Abstract
Insulin exerts positive inotropic effects on cardiac muscle; however, the relationship between cardiac contractility and phosphoinositol-3-kinase/Akt (PI3K/Akt) activation remains unclear. We hypothesized that the positive inotropic effects of insulin are dose-dependent and mediated via the PI3K/Akt pathway in isolated normal rat hearts. The Institutional Animal Investigation Committee approved the use of hearts excised from rats under pentobarbital anesthesia. The hearts were perfused at a constant pressure using the Langendorff technique. After stabilization (baseline), the hearts were randomly divided into the following four insulin (Ins) groups: 1) Ins0 (0 IU/L), 2) Ins0.5 (0.5 IU/L), 3) Ins5 (5 IU/L), and 4) Ins50 (50 IU/L) (n = 8 in each group). To clarify the role of the PI3K/Akt pathway in insulin-dependent inotropic effects, we also treated the insulin groups with the PI3K inhibitor wortmannin (InsW): 5) InsW0 (0 IU/L), 6) InsW0.5 (0.5 IU/L), 7) InsW5 (5 IU/L), and 8) InsW50 (50 IU/L). Hearts were perfused with Krebs–Henseleit buffer solution with or without wortmannin for 10 min, followed by 20 min perfusion with the solution containing each concentration of insulin. The data were recorded as the maximum left ventricular derivative of pressure development (LV dP/dt max). Myocardial p-Akt levels were measured at 3 min, 5 min, and at the end of the perfusion. In the Ins groups, LV dP/dt max in Ins5 and Ins50 increased by 14% and 48%, respectively, 3 min after insulin perfusion compared with the baseline. Tachyphylaxis was observed after 10 min in the Ins5 and Ins50 treatment groups. Wortmannin partially inhibited the positive inotropic effect of insulin; although insulin enhanced p-Akt levels at all time points compared with the control group, this increase was suppressed in the presence of wortmannin. The positive inotropic effect of insulin is dose-dependent and consistent with Akt activation. This effect mediated by high doses of insulin on cardiac tissue was temporary and caused tachyphylaxis, potentially triggered by Akt overactivation, which leads beta 1 deactivation.
Similar content being viewed by others
Introduction
Many inotropic agents, such as ephedrine, dopamine, and dobutamine1, exert dose-dependent, positive inotropic effects and are commonly used during surgery under general anesthesia2. Most of these agents stimulate beta receptors, leading to protein kinase A activation. However, they increase myocardial oxygen consumption, cause arrhythmia, and exert no cardioprotective effects. Therefore, the use of positive inotropic agents that exert their effects through other pathways would be better for anesthesia maintenance.
Insulin also exerts positive inotropic effects on cardiac muscle in animal models3,4,5. In addition, hemodynamic effects of high doses of insulin have been reported in healthy volunteers6. Insulin activates the phosphoinositol-3-kinase/Akt (PI3K/Akt) pathway and the substrates of Akt influence every aspect of cellular function, including growth, survival, proliferation, metabolism, glucose uptake, gene expression, and cell–cell communication by initiating the production of paracrine and autocrine factors7.
Insulin promotes utilization of glucose as the main cardiac energy substrate and can reduce coronary artery resistance and myocardial oxygen consumption, increase cardiac efficiency8, while Akt activates calcium handling9 and glucose uptake8. Therefore, the positive inotropic effect of insulin is believed to be mediated via the PI3K/Akt pathway. However, it is unknown whether cardiac contractility and Akt activation increase with insulin concentration. Therefore, we hypothesized that insulin could activate Akt in a dose-dependent manner to mediate its inotropic effects in the heart. In the present study, we assessed the relationship between insulin concentration and the inotropic effects mediated by the PI3K/Akt pathway in an isolated rat heart model, which allows testing the effect of different cardiovascular drugs on the coronary vasculature, muscle contraction, and heart rate (HR), without the interference of any other organ10.
Methods
The experimental protocol used in this study was reviewed and approved by the University of Yamanashi Animal Care Committee (Protocol number A26-19). All methods were carried out in accordance with the guidelines of the “Animal experiment rules in University of Yamanashi” established by the Animal experimentation facility, University of Yamanashi. The study was carried out in compliance with the ARRIVE guidelines.
Langendorff technique for isolated heart perfusion
Male Wistar rats (9 weeks old, 300–320 g) were anesthetized via intraperitoneal injection of 80 mg/kg pentobarbital sodium. The hearts were isolated and promptly immersed in cold modified Krebs–Henseleit (KH) buffer containing 118 mmol/L NaCl, 25 mmol/L NaHCO3, 4.7 mmol/L KCl, 1.2 mmol/L KH2PO4, 1.2 mmol/L MgSO4, 2.0 mmol/L CaCl2, 0.5 mmol/L di-NaEDTA, and 5.5 mmol/L glucose at 4 °C. The aorta was cannulated, and retrograde arterial perfusion was established at a constant pressure of 65 mm Hg with modified KH buffer. The KH solution was oxygenated with a mixture of 95% O2 and 5% CO2 and maintained at 37 °C. A small latex balloon was inserted into the left ventricle through the mitral valve and connected to a pressure transducer (TruWave, Edwards Lifesciences, CA, USA) to continuously monitor left ventricular (LV) pressure. The balloon volume was filled with water to maintain an LV end-diastolic pressure equivalent of 5–7 mmHg. A catheter was inserted into the pulmonary artery to collect the coronary venous return and measure the coronary flow.
Experimental protocol
Experiment 1
To investigate the dose-dependent positive inotropic effect of insulin, the HR and contractility of the isolated rat hearts were allowed to stabilize for 15 min to achieve stable hemodynamics, after which the hearts were randomly assigned to the following four groups (n = 8 for each group): 1) Insulin 0 IU/L (Ins0; Control), 2) Insulin 0.5 IU/L (Ins0.5), 3) Insulin 5 IU/L (Ins5), and 4) Insulin 50 IU/L (Ins50). The exclusion criteria were HR < 200 bpm, a maximum LV pressure derivative (LV dP/dt max) < 2000 mmHg/s, and multiple arrhythmias after 10 min of stabilization. The experimental design is illustrated in Fig. 1. Hearts were perfused with KH buffer for 10 min, followed by perfusion with the insulin solutions for 20 min. Baseline hemodynamics were recorded just before perfusion, with each concentration started at 0 min. Following perfusion, the whole rat hearts were quickly frozen in liquid nitrogen and freeze-dried for 6 days before measuring p-Akt in the myocardial muscle.
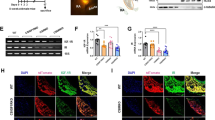
Experimental workflow for insulin perfusion in isolated rat hearts. In the insulin treatment (Ins) groups, hearts were perfused for 10 min with Krebs–Henseleit (KH) buffer containing 5.5 mmol/L glucose, followed by 20 min perfusion with each concentration of insulin (Experiment 1). In the insulin plus wortmannin treatment (InsW) groups, the hearts were perfused for 10 min with KH buffer containing 100 nmol/L wortmannin and 5.5 mmol/L glucose along with each concentration of insulin (Experiment 2). The hearts were then perfused for 20 min with a solution of each concentration of insulin and sampled for p-Akt measurement (Experiments 1 and 2). The HR and left ventricular derivative of pressure development (LV dP/dt) were measured 0, 3, 5, 10, 15, and 20 min after administration of each experimental perfusate, and the coronary effluent and partial pressure of oxygen were measured after 0, 5, 10, 15, and 20 min (Experiment 1 and 2). Whole heart muscles were sampled for p-Akt measurement at 3 and 5 min of insulin or control solution administration (Experiment 3).
Experiment 2
To clarify the role of the PI3K/Akt pathway in insulin-induced inotropic effects, we allocated hearts to the following four groups (n = 8 for each group) that were treated with wortmannin, a specific inhibitor of PI3Ks: 5) Insulin 0 IU/L (InsW0; Control), 6) Insulin 0.5 IU/L (InsW0.5), 7) Insulin 5 IU/L (InsW5), and 8) Insulin 50 IU/L (InsW50). In these four groups, the hearts were perfused with KH solution containing 100 nmol/L wortmannin for the first 10 min and then with the different insulin concentration solutions for 20 min. Following perfusion, the whole rat hearts were quickly frozen in liquid nitrogen and freeze-dried for 6 days.
Experiment 3
To measure the p-Akt value at 3 min and 5 min of insulin or control solution administration, whole heart muscles (n = 8 from each group) were sampled for p-Akt measurements using the technique described above (Fig. 1).
Measurements
The HR (bpm) and LV dP/dt max (mmHg/s) were recorded continuously during the heart perfusions. Coronary flow (CF) was measured by timed collection of the perfusate from the catheter inserted into the pulmonary artery at baseline and immediately before (control) and after 5, 10, 15, and 20 min perfusion with insulin. Oxygen tension was measured using a blood gas analyzer (iSTAT1 analyzer; Abbott, JAPAN, Tokyo). Oxygen consumption was calculated using the formula described by Neely et al.11. Oxygen consumption (mmol/h per g) = ((arterial – venous oxygen tension) (mm Hg) / 760 (mm Hg)) × solubility of oxygen at 37 °C (ml/ml H2O) / 22.4 [ml/mmol]) × (CF [ml/h] / dry weight of heart [g]).
The freeze-dried myocardium was suspended in an assay lysis buffer (Lysis Buffer 6, R&D Systems, Minneapolis, MN, USA) containing phenylmethanesulfonyl fluoride (2 mM, Sigma-Aldrich, Inc., St. Louis, MO, USA) and a protease inhibitor cocktail (Sigma-Aldrich, Inc.). The samples were homogenized using a micro-homogenizing system (MicroSmash MS-100R, TOMY SEIKO Co., Ltd., Tokyo, Japan), and the homogenates were centrifuged for 5 min at 2000 × g12. The supernatants were assayed for p-Akt using enzyme-linked immunosorbent assay ([pSer473/474] Akt1/2, Enzo, Farmingdale, NY, USA). The concentrations of p-Akt were quantified spectrophotometrically (Spectra Max 340, Molecular Devices, Sunnydale, CA, USA) at 450 nm. The wavelength correction was set at 540 nm. The values are expressed as milligrams p-Akt per gram dry heart weight.
Statistical analysis
Data are presented as mean ± standard deviation (SD). Intergroup comparisons for baseline measurements such as hemodynamic data and dry heart weight were performed using one-way analysis of variance (ANOVA). Changes in hemodynamics and the concentrations of p-Akt were analyzed using repeated two-way ANOVA with post-hoc Bonferroni test. Two-sided P values < 0.05 were considered statistically significant.
Sample size calculation was based on the expected difference in contractility (LV dP/dt max) between the groups. The results of a preliminary study showed a percent change in LV dP/dt max that was equivalent to 0% in the control group, 10% in the Ins0.5 group, 30% in the Ins5 group, and 70% in the Ins50 group 3 min after insulin administration. At least eight rats were required in each group to achieve a power level of 80%, with an alpha error of 5% (SD = 40%). All statistical analyses were performed using SPSS ver.23 for Windows (IBM, Chicago, IL, USA).
Ethics approval and consent to participate
The study was approved by the Ethics Committee on Animal Research of the University of Yamanashi (Protocol number A26-19, December 22, 2014). Consent to participate is not applicable.
Results
Hemodynamic data are presented in the figures. Intragroup differences are indicated using asterisks or dagger marks, and marks of intragroup differences have been omitted.
Experiment 1: Effect of insulin dosage on hemodynamic parameters in the isolated rat heart
There were no significant differences in baseline HR, LV dP/dt max, CF, and dry heart weight in each group (Table 1). High doses of insulin (5 and 50 IU/L) had a significant inotropic effect in the early phase (at 3 min), but tachyphylaxis was observed thereafter. The low dose of insulin (0.5 IU/L) had a weak but continuous inotropic effect (Fig. 2A). There were no significant intergroup differences in the HR. In the Ins5 (3 and 5 min) and Ins50 (3, 5, and 10 min) groups, HR decreased temporarily (Fig. 3A) compared with that at 0 min. The CF did not change significantly throughout the experiment in any of the treatment groups (Additional File 1A), neither did oxygen consumption in any of the insulin treatment groups (Fig. 4A).
Effect of Insulin with or without wortmannin on the changes in LV dP/dt max over time in each group (n = 8). Insulin treatment groups (Ins) are shown in A. Insulin plus wortmannin treatment groups (InsW) are shown in B. LV dP/dt max for 5 and 50 IU/L insulin at 3 min and that for 50 IU/L at 5 min increased significantly compared to that in Ins 0 (control group; intergroup comparison) (A). LV dP/dt in Ins0.5 increased at 10 min and thereafter, that in Ins 5 increased at 3 min only, and that in Ins50 increased at all time points but those at 5–20 min were lower than those at 3 min (in the intragroup comparison) (A). In the presence of wortmannin, LV dP/dt in InsW50 was higher than that in InsW0, and those in InsW5 and Ins50 were higher than those in InsW0.5 at 3 min (B). LV dP/dt in InsW5 (at 3 min) and InsW50 (at 3 and 5 min) increased temporarily (in the intragroup comparison) (B) Data are presented as the mean ± SD. *P < 0.05 versus 0 min. †P < 0.05 versus 3 min. Marks of intergroup differences have been omitted. LV dP/dt max (mmHg/s), maximum of left ventricular derivative of pressure development.
Effect of insulin with or without wortmannin on changes in the heart rate over time in each group (n = 8). Insulin treatment groups (Ins) are shown in (A). Insulin plus wortmannin treatment groups (InsW) are shown in B. There were no significant intergroup differences (A, B). In Ins 5 (3 and 5 min) and Ins50 (3, 5, and 10 min), HR was temporarily decreased (in the intragroup comparison) (A). HR in InsW0.5 was decreased at 10 min and thereafter, that in InsW5 was decreased at all time points, and that in Ins W50 was decreased within 10 min (in the intragroup comparison) (B). Data are presented as mean ± SD. *P < 0.05 versus 0 min.
Effect of insulin with or without wortmannin on changes in oxygen consumption over time in each group (n = 8). Insulin treatment groups (Ins) are shown in A. Insulin plus wortmannin treatment groups (InsW) are shown in B. There were no significant intragroup and intergroup differences in oxygen consumption in the insulin group (A). There was no significant intergroup difference at any time point in the InsW groups. Oxygen consumption in InsWT5 increased at 15 and 20 min compared to that baseline, but this change was not observed in InsWT50 (in the intergroup comparison) (B). Data are presented as the mean ± SD.
Therefore, insulin had a dose-dependent positive inotropic effect. The effect of low-dose insulin was continuous, while that of high-dose insulin was transient, and the HR was also temporarily decreased. The inotropic effect was exerted without increasing oxygen consumption.
Experiment 2: Roles of pAkt activation on inotropic effect in isolated rat heart
In the presence of wortmannin, there were no significant differences in baseline HR, LV dP/dt max, CF and dry heart weight in each group (Table 1). High doses of insulin (InsW 5 and InsW50) showed a temporary inotropic effect (at 3 min and at 3 and 5 min, respectively) even in the presence of wortmannin; however, the inotropic effect mediated by low doses of insulin was inhibited (Fig. 2B). The HR decreased after 10, 15, and 20 min in InsW0.5, at all time points in InsW5, and after 3 and 5 min in InsW50 (Fig. 3B). The CF did not change significantly throughout the experiment in any of the wortmannin treatment groups (Additional File 1B). Oxygen consumption in InsW5, but not in InsW50, increased by only 10% and 11% at 15 and 20 min, respectively, compared to that at baseline (Fig. 4B). Hence, wortmannin, a PI3K specific inhibitor, partially inhibited the positive inotropic effect of insulin.
Experiment 3: Insulin concentration with and without PI3K inhibitor and Akt activation at different time points
In all insulin groups, p-Akt levels were increased at all time points compared with that in the control group (Fig. 5A). However, in all insulin groups, p-Akt levels in the later time points (at 20 min) were decreased compared to those at 3 min (Fig. 5A). In the presence of wortmannin, this increase was observed only in the early phases (3 and 5 min) of these experiments (Fig. 5B). In all insulin groups, pAkt levels in the presence of wortmannin in the later time points (at 5 or 20 min) were also decreased compared to those at 3 min (Fig. 5A).
Effect of insulin with or without wortmannin on changes in p-Akt levels over time in each group (n = 8). Insulin treatment groups (Ins) are shown in A. Insulin plus wortmannin treatment groups (InsW) are shown in B. p-Akt levels were increased at all time points compared with those in the control group (in the intergroup comparison) (A). In all insulin groups, p-Akt levels at the later time point (at 20 min) were decreased compared to those at 3 min (in the intragroup comparison) (A); in the presence of wortmannin, this change was only noticed in at the early time points (3 and 5 min) (in the intergroup comparison) (B). In all insulin groups in the presence of wortmannin, pAkt levels at the later time points (at 5 or 20 min) were also decreased compared to those at 3 min (in the intragroup comparison) (B). Data are presented as the mean ± SD. Marks of intergroup differences have been omitted *P < 0.05 versus 3 min. †P < 0.05 versus 5 min.
Akt phosphorylation and cardiac contractility increased concomitantly with insulin concentration during the early phase of treatment, but some discrepancies were observed between the p-Akt level and myocardial performance during the late phase (at 5 and 20 min).
Discussion
In this study, on assessing the relationship between insulin concentration and the inotropic effects mediated by the PI3K/Akt pathway in an isolated rat heart model, we found that the positive inotropic effect of insulin during the early time points (within 3 min) was dose-dependent and was likely mediated by the PI3K/Akt pathway because of a concomitant increase in Akt phosphorylation and cardiac contractility. In contrast, tachyphylaxis was detected in groups with high doses of insulin (Ins5 and Ins50). Low doses of insulin (Ins0.5 group) exerted weak but continuous positive inotropic effects even in the later time points (at 5 and 20 min). These findings suggest that factors other than pAkt are involved in the mechanism of tachyphylaxis because some discrepancies were observed between p-Akt levels and myocardial performance.
Inotropy is modulated by calcium following its entry into myocardial cells via L-type calcium channels, calcium release by the sarcoplasmic reticulum (SR) via the activation of ryanodine receptors (RyR), calcium binding to protein, troponin C, myosin phosphorylation, SR Ca2+ (SERCA) ATPase activity, and calcium efflux across the sarcolemma mediated by an ATP-dependent Ca2+ pump Na+/Ca2+ exchanger and Na/K/ATPase pump13. Insulin increases calcium entry through L-type channels14 and Na+/Ca2+ exchangers15. In addition, insulin increases the mRNA expression of RyR and SERCA ATPase16. These improvements in calcium binding and/or trans-sarcolemma calcium transportation are mediated by PI3K/Akt activation. Insulin binding to its receptor leads to the activation of the PI3K/Akt pathway, which is a main player in mediating the metabolic effects of insulin. Several reports have shown that Akt phosphorylation also regulates L-type calcium channels17, RyR activation18, myosin phosphorylation9, and (SERCA) ATPase activity19. When a calcium in perfusate was used within a biological range (1.25 mmol/L), the inotropic effects of insulin were mediated dose dependently in isolated rat hearts20. Our results demonstrated that Akt activation was almost consistent with cardiac contractility 3 min after insulin administration, thereby contributing to enhanced inotropic effects.
Indeed, the inotropic effect of low dose insulin (0.5 IU/L) was not observed in the presence of a specific inhibitor of PI3Ks, further supporting the role of Akt activation in inotropic effects in the normal rat heart.
However, the positive inotropic effects were temporary at high insulin concentrations, and the p-Akt values did not correlate with myocardial performance during the late phase of insulin treatment. Although p-Akt levels in the insulin groups were higher than those in the control group at 20 min, cardiac contractility and oxygen consumption were comparable among all groups at 20 min. A previous study reported that the inotropic effect under a supraphysiological insulin concentration (25 IU/L) was abolished when the heart was perfused with insulin for 10 min21. It was speculated that glycolytic ATP formation plays a key role in the development of insulin-induced tachyphylaxis. The heart requires a constant supply of fuel and oxygen to maintain its intracellular ATP level and the myocardial contraction/relaxation cycle22. In our study, oxygen and glucose was supplied continuously by oxygenated perfusate and oxygen consumption, which was shown in additional file 1, was similar independent of insulin concentration or presence of wortmannin. Our data also revealed a higher pAkt level at all time points in the insulin groups than in the control group. It suggested that ATP production should increase in the presence of insulin because glucose uptake through glucose transporters (GLUTs; mainly GLUT4 in adult heart) is promoted via PI3K/Akt activation in a dose-dependent manner8,22 when glucose and insulin concentrations increase. Therefore, other factors are likely to influence high-dose insulin-induced tachyphylaxis, such as cAMP. Recently. Oudit et al. reported that the loss of PI3K can increase basal myocardial cAMP levels and myocardial expression of adenylate cyclase23. Moreover, PI3K signaling negatively regulates β-adrenergic positive inotropic effects24; therefore, insulin-induced tachyphylaxis may be observed when cAMP suppression following Akt activation supersedes calcium handling activation. This hypothesis may explain the partial suppression of Akt activation, ameliorated inotropic effect of insulin, and lack of tachyphylaxis in hearts pre-treated with wortmannin. However, further studies are needed to clarify the occurrence of tachyphylaxis.
We observed decreased HR in the presence of high doses of insulin. The HR depends on the rate at which the sinoatrial node (SA) produces action potentials, while β1 adrenoceptors, M2 muscarinic receptors, and messengers play important roles in regulating it. Activation of β1 adrenoceptors expressed on the membrane of pacemaker cells activate Gs-proteins, leading to increased levels of cAMP, which binds to hyperpolarization-activated cyclic nucleotide-gated channels that increase the current and rate of depolarization during pacemaker potential. cAMP also increases the Ca2+ current, opening time of L-type calcium channels, and the speed of phase 0. Acetylcholine binds to the M2 muscarinic receptor and activates the coupled Gi-protein, which increases K+ flow out of the cell and decreases the membrane potential, increasing the time taken by pacemaker cells to reach their threshold values25. Lin et al. reported that PI3K activation increases the HR independent of the autonomic nervous system because Akt inhibition slows the pacing rate of the SA26. Conversely, Akt also stimulates the muscarine receptor18 and Gi-proteins27, which suggests that the muscarinic effect may be dominant in high doses of insulin compared to increased current.
In this study, insulin enhanced myocardial contractility without increasing myocardial oxygen consumption. We have previously reported that insulin exerts an ischemic protective effect on the same isolated rat heart model12 and, therefore, an inotropic effect mediated by the PI3K/Akt pathway might maintain hemodynamics during general anesthesia. We need further study such as effects of combination of a lower dose of insulin with catecholamines and /or for female rats for clinical application.
This study had some limitations. First, the insulin 5 and 50 IU/L concentrations were supraphysiologic. Second, the dose of wortmannin used might not have been sufficient to completely inhibit Akt activation. Third, we did not measure the downstream effects of the PI3K/Akt pathway and, thus, further studies are required to clarify the details underlying its downstream effects. Fourth, although in our model we constantly supplied 5.5 mmol/L of glucose, we did not consider the risk of hypoglycemia. In the clinical setting, meticulous glucose administration would be required to avoid hypoglycemia.
Conclusion
Insulin activates the PI3K/Akt pathway in a dose-dependent manner, which leads to increased cardiac contractility in isolated intact rat hearts. High doses of insulin exerted transient inotropic effects, which could be reduced by wortmannin treatment. Further studies are needed to clarify the downstream events of the tachyphylaxis pathway.
Data availability
The datasets used and analyzed during this study are available from the corresponding author upon reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- GLUT:
-
Glucose transporter
- HR:
-
Heart rate
- KH:
-
Krebs–Henseleit
- LV:
-
Left ventricular
- LV dP/dt max:
-
Maximum LV pressure derivative
- Ins0:
-
Insulin 0 IU/L
- Ins0.5:
-
Insulin 0.5 IU/L
- Ins5:
-
Insulin 5 IU/L
- Ins50:
-
Insulin 50 IU/L
- InsW0:
-
Insulin 0 IU/L and wortmannin
- InsW0.5:
-
Insulin 0.5 IU/L and wortmannin
- InsW5:
-
Insulin 5 IU/L and wortmannin
- InsW50:
-
Insulin 50 IU/L and wortmannin
- PI3K/Akt:
-
Phosphoinositol-3-kinase/Akt
- RyR:
-
Ryanodine receptors
- SA:
-
Sinoatrial node
- SD:
-
Standard deviation
- SERCA:
-
Sarcoplasmic reticulum Ca2+
- SR:
-
Sarcoplasmic reticulum
References
Butterworth, J. Selecting an inotrope for the cardiac surgery patient. J. Cardiothorac. Vasc. Anesth. 7(Suppl 2), 26–32 (1993).
Smith, L. D. & Oldershaw, P. J. Inotropic and vasopressor agents. Br. J. Anaesth. 56(7), 767–780 (1984).
Rieker, R. P., Lee, J. C. & Downing, S. E. Positive inotropic action of insulin on piglet heart. Yale J. Biol. Med. 48(5), 353–360 (1975).
Lucchesi, B. R., Medina, M. & Kniffen, F. J. The positive inotropic action of insulin in the canine heart. Eur. J. Pharmacol. 18(1), 107–115 (1972).
Lee, J. C. & Downing, S. E. Effects of insulin on cardiac muscle contraction and responsiveness to norepinephrine. Am. J. Physiol. 230(5), 1360–1365 (1976).
Klein, L. J., van Campen, C. M., Sieswerda, G. T., Kamp, O. & Visser, F. C. Effects of high-dose insulin infusion on left ventricular function in normal subjects. Neth. Heart J. 18(4), 183–189 (2010).
Sussman, M. A. et al. Myocardial AKT: The omnipresent nexus. Physiol. Rev. 91(3), 1023–1070 (2011).
Iliadis, F., Kadoglou, N. & Didangelos, T. Insulin and the heart. Diabetes Res. Clin. Pract. 93(Suppl 1), S86-91 (2011).
Cittadini, A. et al. Adenoviral gene transfer of Akt enhances myocardial contractility and intracellular calcium handling. Gene Ther. 13(1), 8–19 (2006).
Skrzypiec-Spring, M., Grotthus, B., Szelag, A. & Schulz, R. Isolated heart perfusion according to Langendorff—Still viable in the new millennium. J. Pharmacol. Toxicol. Methods 55(2), 113–126 (2007).
Neely, J. R., Liebermeister, H., Battersby, E. J. & Morgan, H. E. Effect of pressure development on oxygen consumption by isolated rat heart. Am. J. Physiol. 212(4), 804–814 (1967).
Sato, T. et al. Insulin preconditioning elevates p-Akt and cardiac contractility after reperfusion in the isolated ischemic rat heart. BioMed. Res. Int. 2014, 536510 (2014).
K K: Cardiovascular Physiology Concept, 3rd ed. (2021).
Maier, S. et al. Stimulation of L-type Ca2+ current in human atrial myocytes by insulin. Cardiovasc. Res. 44(2), 390–397 (1999).
von Lewinski, D., Bruns, S., Walther, S., Kögler, H. & Pieske, B. Insulin causes [Ca2+]i-dependent and [Ca2+]i-independent positive inotropic effects in failing human myocardium. Circulation 111(20), 2588–2595 (2005).
Teshima, Y. et al. Diminished expression of sarcoplasmic reticulum Ca(2+)-ATPase and ryanodine sensitive Ca(2+)channel mRNA in streptozotocin-induced diabetic rat heart. J. Mol. Cell Cardiol. 32(4), 655–664 (2000).
Catalucci, D. et al. Akt regulates L-type Ca2+ channel activity by modulating Cavalpha1 protein stability. J. Cell Biol. 184(6), 923–933 (2009).
Baine, S. et al. Muscarinic-dependent phosphorylation of the cardiac ryanodine receptor by protein kinase G is mediated by PI3K-AKT-nNOS signaling. J. Biol. Chem. 295(33), 11720–11728 (2020).
Chen, Y. et al. Hydrogen sulfide regulates cardiac sarcoplasmic reticulum Ca(2+) uptake via K(ATP) channel and PI3K/Akt pathway. Life Sci. 91(7–8), 271–278 (2012).
Schmidt, H. D. & Koch, M. Influence of perfusate calcium concentration on the inotropic insulin effect in isolated guinea pig and rat hearts. Basic Res. Cardiol. 97(4), 305–311 (2002).
Sethi, R. et al. Characteristics and mechanisms of tachyphylaxis of cardiac contractile response to insulin. Int. J. Cardiol. 38(2), 119–130 (1993).
Beg, M., Abdullah, N., Thowfeik, F. S., Altorki, N. K. & McGraw, T. E. Distinct Akt phosphorylation states are required for insulin regulated Glut4 and Glut1-mediated glucose uptake. Elife 6, e26896 (2017).
Oudit, G. Y. & Penninger, J. M. Cardiac regulation by phosphoinositide 3-kinases and PTEN. Cardiovasc. Res. 82(2), 250–260 (2009).
Leblais, V. et al. Phosphatidylinositol 3-kinase offsets cAMP-mediated positive inotropic effect via inhibiting Ca2+ influx in cardiomyocytes. Circ. Res. 95(12), 1183–1190 (2004).
Pérez-Riera, A. R., Barbosa-Barros, R., Daminello-Raimundo, R., de Abreu, L. C. & Nikus, K. Current aspects of the basic concepts of the electrophysiology of the sinoatrial node. J. Electrocardiol. 57, 112–118 (2019).
Lin, R. Z. et al. Regulation of heart rate and the pacemaker current by phosphoinositide 3-kinase signaling. J. Gen. Physiol. 151(8), 1051–1058 (2019).
Anger, T. et al. RGS protein specificity towards Gq- and Gi/o-mediated ERK 1/2 and Akt activation, in vitro. J. Biochem. Mol. Biol. 40(6), 899–910 (2007).
Acknowledgements
We thank M. Koshimizu, M. Abe and K. Tanaka for their valuable technical assistance. This work was presented in part at the Annual Meeting of American Society of Anesthesiology, San Diego, USA, October 24–29, 2015 and the Annual Meeting of Canadian Anesthesiologist’s Society, Montreal, Canada, June 15-18, 2018.
Funding
This work was supported by a Grant-in-Aid (C) for Scientific Research (KAKENHI Grant no. 26462352) from the Japan Society for the Promotion of Science (JSPS).
Author information
Authors and Affiliations
Contributions
Y.N. designed and conducted the study, collected and analyzed data, and prepared the manuscript. K.A. helped in designing and conducting the study, collecting and analyzing data, and preparing the manuscript. H.S. helped in designing the study and preparing the manuscript. T.S. helped in designing the study and preparing the manuscript. T.O. helped in conducting the study, collecting and analyzing data, and preparing the manuscript. K.O. helped in interpreting the data and preparing the manuscript. T.M. helped in preparing the manuscript. T.S. helped in designing the study and preparing the manuscript. T.M. helped in designing the study and preparing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakadate, Y., Kawakami, A., Sato, H. et al. PI3K/Akt pathway mediates the positive inotropic effects of insulin in Langendorff-perfused rat hearts. Sci Rep 12, 9793 (2022). https://doi.org/10.1038/s41598-022-14092-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-14092-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.