Abstract
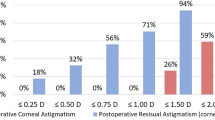
Surgical outcomes of toric intraocular lens (IOL) implantation for 8 years after surgery were analyzed. Data were retrospectively collected in 176 eyes of 176 patients before and 1 month, 1, 3, 5, and 8 years after phacoemulsification and implantation of a toric IOL. Preoperative corneal and postoperative manifest astigmatism was analyzed by converting to power vector notations; horizontal/vertical (J0) and oblique (J45) astigmatism components. Toric IOL implantation significantly reduced pre-existing astigmatism by decreasing J0 in eyes with preoperative with-the-rule (WTR) astigmatism, increasing J0 in eyes with against-the-rule (ATR) astigmatism, and correcting J45 in eyes with oblique astigmatism. After surgery, the eyes with preoperative ATR astigmatism showed a significant ATR astigmatic shift, and J0 at 5 and 8 years was significantly smaller than that at 1 month postoperatively. Uncorrected distance visual acuity was also significantly worse at 5 and 8 years than at 1 month postoperatively. In eyes with WTR and oblique astigmatism, the effects of toric IOLs on astigmatism and visual acuity were sustained for 8 years. The long-term astigmatism-correcting effects did not differ among the models of toric IOL used in this study, SN6AT3–8 (Alcon Laboratories). In eyes with preoperative ATR astigmatism, astigmatism-correcting effects of toric IOLs decreased at 5 years and later postoperatively, indicating that overcorrection may be considered at the time of cataract surgery. In eyes with WTR and oblique astigmatism, the effects of toric IOLs were maintained throughout the 8-year follow-up period.
Similar content being viewed by others
Introduction
The efficacy and usefulness of toric intraocular lens (IOL) implantation to reduce or neutralize pre-existing corneal astigmatism at the time of cataract surgery are well addressed1,2. Various factors are known to help improve the surgical outcomes of toric IOLs, such as introduction of sophisticated biometry and lens power calculation formula3,4,5,6,7, advent of image-guided digital marking systems8,9,10,11, refinement of IOL surface finish and design to reduce misalignment after surgery12,13, better understanding of factors that influence postoperative rotational stability of toric IOLs14,15, and widespread use of surgical techniques to minimize surgically induced astigmatism. Longitudinal studies on the results of toric IOLs, however, have been confined to 1- or 2-year follow-up16,17,18,19,20,21,22,23, and long-term outcomes of toric IOLs have not been well studied24. Especially, little is known how long the astigmatism-correcting effects of toric IOLs continue or diminish over years. In addition, long-term changes in visual acuity after toric IOL implantation remain unclear. We conducted the current retrospective study to investigate the time-course of changes in the effects of toric IOLs for 8 years after surgery, in consideration of the influence of preoperative corneal astigmatism type.
Patients and methods
Patients
We retrospectively reviewed the medical records of patients who had undergone phacoemulsification and implantation of a toric IOL for age-related cataract at six surgical sites. Only patients who were followed up for 8 years or longer after surgery were selected. If both eyes of a patient had been operated on, the first-operated eye was included in the analyses. Toric IOLs were indicated for eyes having corneal regular astigmatism of 0.75 diopter or more. Eyes were excluded from the subjects if they had corneal diseases, retinal diseases, glaucoma, uveitis, and other diseases that influence postoperative visual acuity or refraction. Those with a history of ocular surgery other than cataract surgery were also excluded. Eyes that underwent laser capsulotomy for posterior capsule opacification were included. Eyes with significant IOL misalignment > 15 degrees were excluded from analyses. Contact lens users were not included in the subjects.
For the IOL power calculation, the axial length and curvature of corneal anterior surface were measured using the IOLMaster (Carl Zeiss Meditec GmbH). The target refraction was not necessarily emmetropia but determined according to patients' preference. Using the designated manufacturer’s online calculator program, the IOL cylinder power and alignment axis were calculated. The surgically induced astigmatism (SIA) of 0.2–0.4 D was used for calculation.
Since this was a retrospective study, surgical procedures were not standardized before surgery. In general, the following procedures were employed. Preoperatively, with the patients in an upright seated position to avoid cyclotorsion errors, the corneal limbus was marked along the principal meridians at the slit lamp. At the beginning of surgery, the target axis for toric IOL alignment was identified and manually marked with a spatula or marker on the limbus. Following cataract removal through a temporal corneal or sclerocorneal incision, a toric IOL (SN6AT3–8, Alcon Laboratories, Fort Worth, Texas, USA) was implanted in the capsular bag using an injector and rotated to the final position by aligning the reference marks on the IOL with the limbal axis marks. No suture was placed on the incision. Limbal relaxing incision or astigmatic keratotomy was not conducted. Eyes with intraoperative complications were excluded from the subjects. None of the eyes underwent secondary surgical intervention to reposition the toric IOL for the correction of axis misalignment.
The study adhered to the tenets of the Declaration of Helsinki, and the institutional review board of Tsukuba University Hospital approved the study protocol. The committee waived the requirement for patient informed consent regarding the use of their medical record data in accordance with the regulations of the Japanese Guidelines for Epidemiologic Study issued by the Japanese Government. Clinical trial registration was not required owing to the observational nature of the study. All participants were at least 18 years old.
Data analysis
Preoperative keratometry, postoperative manifest astigmatism, and postoperative uncorrected (UDVA) and corrected distance visual acuity (CDVA) were analysed. The preoperative corneal astigmatism was categorized into three types; astigmatism in which the steeper meridian was within ± 30 degrees of the vertical axis was defined as with-the-rule (WTR), astigmatism with the steeper meridian of ± 30 degrees of the horizontal axis was classified as against-the-rule (ATR), and all others were considered to be oblique astigmatism.
Before the data were converted into power vector components, the astigmatic data from the left eye were mirrored horizontally to retain the correct nasal/temporal orientation with the right eye. The preoperative corneal and postoperative refractive astigmatism was decomposed into two components, vertical/horizontal and oblique astigmatism components, using the power vector analysis described by Thibos et al.25. The vertical/horizontal astigmatism component is expressed as the Jackson cross-cylinder, axes at 90 degrees and 180 degrees (J0), and the oblique astigmatism component as the Jackson cross-cylinder, axes at 45 degrees and 135 degrees (J45). A positive J0 represents WTR astigmatism, and a negative J0 indicates ATR astigmatism. A positive J45 shows counter-clockwise oblique astigmatism, while a negative J45 denotes clockwise oblique astigmatism.
Statistical analysis
Numerical data are presented as mean ± standard deviation unless otherwise noted. For assessment of data taken at different time points, the repeated measures analysis of variance (repeated measures ANOVA) was used, followed by a post hoc test with the Bonferroni correction. Comparison of paired variables was conducted using the paired t-test. All statistical tests were 2-sided and a p-value of less than 0.05 was considered significant. Statistical analysis was performed using the SPSS software version 27 (IBM Corp, Armonk, NY).
A pre-study power calculation using a significance level of 5% (α) and a power of 80% (1-β) showed that a sample size of 31–40 would be required to detect a clinically relevant difference in astigmatism between preoperative and postoperative time points. In this calculation, a standard deviation of changes in astigmatism was assumed based on previously published studies24,26.
Results
Astigmatism
Data from 176 eyes of 176 patients were analysed. Their age at the time of cataract surgery was 72.8 ± 8.6 years old and ranged from 42 to 84 years old. Patients’ demographics are summarized in Table 1. The model of toric IOLs used was SN6AT3 in 61 eyes, SN6AT4 in 56 eyes, SN6AT5 in 45 eyes, SN6AT6 in 5 eyes, SN6AT7 in 6 eyes, and SN6AT8 in 3 eyes. The number of eyes examined at each point was 176 preoperatively, 176 at 1 month, 145 at 1 year, 160 at 3 years, 165 at 5 years, and 176 at 8 years postoperatively.
The time course of changes in J0 and J45 are shown in Fig. 1. The mean J0 significantly decreased after surgery (p = 0.002), while mean J45 did not show significant changes (p = 0.902). All postoperative J0 values from 1 month to 8 years were significantly smaller than the preoperative J0 value (p < 0.001).
Time course of changes in astigmatism. Toric IOL implantation significantly decreased J0 (p = 0.002), but not J45 (p = 0.902). When postoperative values from 1 month to 8 years were compared, statistically significant changes were found in J0 (p < 0.001) but not in J45 (p = 0.743). The J0 at 5 years (*p = 0.008) and 8 years (**p < 0.001) were significantly smaller than J0 at 1 month postoperatively.
When postoperative values from 1 month to 8 years were compared, statistically significant changes were found in J0 (p < 0.001), but not in J45 (p = 0.743). The mean J0 at 5 years (p = 0.008) and 8 years (p < 0.001) postoperatively were significantly smaller than the mean J0 at 1 month postoperatively. From 1 month to 8 years after surgery, J0 declined by 0.201 ± 0.563 D. Double-angle plot analyses of preoperative corneal astigmatism and manifest astigmatism at 1 month and 8 years postoperatively are shown in Fig. 2.
Changes in J0 and J45 were analysed in eyes with preoperative WTR (Fig. 3), ATR (Fig. 4), and oblique astigmatism (Fig. 5). Toric IOL implantation significantly reduced preoperative astigmatism in all groups. In eyes with WTR astigmatism, surgery significantly decreased J0 (p < 0.001), but not J45 (p = 0.782). In eyes with ATR astigmatism, J0 significantly increased by surgery (p < 0.001), while no change was found in J45 (p = 0.825). In eyes with oblique astigmatism, surgery induced a significant increase in J45 (p = 0.045), but not in J0 (p = 0.912).
Time course of changes in astigmatism in eyes with preoperative against-the-rule astigmatism. Toric IOL implantation significantly increased J0 (p < 0.001), but not J45 (p = 0.825). When postoperative values were compared, J0 showed significant changes after surgery (p < 0.001), and J0 values at 5 years (*p < 0.001) and 8 years (*p < 0.001) were significantly smaller than that at 1 month postoperatively. The mean J45 remained stable from 1 month to 8 years after surgery (p = 0.964).
Time course of changes in astigmatism in eyes with preoperative oblique astigmatism. Toric IOL implantation significantly increased J45 (p = 0.045), but not J45 (p = 0.912). When postoperative values were compared, J0 (p = 0.972) and J45 (p = 0.189) did not change significantly from 1 month to 8 years.
When postoperative values from 1 month to 8 years were compared, there were no significant fluctuations in J0 (p = 0.511) and J45 (p = 0.679) in eyes with WTR astigmatism (Fig. 3). In eyes with ATR astigmatism (Fig. 4), J0 value showed significant changes after surgery (p < 0.001), and J0 at 5 years (p < 0.001) and 8 years (p < 0.001) postoperatively were significantly smaller than that at 1 month postoperatively. The mean J45 remained steady after surgery (p = 0.964). In eyes with oblique astigmatism (Fig. 5), J0 (p = 0.972) and J45 (p = 0.189) did not fluctuate significantly from 1 month to 8 years after surgery.
Postoperative time course of changes in J0 (Fig. 6) and J45 (Fig. 7) was not significantly different among the models of toric IOLs.
Visual acuity
The time course of changes in UDVA and CDVA after surgery was analysed. Both UDVA (p < 0.001) and CDVA (p < 0.001) showed significant changes after surgery (Fig. 8). UDVA at 5 years (p = 0.004) and 8 years (p < 0.001) postoperatively was significantly worse than UDVA at 1 month postoperatively. CDVA at 5 years (p = 0.001) and 8 years (p < 0.001) after surgery was significantly worse than CDVA at 1 month postoperatively.
Time course of changes in corrected (CDVA) and uncorrected distance visual acuity (UDVA). Both UDVA (p < 0.001) and CDVA (p < 0.001) showed significant changes after surgery. UDVA at 5 years (*p = 0.004) and 8 years (**p < 0.001) postoperatively was significantly worse than UDVA at 1 month postoperatively. CDVA at 5 years (**p < 0.001) and 8 years **(p < 0.001) after surgery was significantly worse than CDVA at 1 month postoperatively. logMAR logarithm of minimum angle of resolution.
Visual acuity changes were analysed in eyes with preoperative WTR (Fig. 9), ATR (Fig. 10), and oblique astigmatism (Fig. 11). In eyes with WTR astigmatism, both UDVA (p = 0.064) and CDVA (p = 0.109) remained stable after surgery. In eyes with oblique astigmatism, postoperative changes in UDVA (p = 0.074) and CDVA (p = 0.113) were not statistically significant.
Time course of changes in uncorrected (UDVA) and corrected distance visual acuity (CDVA) in eyes with preoperative against-the-rule astigmatism. UDVA (p < 0.001) and CDVA (p < 0.001) showed a significant decline after surgery. UDVA at 5 years (*p = 0.009) and 8 years (**p < 0.001) postoperatively was significantly worse than UDVA at 1 month postoperatively. CDVA at 5 years (†p = 0.003) and 8 years (‡p = 0.002) after surgery was significantly worse than CDVA at 1 month postoperatively. logMAR logarithm of minimum angle of resolution.
In eyes with ATR astigmatism (Fig. 10), UDVA (p < 0.001) and CDVA (p < 0.001) showed significant declines after surgery. UDVA at 5 years (p = 0.009) and 8 years (p < 0.001) postoperatively was significantly worse than UDVA at 1 month postoperatively. CDVA at 5 years (p = 0.003) and 8 years (p = 0.002) after surgery was significantly worse than CDVA at 1 month postoperatively. While UDVA considerably deteriorated from 0.051 logMAR (20/22) at 1 month to 0.143 logMAR (20/28) at 8 years, changes in CDVA were minimum from − 0.092 logMAR (20/16) at 1 month to − 0.069 logMAR (20/17) at 8 years. Changes in logMAR UDVA from 1 month to 8 years (0.188 ± 0.014) were significantly larger than those in logMAR CDVA during the same period (0.077 ± 0.006) (p < 0.001).
Postoperative time course of changes in UDVA (Fig. 12) and CDVA (Fig. 13) was not significantly different among the models of toric IOLs.
Discussion
We found that toric IOL implantation significantly reduced pre-existing astigmatism regardless of the type of preoperative corneal astigmatism; by decreasing power vector notation J0 (horizontal/vertical astigmatism component) in eyes with WTR astigmatism, increasing J0 in eyes with ATR astigmatism, and correcting J45 (oblique astigmatism component) in eyes with oblique astigmatism. Long-term astigmatism-correcting effects of toric IOLs, however, varied depending on the type of preoperative astigmatism. In eyes with WTR and oblique astigmatism, postoperative astigmatism remained stable from 1 month to 8 years after surgery. On the other hand, in eyes with ATR astigmatism, there was a constant decline in postoperative J0, and mean J0 at 5 years and later was significantly smaller than that at 1 month postoperatively, indicating a significant ATR astigmatic shift after surgery. From 1 month to 8 years postoperatively, J0 was reduced by 0.201 ± 0.563 D. This result is in good agreement with a previous study by Hayashi et al.27 who reported ATR astigmatic changes of 0.33 D over 10 years after 4.1-mm incision sutureless cataract surgery in patients who were 61.8 ± 6.0 years old at baseline. They also reported that eyes that did not have surgery showed ATR changes of 0.21 D over 10 years from baseline age of 59.9 ± 5.8 years old. Gudmundsdottir et al.28 reported a mean ATR astigmatic change of 0.13 D over 5 years in a normal adult population who were 50 years and older at baseline. Judging from the results of these previous and current studies, long-term changes in astigmatism after small incision cataract surgery appear to represent the physiological ATR astigmatic shift that is commonly associated with aging.
In eyes with preoperative WTR and oblique astigmatism, postoperative changes in power vector notation J0 and J45 were not significant, indicating that astigmatism-correcting effects of toric IOLs in those eyes were maintained at least for 8 years after surgery. Hayashi et al.24 assessed long-term changes in the refractive effect of toric IOL implantation and reported similar results. In eyes with preoperative ATR astigmatism, manifest refractive and corneal astigmatism significantly changed toward ATR astigmatism during the 6.6-year follow-up period24. In eyes with preoperative WTR astigmatism, manifest refractive and corneal astigmatism did not change significantly for 6.8 years after surgery. Eyes with oblique astigmatism were not included in their study. Longer-term outcomes of toric IOL implantation, however, such as ≥ 10 years remain unknown. In fact, the J0 curve in Fig. 3 and J45 curve in Fig. 5 in the current study imply that astigmatism-correcting effects of toric IOLs may eventually wane if more extensive studies in terms of both length of the follow-up period and number of subjects are conducted. This would be the subject of future studies.
Until now, long-term time-course of changes in visual acuity after toric IOL implantation have not been well studied. We found that the overall trends of postoperative visual acuity were similar to those of postoperative astigmatic changes aforementioned. In eyes with preoperative WTR and oblique astigmatism, postoperative UDVA and CDVA remained steady from 1 month to 8 years. On the other hand, in eyes with preoperative ATR astigmatism, both UDVA and CDVA significantly deteriorated at 5 years and later after surgery. In particular, changes in UDVA were more prominent than those in CDVA. While UDVA considerably declined from 0.051 logMAR (20/22) at 1 month to 0.143 logMAR (20/28) at 8 years, changes in CDVA were minimum from − 0.092 logMAR (20/16) at 1 month to − 0.069 logMAR (20/17) at 8 years. Changes from 1 month to 8 years were significantly larger in UDVA than in CDVA. From the current results alone, it is impossible to determine the exact mechanism of action underlying deterioration of UDVA and CDVA after surgery. Especially, changes in regular astigmatism cannot explain the worsening of CDVA. We assume that deterioration of UDVA reflects the long-term ATR astigmatic shifts, while changes in CDVA may be attributable to, at least in part, aging changes in visual function including undetected retinal pathologies29,30 and increases in irregular corneal astigmatism31,32. It has been reported that corneal irregular astigmatism as measured by corneal topography was significantly larger in eyes with ATR astigmatism than in those with WTR astigmatism33.
Six models of toric IOLs were used in the current study, SN6AT3–8. The postoperative time course of changes in the power vector notation J0 (Fig. 6) and J45 (Fig. 7) did not differ significantly among the different models of toric IOL. Similarly, postoperative UDVA (Fig. 12) and CDVA (Fig. 13) were not significantly different among toric IOL models. Thus, all models of toric IOLs used in the current study were almost equally effective to treat cataract patients with pre-existing astigmatism. Xiao et al.34 demonstrated that the optical quality after surgery was not significantly different among eyes that received toric IOLs with a different cylinder power, SN60T3 to T6. Bauer et al.35 showed comparable surgical outcomes after implantation of SN60T3 to T5. In the current study, we also confirmed that toric IOLs SN6AT3 to AT8 provided comparable and satisfactory long-term clinical outcomes.
There were several limitations to the current study. First, because this study was conducted in a retrospective manner, several important data were missing, such as amount of toric IOL axis misalignment, postoperative keratometry, and corneal topography to evaluate irregular astigmatism. In addition, although eyes with apparent ocular disorders were excluded, the judgement was based only on the retrospective chart review. Second, number of eyes with preoperative oblique astigmatism was small, and thus the statistical analyses in that group may have been underpowered. Similarly, number of eyes with higher toricity IOLs, such as SN6AT6–8, is limited, yielding insufficient statistical power in these subgroups.
In conclusion, long-term surgical outcomes of cataract surgery with toric IOL implantation were investigated. Preoperative corneal and postoperative manifest astigmatism was converted to power vector notations J0 (horizontal/vertical component) and J45 (oblique component). In eyes with preoperative WTR and oblique astigmatism, the astigmatism-correcting effects continued during the 8-year follow-up period. In eyes with preoperative ATR astigmatism, postoperative astigmatism showed an ATR shift, and J0 at 5 and 8 years postoperatively was significantly lower than that at 1 month postoperatively. Visual acuity, especially UDVA, at 5 and 8 years after surgery was significantly worse than that at 1 month after surgery. Given these long-term trends, surgeons may consider overcorrection of astigmatism in eyes with preoperative ATR astigmatism at the time of cataract surgery using toric IOLs.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kessel, L. et al. Toric intraocular lenses in the correction of astigmatism during cataract surgery: A systematic review and meta-analysis. Ophthalmology 123, 275–286 (2016).
Xue, K. et al. Real-world refractive outcomes of toric intraocular lens implantation in a United Kingdom National Health Service setting. BMC Ophthalmol. 18, 30 (2018).
Abulafia, A. et al. New regression formula for toric intraocular lens calculations. J. Cataract Refract. Surg. 42, 663–671 (2016).
Canovas, C. et al. New algorithm for toric intraocular lens power calculation considering the posterior corneal astigmatism. J. Cataract Refract. Surg. 44, 168–174 (2018).
Skrzypecki, J., Sanghvi Patel, M. & Suh, L. H. Performance of the Barrett Toric Calculator with and without measurements of posterior corneal curvature. Eye (London) 33, 1762–1767 (2019).
Kane, J. X. & Connell, B. A comparison of the accuracy of 6 modern toric intraocular lens formulas. Ophthalmology 127, 1472–1486 (2020).
Yang, S., Byun, Y. S., Kim, H. S. & Chung, S. H. Comparative accuracy of Barrett Toric Calculator with and without posterior corneal astigmatism measurements and the Kane Toric formula. Am. J. Ophthalmol. 231, 48–57 (2021).
Webers, V. S. C. et al. Image-guided system versus manual marking for toric intraocular lens alignment in cataract surgery. J. Cataract Refract. Surg. 43, 781–788 (2017).
Mayer, W. J. et al. Comparison of visual outcomes, alignment accuracy, and surgical time between 2 methods of corneal marking for toric intraocular lens implantation. J. Cataract Refract. Surg. 43, 1281–1286 (2017).
Titiyal, J. S. et al. Comparative evaluation of toric intraocular lens alignment and visual quality with image-guided surgery and conventional three-step manual marking. Clin. Ophthalmol. 12, 747–753 (2018).
Zhou, F. et al. Comparative meta-analysis of toric intraocular lens alignment accuracy in cataract patients: Image-guided system versus manual marking. J. Cataract Refract. Surg. 45, 1340–1345 (2019).
Osawa, R., Oshika, T., Sano, M., Yuguchi, T. & Kaiya, T. Rotational stability of modified toric intraocular lens. PLoS ONE 16, e0247844 (2021).
Takaku, R., Nakano, S., Iida, M. & Oshika, T. Influence of frosted haptics on rotational stability of toric intraocular lenses. Sci. Rep. 11, 15099 (2021).
Zhu, X., He, W., Zhang, K. & Lu, Y. Factors influencing 1-year rotational stability of AcrySof Toric intraocular lenses. Br. J. Ophthalmol. 100, 263–268 (2016).
Sasaki, K. et al. Anterior capsule coverage and rotational stability of an acrylic toric intraocular lens. J. Cataract Refract. Surg. 47, 618–621 (2021).
Kwartz, J. & Edwards, K. Evaluation of the long-term rotational stability of single-piece, acrylic intraocular lenses. Br. J. Ophthalmol. 94, 1003–1006 (2010).
Kim, M. H., Chung, T. Y. & Chung, E. S. Long-term efficacy and rotational stability of AcrySof toric intraocular lens implantation in cataract surgery. Korean J. Ophthalmol. 24, 207–212 (2010).
Miyake, T. et al. Long-term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. J. Cataract Refract. Surg. 40, 1654–1660 (2014).
Ninomiya, Y. et al. Toric intraocular lenses in eyes with with-the-rule, against-the-rule, and oblique astigmatism: One-year results. J. Cataract Refract. Surg. 42, 1431–1440 (2016).
Gyöngyössy, B., Jirak, P. & Schönherr, U. Long-term rotational stability and visual outcomes of a single-piece hydrophilic acrylic toric IOL: A 1.5-year follow-up. Int. J. Ophthalmol. 10, 573–578 (2017).
Fernández-Muñoz, E. et al. Long-term refractive outcomes in patients with cataracts and keratoconus after phacoemulsification with toric intraocular lens implant. Eur. J. Ophthalmol. 31, 1532–1539 (2021).
Zhong, H., Qin, H., Wang, H. J. & Wang, Z. Y. Objective visual quality one year after toric IOL implantation for correction of moderate and high corneal astigmatism. Int. J. Ophthalmol. 14, 245–249 (2021).
Nováček, L. V. et al. Evaluation of astigmatism-correcting efficiency and rotational stability after cataract surgery with a double-loop haptic toric intraocular lens: A 1-year follow-up. Biomed. Hub 6, 30–41 (2021).
Hayashi, K., Yoshida, M., Hayashi, S. & Hirata, A. Long-term changes in the refractive effect of a toric intraocular lens on astigmatism correction. Graefes Arch. Clin. Exp. Ophthalmol. 260, 509–519 (2022).
Thibos, L. N. & Horner, D. Power vector analysis of the optical outcome of refractive surgery. J. Cataract Refract. Surg. 27, 80–85 (2001).
Inoue, Y. et al. Impact of small incision sutureless cataract surgery on the natural course of astigmatism in 10 to 20 years. J. Cataract Refract. Surg. https://doi.org/10.1097/j.jcrs.0000000000000941 (2022).
Hayashi, K., Manabe, S. I., Hirata, A. & Yoshimura, K. Changes in corneal astigmatism during 20 years after cataract surgery. J. Cataract Refract. Surg. 43, 615–621 (2017).
Gudmundsdottir, E., Arnarsson, A. & Jonasson, F. Five-year refractive changes in an adult population: Reykjavik Eye Study. Ophthalmology 112, 672–677 (2005).
Neely, D. C. et al. Prevalence of undiagnosed age-related macular degeneration in primary eye care. JAMA Ophthalmol. 135, 570–575 (2017).
Lemmens, S. et al. The prevalence of undiagnosed age-related sight-threatening diseases in self-proclaimed healthy individuals. J. Ophthalmol. 2020, 3709793 (2020).
Oshika, T., Klyce, S. D., Applegate, R. A. & Howland, H. C. Changes in corneal wavefront aberrations with aging. Investig. Ophthalmol. Vis. Sci. 40, 1351–1355 (1999).
Kemraz, D. et al. Age-related changes in corneal spherical aberration. J. Refract. Surg. 34, 760–767 (2018).
Ueno, Y. et al. Comparison of corneal irregular astigmatism by the type of corneal regular astigmatism. Sci. Rep. 11, 15769 (2021).
Xiao, X. W., Hao, J., Zhang, H. & Tian, F. Optical quality of toric intraocular lens implantation in cataract surgery. Int. J. Ophthalmol. 8, 66–71 (2015).
Bauer, N. J., de Vries, N. E., Webers, C. A., Hendrikse, F. & Nuijts, R. M. Astigmatism management in cataract surgery with the AcrySof toric intraocular lens. J. Cataract Refract. Surg. 34, 1483–1488 (2008).
Author information
Authors and Affiliations
Contributions
T.O., S.N., and Y.I. designed the study described here. T.O., S.N., Y.F., Y.N., Y.I., H.T., K.M., M.H., T.S., and T.K. recruited participants and collected data. T.O. performed statistical analyses, drafted the main manuscript text, and prepared figures. All authors reviewed and revised the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
Dr. Tetsuro Oshika received compensation as a consultant from Alcon, Johnson & Johnson Vision, Santen Pharmaceutical, and Mitsubishi Tanabe. He receives research support from Santen Pharmaceutical, Tomey, Alcon, Senju Pharmaceutical, Johnson & Johnson Vision, HOYA, KOWA Pharmaceutical, Otsuka Pharmaceutical, Novartis, Pfizer, and Topcon. Other authors do not have any conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oshika, T., Nakano, S., Fujita, Y. et al. Long-term outcomes of cataract surgery with toric intraocular lens implantation by the type of preoperative astigmatism. Sci Rep 12, 8457 (2022). https://doi.org/10.1038/s41598-022-12426-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12426-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.