Abstract
Some patients with COVID-19 pneumonia develop an associated cytokine storm syndrome that aggravates the pulmonary disease. These patients may benefit of anti-inflammatory treatment. The role of colchicine in hospitalized patients with COVID-19 pneumonia and established hyperinflammation remains unexplored. In a prospective, randomized controlled, observer-blinded endpoint, investigator-initiated trial, 240 hospitalized patients with COVID-19 pneumonia and established hyperinflammation were randomly allocated to receive oral colchicine or not. The primary efficacy outcome measure was a composite of non-invasive mechanical ventilation (CPAP or BiPAP), admission to the intensive care unit, invasive mechanical ventilation requirement or death. The composite primary outcome occurred in 19.3% of the total study population. The composite primary outcome was similar in the two arms (17% in colchicine group vs. 20.8% in the control group; p = 0.533) and the same applied to each of its individual components. Most patients received steroids (98%) and heparin (99%), with similar doses in both groups. In this trial, including adult patients with COVID-19 pneumonia and associated hyperinflammation, no clinical benefit was observed with short-course colchicine treatment beyond standard care regarding the combined outcome measurement of CPAP/BiPAP use, ICU admission, invasive mechanical ventilation or death (Funded by the Community of Madrid, EudraCT Number: 2020-001841-38; 26/04/2020).
Similar content being viewed by others
Introduction
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV2) infection, responsible for coronavirus disease 2019 (COVID-19), is associated with high mortality secondary to pneumonia1. Current evidence suggests that some patients with COVID-19 pneumonia develop an associated cytokine storm syndrome that aggravates the pulmonary disease2. The use of dexamethasone3 has been was shown to reduce mortality in these patients, supporting the importance of the inflammatory process.
Colchicine is an anti-inflammatory drug with appealing features for the treatment of the associated hyperinflammation in this setting. First, colchicine inhibits the production of chemokines involved in leukocyte recruitment and activation4,5. Second, colchicine may have an immunomodulatory effect on pulmonary leukocytes6. Third, what in another context would be considered an adverse effect leading to a greater risk of pneumonia, in the COVID-19 hyperinflammation phase, here may act as an effective treatment. Moreover, COVID-19 has been associated with cardiac complications7,8, and therefore, colchicine, as a cardioprotective drug9, could prevent this associated damage. Finally, colchicine is characterized by a safe profile in terms of adverse effects.
The COLCORONA trial, a randomized, double-blind, placebo-controlled, investigator-initiated trial, included 4488 non hospitalized patients with SARS-CoV-2 infection; in the predefined subset of patients with PCR-confirmed COVID-19, colchicine reduced the composite rate of death or hospitalizations10. Colchicine in hospitalized patients with SARS-CoV-2 infection has been previously assessed. In the GRECCO-19 trial, an open-label randomized trial including 105 hospitalized patients for SARS-CoV-2 infection, colchicine improved time to clinical deterioration; however, no significant difference was observed in clinical respiratory complications or death11. Recently, the RECOVERY trail, a randomized, controlled, open-label trial including 11,340 hospitalized patients with COVID-19, showed no differences in the composite endpoint of invasive mechanical ventilation or death12.
Nevertheless, none of these studies specifically focused on the important subset of patients with associated hyperinflammation.
The role of colchicine in hospitalized patients with moderate to severe COVID-19 pneumonia and established hyperinflammation remains unknown.
The primary aim of the trial was to determine whether adding colchicine to standard of care background therapy reduces clinical events in hospitalized patients with moderate to severe COVID19 pneumonia and established hyperinflammation, compared to standard treatment (EudraCT Number: 2020-001841-38; 26/04/2020).
Methods
We conducted a prospective, randomized controlled, observer-blinded endpoint (PROBE), investigator-initiated trial.
Study population
Hospitalized patients with COVID-19 pneumonia were eligible if they were ≥ 18 years of age and presented with at least 2 of the following 4 inflammatory criteria: C-reactive protein > 4 mg/dL, D-dimer > 1 mg/L, ferritin > 1000 ng/mL or fever ≥ 38 °C in the last 24 h. The diagnosis of SARS-CoV-2 was made using polymerase chain reaction testing on a nasopharyngeal swab specimen in all patients. All patients had a chest X-ray test assessed by expert radiologists supporting the diagnosis of pneumonia. Furthermore, radiologists assigned each chest X-ray a RALE score, reflecting the extent of lung involvement from COVID-19 pneumonia13.
Patients were excluded if they had concomitant active inflammatory bowel disease, diarrhea or malabsorption; estimated glomerular filtration rate less than 30 mL/min/1.73 m2; severe hepatic cirrhosis or acute hepatitis; granulocytopenia (< 500/mm3); low platelet count (< 50 × 109/L); concomitant treatment with ritonavir; chronic treatment with colchicine or immunosuppression treatment; history of significant sensitivity to colchicine; pregnant women, or participating in another clinical trial. Patients were excluded if they were already receiving either non-invasive or invasive respiratory support at the time of screening.
Clinicians assessed the initial eligibility of the patients. Thereafter, masked randomization was centralized and done electronically by the principal investigators of each site using an automated interactive web-response system (www.studyrandomizer.com). Recruited patients were randomly assigned, in a 1:1 ratio, to colchicine (5 days of oral treatment: 1 mg loading dose and then 0.5 mg/day) or no colchicine, using an allocation sequence that was computer-generated using a blocking schema with block sizes of four. Allocation sequence was not stratified.
An academic steering committee designed the trial protocol (available as Supplemental material) and oversaw the study execution. The clinical research pharmacy monitored the appropriate drug administration. Four tertiary university hospitals participated in the study. Sites and investigators are presented in the Online Appendix. For each analysis, patients with missing value were excluded following a strategy of complete-case analysis. Regarding quality control, the data of all patients were recorded electronically in a database created for this purpose. The database was debugged by means of logical, range and consistency tests. Once the data had been linked, the patient identifiers were anonymized. Each patient, or the patient’s legally authorized representative, provided informed consent. The trial was conducted in accordance with the International Conference on Harmonisation E6 guidelines for Good Clinical Practice and the Declaration of Helsinki. This trial was approved by the Spanish Agency of Medicines and Medical Devices and all the corresponding local Clinical Research Ethics Committee (Hospital Universitario de La Princesa, Hospital General Universitario Gregorio Marañon, Hospital Universitario de Cabueñes and Hospital Universitario Fundación Jiménez Díaz).
Main outcomes
The primary efficacy outcome measure was a composite of non-invasive mechanical ventilation (CPAP or BiPAP), admission to the intensive care unit, invasive mechanical ventilation requirement or death. The primary outcome measure was overseen and adjudicated by an independent clinical event committee which was blinded to treatment allocation. In patients previously suffering from sleep apnea syndrome, the use of CPAP was only considered as an outcome if clinically indicated for oxygenation therapy after failure of standard oxygenation support. Secondary outcomes were hospital stay and changes in laboratory biomarkers of inflammation and troponin. The incidence and severity of adverse events were prospectively evaluated.
Statistical analyses
Quantitative variables are presented as mean ± standard deviation or median (interquartile range) as required. Comparisons between both arms were made with the Student’s t-test or Mann–Whitney–Wilcoxon test. Categorical variables are expressed as frequency (percentage) and both arms were compared with χ2 test and Fisher’s exact test when necessary. It was estimated that a sample size of approximately 240 randomized patients, with 120 patients in each treatment arm, would be required to detect a 50% relative risk reduction with colchicine, considering a primary endpoint event rate of 30% in the control group, with a power of 80% and a two-sided test at the 0.05 significance level. The efficacy analyses were conducted using an intention-to-treat analysis. The composite primary outcome, as well as its components, were compared between the two groups using logistic regression analyses and odds ratios (95%CI) were provided. In addition, pre-specified subgroup analyses of the composite primary outcome measure were performed according to well-established risk factors for poor outcome in COVID-19, including age, sex, hypertension, body mass index (BMI), days from onset of symptoms, pneumonia extension in chest X-ray and oxygen support requirement at recruitment3,13,14,15,16,17. Statistical analyses were performed using STATA 14.2 package (StataCorp, LLC, Texas).
Results
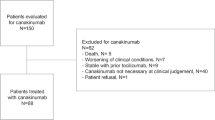
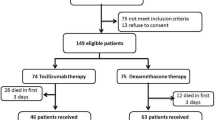
All patients were recruited between August 2020 and March 2021. Of them, one patient withdrew consent. Finally, 119 patients formed the colchicine group and 120 the control group (Fig. 1).
The baseline characteristics of patients are shown in Table 1. Patients were enrolled with a mean of 1.9 ± 1.9 days after hospital admission and a mean of 9.0 ± 3.4 days after the onset of symptoms. The mean age was 65 ± 16 years and 59% were male. Mean BMI was 27.5 ± 4.5, 16% had diabetes, 40% were hypertensive and 7% had a history of coronary artery disease. The two groups showed no significant differences in the clinical baseline characteristics. According to the WHO disease severity classification, 53 (22%) and 186 (78%) participants had moderate and severe COVID-19 disease, respectively. No differences were observed between the two groups on disease severity. Considering days from admission, the control group patients were recruited slightly earlier (2.1 ± 2.3 days in the colchicine group vs. 1.6 ± 1.1 days in the control group; p = 0.026). However, no difference was detected in terms of days from the onset of symptoms.
Regarding inflammation markers at recruitment, mean ferritin was higher in colchicine group (1346.9 ± 1023.6 ng/mL in colchicine group vs. 1053.6 ± 796.3 ng/mL in control group; p = 0.018) while mean d-dimer was higher in control group (0.9 ± 0.7 mg/L in colchicine group vs. 1.1 ± 0.9 mg/L in control group; p = 0.026) mg/L. No significant differences were observed in temperature, C-reactive protein and interleukin 6 values.
Clinical endpoints
The composite primary outcome occurred in 19.3% of the total study population. Specifically, 10.5% were admitted to intensive care units, 14.2% received non-invasive ventilation (CPAP or BiPAP), 6.3% were invasively ventilated and 6.7% died during hospitalization. The composite primary outcome was similar in the two arms (17% in the colchicine group vs. 20.8% in the control group; p = 0.533) and the same applied to each of its individual components (Table 2).
Most patients received steroids (98%) with a similar peak dose of steroids in both groups (17.9 ± 12.1 mg of dexamethasone equivalent dose in colchicine group and 16.6 ± 12.8 mg in the control group; p = 0.418). A 99% of the patients received heparin (59.9% prophylactic, 31.4% intermediate and 8.0% anticoagulant doses) with no difference between the groups. None of the patients received hydroxychloroquine. Two patients of the colchicine group received lopinavir/ritonavir. Remdesivir was administered in 37 patients (19 patients in the colchicine group vs. 18 in the control group; p = 0.859). A total of 47 patients received tocilizumab during the hospitalization (30 in the colchicine group vs. 17 in the control group; p = 0.035). The use of other monoclonal antibodies was very minimal (anakinra to 1 patient in each group; baricitinib was administered to 1 patient in colchicine group and to 2 patients in the control group).
Pre-specified subgroup analyses are shown in Fig. 2. Results of most subgroups were consistent with the main analysis. However, in overweight patients, the colchicine group showed a lower prevalence of the composite primary outcome (11.7% in the colchicine group vs. 27.3% in the control group; OR 0.35, 95% CI 0.13–0.94; p = 0.038).
Mean hospital stay was 11.3 ± 9.6 days. No differences were seen between the two groups (p = 0.765).
Inflammatory laboratory markers and troponin
Results of inflammatory markers at recruitment, on the 3rd and 5th day are shown in Fig. 3. Apart from the difference at recruitment commented above, no statistically significant differences were found on the inflammatory biomarkers on the 3rd and 5th day, except for the ferritin on the 3rd day in which higher levels for colchicine were found (p = 0.024). Troponin showed no differences both at recruitment (12 ± 21 ng/L in the colchicine group vs. 11 ± 10 ng/L; p = 0.661) and at 5th day (15 ± 33 ng/L in the colchicine group vs. 9 ± 8 ng/L; p = 0.101).
Adverse events
Following exclusion criteria, none of the patients had diarrhea at recruitment. Diarrhea incidence was infrequent and similar in both groups (3.4% in the colchicine group vs. 1.7% in the control group; p = 0.683). Colchicine was interrupted prematurely due to diarrhea only in one patient. Thrombotic events, defined as deep vein thrombosis or pulmonary embolism, were diagnosed in 1.7% of patients in the colchicine group and 4.2% of those in the control group (p = 0.446). No hematologic disorders or abnormalities were detected.
Discussion
To our knowledge, this is the first study assessing the clinical efficacy of colchicine in hospitalized patients with COVID-19 pneumonia and established hyperinflammation. In this randomized trial adding colchicine to standard background therapy was not associated with a lower risk of CPAP/BiPAP use, ICU admission, invasive ventilation requirement or death.
When the study was designed, COVID-19 patients had worse clinical outcomes at the beginning of the pandemic as steroids and heparins had not yet been included in the standard treatment protocols. Nonetheless, most patients included in our trial received steroids and heparins, potentially explaining, at least in part, a lower than expected rate of the observed primary clinical endpoint. For this reason, the main analysis might have been underpowered. Moreover, the optimal dosage of colchicine in COVID-19 patients is still undefined. Remarkably, the proposed dose of colchicine was safe in our population with moderate to severe COVID-19 pneumonia.
The SARS-CoV-2 interaction with macrophages promotes the nod-like receptor protein 3 (NLRP3) inflammasome assembly, a proinflammatory complex which drives to several cytokines release including IL-1β and IL-6. These pro-inflammatory cytokines induce neutrophil activation and infiltration into the infected tissues, which, in excess, aggravate the clinical condition. Considering that colchicine has shown to inhibit NLRP3 inflammasome and neutrophil activation, it has been considered a valid candidate as potential treatment for COVID-1918,19. Two randomized clinical studies previously suggested a beneficial effect of colchicine in hospitalized patients with COVID-19, recruiting only 72 and 105 patients, respectively. Specifically, Lopes et al. observed a reduction of hospital stay, whereas Deftereos et al. documented a significant improvement in time to clinical deterioration in those participants receiving colchicine11,20. However, the results remained uncertain as both trials had a small sample size and a low rate of events. On the other hand, the colchicine arm of the RECOVERY trial, a large randomized clinical trial, found no clinical benefit. Moreover, colchicine showed no beneficial effect on the need of mechanical ventilation or 28-day mortality in a recent randomized clinical trial including 1279 patients hospitalized with COVID-19 pneumonia21. Nevertheless, none of these previous studies focused on patients with COVID-19 pneumonia and established hyperinflammation, a subset of patients particularly attractive to assess the effect of colchicine.
In the pre-specified subgroup analysis, overweight patients in the colchicine group showed a statistically significant lower prevalence of CPAP/BiPAP use, ICU admission, invasive ventilation or death. Interestingly, in the scenario of SARS-CoV-2 infection, overweight and obesity are associated with a higher risk of hospital admission22 and progression to severe COVID23. However, since the RECOVERY and ECLA PHRI COLCOVID trials did not collect BMI information12,21, this is the first clinical trial analyzing the effect of colchicine on overweight patients. Remarkably, the excess of macronutrients in the adipose tissues predisposes to the releases of inflammatory mediators which participate in the cytokine storm aggravating COVID-192. Furthermore, colchicine was previously demonstrated to significantly improve the inflammatory markers in obese patients without significant medical illness24. For all these reasons, overweight patients with COVID-19 pneumonia and established hyperinflammation might particularly benefit from colchicine treatment. In a post-hoc analysis we found no differences in the background therapy of overweight patients during hospitalization, including tocilizumab. On the other hand, proposed dose and treatment duration of colchine might be insufficient to observe beneficial effects on obese patients. Thus, despite being appealing from a pathophysiological standpoint, major care should be paid to interpret this subgroup considering its limited size. Therefore, results should be only considered as hypothesis-generating and would require confirmation in further studies.
Colchicine had no beneficial effect on myocardial injury measured as troponin release on the 5th day. However, considering the stabilizing effect of colchicine on atherosclerotic plaques5,9, patients with coronary artery disease would theoretically be the subgroup of patients more responsive to colchicine. Since coronary artery disease was present only in 6.7% of the study patients, our cohort may not be appropriate to rule out a potentially protective role of colchicine on myocardial injury associated with COVID-19.
Our study has several limitations. As discussed, the event rate was lower than expected, therefore, reducing the power of the main analysis. Besides, the lack of placebo may introduce a performance bias that cannot be excluded. However, this was partially mitigated by the blinding of outcome assessment using an independent external clinical event committee. Despite the short-course colchicine treatment, a longer biological effect was expected as the drug’s half-life is of about 60 h in leukocytes. Despite using a masked randomization scheme, which is a common method to mitigate allocation biases in baseline characteristics, our study showed differences between groups in term of ferritin and d-dimer levels at randomization. These differences in inflammatory markers might explain the higher rate of tocilizumab administration in the colchicine group during the hospital stay.
Conclusions
In a cohort of 240 hospitalized adult patients with COVID 19 pneumonia and associated hyperinflammation, no clinical benefit was observed with short-course colchicine treatment beyond standard care regarding the combined outcome measurement of CPAP/BiPAP use, ICU admission, invasive mechanical ventilation or death. Further studies are warranted to identify COVID-19 patients potentially experiencing a clinical benefit with colchicine treatment.
Data availability
Data sharing will be considered upon reasonable request including a detailed research plan with the corresponding author.
References
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382(8), 727–733 (2020).
Chen, L. Y. C. & Quach, T. T. T. COVID-19 cytokine storm syndrome: A threshold concept. Lancet Microbe 2(2), e49-50 (2021).
RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N. Engl. J. Med. 384(8), 693–704 (2021).
Leung, Y. Y., Yao Hui, L. L. & Kraus, V. B. Colchicine-update on mechanisms of action and therapeutic uses. Semin. Arthritis Rheum. 45, 341–350 (2015).
Cecconi, A. et al. Effects of colchicine on atherosclerotic plaque stabilization: A multimodality imaging study in an animal model. J. Cardiovasc. Transl. Res. 14(1), 150–160 (2021).
Tardif, J.-C. et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N. Engl. J. Med. 381(26), 2497–2505 (2019).
Guo, T. et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 5(7), 811 (2020).
Salamanca, J. et al. COVID-19 “fulminant myocarditis” successfully treated with temporary mechanical circulatory support. JACC Cardiovas. Imaging 13, 2457–2459 (2020).
Roubille, F. & Tardif, J. C. Colchicine for secondary cardiovascular prevention in coronary disease. Circulation 142, 1901 (2020).
Tardif, J.-C. et al. Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial. Lancet Respir. Med. https://doi.org/10.1016/S2213-2600(21)00222-8 (2021).
Deftereos, S. G. et al. Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: The GRECCO-19 randomized clinical trial. JAMA Netw. Open 3(6), e2013136 (2020).
RECOVERY Collaborative Group. Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet Respir. Med. 9(12), 1419–1426 (2021).
Cozzi, D. et al. Chest X-ray in new coronavirus disease 2019 (COVID-19) infection: Findings and correlation with clinical outcome. Radiol. Med. 125(8), 730–737 (2020).
Gao, M. et al. Associations between body-mass index and COVID-19 severity in 6·9 million people in England: A prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 9(6), 350–359 (2021).
Katz, M. H. Regardless of age, obesity and hypertension increase risks with COVID-19. JAMA Intern. Med. 181, 379–381 (2021).
Peckham, H. et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 11(1), 1–10 (2020).
Hyun, J. H. et al. Effects of early corticosteroid use in patients with severe coronavirus disease 2019. BMC Infect. Dis. 21(1), 506 (2021).
Reyes, A. Z. et al. Anti-inflammatory therapy for COVID-19 infection: The case for colchicine. Ann. Rheum. Dis. 80(5), 550–557 (2021).
Zein, A. F. M. Z. & Raffaello, W. M. Effect of colchicine on mortality in patients with COVID-19—A systematic review and meta-analysis. Diabetes Metab. Syndr. 16(2), 102395 (2022).
Lopes, M. I. et al. Beneficial effects of colchicine for moderate to severe COVID-19: A randomised, double-blinded, placebo-controlled clinical trial. RMD Open 7(1), e001455 (2021).
Diaz, R. et al. Effect of colchicine vs usual care alone on intubation and 28-day mortality in patients hospitalized with COVID-19: A randomized clinical trial. JAMA Netw. Open 4(12), e2141328–e2141328 (2021).
Hamer, M., Gale, C. R., Kivimäki, M. & Batty, G. D. Overweight, obesity, and risk of hospitalization for COVID-19: A community-based cohort study of adults in the United Kingdom. Proc. Natl. Acad. Sci. U.S.A. 117(35), 21011–21013 (2020).
Cai, Q. et al. Obesity and COVID-19 severity in a designated hospital in Shenzhen, China. Diabetes Care 43(7), 1392–1398 (2020).
Demidowich, A. P. et al. Effects of colchicine in adults with metabolic syndrome: A pilot randomized controlled trial. Diabetes Obes. Metab. 21(7), 1642–1651 (2019).
Acknowledgements
We dedicate this work to the memory of people who have given their lives in the care of COVID-19 patients. We thank all doctors, nurses and technicians who made this project possible. In addition, we thank the Spanish Society of Cardiology (promoter of the study) for the logistic support.
Funding
The trial was funded by the Directorate-General for Research, Teaching and Documentation of the Department of Health of the Community of Madrid.
Author information
Authors and Affiliations
Contributions
A.C., F.S.M., H.D.L.F., L.J.J.B., M.A.S.B., M.C., P.C., J.A, C.S., and F.A. designed the study. A.C., P.M.V., A.V., C.V.O., A.B., E.F.A., P.R., S.H.M., M.J.O., M.C., R.P.S., R.F.M.M., A.B.H., E.G.C., G.I., E.A., D.P.C., A.A.O., E.F.C., A.M.J., and A.A. collected data. A.C., P.M. and A.S.G. performed the analyses. A.C., P.M.V., F.S.M., M.C., L.J.J.B., and FA wrote the manuscript. All authors critically reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cecconi, A., Martinez-Vives, P., Vera, A. et al. Efficacy of short-course colchicine treatment in hospitalized patients with moderate to severe COVID-19 pneumonia and hyperinflammation: a randomized clinical trial. Sci Rep 12, 9208 (2022). https://doi.org/10.1038/s41598-022-13424-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13424-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.