Abstract
Serum creatinine level (SCr) typically decreases during pregnancy due to physiologic glomerular hyperfiltration. Therefore, the clinical practice of estimated glomerular filtration rate (eGFR) based on SCr concentrations might be inapplicable to pregnant women with kidney disease since it does not take into account of the pregnancy-related biological changes. We integrated the Wonju Severance Christian Hospital (WSCH)-based findings and prior knowledge from big data to reveal the relationship between the abnormal but hidden SCr level and adverse pregnancy outcomes. We analyzed 4004 pregnant women who visited in WSCH. Adverse pregnancy outcomes included preterm birth, preeclampsia, fetal growth retardation, and intrauterine fetal demise. We categorized the pregnant women into four groups based on the gestational age (GA)-unadjusted raw distribution (Q1–4raw), and then GA-specific (Q1–4adj) SCr distribution. Linear regression analysis revealed that Q1-4adj groups had better predictive outcomes than the Q1–4raw groups. In logistic regression model, the Q1–4adj groups exhibited a robust non-linear U-shaped relationship with the risk of adverse pregnancy outcomes, compared to the Q1–4raw groups. The integrative analysis on SCr with respect to GA-specific distribution could be used to screen out pregnant women with a normal SCr coupled with a decreased renal function.
Similar content being viewed by others
Introduction
Pregnancy is known to cause physiological alterations, including blood volume expansion via increased cardiac output and decreased systemic vascular resistance1,2. Specifically, systemic vasodilation and glomerular hyperfiltration are normal hemodynamic adaptations in pregnancy1. As gestational age (GA) increases, the glomerular filtration rate (GFR) during pregnancy increases physiologically, and the serum creatinine level decreases3. The currently used GFR estimation formula based on blood creatinine concentrations cannot be accurately applied in pregnant women4,5.
The Modification of Diet in Renal Disease (MDRD) formula4, which estimates GFR using a combination of serum markers and clinical parameters, has become a standard clinical method to estimate renal function in patients with chronic kidney disease (CKD). The feasibility of using this formula in the pregnant population has not been well studied, and guidelines on application of the MDRD formula specifically exclude interpretation in pregnant women5,6. Hence, it can be interpreted as a normal reference range for pregnant women with abnormal kidney function because it does not reflect normal physiological changes during pregnancy5. This makes it difficult to diagnose early and provide proper treatment for complications that can affect both fetuses and mothers7.
The incidence of CKD increases with pregnancy at advanced maternal ages2. Women with renal disorders face several problems in pregnancy due to increased physiologic changes accompanying renal dysfunction, including risk for disease progression, the potential teratogenicity of medications, and the increased risk of complications such as preeclampsia and preterm delivery2,8,9,10. Therefore, it is important to accurately evaluate renal function during pregnancy11.
Pregnancy status in CKD patients is known to be related with adverse pregnancy outcomes, such as pre-eclampsia12 and premature delivery13,14. Pregnant women diagnosed with CKD were typically categorized into three groups based on the severity of kidney dysfunction: mild (SCr < 1.5 mg/dL), moderate (1.5–2.5 mg/dL), and severe (> 2.5 mg/dL)14. However, Smith et al.5 suggested that the sole application of SCr concentration or SCr-based equations tend to substantially underestimate renal function during pregnancy. The Torino-Cagliari Observational Study15 found that the risk of adverse pregnancy outcomes increases stepwise as CKD stage 1 transitions to stages 4–5. However, the risk of adverse pregnancy outcomes was not significantly different between pregnant CKD stage 1 patients and normal pregnant women5. Multidisciplinary expert groups in Seoul National University focused on GFR estimated by midterm SCr to identify the association between kidney function and adverse pregnancy outcomes9.
Our study had two main tasks. First, we integrated an automatic platform and a manual method to establish a dataset on pregnant women. The automatic work was performed by a laboratorian, a computer scientist, and a database administrator, and the manual task was performed by domain experts, including an obstetrician and a family medicine doctor. Second, we implemented prior knowledge16 to improve the predictive power of adverse pregnancy outcomes. Recently, Harel, Ray and their colleagues8,16 collected approximately 362,000 measurements of SCr levels from 243,534 women, and established the GA-specific distribution. In this study, we applied the previously validated findings to identify the association between kidney function and adverse pregnancy outcomes.
Results
Determination of SCr group based on the GA-specific SCr distribution
We analyzed 4004 pregnant women who visited Wonju Severance Christian Hospital (WSCH) during the study period. For the 4004 subjects, 10,126 measurements of SCr levels existed, indicating that a person had an average of 2.53 times of SCr evaluations. In most cases (n = 1942), the SCr was measured once; it was measured 23 times in two cases and 24 times in one case (Fig. 1). For patients with multiple SCr measurements, we used the maximum estimated value of SCr level.
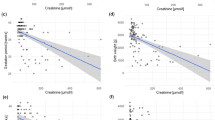
We used two methods for grouping all pregnancies based on the level of SCr (Fig. 2). At first, we divided SCr into four groups based on the 25th, 50th, and 75th percentile of SCr levels (Fig. 2A), thereby, 1097, 978, 955, and 974 subjects were evenly grouped into four raw groups by SCr levels [quartile (Q)1raw to Q4raw, respectively]. For the other method, we grouped all SCr results according to the distribution of GA-specific SCr levels, as proposed by Harel and colleagues16. In detail, we mapped our SCr results onto this distribution that includes GA and SCr levels as X and Y axes, respectively (Fig. 2B). As a result, 1,888, 813, 835, and 468 subjects were arranged into four groups [Q1adj (an adjusted group by GA-specific Scr distribution) to Q4adj, respectively].
Figure shows the two methods used to categorize the subjects into four groups based on the levels of serum creatinine (SCr). (A) Figure shows the distribution of our original or raw data. (B) Figure shows the abstract version of the distribution of gestational age-specific serum creatinine made by Harel et al16.
Medical and biochemical characteristics
General characteristics, including medical and biochemical data based on the four SCr groups determined by the GA-specific SCr distribution16 are summarized in Table 1. The average SCr levels showed a stepwise increase as it transitioned from the Q1adj to Q4adj group. The mean age was lowest in Q1adj group, but did not significantly differ among Q2adj to Q4adj groups (Table 1). The subjects in the Q4adj group had the following characteristics when compared to the Q1adj group: high ratio of multi-para, diabetes, preterm birth (PTB), preeclampsia, and fetal growth retardation (FGR) (Table 1).
Associational patterns of two grouping methods based on different SCr distributions with adverse pregnancy outcomes
The SCr groups stratified based on raw SCr distribution (Q1raw–Q4raw) could reflect the adverse pregnancy outcomes. In detail, the number of cases with two or more adverse pregnancy outcomes significantly increased from Q1raw to Q4raw. However, the ratio of cases with two or more number of adverse pregnancy outcomes increased gradually from Q1raw to Q3raw, but drastically from Q3raw to Q4raw (Fig. 3A). The four groups made by the GA-specific SCr distribution showed a more gradual pattern of increase in cases with an adverse pregnancy outcomes (Fig. 3B), compared to the original SCr distribution. For the cases with two or more adverse outcomes, two grouping methods showed a well-characterized stepwise increase pattern (Fig. 3A,B). In uni- or multivariate linear regression (LiR) with SCr group and the number of adverse pregnancy outcomes set as independent and dependent variables, the GA-specific SCr group had high beta-coefficients and low p-values, compared to the groups determined by the original SCr distribution (Fig. 3C).
Association between SCr groups and the number of adverse pregnancy outcomes. (A,B) Adverse pregnancy outcomes include preterm birth, preeclampsia, fetal growth retardation, and intrauterine fetal death; therefore, the maximum value of the number of pregnancy outcomes is four. (C) Y-axis indicates beta-coefficients obtained from linear regression with the number of adverse pregnancy outcomes and SCr groups (Q1–4raw or Q1–4adj) set as dependent and independent variables, respectively. Age, hypertension, diabetes, and parity types are covariates for multivariate models. *, **, *** indicate p value < 0.001, < 0.00001, < 0.0000001, respectively.
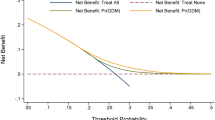
We re-grouped all subjects into two groups (with or without an adverse pregnancy outcomes), then conducted uni- or multivariate logistic regression (LR) considering the binary status (adverse pregnancy outcomes vs. control) and quartile group of SCr (Q1–Q4raw or Q1–Q4adj) as dependent and independent variables, respectively. Both original and GA-specific SCr distributions had non-linear U shaped associations with adverse pregnancy outcomes, but the results in Q3raw and Q4raw showed insignificant results (Fig. 4A). The GA-specific SCr groups showed a significant U-shaped relationship with the risk for adverse pregnancy outcomes (Fig. 4A). The relational pattern between SCr and PTB was similar with that of all types of adverse pregnancy outcomes (Fig. 4B). In cases of preeclampsia and FGR, the SCr level exhibited a monotonic increasing pattern of relationship (Fig. 4C,D). For intrauterine fetal demise (IUFD), Q1adj and Q4adj had a significantly increased risk (Fig. 4E).
Logistic regression. Q2raw and Q2adj were used as references in all models. Age, hypertension, diabetes, and parity types are covariates for multivariate models. Logistic regression method was used to reveal the relationship between main outcome and four groups based on serum creatinine measurements. Relationship of the four SCr groups with all types of adverse pregnancy outcomes (A), preterm birth (B), preeclampsia (C), fetal growth retardation (D), and intrauterine fetal demise (E) are illustrated.
Discussion
In this retrospective study, we identified that SCr level could predict the risk of adverse pregnancy outcomes as well as the number of co-occurred adverse pregnancy outcomes. Specifically, when using the GA-specific SCr distribution16, the predictive power of adverse pregnancy outcomes was more robust based on the beta-coefficients and their p-values, compared to the raw SCr distribution (Fig. 3). Moreover, we identified that SCr groups (Q1adj–Q4adj) determined by the GA-specific SCr distribution exhibited a non-linear U-shaped relationship with the risk of adverse pregnancy outcomes. Park et al.9 reported the convergent findings with our results that midterm GFR had a non-linear relationship with the adverse pregnancy outcomes.
Several studies have pinpointed that exclusively using SCr-based equations could result in the misclassification of kidney function during pregnancy5,16. To overcome this limitation, Park et al.9 only analyzed the midterm GFR values estimated based on SCr levels and their relationship with adverse pregnancy outcomes. Moreover, Harel et al.16 collected approximately 362,000 SCr results from about 240,000 women and generated the GA-specific SCr distribution. We could not find the GA-specific GFR distribution and could only obtain the GA-specific SCr distribution16, so we designed the linear regression or logistic regression models based on SCr levels, not GFR values. Direct application of the findings obtained from the Canadian population to the Korean pregnant women population may yield inaccurate results due to genetic and ethnic differences. However, we considered this distribution to be generalized, and not biased results because it was obtained from over 360,000 results16. In addition, it was obvious to provide an improved prediction of the adverse pregnancy outcomes of Korean women when using the Canadian-based distribution. Future studies to curate Korean-specific SCr distribution based on GA are needed. Moreover, it is crucial to establish the GA-specific GFR distribution.
SCr value is dependent on muscle mass or body composition, such as age, sex, and ethnicity17. Due to many factors adversely impacting the accurate estimation of GFR, Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend confirming CKD status in a specific population initially determined based on GFR estimated by SCr (eGFRCr) using an alternative method, such as GFR estimated by serum cystatin C (eGFRcys)18. Our study also focused on the inaccurate estimation of kidney function measured by SCr in a specific population (ie, pregnant women), and suggested that the combined information of SCr level and gestational age-specific SCr distribution16 could improve the prediction of adverse pregnancy outcomes. In pregnancy, albeit kidney hyperfiltration, the maternal serum level of cystatin C is known to be more stable than SCr before the third trimester19. Serum level of cystatin C is known to be elevated in the third trimester of pregnancy; however, its underlying mechanism is not converged19,20,21. In general population, cumulative evidence has supported that eGFRcys is a good alternative method for the GFR estimation, specifically in subgroup exhibiting low muscle amount: elderly population, vegetarians, and those with muscle wasting, chronic disease, or limb amputation22. Moreover, most studies commonly suggested that a combined creatinine and cystatin C equation proposed more accurate estimates and greater precision than GFR estimated from creatinine or cystatin C alone22,23. Taken together, we suggest that the kidney function of pregnant women is to be measured via multiple serum indices, such as creatinine and cystatin C.
Adverse pregnancy outcomes, such as preeclampsia and PTB, have been considered the leading causes of perinatal morbidity and mortality worldwide24,25. Therefore, establishing a prediction model for adverse pregnancy outcomes is crucial to help minimize adverse perinatal outcomes26,27. The establishment of the prediction model included two main tasks: one is the feature selection and the other is the optimization of parameters using several machine learning methods28. The present study focused on feature selection. Moreover, our results were obtained from previously validated findings16, also called prior knowledge, indicating that our study analyzed data based on the Bayesian approach or transfer learning29. Our findings indicated a non-linear relationship between SCr levels and adverse pregnancy outcomes; therefore, machine learning methods (e.g., support vector machine, random forest, or deep learning)30 that can deal with data exhibiting characteristics of the non-linear or complex relationships among features30 are needed to screen patients with high risk adverse pregnancy outcomes.
In the present study, multidisciplinary experts (i.e., laboratorian, database administrator, obstetrician, and computer scientist) performed multiple tasks to construct a database to identify the risk factors for adverse pregnancy outcomes. Initially, obstetricians are responsible for the literature-based review to select candidate features. Later, laboratorian, database administrator, and computer scientist constructed an initial dataset using the automatic platform, including the candidate variables. Then, the obstetrician and laboratorian manually updated the patient’s medical history and pregnancy outcomes.
This study has several limitations. First, because the WSCH is a tertiary hospital, the prevalence of pregnant women with adverse pregnancy outcomes is high compared to general population. To obtain generalized findings, the multi-institutional study or registry is needed, and this study could motivate the multi-center approach. Second, several biomarkers could not be analyzed since the database (e.g., electronic health records and automatic platform) is not designed to compile them. For example, we could not analyze data, such as body mass index (BMI) or waist circumference because they were not recorded at the time of initial pregnancy evaluation. Moreover, due to the retrospective design, we could not control the re-examination of blood tests of pregnant women, resulting that most women examined blood only had a time point of measurement (Fig. 1). Future study that is reinforced with these limitations could identify the valuable pathophysiological signatures related to decreased renal function and blunted hyperfiltration, and adverse pregnancy outcomes.
We implemented prior knowledge6 obtained from the enormously large scale of data and observed that elevated SCr levels were significantly related with the risk of adverse pregnancy outcomes. This study is a basic task of developing an algorithm to predict the possibility of adverse pregnancy outcomes based on the pregnant women's SCr levels adjusted by gestational weeks.
Methods
Data collection
We performed a retrospective study on pregnant women giving birth between January 2010 and December 2020 at the WSCH. Eligible subjects were women who had a singleton birth at more than 20 weeks gestation and were aged 16–50 years at the time of delivery. We constructed the initial dataset with the above criterion (i.e., 20 weeks and age) by database administrator as our previous work29. Afterward, we selected pregnancy cases based on patients’ case notes that had been manually recorded by the department of Obstetrics and Gynecology. We excluded pregnant women that did not have data for SCr levels and SCr measurement times.
The present study was approved by the Institutional Review Boards (IRB) of WSCH (CR321084). This study was conducted in accordance with the principles of the Declaration of Helsinki. The study was an observational study without medical intervention, so the need to obtain informed consent from patients was waived. The waiver of informed consent was also confirmed by the above IRB of WSCH (CR321084).
Adverse pregnancy outcomes
Several studies have analyzed the association between kidney function and adverse pregnancy outcomes8,16. Park et al.7 defined pregnancy outcomes as being adverse when a pregnant woman has one or more of the following: PTB, low birth weight, or preeclampsia. Harel et al.14 selected extreme PTB, preeclampsia, perinatal mortality, and severe FGR as the main adverse pregnancy outcomes. Motivated by these studies, we determined PTB (delivery before 37 weeks gestation), preeclampsia (blood pressure ≥ 140/90 with significant proteinuria and/or end organ damage), FGR (birthweight below 10th percentile adjusted for gestational age), and IUFD as adverse pregnancy outcomes.
Covariates
Harel et al.8 determined maternal age, rural residence, region of origin, gestational week, preconception SCr, chronic diseases (diabetes and hypertension), and tobacco/illicit drug (each ≤ years before conception) as covariates. Park et al.7 selected age, BMI, weight gain until delivery, hypertension, diabetes, hypertensive disorder during pregnancy, previous history of stillbirth/miscarriage, multiparity, and hospitalization status. Motivated by these studies, we categorized the parity type into two groups: nulliparity and multiparity. For underlying maternal diseases, hypertension and diabetes were included in this study, which were determined only by diagnosis code (i.e., ICD10) due to lack of data pertaining to blood pressure or serum fasting glucose at the time of SCr measurement. SCr measurement was performed using the Cobas® 8000 system (Cobas® c 702 and e 601 module; Roche Diagnostics, Switzerland).
Statistics
Continuous and categorical variables were analyzed according to the four groups categorized by the GA-specific SCr distribution16 using one-way analysis of variance (ANOVA) and Chi-square test, respectively. To test for linear trends of categorical or continuous variables, we determined the median SCr levels of each group as continuous variables in the Chi-square test and one-way ANOVA. All statistical analyses and graphic works were performed using R software (version 4.0.1, the R Foundation). A two-sided p value less than 0.05 was considered to indicate statistical significance for all analyses.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Cheung, K. L. & Lafayette, R. A. Renal physiology of pregnancy. Adv. Chronic Kidney Dis. 20, 209–214. https://doi.org/10.1053/j.ackd.2013.01.012 (2013).
Gonzalez Suarez, M. L., Kattah, A., Grande, J. P. & Garovic, V. Renal disorders in pregnancy: Core curriculum 2019. Am. J. Kidney Dis. 73, 119–130. https://doi.org/10.1053/j.ajkd.2018.06.006 (2019).
Wiles, K. et al. Serum creatinine in pregnancy: A systematic review. Kidney Int. Rep. 4, 408–419. https://doi.org/10.1016/j.ekir.2018.10.015 (2018).
Levey, A. S. et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 145, 247–254 (2006).
Smith, M. C., Moran, P., Ward, M. K. & Davison, J. M. Assessment of glomerular filtration rate during pregnancy using the MDRD formula. BJOG 115, 109–112. https://doi.org/10.1111/j.1471-0528.2007.01529.x (2008).
Maynard, S. E. & Thadhani, R. Pregnancy and the kidney. J. Am. Soc. Nephrol. 20, 14–22. https://doi.org/10.1681/asn.2008050493 (2009).
Webster, P., Lightstone, L., McKay, D. B. & Josephson, M. A. Pregnancy in chronic kidney disease and kidney transplantation. Kidney Int. 91, 1047–1056. https://doi.org/10.1016/j.kint.2016.10.045 (2017).
Harel, Z., Park, A. L. & Ray, J. G. Blunted glomerular hyperfiltration in pregnancy and risk of adverse perinatal outcomes. Am. J. Kidney Dis. 76, 297–299. https://doi.org/10.1053/j.ajkd.2020.02.437 (2020).
Park, S. et al. Midterm eGFR and adverse pregnancy outcomes: The clinical significance of gestational hyperfiltration. Clin. J. Am. Soc. Nephrol. 12, 1048–1056. https://doi.org/10.2215/cjn.12101116 (2017).
Hui, D. & Hladunewich, M. A. Chronic kidney disease and pregnancy. Obstet. Gynecol. 133, 1182–1194. https://doi.org/10.1097/aog.0000000000003256 (2019).
Lopes van Balen, V. A. et al. Maternal kidney function during pregnancy: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 54, 297–307. https://doi.org/10.1002/uog.20137 (2019).
Kristensen, J. H., Basit, S., Wohlfahrt, J., Damholt, M. B. & Boyd, H. A. Pre-eclampsia and risk of later kidney disease: Nationwide cohort study. BMJ 365, l1516. https://doi.org/10.1136/bmj.l1516 (2019).
Crump, C., Sundquist, J., Winkleby, M. A. & Sundquist, K. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: National cohort study. BMJ 365, l1346. https://doi.org/10.1136/bmj.l1346 (2019).
Vellanki, K. Pregnancy in chronic kidney disease. Adv. Chronic Kidney Dis. 20, 223–228. https://doi.org/10.1053/j.ackd.2013.02.001 (2013).
Piccoli, G. B. et al. Risk of adverse pregnancy outcomes in women with CKD. J. Am. Soc. Nephrol. 26, 2011–2022. https://doi.org/10.1681/asn.2014050459 (2015).
Harel, Z. et al. Serum creatinine levels before, during, and after pregnancy. JAMA 321, 205–207. https://doi.org/10.1001/jama.2018.17948 (2019).
Stevens, L. A., Coresh, J., Greene, T. & Levey, A. S. Assessing kidney function—Measured and estimated glomerular filtration rate. N. Engl. J. Med. 354, 2473–2483. https://doi.org/10.1056/NEJMra054415 (2006).
Summary of Recommendation Statements. Kidney Int. Suppl. 2011(3), 5–14. https://doi.org/10.1038/kisup.2012.77 (2013).
Saxena, A. R. et al. Correlation of cystatin-C with glomerular filtration rate by inulin clearance in pregnancy. Hypertens. Pregnancy 31, 22–30. https://doi.org/10.3109/10641955.2010.507845 (2012).
Strevens, H., Wide-Swensson, D., Torffvit, O. & Grubb, A. Serum cystatin C for assessment of glomerular filtration rate in pregnant and non-pregnant women. Indications of altered filtration process in pregnancy. Scand. J. Clin. Lab. Investig. 62, 141–147. https://doi.org/10.1080/003655102753611771 (2002).
Kristensen, K., Larsson, I. & Hansson, S. R. Increased cystatin C expression in the pre-eclamptic placenta. Mol. Hum. Reprod. 13, 189–195. https://doi.org/10.1093/molehr/gal111 (2007).
Levey, A. S., Fan, L., Eckfeldt, J. H. & Inker, L. A. Cystatin C for glomerular filtration rate estimation: Coming of age. Clin. Chem. 60, 916–919. https://doi.org/10.1373/clinchem.2014.225383 (2014).
Inker, L. A. et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 367, 20–29. https://doi.org/10.1056/NEJMoa1114248 (2012).
van Esch, J. J. A., van Heijst, A. F., de Haan, A. F. J. & van der Heijden, O. W. H. Early-onset preeclampsia is associated with perinatal mortality and severe neonatal morbidity. J. Matern. Fetal Neonatal. Med. 30, 2789–2794. https://doi.org/10.1080/14767058.2016.1263295 (2017).
Simmons, L. E., Rubens, C. E., Darmstadt, G. L. & Gravett, M. G. Preventing preterm birth and neonatal mortality: Exploring the epidemiology, causes, and interventions. Semin. Perinatol. 34, 408–415. https://doi.org/10.1053/j.semperi.2010.09.005 (2010).
Glover, A. V. & Manuck, T. A. Screening for spontaneous preterm birth and resultant therapies to reduce neonatal morbidity and mortality: A review. Semin. Fetal Neonatal. Med. 23, 126–132. https://doi.org/10.1016/j.siny.2017.11.007 (2018).
Serra, B. et al. A new model for screening for early-onset preeclampsia. Am. J. Obstet. Gynecol. 222(608), e601-608.e618. https://doi.org/10.1016/j.ajog.2020.01.020 (2020).
Lee, T. & Lee, H. Prediction of Alzheimer’s disease using blood gene expression data. Sci. Rep. 10, 3485. https://doi.org/10.1038/s41598-020-60595-1 (2020).
Hwang, S. et al. A deep neural network for estimating low-density lipoprotein cholesterol from electronic health records: Real-time routine clinical application. JMIR Med. Inform. 9, e29331. https://doi.org/10.2196/29331 (2021).
LeCun, Y., Bengio, Y. & Hinton, G. Deep learning. Nature 521, 436–444 (2015).
Author information
Authors and Affiliations
Contributions
Y.U.: conceptualization, investigation, analysis and interpretation; J.K. and S.H.: writing-original draft preparation; Y.U. and S.-J.C: writing-review and editing, supervision; J.K. and S.-J.C.: data collection and statistical analyses; S.H. and D.-M.S: data collection, verification and system application simulation; T.-S.L and S.H.: organization and design of materials; J.C: data review and analysis. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Case 1
A 35 years woman visited in the department of Obstetrics for the laboratory tests at initial pregnancy evaluation. She had no medical history such as hypertension, diabetes, and CKD. Her GA was 10 weeks and the SCr level was 26.5 μmol/L (0.3 mg/dL) which is within normal range. She measured SCr level at 18 week of GA, showing normal value of 61.9 μmol/L (0.7 mg/dL). We mapped her SCr levels onto GA-specific SCr distribution made by Harel et al.16, and found that the SCr levels were located in Q1 and Q4 (Fig.
Application of the gestational age-specific serum creatinine distribution16 in clinical setting.
5) indicating a high risk of decreased renal function or blunted hyperfiltration in 18 weeks. She finally exhibited two cases of adverse pregnancy outcomes, including PTB and FGR.
Case 2
A 28 years women visited WSCH for the laboratory tests at the first prenatal encounter. She had no medical history. Her GA was 28.86 weeks and the SCr was measured once and its level was 60.996 μmol/L (0.69 mg/dL) that is normal range. After mapping it onto the GA-specific SCr distribution16, it was located in Q4 (Fig. 5). She finally resulted three cases of adverse pregnancy outcomes, including PTB, preeclampsia, and FGR.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kang, J., Hwang, S., Lee, T.S. et al. Gestational age-specific serum creatinine can predict adverse pregnancy outcomes. Sci Rep 12, 11224 (2022). https://doi.org/10.1038/s41598-022-15450-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15450-w
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.