Abstract
Studies of microbiota reveal inter-relationships between the microbiomes of the gut and lungs. This relationship may influence the progression of lung disease, particularly in patients with cystic fibrosis (CF), who often experience extraoesophageal reflux (EOR). Despite identifying this relationship, it is not well characterised. Our hypothesis is that the gastric and lung microbiomes in CF are related, with the potential for aerodigestive pathophysiology. We evaluated gastric and sputum bacterial communities by culture and 16S rRNA gene sequencing in 13 CF patients. Impacts of varying levels of bile acids, pepsin and pH on patient isolates of Pseudomonas aeruginosa (Pa) were evaluated. Clonally related strains of Pa and NTM were identified in gastric and sputum samples from patients with symptoms of EOR. Bacterial diversity was more pronounced in sputa compared to gastric juice. Gastric and lung bile and pepsin levels were associated with Pa biofilm formation. Analysis of the aerodigestive microbiomes of CF patients with negative sputa indicates that the gut can be a reservoir of Pa and NTM. This combined with the CF patient’s symptoms of reflux and potential aspiration, highlights the possibility of communication between microorganisms of the gut and the lungs. This phenomenon merits further research.
Similar content being viewed by others
Introduction
Cystic fibrosis (CF) is the most common genetic condition affecting Caucasians1. Patients treated at specialist CF facilities show better survival rates, with effective care for lung disease a primary goal2. The advantages offered by specialist CF facilities are also linked to care across multiple disciplines, with significance attributed to treatment of gastro-intestinal issues. This includes gastro-oesophageal reflux (GOR), which occurs in around 50% of people with CF3. A number of causes for GOR in CF are suggested. These include a greater transient relaxation of the lower oesophageal sphincter (LOS), lower LOS pressure and delayed stomach emptying. It is also possible that physiotherapeutic interventions and coughing create a higher gradient of pressure in the abdomino-thoracic region4, leading to reflux. The functional importance of this includes the finding that people with CF who experience GOR tend to have poorer lung function5.
Microaspiration and potential gut to lung microbial movement has been shown in radiolabel studies of normal subjects6 and it is suggested that people with CF suffer a high burden of aspiration linked with reflux3. The stomach is sometimes considered a hostile environment which does not allow microbial pathogen survival. In fact however microbes can flexibly withstand extreme conditions, surviving high pH levels, digestive enzymes, strong detergent, and host immune reactions7.
We have previously described clonally related, CF relevant microbiology in gastric juice and sputum samples from people with CF, including Pseudomonas aeruginosa (Pa), and nontuberculosis mycobacteria (NTM) among other genera8,9. GOR is a major co-morbidity in CF and is associated with the presence of bile acids in the lungs most likely by micro-aspiration. The repeatability of our recently described “CF aerodigestive microbiome” has not been documented and there is limited understanding of how the GI environment interacts with microbiological isolates obtained from CF patients. Bile acids (BAs) have been observed within sputum, bronchoalveolar lavage (BAL) and end stage lung disease in people with CF, at concentration levels between 0.4 μM10 and 1 mM11,12,13. In vitro studies have found that bovine bile can lead Pa and a number of pathogenic species to take up biofilm modality14.
Therefore, it is important to further explore how the lung and GI environment might interact with microbiological survival and biofilm growth of patient microorganisms, which are known to be associated with morbidity and mortality in CF lung disease. The aim of this paper therefore is to determine whether our finding of gastric and lung microbiomes were repeatable in people with CF. Complimentary laboratory experimental studies on Pa isolates from CF patients were also performed to investigate Pa lifestyle in simulated aerodigestive environments and potential formation of biofilms.
Materials and methods
Patient cohorts
This study was approved by the Newcastle University Biobank and the Newcastle and North Tyneside 1 Research Ethics Committee. All study participants provided written informed consent prior to initiation of the study. All methods were carried out in accordance with relevant guidelines and regulations.
CF patients receiving percutaneous endoscopic gastrostomy (PEG) feeding represented an important opportunity to directly sample gastric juice, with less potential for contamination with oropharnygeal commensals. From the 270 CF patients attending the regional CF Centre, all adult stable CF patients receiving PEG tube feeding, were therefore included in this study; 13 patients who attended the clinic during the course of the study between 22/05/2013 and 17-04/2014 were studied. No PEG fed CF patients were excluded or positively selected for the study.
Patient samples and molecular based studies
Two sets of gastric juice and sputum samples were collected 6 months apart, (T1 and T2) from all (n = 13) available CF patients fed via percutaneous endoscopic gastrostomy (PEG) tube in our regional CF centre. Methods previously outlined9 were used to analyse gastric juice and sputum microbes. Bacterial profiling of the variable region 4 (V4) of the 16S rRNA gene was carried out by NU-OMICS (Northumbria University) based on the Schloss wet-lab MiSeq SOP15. Briefly, PCR was carried out using 1× Accuprime Pfx Supermix, 0.5 µM each primer and 1 µl of template DNA under the following conditions 95 °C 2 min, 30 cycles 95 °C 20 s, 55 °C 15 s, 72 °C 5 min with a final extension 72 °C 10 min. One positive and one negative control sample were included in each 96 well plate and carried through to sequencing. PCR products were normalised using SequalPrep™ Normalization kit (Invitrogen) as described in the manufacturer’s instructions and combined into four pools. Pools were combined in equimolar amounts to create a single library then denatured using 0.2 N NaOH for 5 min followed by a 2 min incubation at 96 °C. The library was diluted to a final concentration of 4.5 pM, supplemented with 5% PhiX and loaded onto a MiSeq V2 500 cycle cartridge, Each pool was quantified using fragment size determined by BioAnalyzer (Agilent Technologies) and concentration by Kappa qPCR (Kappa Biosystems).
Raw fastq files were processed using Mothur (v1.35.1) as described in the MiSeq SOP15. Sequences were aligned to the Silva database and chimeric sequences were detected by Chimera.uchime and removed from downstream analysis. OTUs were selected at a 97% similarity threshold and taxonomy was assigned using the Ribosomal database project 16S rRNA reference (v16) using a cut off value of 70 producing a total of 4,366,517 reads. The samples were subsampled using the sub.sample command in Mothur to 1000 reads per sample.
Pa and NTM strain typing
Strain typing was performed using methods previously outlined (13). All isolates were identified by matrix assisted laser desorption ionisation time-of-flight (MALDI-TOF) mass spectrometry (Bruker Daltonics, UK). Pa and mycobacteria were strain typed using variable number tandem repeat (VNTR) analysis, (Colindale, UK), independently of the author’s laboratories. For PA: amplification of 9 VNTR loci (ms61, ms172, ms207, ms209, ms211, ms213, ms214, ms217 and ms222)as described by Vu-Thien et al.16 and Onteniente et al.17. Mycobacterium was identified by rpoB, sodA and hsp65 gene sequencing and strain typed using amplification of 9 VNTR loci (3416, 4356, 3163, 4038, 4093, 3320,2177,3398, 2220) for variable number repeat analysis (VNTR), Colindale, UK18,19.
Whole genome sequencing (WGS)
In 2 patients, where clonally related Pa was identified in gastric juice and lung samples, WGS was used to confirm the close relationship between the isolates. In brief DNA was extracted from selected isolates using the QIAGEN PowerLyzer Power soil kit. Libraries were prepared from 1 ng of extracted DNA using the Nextera XT kit (Illumina) and sequenced by NU-OMICs using the V2 500 cycle reagent kit on the MiSeq benchtop sequencer.
The forward and reverse reads were checked for quality using FastQC and trimmed using Trimmomatic (v0.38.1) to remove any remaining Nextera adapter sequences and a sliding window of Q20 across 4 bp. The trimmed sequences were used for assembly using SPAdes (v3.12.0) with careful correction enabled and kmer detection of 21, 33, 55 and contigs less than 1000 bp were removed. The quality of assemblies was assessed using QUAST (v4.4) and CheckM (v1.0.18) (Supplementary Table S1). The assembles were corrected in Mauve using the Move contigs algorithm with Pseudomonas aeruginosa C-NN2 (Accession NZ_LT883143) identified as an appropriate reference from VNTR typing. The Average Nucleotide Identity (ANI) between draft genomes from each of the isolates from the same patient were generated using ANI Calculator with a minimum contig length of 1000 bp20,21 and window size of 1000 bp and a step size of 200 bp (Fig. 1).
The raw data for the 16S rRNA gene V4 amplicon sequencing and the genome assemblies is deposited to the NCBI BioSample database with accession numbers SAMN26565353–SAMN26565426 (https://www.ncbi.nlm.nih.gov/biosample/).
Symptoms of extra oesophageal reflux
Patient symptoms of extraoesophageal reflux (EOR) were assessed using the Reflux Symptoms Index (RSI) score. The RSI is a simple validated22, questionnaire consisting of nine questions regarding the symptoms of laryngopharyngeal reflux disease (LPRD), where the patient is asked to score from zero to five depending on the severity of the symptom. An RSI of > 13 is considered as abnormal22 (Supplementary Appendix 1).
Experimental evaluation of P. aeruginosa lifestyle in models of the human aerodigestive environment
Materials and chemicals
All reagents were obtained from Sigma-Aldrich, Poole, Dorset, UK. To reach pH targets ranging from 2.5 to 7.4, 1 Molar HCl was added to Phosphate-buffered saline (PBS), and this was then used to create porcine pepsin solutions of between 0.5 and 1.5 mg/ml. Four bile acids; lithocholic acid (LCA), cholic acid (CA), deoxycholic acid (DCA) and chenodeoxycholic acid (CDCA) were used ; from 0.3 to 20 mM/l, in line with gastric concentrations23,24, and from 9.4 to 150 µM/l, for lung informed by BAL measurements in people with CF10,11,12,13.
Strains of bacteria and cultures used
Pa strains Pa01, S33, S34 and Pa14 were used. S33 and S34 were isolated from 2 CF gastric juice samples9. Isolates reference Pa01 and Pa14 are from the International panel of Pa25. Columbia blood agar was used for subculturing the strains at 37 °C in the presence of oxygen until the next day.
Establishing effects of pepsin and acidity level on P. aeruginosa
A 10 µl Pa Inoculum was taken from a 0.5 McFarland standard Pa suspension (comparable density suspension 1.5 × 108 cfu/ml), pre-incubated with a 1 ml solution containing the test challenge substances, with 10 µl being taken at durations of 0 min, 5, 30, 60 and 120 min. These underwent dilution in 1.98 ml PBS, pH 7.4. 50 µl of the neutralised suspension of bacteria was taken for plating in blood agar, and this was done in triplicate, to give about 50–60 Pa colonies. Viable counts were determined after culturing at 37 °C for 24 h under aerobic conditions (Supplementary Appendix 2A).
Biofilm assay: microtiter-plate test
The biofilm assay used a standard microtiter plate assay using a crystal violet (cv) based staining protocol quantified by changes in optical density (Supplementary Appendix 2B). The cv staining method, originally described by O’Toole and Kolter in 1998 to identify biofilm-deficient mutants26, has become the clinical microbiology lab “gold standard” for quantifying biofilms in a microtitre dish. It is an inexpensive assay that can be routinely performed with relative ease27, can be used for both Gram-positive and Gram-negative organisms, and is suitable for qualitative and quantitative measurements of bacterial cells adherence to a variety of surfaces28. In spite of its popularity, the CV technique is an indirect measure of biofilm formation as it can measure adherence of bacterial cells that adhere to surfaces without forming biofilms29. These issues may contribute to a large variability between samples that may complicate the interpretation of biofilm screening results.
Statistical analysis
Bland and Altman plots were used to assess agreement between Shannon diversity measures at T1 and T2 of repeated samples. This methodology has been widely used to assesses agreement between repeated biological measures30,31.
Data were summarised graphically and statistically analysed via analysis of variance (ANOVA). The Siegal–Tukey test was employed for comparison of OD measurements from microtiter plate testing for samples containing bile and those which did not. The t-test was used for post hoc two-by-two comparisons to compliment the ANOVA approach. Statistical significance was assumed for all findings with a p value equal to or smaller than 0.05.
Results
CF patients and symptoms of extra oesophageal reflux (EOR)
The patients in this investigation, with a median age of 25 (range 18–32 year) demonstrated moderate to severe CF lung disease, common amongst the PEG-fed CF population (median forced expiratory volume in one second (FEV1) at T1, 1.65 l (38% predicted (compared to normal based on height, weight, and race) range 0.5–3.5 l (12–88%); median FEV1 at T2, 1.35 l (42% predicted) range 0.46–3.25 l (11–82%). They also showed low body mass index (BMI) (median at T1 19.4, range 15.2–23.2; median at T2 19.3, range 15.3–22.8). All were long term users of antibiotics (average use 70 days/year, range 14–197 at T1, and 79 days/year, range 14–190 at T2). All used acid suppressants and were EOR symptomatic; median RSI score 17 (range 13–36, n = 13). Table 1 contains the clinical details of the CF patients included in this study.
Comparing Pa isolated from gastric juice and sputum samples
Gastric juice and sputum samples from 13 CF patients (CF1–13) were taken on two separate occasions (T1 and T2) 6 months apart.
Pa were isolated from 2 out of 13 gastric juice samples (CF1 and CF11) at T1 and in 2 different patients at T2 (CF5 and CF8). In CF sputum samples, Pa were isolated from 9 CF patients at T1 (CF1, 5, 7–13) and from 5 CF patients at T2 (CF3, 8, 9, 11, 12).
Comparing the paired bacterial profile isolated from the gastric juice and sputum sample from the same patient showed that Pa were clonally related (confirmed by variable number tandem repeat (VNTR) between gastric juice and sputum samples in 2 patients (CF1 and 11) at T1 and in 1 patient at T2 (CF8) (Tables 2, 3).
Whole genome sequencing
In two patients where clonally related Pa were identified in gastric juice and lung samples by VNTR (patients 1 and 11, T1) (Table 3). WGS was used to confirm this close relationship between the isolates. The mean ANI for these isolates was 99.99% for patient 1 and 99.98% for patient 11. Figure 1 shows a representative illustration of the WGS data (patient 11, T1) showing a close relationship between the annotated genomes.
Comparing NTM in repeated gastric juice and sputum samples
Gastric juice and sputum samples from 13 CF patients (CF1–13) were taken on two separate occasions (T1 and T2) 6 months apart and compared for the presence of NTM. Cross sectional data at T2 have been previously published8.
Comparing the microbial profiles isolated from the gastric juice and sputum sample from the same patients showed that NTM were isolated among 5 different patients (Table 2).
At T1, only 2 patients had Mycobacteroides abscessus subsp. abscessus in their sputum (CF4 and 6), while at T2, a higher prevalence of NTM was detected compared to T1 with four out of 13 CF patients (four in their sputum and 2 of them had NTM in their gastric juice) having detectable NTM (CF 3, 4, 9, and 13).
Among those patients with sputum colonisation NTM at T2, 4 patients had NTM colonisation in their sputum, 3 patients with Mycobacteroides abscessus subsp. massiliense (CF3, CF9, CF13) and 1 with Mycobacteroides abscessus subsp. abscessus (CF4). Among the patients with sputum isolates, 2 had the same strain of NTM confirmed by VNTR in their gastric juice (M. massiliense in CF3 and CF13) (Tables 2, 4).
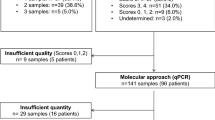
Bacterial profiles of repeated gastric juice and sputum microbiome samples based on 16S rRNA gene sequencing
There was insufficient sample for 3 patients. Ten paired sputa and gastric juice samples were therefore available for molecular analysis. The two patient sampling time points measured by alpha diversity and Shannon diversity index, showed biological variability. The CF sputum tended to have higher but not statistically significant microbial diversity at T2 (Fig. 2A). In comparison with sputum samples, the gastric juice samples showed less variation in alpha diversity between time points (Fig. 2A, Supplementary Fig. S1), Bland and Altman plots indicated greater fluctuations in the Shannon diversity index in sputum samples (Figs. 2C) compared to gastric juice samples (Figs. 2B, Supplementary Fig. S1). PERMANOVA analyses were used to compare bacterial profiles in CF gastric juice and sputa (Supplementary Fig. S2), this indicated that the centroids and spread of the profiles overlapped between the groups (p = 0.08).
(A) Alpha diversity (left) and Shannon diversity index (right) of repeated CF gastric juice (CFGJ) and CF sputum (CFS) samples at the two time points (T1 and T2, n = 10). (B) Bland Altman plot of the Shannon diversity index of gastric juice samples (n = 10) from CF patients at 2 time points (T1 and T2). The mean of the Shannon diversity of each subject (x-axis) is plotted against the differences between T1 and T2 (y-axis). Mean difference between T1 and T2 = 0.14 (SD 0.86). (C) Bland Altman plot of the Shannon diversity index sputum samples (n = 10) from CF patients at 2 time points (T1 and T2). The mean of the Shannon diversity of each subject (x-axis) is plotted against the differences between T1 and T2 (y-axis). Mean difference between T1 and T2 = 0.72 (SD 1.35).
Pa lifestyle in simulated aerodigestive environments
Experimental work investigating tolerance of acidity for the 4 strains of Pa in PBS and using pH conditions of 7.4 as a control with which to compare the results, show that below pH 4, a significant growth inhibition of Pa was achieved at 2 h (F (6,14) = 4.866, p < 0.001). This significant effect also appeared at lower pH values, with shorter incubation times. (Supplementary Fig. S3).
Effects of pepsin
Incubating Pa in PBS containing porcine pepsin at 0.5, 1 and 1.5 mg/ml, at a range of pH levels demonstrated that all 4 Pa strains were sensitive to proteolysis. At a pH level of 3, the samples displayed a large decrease in viable microbes (colony number), and the majority had not survived a 15 min incubation (Supplementary Fig. S4). There was also a complete loss of bacteria where pH was 3.5, and at 1 and 1.5 mg of porcine pepsin, all had been killed by 60 min’ incubation, whereas for 0.5 mg, this had been achieved by 120 min (Supplementary Fig. S5).
For samples incubated at pH 4, porcine pepsin had a lesser impact on Pa strains following 15-min. Approximately 15% of bacterial cells were killed at 15 min where pepsin was present, and 30% at 120 min. In the non-pepsin sample, just 12% were killed (Supplementary Fig. S6). There was no significant effect of pepsin on bacteria at pH 5 (F (3,16) = [1.906], p = 0.169) (Supplementary Fig. S7).
The impact of bile acids at concentrations found in gastric juice on Pa growth
Incubation of Pa with four different bile acids in concentrations from 0.3 to 20 mmol/l had a negative impact on growth, although there was variability between strains. Lithocholic acid reduced growth significantly (p < 0.05) in two of the strains of Pa (S33 and S34) at a 1.25 mmol/l concentration or above, while the remaining two strains were impacted when the concentration reached 5 mmol/l or above (F ((4, 16.64) = [6.659], (p = 0.002) (Fig. 3A). Incubation with DCA reduced growth significantly for two of the strains (S33 and S34), at the lowest concentration of 0.3 mmol/l, while for the remaining two strains, growth was reduced significantly (F (2,93) = [39.86], (p = 0.005) when DCA concentrations were over 1.25 mmol/l (Fig. 3B). Both CDCA (Fig. 3C) and CA (Fig. 3D) concentrations of over 2.5 mmol/l (F (7, 21) = [16.33], p = 0.009) and 5 mmol/l significantly (F (7,24) = [3.745], (p = 0.007) reduced the growth of Pa, respectively. There was therefore variability among different strains in term of bile tolerance.
The Impact of bile acids at concentrations found in gastric juice indicated increased formation of Pa biofilm, for each strain, at varying bile acids concentrations (Fig. 3E–H; increase in OD 570/600 values). Statistically significant increases in biofilm formation were observed at 20 mmol/l for all bile acids (F(2,18) = 6.576, p = 0.033) (Fig. 3E–H).
Impact of bile acids, at concentrations found in lung, on Pa growth and biofilm formation
When Pa was incubated with bile acid levels at CF lung relevant levels informed by BAL (9.4 µmol/l to 150 µmol/l), Pa growth was not altered (Fig. 4A–D). There was a significant increase (F (4,9.5) = [9.951], p = 0.007) in biofilm formation however (Fig. 4E–H), with variability in the strain response to bile acids. 9.951 (4.000, 9.477).
Discussion
Our study provides novel data repeatedly characterising gastric and lung microbiomes in people with CF. Pathogens including clonally related strains of Pa and NTM were isolated in gastric and lung samples from patients with symptoms of EOR, with variation over time. Exposure to bile and pepsin levels relevant to gastric and lung compartments were associated with Pa biofilm formation. It is likely that gastric juice Pa and NTM may derive from swallowed sputum containing Pa that is cleared from the lung following cough. However, We previously found that the digestive tract and airways were populated by bacteria which were sometimes related and of known importance in CF lung disease, including biofilm forming strains of Pa32,33. This highlights the possibility that the stomach could constitute a viable bacterial reservoir, relevant to the overall pathophysiology of CF. Our data indicate that although Gastric juice Pa may be swallowed following mucocilliary clearance of a diseased airway, Pa could also be derived through diverse routes and sources, including but not restricted to microaspiration for lung Pa. These findings may be relevant for detection, surveillance and eradication of organisms and suggests potential gut to lung transmission following aspiration, which warrants further study.
A relationship between aspiration of gastric contents during a reflux event and deterioration of lung function is implied by the finding of poorer lung function in CF patients with acid reflux5. Our study confirmed a high burden of gastrointestinal symptoms in people with CF34 and suggests that the connection between the airways and the stomach may be relevant to lung infection9,35. We propose that cough and other symptoms of EOR mean that a gastric reservoir could be relevant to transfer of organisms within and between patients. Cough aerosols, fomite transmission and EOR and aspiration represent potential mechanisms of transfer that could be investigated in future research.
There is increasing awareness that both the gut and lung microbiome may have an important role in overall CF pathophysiology, but there are limited numbers of studies36. In a previous paper from our group clonally related strains of Pa were identified in sputum and gastric juice in 4 people with CF9. Our present longitudinal follow up study confirmed that a closely related Pa was present in the sputum and gastric juice of some patients. Moreover, two patients had clonally related strains of M. massiliense in their sputum and gastric juice. Our present study builds on and strengthens our previous findings, using whole genome sequencing to confirm that Pa found in both gut and lung were closely related, confirming the VNTR results with a different analytical platform and analysis.
The swallowing of expectorated sputa is a normal homeostatic mechanism that could lead to the isolation of clonally related microorganisms in the gut and lung environments. Previous studies have also indicated the possibility of microflora exchange between the stomach and the lungs, in children with chronic cough37. It is of interest that previous radioisotope studies have shown that 50% of adult normal volunteers had gastric tracer in the lung following sleep, with the quantities of tracer aspirated ranging from 0.01 to 0.2 ml38. This order of magnitude was discussed as “likely to contain bacterial organisms in physiologically significant quantities”39. In our study Identification of patients who had gastric samples with NTM but who had negative sputa, indicate the possibility that NTM gastric isolates may be independent from respiratory sources.
Our description of an aerodigestive microbiome prompted us to perform complimentary laboratory based work that investigated the potential for lung and gastric environments to interact with microbes. We demonstrated a significant bactericidal impact for Pa in acidic conditions < pH 3 but at higher pH levels, the impact was small. When pepsin is present in acid conditions, Pa were more effectively destroyed. Other research into the impact of acidity on bacteria in Serratia marcescens are consistent with our findings40.
Thus, the effectiveness of the stomach’s bacterial barrier function varies with pH. The pH of the stomach can be modulated physiologically and with medication. Food entering the stomach, can contain bacteria and lower acidity, bringing pH to between 3 and 4.5. Pathogens which are bound to components of the food in the stomach find some protection from acidity in this way41. Pepsin concentration is a second element in bactericidal activity in the stomach, with effectiveness much more notable at levels > 1.0 mg/ml compared with 0.5 mg/ml in our data.
Gastric pH can also be altered by therapy. According to the United States CF Foundation Patient Registry, 70% of patients were treated with medication to block gastric acid, while Com et al. report up to 100% of patients are treated at some centres42. This is often for symptoms of GOR.
CF patients may also take acid inhibition medication to enhance the efficacy of pancreatic enzyme replacement therapy; a mainstay of modern CF patient care, associated with better life expectancy43,44. While generally considered a safe therapeutic approach, the role of ant-acid treatment and reflux in CF is an area of current debate45,46. Recent reviews and patient and public involvement identify this as an important research gap47.
We have previously accurately quantified the presence of lung bile acids in people with CF before and after lung transplant11,13. This prompted us to model the effect of bile acids on patient-derived organisms of the aerodigestive microbiome, complementing our work on pH and pepsin. At concentrations similar to those in the stomach, bile acids had a potential negative impact on Pa growth, with a tendency to form a biofilm. Interestingly there was variability between strains in this. Different, lab reference and clinically derived Pa strains were investigated, which seemed to have different responses to bile acids. This could be investigated further in future studies.
The behaviour of Pa was different when challenged with lower concentrations of bile acids, analogous to lung levels. Pa growth was unchanged, but a rise in biofilm formation was observed. The findings suggest the presence of bile acids within the lungs may be a significant environmental pressure on Pa phenotype. This could be a contributory factor to the decrease in lung function and morbidity observed in CF respiratory disease14,48. Our results support reports that a bovine bile concentration of 0.1–1 mmol/ml causes pathogenic microbes, including Pa, to move into a chronic infective14, biofilm form, with antibiotic resistance49. This process may be dependent on the production of pseudomonas quinolone signal (PQS), produced in the presence of bovine bile salts14,50.
We postulate that our findings may be particularly important if bacteria enter the lungs as a direct inoculum following gastric reflux and aspiration. It is possible that Pa in the stomach, converted to biofilm by the effect of high bile acid levels, is refluxed into the airways, where bile acids represent an ongoing environmental pressure to drive and maintain Pa biofilms. Pa entering the lung from sources other than the stomach may also be converted to biofilm by the effect of the low level of bile acid present in the airway environment.
Our study has limitations. Our descriptive, associative approach cannot prove gastric to lung transmission of organisms and although we collected samples from all available CF patients fed via PEG in our regional CF centre, we recognise this is a small number of patients. We made an informed choice to study PEG-fed patients to mitigate against the possibility of commensalism in our gastric microbiology. It could therefore be argued that our results may be limited to the PEG-fed population studied. Our study population had moderate to severe CF lung disease and may also have been at risk of NTM colonisation due to gastrostomy associated breach of barrier defence, which has been described in tuberculosis51.
The current study should stimulate further research into the mechanisms through which aspiration may lead to chronic inflammatory states and infections in CF. Further research into the relationship between the lung and stomach microbiomes could include extending the period of longitudinal follow up of CF patients. Patient derived isolates could also be grown within gastric fluid collected from people with CF, to determine how organisms may survive, through adaptation and biofilm formation. Such work could provide a novel route for developing new therapeutic interventions, which may also be relevant to other chronic lung diseases associated with reflux and aspiration52.
References
LiPuma, J. J. The changing microbial epidemiology in cystic fibrosis. Clin. Microbiol. Rev. 23, 299–323 (2010).
Mahadeva, R. et al. Clinical outcome in relation to care in centres specialising in cystic fibrosis: cross sectional studyCommentary: Management in paediatric and adult cystic fibrosis centres improves clinical outcome. BMJ 316, 1771–1775 (1998).
Blondeau, K. et al. Gastro-oesophageal reflux and aspiration of gastric contents in adult patients with cystic fibrosis. Gut 57, 1049–1055 (2008).
Pauwels, A. et al. Gastric emptying and different types of reflux in adult patients with cystic fibrosis. Aliment. Pharmacol. Ther. 34, 799–807 (2011).
Navarro, J. et al. Factors associated with poor pulmonary function: Cross-sectional analysis of data from the ERCF. Eur. Respir. J. 18, 298–305 (2001).
Gleeson, K., Maxwell, S. L. & Eggli, D. F. Quantitative aspiration during sleep in normal subjects. Chest 111, 1266–1272 (1997).
Sachs, G., Scott, D., Weeks, D. & Melchers, K. Gastric habitation by Helicobacter pylori: Insights into acid adaptation. J. Neurosci. 18, 8505–8514 (2000).
Al-Momani, H. et al. Nontuberculous mycobacteria in gastrostomy fed patients with cystic fibrosis. Sci. Rep. 7, 46546 (2017).
Al-Momani, H. et al. Microbiological profiles of sputum and gastric juice aspirates in Cystic Fibrosis patients. Sci. Rep. 6, 26985 (2016).
Pauwels, A. et al. Bile acids in sputum and increased airway inflammation in patients with cystic fibrosis. Chest J. 141, 1568–1574 (2012).
Aseeri, A. et al. Bile acids are present in the lower airways of people with cystic fibrosis. Am. J. Respir. Crit. Care Med. 185, 463–463 (2012).
D’Ovidio, F. et al. Bile acid aspiration and the development of bronchiolitis obliterans after lung transplantation. J. Thorac. Cardiovasc. Surg. 129, 1144–1152 (2005).
Brodlie, M. et al. Bile acid aspiration in people with cystic fibrosis before and after lung transplantation. Eur. Respir. J. 46, 1820 (2015).
Reen, F. J., Woods, D. F., Mooij, M. J., Adams, C. & O’Gara, F. Respiratory pathogens adopt a chronic lifestyle in response to bile. PLoS ONE 7, e45978 (2012).
Kozich, J. J., Westcott, S. L., Baxter, N. T., Highlander, S. K. & Schloss, P. D. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the MiSeq Illumina sequencing platform. Appl. Environ. Microbiol. 79, 5112–5120 (2013).
Vu-Thien, H. et al. Multiple-locus variable-number tandem-repeat analysis for longitudinal survey of sources of Pseudomonas aeruginosa infection in cystic fibrosis patients. J. Clin. Microbiol. 45, 3175–3183 (2007).
Onteniente, L., Brisse, S., Tassios, P. T. & Vergnaud, G. Evaluation of the polymorphisms associated with tandem repeats for Pseudomonas aeruginosa strain typing. J. Clin. Microbiol. 41, 4991–4997 (2003).
Harris, K. A. et al. Molecular fingerprinting of Mycobacterium abscessus strains in a cohort of paediatric Cystic Fibrosis patients. J. Clin. Microbiol. 50, 1758 (2012).
Turton, J. F. et al. Evaluation of a nine-locus variable-number tandem-repeat scheme for typing of Pseudomonas aeruginosa. Clin. Microbiol. Infect. 16, 1111–1116 (2010).
Rodriguez-R. L. M. & Konstantinidis, K. T. The Enveomics Collection: A Toolbox for Specialized Analyses of Microbial Genomes and Metagenomes. Report No. 2167–9843 (PeerJ Preprints, 2016).
Goris, J. et al. DNA–DNA hybridization values and their relationship to whole-genome sequence similarities. Int. J. Syst. Evol. Microbiol. 57, 81–91 (2007).
Belafsky, P. C., Postma, G. N. & Koufman, J. A. Validity and reliability of the reflux symptom index (RSI). J. Voice 16, 274–277 (2002).
Pearson, J. P. & Parikh, S. Review article: Nature and properties of gastro-oesophageal and extra-oesophageal refluxate. Aliment. Pharmacol. Ther. 33, 2–7 (2011).
Ali, M. S., Parikh, S., Chater, P. & Pearson, J. P. Bile acids in laryngopharyngeal refluxate: Will they enhance or attenuate the action of pepsin? Laryngoscope 123, 434–439 (2013).
De Soyza, A. et al. Developing an international Pseudomonas aeruginosa reference panel. Microbiologyopen 2, 1010–1023 (2013).
O’Toole, G. A. & Kolter, R. Flagellar and twitching motility are necessary for Pseudomonas aeruginosa biofilm development. Mol. Microbiol. 30, 295–304 (1998).
Haney, E. F., Trimble, M. J., Cheng, J. T., Vallé, Q. & Hancock, R. E. Critical assessment of methods to quantify biofilm growth and evaluate antibiofilm activity of host defence peptides. Biomolecules 8, 29 (2018).
O’Toole, G. A. Microtiter dish biofilm formation assay. JoVE 47, e2437 (2011).
Roy, R., Tiwari, M., Donelli, G. & Tiwari, V. Strategies for combating bacterial biofilms: A focus on anti-biofilm agents and their mechanisms of action. Virulence 9, 522–554 (2018).
Giavarina, D. Understanding bland altman analysis. Biochem. Med. 25, 141–151 (2015).
Myles, P. S. & Cui, J. Using the Bland–Altman method to measure agreement with repeated measures. 309–311 (Oxford University Press, 2007).
Al-Momani, H. et al. Microbiological profiles of sputum and gastric juice aspirates in cystic fibrosis patients. Sci. Rep. 6, 1–8 (2016).
Al-Momani, H. et al. Nontuberculous mycobacteria in gastrostomy fed patients with cystic fibrosis. Sci. Rep. 7, 1–7 (2017).
Zeybel, G. L. et al. Ivacaftor and symptoms of extra-oesophageal reflux in patients with cystic fibrosis and G551D mutation. J. Cyst. Fibros. 16, 124–131 (2017).
Rogers, G. B. et al. Use of 16S rRNA gene profiling by terminal restriction fragment length polymorphism analysis to compare bacterial communities in sputum and mouthwash samples from patients with cystic fibrosis. J. Clin. Microbiol. 44, 2601–2604 (2006).
Héry-Arnaud, G., Boutin, S., Cuthbertson, L., Elborn, S. J. & Tunney, M. M. The lung and gut microbiome: What has to be taken into consideration for cystic fibrosis? J. Cyst. Fibros. 18, 13 (2018).
Rosen, R. et al. 16S community profiling identifies proton pump inhibitor related differences in gastric, lung, and oropharyngeal microflora. J. Pediatr. 166, 917–923 (2015).
Althuwaybi, A. et al. A narrative review of the potential role of microaspiration and a dysregulated aerodigestive microbiome in lung disease. Ann. Esophagus. https://doi.org/10.21037/aoe-2020-ebmg-04 (2021).
Huxley, E. J., Viroslav, J., Gray, W. R. & Pierce, A. K. Pharyngeal aspiration in normal adults and patients with depressed consciousness. Am. J. Med. 64, 564–568 (1978).
Giannella, R., Broitman, S. & Zamcheck, N. Gastric acid barrier to ingested microorganisms in man: Studies in vivo and in vitro. Gut 13, 251–256 (1972).
Rosina, A. Rapid anterograde movement of the fluorescent tracer fast blue: A new method for tracing central connections. Neurosci. Lett. 33, 217–221 (1982).
Com, G., Cetin, N. & O’Brien, C. E. Complicated Clostridium difficile colitis in children with cystic fibrosis: Association with gastric acid suppression? J. Cyst. Fibros. 13, 37–42 (2014).
Littlewood, J. M., Wolfe, S. P. & Conway, S. P. Diagnosis and treatment of intestinal malabsorption in cystic fibrosis. Pediatr. Pulmonol. 41, 35–49 (2006).
Proesmans, M. & De Boeck, K. Omeprazole, a proton pump inhibitor, improves residual steatorrhoea in cystic fibrosis patients treated with high dose pancreatic enzymes. Eur. J. Pediatr. 162, 760–763 (2003).
van Horck, M. et al. Risk factors for lung disease progression in children with cystic fibrosis. Eur. Respir. J. 51, 1702509 (2018).
Al Momani, H. et al. Risk factors for lung disease progression in children with cystic fibrosis. Eur. Respir. J. 52, 1801492 (2018).
Rowbotham, N. J., Smith, S., Prayle, A. P., Robinson, K. A. & Smyth, A. R. Gaps in the evidence for treatment decisions in cystic fibrosis: A systematic review. Thorax 74, 229 (2018).
Reen, F. J. et al. Bile signalling promotes chronic respiratory infections and antibiotic tolerance. Sci. Rep. 6, 29768 (2016).
Stewart, P. S. & Costerton, J. W. Antibiotic resistance of bacteria in biofilms. The Lancet 358, 135–138 (2001).
Yang, L., Nilsson, M., Gjermansen, M., Givskov, M. & Tolker-Nielsen, T. Pyoverdine and PQS mediated subpopulation interactions involved in Pseudomonas aeruginosa biofilm formation. Mol. Microbiol. 74, 1380–1392 (2009).
Snider, D. E. Tuberculosis and gastrectomy. Chest 87, 414–415 (1985).
McDonnell, M. J. et al. Current therapies for gastro-oesophageal reflux in the setting of chronic lung disease: State of the art review. ERJ Open Res. 6, 00190 (2020).
Acknowledgements
H Al-momani received financial support from the faculty of medicine at The Jordanian Hashemite University. C Ward, J Pearson, SM Griffin and Rhys Jones were supported by a UK Government Technology Strategy Board Knowledge Transfer Partnership (Certificate No. KTP008821), between Newcastle University and Newcastle upon Tyne Hospitals NHS Foundation Trust. C Ward was supported by the Medical Research Foundation Grant MRF-091-0001-RG-GARNE. And an unrestricted research grant from Boehringer Ingelheim. M Brodlie supported by a Medical Research Council Clinician Scientist fellowship. This research was supported by a Venture and Innovation Award from the CF Trust. Grant reference No. VIA 099. We are very grateful to Dr Dervla Kenna, Public Health England, Colindale, London, U.K. for her expert independent work on VNTR isolate typing. We would also like to acknowledge the help of people with CF and their careers in our study.
Author information
Authors and Affiliations
Contributions
H.A. was responsible for the patient sampling. He analysed data and co-wrote the manuscript. A.P. was the Microbiology Biomedical Scientist for the study and co-wrote the manuscript. C.S., A.N. and S.C. were responsible for the NGS methodology, data analysis and co-wrote the manuscript. R.J., A.K., A.R., I.F. and M.G. were clinical gastrointestinal investigators. They recruited the non CF patients and performed endoscopy. They reviewed and contributed to manuscript drafts. S.B., S.D., A.A. and T.F. were responsible for the recruitment and clinical phenotyping of the CF patients. They co-wrote and/or reviewed the manuscript. M.B., M.W. co-wrote and reviewed the manuscript. J.P. and C.W. were lead investigators for the study, responsible for the study design. J.P. co-wrote the manuscript. Ward wrote the manuscript drafts.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al-Momani, H., Perry, A., Nelson, A. et al. Exposure to bile and gastric juice can impact the aerodigestive microbiome in people with cystic fibrosis. Sci Rep 12, 11114 (2022). https://doi.org/10.1038/s41598-022-15375-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15375-4
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.