Abstract
Disease progression (DP) is an important parameter for the prognosis of idiopathic pulmonary fibrosis (IPF). This study aimed to evaluate the baseline serum biomarkers for predicting the DP in IPF. Seventy-four patients who were diagnosed with IPF and had their serum Krebs von den Lungen-6 (KL-6) and monocyte count, which might be associated with prognosis of IPF, checked more than twice were included. KL-6 ≥ 1000 U/mL and monocyte ≥ 600/μL were arbitrarily set as the cut-off values for DP. The DP was defined as a 10% reduction in forced vital capacity, a 15% reduction in diffusing capacity of the lung for carbon monoxide relative to the baseline, or disease-related mortality. Of the 74 patients, 18 (24.3%) were defined as having DP. The baseline KL-6 level was significantly increased in the DP group compared to the stable disease group (median, 1228.0 U/mL vs. 605.5 U/mL, P = 0.019). Multivariate Cox analyses demonstrated that a high KL-6 level (KL-6 ≥ 1000 U/mL; hazard ratio, 2.761 or 2.845; P = 0.040 or 0.045) was independently associated with DP in each model. The baseline serum KL-6 level might be a useful biomarker for DP in IPF.
Similar content being viewed by others
Introduction
Idiopathic pulmonary fibrosis (IPF) is a specific form of chronic, progressive, fibrosing interstitial pneumonia of unknown cause1. Although patients with IPF have a poor prognosis, with a median survival of 3–5 years, the clinical courses of these patients are highly variable2,3. Various clinical parameters are known to predict the prognosis of IPF, including older age, smoking history, lower body mass index (BMI), poorer lung function, greater disease extent, and various comorbidities4.
Among these parameters, physiologic parameters that can be obtained from the pulmonary function test (PFT) provide crucial information for managing patients with IPF5. Several studies have shown that disease progression (DP), which is defined as a decline in lung volume (forced vital capacity [FVC]) and/or a decline in gas exchange (diffusing capacity of the lung for carbon monoxide [DLco]) is associated with poor prognosis in patients with IPF4,6. Indeed, these physiologic parameters served as the primary end-point in previous clinical trials of anti-fibrotic agents7,8.
Blood biomarkers have been shown to emerging evidence in patients with IPF in clinical practice9,10. Several blood biomarkers, including lung-epithelium specific proteins, chemokines, growth factors, proteases, and other serological markers, have been studied widely in the fields of diagnosis, disease severity, and prognosis in patients with IPF11,12,13. Among them, Krebs von den Lungen-6 (KL-6) is used in clinical practice and elevated level of KL-6 is known to predict mortality in patients with IPF14,15,16,17. Recently, increased monocyte count is reported to be associated with poor outcomes in patients with IPF18,19,20,21. However, the role of biomarkers in predicting the DP of patients with IPF is ill-defined. Additionally, the majority of studied biomarkers are difficult to use in real world clinical practice. Therefore, this study evaluated the predictive values of serum biomarkers, including KL-6 and monocyte count, for predicting the DP in IPF.
Results
Baseline characteristics
Eighteen patients (24.3%) were classified as having DP according to the abovementioned criteria. The median follow-up period was 9 months. The mean age of the patients was 67.9 years, 67 patients (90.5%) were male, and 65 patients (87.8%) had smoking history. The DP group had a higher level of baseline KL-6 (median 1228.0 vs. 605.5 U/mL, P = 0.019) than the stable disease (SD) group (n = 56). However, there was no significant difference in baseline monocyte count between the DP and SD group (median 633.0 vs. 596.5/μL, P = 0.427). Additionally, there were no significant differences between the two groups in demographics, lung function, and exercise capacity (Table 1). As for anti-fibrotic medications, 64 patients (86.5%), 1 patient (1.4%), and 1 patient (1.4%) were prescribed pirfenidone, nintedanib, and both pirfenidone and nintedanib, respectively (data not shown).
The baseline characteristics of the high KL-6 level (≥ 1000 U/mL) group and the low KL-6 level (< 1000 U/mL) group are shown in Table 2. The high KL-6 group had higher monocyte count (median 660.0 vs. 567.0/μL, P = 0.030), lower DLco (47.6 vs. 60.0%, P = 0.004), and lower O2 saturation in the 6-min walk test (6MWT) (87.6 vs. 93.0%, P = 0.001) than the low KL-6 group. However, there was no significant difference between the two groups in demographics and other lung function and exercise capacity.
Correlations between baseline biomarkers and lung function
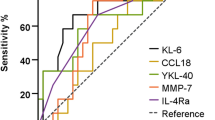
Baseline KL-6 levels were inversely correlated with FVC (r = − 0.238, P = 0.041), DLco (r = − 0.437, P < 0.001), and total lung capacity (TLC) (r = − 0.373, P = 0.007). The baseline KL-6 levels were not correlated with 6MWT distance (r = − 0.137, P = 0.323), while the baseline monocyte counts were inversely correlated with DLco (r = − 0.330, P = 0.004), but not with FVC, TLC, and 6MWT distance (Fig. 1).
Risk factors for disease progression
Univariate analysis demonstrated that a high KL-6 level (≥ 1000 U/mL) was significantly associated with DP, while a high monocyte count (≥ 600/μL) was not. Multivariate analysis demonstrated that a high KL-6 level was independently associated with DP (hazard ratio, 2.761; 95% confidence interval, 1.048–7.273; P = 0.040), after adjusting for BMI. When including clinically significant variables, multivariate analysis demonstrated that a high KL-6 level was independently associated with DP (hazard ratio, 2.845; 95% confidence interval, 1.023–7.912; P = 0.045), after adjusting for age, sex, BMI, forced expiratory volume at 1 s (FEV1), FVC, and DLCO (Table 3). The Kaplan–Meier curve demonstrated that the high KL-6 group showed a higher risk of DP than the low KL-6 group (P = 0.032, Fig. 2). However, the high monocyte count group showed no significant differences from the low monocyte count group (P = 0.440).
We also compared lung function between the increased KL-6 group and the non-increased KL-6 group to determine whether the interval change of KL-6 level is associated with DP. The increased KL-6 group (n = 34) and the non-increased KL-6 group (n = 26) showed no significant differences in the proportion of DP (P = 0.817, Table 4). Moreover, the serially measured lung functions at the 3rd, 6th, and 9th months from baseline were not significantly different between the groups (FVC; P = 0.590, DLco; P = 0.964, Fig. 3).
Discussion
In the current study, the baseline serum KL-6 levels increased in the DP group compared to the SD group in patients with IPF. The baseline serum KL-6 level was independently associated with DP in multivariate analysis. These findings suggest that the baseline serum KL-6 level might be a useful predictive marker for the DP in IPF.
Previous studies have reported that several factors are associated with mortality in IPF, including age, sex, smoking status, dyspnea, BMI, pulmonary hypertension, PFT, 6MWT, and serum and bronchoalveolar lavage fluid biomarkers4,22. Among these factors, declined lung function is one of the best surrogate markers for disease-related mortality in IPF23. In particular, FVC and DLCO are the only physiologic variables in the IPF staging system GAP index24 and they are also used for defining the DP in IPF22. Thus, FVC and DLCO are considered to be good indicators of lung function and prognosis in IPF. As a result, reducing the decline of FVC is an important goal in IPF treatment and is regarded as the primary outcome of studies on anti-fibrotic drugs7,8. However, few studies have focused on the predictors of DP in IPF, especially using biomarkers.
Biomarkers might have advantages in reproducibility because they are less influenced by patients’ general conditions or examiners’ variations. Many potential biomarkers have been studied, including KL-6, SP-A, SP-D, MMPs, and CCLs9,10,11,12,13. Among them, KL-6 is well established and used in clinical practice14,15,16,17. KL-6 is a mucin-like glycoprotein and is strongly expressed on the surface of type II pneumocytes, which are regenerated over the alveolar basement membrane after the death of type I pneumocytes during the lung injury in interstitial lung disease25. Patients with IPF with an elevated level of KL-6 (KL-6 > 1000 U/mL) are known to have increased mortality compared to patients with a KL-6 level within the normal range17,26. In this study, baseline KL-6 ≥ 1000 U/mL was significantly associated with the DP in IPF, suggesting that KL-6 might act as a surrogate marker for DP in IPF.
There are conflicting studies regarding the values of serial changes in serum KL-6 levels for the prognosis in IPF. Wakamatsu et al. reported that patients with increased serum KL-6 levels during follow-up had significant decline in FVC compared to those with no KL-6 increase15. d’Alessandro et al. also showed that patients with persistently elevated KL-6 had decreased FVC, whereas patients with decreased KL-6 had preserved FVC27. However, Ishii et al. suggested that a reduction in serum KL-6 level with untreated IPF does not indicate stable IPF status, but DP in IPF with a natural decline in serum KL-6 level28. It is possible that the serum KL-6 level reflects the extent of damaged alveolar epithelium25 rather than the degree of disease activity. In this study, the increased KL-6 group showed no significant difference in DP and lung function compared to the non-increased KL-6 group. Therefore, our results suggest that patients with high level of baseline serum KL-6 should be considered to have the higher possibility of DP regardless of the follow-up serum KL-6 level. However, it should be considered that patients with severely deteriorated lung function, including deceased, could not perform follow-up lung function test, and therefore may not have been included in the analysis. Further studies will be needed for the serial measurement of KL-6 level.
Monocytes are the largest type of white blood cell. Monocytes can migrate from blood vessels into tissues, where they differentiate into macrophages and dendritic cells29. Monocyte-derived alveolar macrophages can contribute to lung fibrosis, whereas tissue-resident macrophages do not contribute to fibrosis30. An increased monocyte count is associated with poor outcomes in IPF and other fibrotic diseases, including systemic sclerosis, hypertrophic cardiomyopathy, or myelofibrosis18. However, the optimal cut-off value of monocyte count for the prognosis of IPF is still debated. Scott et al. and Teoh et al. reported that a monocyte count ≥ 950/μL was associated with mortality in IPF18,19. Karampitsakos et al. suggested that a monocyte count ≥ 600/μL was related to lower lung function and higher all-cause mortality20. Kreuter et al. showed that a monocyte count ≥ 600/μL was associated with increased risks of IPF progression, all-cause hospitalization, and all-cause mortality21. Considering the results of previous studies, and the fact that only six patients (8%) had a monocyte count ≥ 950/μL in our study, we arbitrarily set a monocyte count ≥ 600/μL as the cut-off value. However, the high monocyte count was not associated with the DP in IPF in our data, possibly because our sample size was small to validate it or because of the influence of other situations, including other co-incidental infections.
This study has some limitations. First, this was a single-center, retrospective, nonrandomized study which might induce a selection bias. Second, the monocyte count was calculated by white blood cell differential on complete blood count (CBC) rather than flow cytometry, so the calculated monocyte count may differ from the real value. However, previous studies checked the monocyte count calculated by white blood cell differential on CBC and showed the associations between the monocyte count and the prognosis in IPF20,21. Third, the follow-up periods were relatively short, with a median follow-up of 9 months. However, approximately one-fourth of patients were classified as having DP, which was sufficient compared to previous studies14,17. Fourth, subgroup analysis according to the anti-fibrotic medication profile could not be performed due to our small sample. Despite these limitations, our study revealed the clinical role of KL-6 in predicting DP of patients with IPF.
This real-world population analysis suggests that elevated baseline serum KL-6 level might predict the DP in IPF and it could be a useful biomarker in clinical practice.
Methods
Study population
Seventy-four patients who were diagnosed with IPF and had their KL-6 and monocyte count checked more than twice between January 2020 and June 2021 at Asan Medical Center, Seoul, Republic of Korea were included in this study. All patients underwent thorough systemic history taking. Patients with definite connective tissue disease or an exposure history in relation to the possible causes of interstitial lung disease were excluded. IPF diagnosis was performed by a multidisciplinary approach, using the diagnostic criteria set by the American Thoracic Society (ATS)/European Respiratory Society (ERS)/Japanese Respiratory Society/Latin American Thoracic Association in 20181. All available baseline clinical parameters were obtained within 3 months of the initial blood sampling time. The study protocol was approved by the Institutional Review Board of Asan Medical Center (approval number: 2021–0787). The requirement for informed consent was waived because of the retrospective study design. The present study complied with the Declaration of Helsinki and all methods were performed in accordance with the relevant guidelines and regulations.
Serum biomarkers
As biomarkers, serum KL-6 and monocyte count were evaluated in this study. The serum KL-6 concentration was measured using a Nanopia KL-6 assay (SEKISUI MEDICAL, Tokyo) using a latex-enhanced immunoturbidimetric assay method. The monocyte count was calculated using white blood cell differential on CBC. Serum KL-6 ≥ 1000 U/mL is well known to predict poor prognosis in IPF, and, as such, was set as the cut-off value in this study15,17,26. However, the optimal cut-off value of monocytes has not yet been validated. Therefore, we arbitrarily set monocytes ≥ 600/μL as a cut-off value based on recent studies20,21. Moreover, to determine whether the interval change in KL-6 level is related to DP, we divided patients into two groups according to the KL-6 level at the 3rd month from the baseline. Patients who had increased KL-6 levels at the 3rd month compared to baseline level were classified as the increased KL-6 group, and other patients were classified as the non-increased KL-6 group.
Disease progression
Spirometry, DLco, and TLC were measured according to the ERS/ATS recommendations31,32. The 6MWT was performed according to the ERS/ATS guidelines33. Baseline was defined as the time when the patients were diagnosed as IPF in our center. Patients visited outpatient clinic approximately every three months and KL-6, CBC, PFT, and 6MWT were performed at every visit as possible. Data collection closing date was June 31, 2021 and at this point, the last clinical data were compared to those of baseline. DP was defined as a 10% reduction in FVC and/or a 15% reduction in DLCO relative to baseline, or disease-related mortality22. If the patient did not meet the DP criteria, the patient was considered to have SD.
Statistical analysis
Continuous variables are presented as means (standard deviation) or median (interquartile range), and categorical variables are expressed as numbers (percentages). Student’s t-test or Mann–Whitney test was used to compare continuous variables, and the χ2 test or Fisher’s exact test was used to compare categorical variables. Correlation analyses using Spearman’s rank correlation coefficients were performed to evaluate the relationship between biomarker levels and lung function. Cox proportional hazard analysis was used to identify risk factors for DP. Variables with P-values < 0.2 on univariate analysis and clinically significant variables were entered into the multivariate models. The period from the time of initial blood sampling to the time of DP was evaluated using Kaplan–Meier survival analysis and the log-rank test. All P-values were two-tailed, with statistical significance set at P < 0.05. All statistical analyses were performed using SPSS software (version 26.0; Statistical Package for the Social Sciences, IBM Corporation, Armonk, NY, USA).
Ethics declarations
The study protocol was approved by the Institutional Review Board of Asan Medical Center (approval number 2021–0787). The requirement for informed consent was waived because of the retrospective study design. The present study complied with the Declaration of Helsinki and all methods were performed in accordance with the relevant guidelines and regulations.
References
Raghu, G. et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am. J. Respir. Crit. Care Med. 198, e44–e68. https://doi.org/10.1164/rccm.201807-1255ST (2018).
Martinez, F. J. et al. The clinical course of patients with idiopathic pulmonary fibrosis. Ann. Intern. Med. 142, 963–967. https://doi.org/10.7326/0003-4819-142-12_part_1-200506210-00005 (2005).
Kim, D. S. Acute exacerbations in patients with idiopathic pulmonary fibrosis. Respir. Res. 14, 86. https://doi.org/10.1186/1465-9921-14-86 (2013).
Collard, H. R. et al. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 168, 538–542. https://doi.org/10.1164/rccm.200211-1311OC (2003).
Egan, J. J., Martinez, F. J., Wells, A. U. & Williams, T. Lung function estimates in idiopathic pulmonary fibrosis: The potential for a simple classification. Thorax 60, 270–273. https://doi.org/10.1136/thx.2004.035436 (2005).
Hanson, D., Winterbauer, R. H., Kirtland, S. H. & Wu, R. Changes in pulmonary function test results after 1 year of therapy as predictors of survival in patients with idiopathic pulmonary fibrosis. Chest 108, 305–310. https://doi.org/10.1378/chest.108.2.305 (1995).
King, T. E. Jr. et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N. Engl. J. Med. 370, 2083–2092. https://doi.org/10.1056/NEJMoa1402582 (2014).
Richeldi, L. et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N. Engl. J. Med. 370, 2071–2082. https://doi.org/10.1056/NEJMoa1402584 (2014).
Guiot, J., Moermans, C., Henket, M., Corhay, J. L. & Louis, R. Blood biomarkers in idiopathic pulmonary fibrosis. Lung 195, 273–280. https://doi.org/10.1007/s00408-017-9993-5 (2017).
Stainer, A. et al. Molecular biomarkers in idiopathic pulmonary fibrosis: State of the art and future directions. Int. J. Mol. Sci. 22, 6255. https://doi.org/10.3390/ijms22126255 (2021).
Rosas, I. O. et al. MMP1 and MMP7 as potential peripheral blood biomarkers in idiopathic pulmonary fibrosis. PLoS Med. 5, e93. https://doi.org/10.1371/journal.pmed.0050093 (2008).
Song, J. W. et al. Blood biomarkers MMP-7 and SP-A: Predictors of outcome in idiopathic pulmonary fibrosis. Chest 143, 1422–1429. https://doi.org/10.1378/chest.11-2735 (2013).
Machahua, C. et al. Serum calprotectin as new biomarker for disease severity in idiopathic pulmonary fibrosis: A cross-sectional study in two independent cohorts. BMJ Open Respir. Res. 8, e000827. https://doi.org/10.1136/bmjresp-2020-000827 (2021).
Ohshimo, S. et al. Baseline KL-6 predicts increased risk for acute exacerbation of idiopathic pulmonary fibrosis. Respir. Med. 108, 1031–1039. https://doi.org/10.1016/j.rmed.2014.04.009 (2014).
Wakamatsu, K. et al. Prognostic value of serial serum KL-6 measurements in patients with idiopathic pulmonary fibrosis. Respir. Investig. 55, 16–23. https://doi.org/10.1016/j.resinv.2016.09.003 (2017).
Jiang, Y. et al. Sequential changes of serum KL-6 predict the progression of interstitial lung disease. J. Thorac Dis. 10, 4705–4714. https://doi.org/10.21037/jtd.2018.07.76 (2018).
Satoh, H., Kurishima, K., Ishikawa, H. & Ohtsuka, M. Increased levels of KL-6 and subsequent mortality in patients with interstitial lung diseases. J. Intern. Med. 260, 429–434. https://doi.org/10.1111/j.1365-2796.2006.01704.x (2006).
Scott, M. K. D. et al. Increased monocyte count as a cellular biomarker for poor outcomes in fibrotic diseases: A retrospective, multicentre cohort study. Lancet Respir. Med. 7, 497–508. https://doi.org/10.1016/S2213-2600(18)30508-3 (2019).
Teoh, A. K. Y. et al. Blood monocyte counts as a potential prognostic marker for idiopathic pulmonary fibrosis: Analysis from the Australian IPF registry. Eur. Respir. J. https://doi.org/10.1183/13993003.01855-2019 (2020).
Karampitsakos, T. et al. Increased monocyte count and red cell distribution width as prognostic biomarkers in patients with Idiopathic Pulmonary Fibrosis. Respir. Res. 22, 140. https://doi.org/10.1186/s12931-021-01725-9 (2021).
Kreuter, M. et al. Monocyte count as a prognostic biomarker in patients with idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 204, 74–81. https://doi.org/10.1164/rccm.202003-0669OC (2021).
Ley, B., Collard, H. R. & King, T. E. Jr. Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 183, 431–440. https://doi.org/10.1164/rccm.201006-0894CI (2011).
du Bois, R. M. et al. Forced vital capacity in patients with idiopathic pulmonary fibrosis: Test properties and minimal clinically important difference. Am. J. Respir. Crit. Care Med. 184, 1382–1389. https://doi.org/10.1164/rccm.201105-0840OC (2011).
Ley, B. et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann. Intern. Med. 156, 684–691. https://doi.org/10.7326/0003-4819-156-10-201205150-00004 (2012).
Ishikawa, N., Hattori, N., Yokoyama, A. & Kohno, N. Utility of KL-6/MUC1 in the clinical management of interstitial lung diseases. Respir. Investig. 50, 3–13. https://doi.org/10.1016/j.resinv.2012.02.001 (2012).
Yokoyama, A. et al. Prognostic value of circulating KL-6 in idiopathic pulmonary fibrosis. Respirology 11, 164–168. https://doi.org/10.1111/j.1440-1843.2006.00834.x (2006).
d’Alessandro, M. et al. Serum concentrations of KL-6 in patients with IPF and lung cancer and serial measurements of KL-6 in IPF patients treated with antifibrotic therapy. Cancers 13, 689. https://doi.org/10.3390/cancers13040689 (2021).
Ishii, H., Kushima, H., Kinoshita, Y., Fujita, M. & Watanabe, K. The serum KL-6 levels in untreated idiopathic pulmonary fibrosis can naturally decline in association with disease progression. Clin. Respir. J. 12, 2411–2418. https://doi.org/10.1111/crj.12946 (2018).
Swirski, F. K. et al. Identification of splenic reservoir monocytes and their deployment to inflammatory sites. Science 325, 612–616. https://doi.org/10.1126/science.1175202 (2009).
Misharin, A. V. et al. Monocyte-derived alveolar macrophages drive lung fibrosis and persist in the lung over the life span. J. Exp. Med. 214, 2387–2404. https://doi.org/10.1084/jem.20162152 (2017).
Macintyre, N. et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur. Respir. J. 26, 720–735. https://doi.org/10.1183/09031936.05.00034905 (2005).
Wanger, J. et al. Standardisation of the measurement of lung volumes. Eur. Respir. J. 26, 511–522. https://doi.org/10.1183/09031936.05.00035005 (2005).
Holland, A. E. et al. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 44, 1428–1446. https://doi.org/10.1183/09031936.00150314 (2014).
Acknowledgements
We thank Kyungil Medical Inc. for providing advice and substantive comments on an earlier draft of this study.
Author information
Authors and Affiliations
Contributions
C.C., J.K., and H.C.K. conceived the conception of this study and its design. C.C., J.K., and H.S.C. collected the data and contributed to the data analysis. C.C. and H.C.K. drafted the manuscript. All authors revised and approved the final manuscript. All authors vouch for the accuracy of the content included in the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chung, C., Kim, J., Cho, H.S. et al. Baseline serum Krebs von den Lungen-6 as a biomarker for the disease progression in idiopathic pulmonary fibrosis. Sci Rep 12, 8564 (2022). https://doi.org/10.1038/s41598-022-12399-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12399-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.