared with those aged 6–12 years (P < 0.05). Similarly, the mutation rate of BRAFV600E in children with unilateral papillary thyroid carcinoma was significantly higher than that in children with bilateral papillary thyroid carcinoma (P < 0.05). BRAFV600E mutation rate of children with diffuse microcalcification on ultrasonography was significantly lower than that of children without diffuse microcalcification (P < 0.05). For tumor size, the maximum tumor diameter of children with BRAFV600E mutations was smaller than that of those without the mutation. The mutation rate of BRAFV600E in children with multifocal involvement was lower than that in those with unifocal involvement. There was no significant difference in the rate of BRAFV600E mutation in patients with or without extrathyroidal extension. The TSH values in those with BRAFV600E mutations were significantly lower than those without and this difference was statistically significant (P < 0.05). In terms of TNM staging, 45 cases with central node metastasis (72.6%) had BRAFV600E mutations, whereas 38 cases with lateral neck node metastasis (43.7%) had BRAFV600E mutations and this difference was statistically significant. There were five cases of lung metastasis, two of whom had BRAFV600E mutations (40%). Of the remaining 164 patients without lung metastasis, 95 had BRAFV600E mutations (57.9%). The presence of BRAFV600E mutations correlated with central node metastasis, and this correlation was statistically significant. Hence, BRAFV600E mutations did not suggest a more aggressive behavior of papillary thyroid carcinoma in pediatric patients.
In the Table 2, we studied the association between diffuse microcalcification (which is an image showing in Fig. 2) and extra-thyroidal extension, and TNM staging. There was no signifcant difference in the number of patients with extrathyroidal extension with or without diffuse microcalcification. However, we found that diffuse microcalcification has different incidence in different T stages, which was statistically significant.And diffuse microcalcification correlated positively with lateral neck node metastasis and this was correlation statistically significant.
Until the date of publication, the retrospective study of the outcomes in 169 cases follow-up was conducted, patients were followed up for at least 1 month (19 (10, 31) months, range 1–48 months). (Table 3). It was found that 41 cases (58.6%) without BRAFV600E mutations required treatment with iodine-131 as compared with 29 cases (41.4%) with BRAFV600E mutations, and this difference was statistically significant. Eight patients required a second surgery. All had cervical lymph node recurrence. Only two of these eight patients (25%) had BRAFV600E mutations.
Discussion
Most studies on the correlation between BRAFV600E mutations and PTC have focused on adult patients. The frequency of BRAFV600E mutations in adults with PTC has been reported to be between 36 and 83%13,14,15,16. A recent meta-analysis in adults reported that BRAF mutations are positively associated with tumor aggressiveness14,17. In recent years, the incidence of PTC in pediatric patients has been found to be increasing. As compared with adult thyroid cancer, lymph node metastasis is more likely to occur and is more aggressive in pediatric thyroid cancer13. However, the prognosis is relatively good18,19. The mechanism underlying these differences is unclear. The role of BRAFV600E mutations in adult thyroid cancer is well established, and researchers have now begun to focus on BRAFV600E mutations in pediatric PTC. The incidence of BRAFV600E in pediatric thyroid cancers has been varied13,20,21. In our study, of 169 children with PTC, the mutation rate of BRAFV600E was 57.4%, which was different from previous reports15,22,23. This may be related to the large number of patients in our study.
We found that the incidence of BRAFV600E mutations in pediatric thyroid cancer was higher in the age group of 13–18 years. We also found that the rate of BRAFV600E mutations in males (72.5%) was higher than that in females (52.7%). Some studies have not found any correlation of BRAFV600E mutations with gender24. These differences may be related to race, region and sample size. The maximum tumor diameter of pediatric patients with BRAFV600E mutations was less than that of patients without BRAFV600E mutations. The mutation rate of BRAFV600E in patients with multifocal disease was lower than that in those with non-multifocal disease. There was no difference in the rate of BRAFV600E mutations in those with extra-glandular invasion as compared with those without, and this was consistent with previous studies25. This is in contrast to reports in adults with PTC where the presence of BRAFV600E mutations correlated significantly with extra-glandular invasion, tumor multifocality and tumor size14,15,17,26,27. BRAFV600E mutations were found in 45 patients (72.6%) with central lymph node metastasis and 38 cases (43.7%) of children with cervical lymph node metastasis, which was consistent with the findings of Japanese workers24,28. BRAFV600E positive rate was not significantly associated with distant metastasis in pediatric PTC, unlike studies in adult PTC27.
We maybe the first to study the relationship between diffuse microcalcification and extra-thyroidal extension, and TNM staging.In this study we found that the diffuse microcalcification correlated positively with lateral neck node metastasis and this was correlation statistically significant, which may be considered as a reference for preoperative prediction of lymph node metastasis.
Seventy children were treated with iodine-131. Of these, 29 (41.4%) had BRAFV600E mutations. Of the 99 patients not treated with iodine-13, BRAFV600E mutations were seen in 68.7%. Studies have shown that BRAFV600E mutations in adult PTC may be a predictor for the efficacy of iodine-13129. On follow-up of our patients, we found that eight patients with cervical lymph node recurrence underwent a second surgery. Only two of these eight patients had a BRAFV600E mutation. However, in adult PTC, BRAFV600E mutations were strongly associated with recurrence. The presence of a BRAFV600E mutation in adult patients was found to be an independent risk factor and was the single most important factor for prediction of recurrence and long-term prognosis. We were not able to study the prognostic value of BRAFV600E mutations in pediatric PTC because of the short period of follow-up in our patients. It is possible that the pathogenesis and mechanism of pediatric PTC are different from those of adult PTC and the role of BRAFV600E mutations may also be different. Our study analyzed the significance of diffuse micro-calcification in pediatric PTC for the first time. We found that it was positively correlated with cervical lymph node metastasis and this finding requires further study.
In conclusion, our study reports the largest number of pediatric PTC patients till date. We found the mutation rate of BRAFV600E in papillary thyroid carcinoma in pediatric patients to be lower than that in adults. BRAFV600E mutations do not seem to suggest a more aggressive course of papillary thyroid carcinoma in pediatric patients in the short term. Long-term follow-up of our patients is required to study the effect of BRAFV600E mutations on recurrence and survival. It may also be worthwhile to search for other molecular markers in pediatric PTC.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Ward, E. et al. Childhood and adolescent cancer statistics, 2014. CA Cancer J. Clin. 64(2), 83–103. https://doi.org/10.3322/caac.21219 (2014).
Mao, X. C. & Wang, K. J. Research progress of thyroid cancer in children and adolescent. Med. Recapitul. 23(8), 1552–1556. https://doi.org/10.3969/j.issn.1006-2084.201708.021 (2017).
Paulson, V. A., Rudzinski, E. R. & Hawkins, D. S. Thyroid cancer in the pediatric population. Genes (Basel) 10(9), 723. https://doi.org/10.3390/genes10090723 (2019).
Yang, L. et al. Analysis of incidence and mortality of thyroid cancer in China, 2010. Chin. J. Prev. Med. 48(8), 663–668. https://doi.org/10.3760/cma.j.issn.0253-9624.2014.08.003 (2014).
Pellegriti, G. et al. Worldwide increasing incidence of thyroid cancer: Update on epidemiology and risk factors. J. Cancer Epidemiol. 2013, 965212. https://doi.org/10.1155/2013/965212 (2013).
Qian, Z. J. et al. Pediatric thyroid cancer incidence and mortality trends in the United States, 1973–2013. JAMA Otolaryngol. Head Neck Surg. 145(7), 617–623. https://doi.org/10.1001/jamaoto.2019.0898 (2019).
Araque, K. A., Gubbi, S. & Klubo-Gwiezdzinska, J. Updates on the management of thyroid cancer. Horm. Metab. Res. 52(8), 562–577. https://doi.org/10.1055/a-1089-7870 (2020).
Luzón-Toro, B. et al. Influencers on thyroid cancer onset: Molecular genetic basis. Genes (Basel) 10(11), 913. https://doi.org/10.3390/genes10110913 (2019).
Penko, K. et al. BRAF mutations are uncommon in papillary thyroid cancer of young patients. Thyroid 15(4), 320–325. https://doi.org/10.1089/thy.2005.15.320 (2005).
Sassolas, G. et al. Oncogenic alterations in papillary thyroid cancers of young patients. Thyroid 22(1), 17–26. https://doi.org/10.1089/thy.2011.0215 (2012).
Onder, S. et al. Classic architecture with multicentricity and local recurrence, and absence of TERT promoter mutations are correlates of BRAF (V600E) harboring pediatric papillary thyroid carcinomas. Endocr. Pathol. 27(2), 153–161. https://doi.org/10.1007/s12022-016-9420-0 (2016).
Haugen, B. R. et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1), 1–133. https://doi.org/10.1089/thy.2015.0020 (2016).
Francis, G. L. et al. Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid 25(7), 716–759. https://doi.org/10.1089/thy.2014.0460 (2015).
Li, C. et al. BRAF V600E mutation and its association with clinicopathological features of papillary thyroid cancer: A meta-analysis. J. Clin. Endocrinol. Metab. 97(12), 4559–4570. https://doi.org/10.1210/jc.2012-2104 (2012).
Gertz, R. J. et al. Mutation in BRAF and other members of the MAPK pathway in papillary thyroid carcinoma in the pediatric population. Arch. Pathol. Lab. Med. 140(2), 134–139. https://doi.org/10.5858/arpa.2014-0612-OA (2016).
Crispo, F. et al. BRAF inhibitors in thyroid cancer: Clinical impact, mechanisms of resistance and future perspectives. Cancers (Basel) 11(9), 1388. https://doi.org/10.3390/cancers11091388 (2019).
Shi, C. et al. Clinicopathological features and prognosis of papillary thyroid microcarcinoma for surgery and relationships with the BRAFV600E mutational status and expression of angiogenic factors. PLoS ONE 11(12), e0167414. https://doi.org/10.1371/journal.pone.0167414 (2016).
Cordioli, M. I. et al. Are we really at the dawn of understanding sporadic pediatric thyroid carcinoma? Endocr. Relat. Cancer 22(6), R311–R324. https://doi.org/10.1530/ERC-15-0381 (2015).
Hogan, A. R. et al. Pediatric thyroid carcinoma: Incidence and outcomes in 1753 patients. J. Surg. Res. 156(1), 167–172. https://doi.org/10.1016/j.jss.2009.03.098 (2009).
Henke, L. E. et al. BRAF V600E mutational status in pediatric thyroid cancer. Pediatr. Blood Cancer 61(7), 1168–1172. https://doi.org/10.1002/pbc.24935 (2014).
Givens, D. J. et al. BRAF V600E does not predict aggressive features of pediatric papillary thyroid carcinoma. Laryngoscope 124(9), E389–E393. https://doi.org/10.1002/lary.24668 (2014).
Nikita, M. E. et al. Mutational analysis in pediatric thyroid cancer and correlations with age, ethnicity, and clinical presentation. Thyroid 26(2), 227–234. https://doi.org/10.1089/thy.2015.0401 (2016).
Yang, L. B. et al. The clinicopathological features of BRAF mutated papillary thyroid cancers in Chinese patients. Int. J. Endocrinol. 2015, 642046. https://doi.org/10.1155/2015/642046 (2015).
Iwadate, M. et al. The clinicopathological results of thyroid cancer with BRAFV600E mutation in the young population of Fukushima. J. Clin. Endocrinol. Metab. 105(12), E4328–E4336. https://doi.org/10.1210/clinem/dgaa573 (2020).
Zurnadzhy, L. et al. The BRAFV600E mutation is not a risk factor for more aggressive tumor behavior in radiogenic and sporadic papillary thyroid carcinoma at a young age. Cancers (Basel) 13(23), 6038. https://doi.org/10.3390/cancers13236038 (2021).
Lupi, C. et al. Association of BRAF V600E mutation with poor clinicopathological outcomes in 500 consecutive cases of papillary thyroid carcinoma. J. Clin. Endocrinol. Metab. 92(11), 4085–4090. https://doi.org/10.1210/jc.2007-1179 (2007).
Frasca, F. et al. BRAF(V600E) mutation and the biology of papillary thyroid cancer. Endocr. Relat. Cancer 15(1), 191–205. https://doi.org/10.1677/ERC-07-0212 (2008).
Oishi, N. et al. Frequent BRAF V600E and absence of TERT promoter mutations characterize sporadic pediatric papillary thyroid carcinomas in Japan. Endocr. Pathol. 28(2), 103–111. https://doi.org/10.1007/s12022-017-9470-y (2017).
Ge, J. et al. The BRAF V600E mutation is a predictor of the effect of radioiodine therapy in papillary thyroid cancer. J. Cancer 11(4), 932–939. https://doi.org/10.7150/jca.33105 (2020).
Author information
Authors and Affiliations
Contributions
Y.L. and Y.W. completed the thesis conception, inquiry and writing, and L.L. and X.Q. completed the thesis validation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Y., Wang, Y., Li, L. et al. The clinical significance of BRAFV600E mutations in pediatric papillary thyroid carcinomas. Sci Rep 12, 12674 (2022). https://doi.org/10.1038/s41598-022-16207-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16207-1
This article is cited by
-
Thyroid Nodules and Follicular Cell-Derived Thyroid Carcinomas in Children
Endocrine Pathology (2023)
-
Genetic alterations landscape in paediatric thyroid tumours and/or differentiated thyroid cancer: Systematic review
Reviews in Endocrine and Metabolic Disorders (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.