Abstract
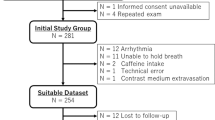
Dobutamine stress echocardiography is an alternative method to exercise stress echocardiography for the evaluation of ischemia. Recently, the novel speckle tracking imaging derived parameter, myocardial work index, was suggested for the evaluation of cardiac performance and was evaluated during exercise stress echocardiography. In this study, we analyzed the effect of dobutamine on myocardial work index variables during normal dobutamine stress echocardiography. Echocardiography examinations of patients with normal dobutamine stress echocardiography were collected and underwent off-line speckle tracking imaging analysis. Myocardial work index parameters were calculated at each dose of dobutamine and compared. 286 patients underwent dobutamine stress echocardiography during the study period. 102 patients were excluded due to pre-existed coronary artery disease or ischemia at dobutamine stress echocardiography. 65 patients were excluded due to suboptimal image quality unsuitable for speckle tracking imaging analysis. The remaining 119 patients with normal results were included. The global work index decreased from 2393.3 to 1864.7 mmHg%, p < 0.0004. Global constructive work decreased from 2681.7 to 2152.6 mmHg%, p = 0.001. Global wasted work increased from 78.8 to 128.3 mmHg%, p < 0.003. Global work efficacy decreased from 96.1 to 91.9%, p < 0.00001. Global strain increased from—19.6 to − 23.7%, p < 0.00001. Dobutamine stress echocardiography results in a decrease of all specific myocardial work index parameters even in normal subjects. Only global myocardial strain improved.
Similar content being viewed by others
Introduction
Dobutamine stress echocardiography (DSE) allows dynamic evaluation of cardiac function during pharmacological stimulation of heart rate, cardiac output, and myocardial oxygen demand. Diagnosis of ischemia is done by visual comparison of left ventricular contraction during dobutamine infusion. In contrast, to exercise stress echocardiography, dobutamine stress echocardiography isn’t expected to provide physiological information. Diagnostic accuracy of dobutamine stress echocardiography is determined by sensitivity for detection of coronary artery disease 61–96%, and specificity 70–100%1. Visual assessment of contractility is based on the evaluation of wall thickening that’s subjective and often completely depends on the experience of the interpreting physician. Recently, few studies evaluated cardiac mechanics during dobutamine stress echocardiography2,3,4 using speckle tracking imaging. The applicability of speckle tracking imaging in dobutamine stress echocardiography is limited by high heart rates. Recently a new speckle tracking imaging parameter, the myocardial work index was introduced5. To better understand the physiology of dobutamine stress echocardiography, we applied speckle tracking imaging, in particular a myocardial work index, in patients with normal dobutamine stress echocardiography.
Materials and methods
Digital files of the patients that undergo dobutamine stress echocardiography examination were examined. All echocardiography exams were performed using Vivid E95, (General Electric) with a standard transducer of 1.7–4 Hz. Frame rate during dobutamine stress echocardiography examinations was in a range of 50–70 fps. Studies with normal results were selected. The clinical characteristics of these patients were obtained from the hospital files. Offline echocardiography analysis included a revision of conventional echocardiography and calculation of myocardial work index variables at baseline and each dose of dobutamine infusion. Speckle tracking imaging analysis was done according to the original recommendations from apical 3-chamber, 4-chamber, and 2-chamber views6. The myocardial work index variables included: Global work index (GWI), Global constructive work (GCW), Global wasted work (GWW), and Global work efficacy (GWE) and were calculated according to the recent recommendations7.
All the patients underwent a standard protocol of dobutamine stress echocardiography with the incremental rise of dobutamine doses every 3 min, from 10 up to 40 mcg/kg/min. Atropine was delivered at the 20 or 30 mg/kg/min dose of dobutamine as recommended8, particularly if the heart rate was not increased as expected. ECG and blood pressure measurements were registered every 3 min. The target heart rate was determined as 85% of maximal predicted heart rate, 85% × (220 − age).
Statistical methods. Continuous data were expressed as means ± standard deviations. The normal distribution for all differences was tested using the Kolmogorov–Smirnov test. A two-tailed, dependent T-test was used. Categorical data were expressed in numbers and percentages. Univariate analysis was performed using Chi-Square/Fisher’s exact test (where appropriate) or to identify significant variables (p < 0.05).
Ethical approval
The study was approved by the Ethics (Helsinki) Committee at Shamir (Assaf Harofeh) Medical Center for the conduct of clinical Studies (No.: 0034-19-ASF). All methods were carried out following relevant guidelines and regulations.
Informed consent was not required as data collection was retrospective, anonymous, and speckle tracking imaging analysis didn’t influence clinical diagnosis. The Ethics (Helsinki) Committee at Shamir (Assaf Harofeh) Medical Center for the conduct of clinical Studies has approved the nonrequirement of informed consent.
Results
During 01.2019–06.2019, dobutamine stress echocardiography examinations were performed in 286 patients. 102 patients were excluded due to a prior history of coronary artery disease or inducible ischemia at dobutamine stress echocardiography. 65 patients were excluded due to reduced echocardiography image quality, which wasn’t sufficient for adequate speckle tracking. The remaining 119 patients with normal dobutamine stress echocardiography were included in the current study. The mean age was 66, there were 38 males (32%). The main indications for the study were chest pain (53%) and shortness of breath (47%), while the most of patients had risk factors for coronary artery disease (Table 1).
The mean ejection fraction (EF) was 59.8%. 53 patients, 45%, received atropine at dobutamine dose 20 or 30 mcg/kg/min, mean atropine dose was 0.7 ± 0.3 mg. All the patients reached target heart rate: 13—at dobutamine doses of 40 mcg/kg/min, 79 at 30 mcg/kg/min, 27 patients reached target heart rate at dobutamine dose 20 mcg/kg/min. Peak heart rate was 89 ± 4% of maximal predicted heart rate. Myocardial work index parameters during each stage of dobutamine stress echocardiography and hemodynamic parameters are represented (Table 2, Fig. 1).
Systolic blood pressure reached a peak at dobutamine doses of 20 mcg/kg/min. Diastolic blood pressure decreased slightly from 76.3 ± 12.2 to 65.6 ± 16.6 mmHg, p = 0.007. Heart rate increased from 72 to 135 bpm, p < 0.00001. Global strain increased from − 19.6 to − 23.7%, p < 0.00001. Global work index (GWI) decreased from 2393.3 ± 503.4 to 1864.7 ± 424.4 mmHg%, p < 0.0004. Global constructive work (GCW) decreased from 2681.7 ± 549.6 to 2152.6 ± 521.7 mmHg%, p = 0.001. Global wasted work (GWW) increased from 78.8 ± 56.5 to 128.3 ± 45.2 mmHg%, p < 0.003. Global work efficacy (GWE) decreased from 96.1 ± 3.1 to 91.9 ± 4.5%, p < 0.00001. Changes in the strain pressure loops during dobutamine stress echocardiography show (Fig. 2) that a small increase in strain during the cardiac cycle results in a steeper elevation of left ventricular pressure during the increment of dobutamine doses.
Pressure-strain loops during normal dobutamine stress echocardiography. LVP left ventricular pressure. MVC mitral valve closure, MVO mitral valve opening, AVC Aortic valve closure, AVO aortic valve opening. A small rise of strain results in a steeper increment of LV pressure during dobutamine stress echocardiography.
The data were analyzed by ML. Intraobserver variability [ML and VT], was performed on 10 patients and ranged up to 5%. Interobserver variability [ML] was done on 10 patients and ranged up to 5%.
Discussion
Dobutamine stress echocardiography is considered a good pharmacological alternative to stress echocardiography, within a generally acceptable safety profile9. Despite it, 7.6% of studies are stopped prematurely because of side effects10. Accelerated protocols of short-term high dose dobutamine infusion were suggested11 in the past. Modern protocols with atropine delivery at 20 and 30 mcg/kg/min were developed more recently to shorten the study and to improve its tolerability8. The various effects of dobutamine during dobutamine stress echocardiography are dose-dependent. Dobutamine has an affinity for cardiac α- and β-receptors. β1-receptors stimulation results in an increase in myocardial contractility, atrioventricular conduction, and heart rate. Stimulation of α-adrenergic receptors results in systemic vasoconstriction, increased myocardial contractility, and raises blood pressure. Stimulation of vascular β2-receptors induces coronary and peripheral arteriolar vasodilatation. The inotropic effect of dobutamine predominates in low doses, and the chronotropic effect develops in high doses12. Low dose dobutamine of 2.5–10 mcg/kg/min, is used for the assessment of viability8. Ischemic protocols of dobutamine stress echocardiography begin with the doses of 10 mcg/kg/min. The majority of patients have experienced a rise in systolic blood pressure, especially patients with preexisting hypertension that are more susceptible to the hypertensive effect of dobutamine13. 82% of our patients were hypertensive and dobutamine infusion resulted in a rise in blood pressure (Fig. 1), which is one of the major determinants of myocardial work index parameters.
Mechanics of cardiac contraction was evaluated recently with novel speckle tracking derived parameter, myocardial work index5,14,15,16,17. Evaluation of cardiac deformation parameters at stress echocardiography imaging up to recently was limited due to suboptimal speckle tracking imaging quality and to the inability to track endocardial border at high heart rates. Visual and quantitative analysis of left ventricular function, calculation of strain, and myocardial work index during high heart rates more than 120/min is problematic on the echocardiography monitors with fixed [non-adaptive] refresh rate, as some frames are distorted or explained twice or dropped. Recently introduced monitors with a high adaptive refresh rate allow an adequate solution to this problem18,19. As well, a better quality of modern echocardiography systems makes echocardiography images more suitable for speckle tracking imaging analysis.
Few studies evaluated strain during exercise stress echocardiography20 and dobutamine stress echocardiography5,17,18,19,20,21,22,23. A novel myocardial work index was investigated in patients during exercise stress echocardiography24,25,26, and in athletes after a half marathon27. During normal exercise stress echocardiography, deterioration was found only in global wasted work25 and global work efficacy25,27; the global work index improved25,27 and global constructive work improved25. In one study26, myocardial work index parameters were compared in normal versus ischemic response. In normal subjects, global longitudinal strain, global work index, global constructive work improved, global wasted work increased, global work efficacy was preserved [96% at rest, 95% at exercise]. In our study, despite improvement in global strain, all the parameters of myocardial work deteriorated during dobutamine stress echocardiography: global work index, global constructive work, global work efficacy, and global wasted work (Table 3). Therefore, the cardiac influence of dobutamine on myocardial work index variables is different from the effect of exercise. Dobutamine stress echo and exercise stress echo, both stress tests, affect conventional echocardiography parameters differently.
In addition to increases in heart rate, systolic blood pressure, and global strain, other indicators of myocardial function are impaired during dobutamine stress echocardiography. End diastolic volume index decreases slightly with exercise and decreases significantly with dobutamine, end-systolic volume index decreases with exercise and decreases significantly with dobutamine, stroke volume decreases significantly during dobutamine infusion and increases with exercise28. Myocardial work index parameters during dobutamine stress echocardiography also behave differently than exercise stress echocardiography (Table 3).
Calculation of target heart rate during exercise stress test based on the real data about oxygen consumption response to exercise, that is linear. A stage of the plateau is reached at near maximal exercise when a heart rate is of about 220 − age, that is the maximal predicted heart rate29, therefore target heart rate during the exercise stress test is set as 85–90% × (220 − age) according to the current guidelines8. Oxygen consumption during dobutamine stress echocardiography is not known, but extrapolating the data from exercise echocardiography and for safety considerations, the target heart rate is empirically set as 85% of maximal predicted heart rate8.
Our results indicate that the dobutamine stress test can overload the heart and age-related heart rate may not be the optimal criterion for interrupting the dobutamine infusion that probably, can be terminated earlier. There is a question if the sensitivity of such a study will not be impaired and further evaluation is needed.
Limitations
-
1.
Only normal examinations were recruited into the study, therefore the researchers were not blinded to the results.
-
2.
In our study we compared our data of dobutamine stress echocardiography with the literature data regarding exercise stress echocardiography that was done on other patients’ populations.
-
3.
Although all our patients achieved a target heart rate, we can’t exclude the possibility of false-negative results.
Conclusions
As we found in our study, during normal dobutamine stress echocardiography, although global myocardial strain increases, all the specific parameters of myocardial work index deteriorate. We can suppose, that the calculated target heart rate may not be the optimal parameter to define termination of dobutamine infusion. Myocardial work index and global strain can be used too. Further investigations of myocardial work index variables in patients with ischemia are needed.
References
Marwick, T. H. Stress echocardiography with nonexercise techniques: Principles, protocols, interpretation, and clinical applications. In The Clinical Practice of Clinical Echocardiography (ed. Otto, C.) (Saunders Elsevier, 2007).
Ng, A. C. et al. Incremental value of 2-dimensional speckle tracking strain imaging to wall motion analysis for detection of coronary artery disease in patients undergoing dobutamine stress echocardiography. Am. Heart J. 158, 836–844 (2009).
Aggeli, C. et al. Two-dimensional speckle tracking for the assessment of coronary artery disease during dobutamine stress echo: Clinical tool or merely research method. Cardiovasc. Ultrasound 13, 43 (2015).
Ilardi, F. et al. Accuracy of global and regional longitudinal strain at peak of dobutamine stress echocardiography to detect significant coronary artery disease. Int. J. Cardiovasc. Imaging 37(4), 1321–1331. https://doi.org/10.1007/s10554-020-02121-y (2021).
Russell, K. et al. A novel clinical method for quantification of regional left ventricular pressure-strain loop area: A non-invasive index of myocardial work. Eur. Heart J. 33, 724–733 (2012).
Leitman, M. et al. Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J. Am. Soc. Echocardiogr. 17(10), 1021–1029. https://doi.org/10.1016/j.echo.2004.06.019 (2004).
Ilardi, F. et al. Myocardial work by echocardiography: Principles and applications in clinical practice. J. Clin. Med. 10(19), 4521. https://doi.org/10.3390/jcm10194521 (2021).
Pellikka, P. A. et al. Guidelines for performance, interpretation, and application of stress echocardiography in ischemic heart disease: From the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 33(1), 1–41. https://doi.org/10.1016/j.echo.2019.07.001 (2020).
Kane, G. C. et al. Safety of stress echocardiography supervised by registered nurses: Results of a 2-year audit of 15,404 patients. J. Am. Soc. Echocardiogr. 21(4), 337–341. https://doi.org/10.1016/j.echo.2007.08.028 (2008).
Secknus, M. A. & Marwick, T. H. Evolution of dobutamine echocardiography protocols and indications: Safety and side effects in 3,011 studies over 5 years. J. Am. Coll. Cardiol. 29(6), 1234–1240. https://doi.org/10.1016/s0735-1097(97)00039-9 (1997).
Burger, A. J., Notarianni, M. P. & Aronson, D. Safety and efficacy of an accelerated dobutamine stress echocardiography protocol in the evaluation of coronary artery disease. Am. J. Cardiol. 86(8), 825–829. https://doi.org/10.1016/s0002-9149(00)01100-0 (2000).
Ruffolo, R. R. Jr., Spradlin, T. A., Pollock, G. D., Waddell, J. E. & Murphy, P. J. Alpha and beta adrenergic effects of the stereoisomers of dobutamine. J. Pharmacol. Exp. Ther. 219(2), 447–452 (1981).
Ashkar, H., Adnan, G. & Makaryus, A. N. Dobutamine (StatPearls Publishing, 2021).
Boe, E. et al. Non-invasive myocardial work index identifies acute coronary occlusion in patients with non-ST-segment elevation-acute coronary syndrome. Eur. Heart J. Cardiovasc. Imaging 16(11), 1247–1255. https://doi.org/10.1093/ehjci/jev078 (2015).
Galli, E. et al. Value of myocardial work estimation in the prediction of response to cardiac resynchronization therapy. J. Am. Soc. Echocardiogr. 31(2), 220–230 (2018).
Chan, J. et al. A new approach to assess myocardial work by non-invasive left ventricular pressure-strain relations in hypertension and dilated cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging 20(1), 31–39. https://doi.org/10.1093/ehjci/jey131 (2019).
Manganaro, R. et al. Echocardiographic reference ranges for normal non-invasive myocardial work indices: Results from the EACVI NORRE study. Eur. Heart J. Cardiovasc. Imaging 20(5), 582–590. https://doi.org/10.1093/ehjci/jey188 (2019).
Tyomkin, V. et al. Is it time to revise the guidelines and recommendations for digital echocardiography? J. Am. Soc. Echocardiogr. 31(5), 634–636. https://doi.org/10.1016/j.echo.2018.01.021 (2018).
Leitman, M. et al. Standards on digital echocardiography: An Israel Heart Society Position Paper Presented by the Israel Working Group on Echocardiography. Isr. Med. Assoc. J. 21(8), 524–527 (2019).
Leitman, M. et al. Speckle tracking imaging in normal stress echocardiography. J. Ultrasound Med. 36(4), 717–724. https://doi.org/10.7863/ultra.16.04010 (2017).
Govind, S. C. et al. Quantification of low-dose dobutamine stress using speckle tracking echocardiography in coronary artery disease. Eur. J. Echocardiogr. 10(5), 607–612. https://doi.org/10.1093/ejechocard/jep011 (2009).
Gopal, A. S. et al. Quantification of low-dose dobutamine stress using speckle tracking echocardiography in coronary artery disease. Eur. J. Echocardiogr. 10(5), 607–612. https://doi.org/10.1093/ejechocard/jep011 (2009).
Uusitalo, V. et al. Two-dimensional speckle-tracking during dobutamine stress echocardiography in the detection of myocardial ischemia in patients with suspected coronary artery disease. J. Am. Soc. Echocardiogr. 29(5), 470–479. https://doi.org/10.1016/j.echo.2015.12.013 (2016).
Clemmensen, T. S. et al. Left ventricular pressure-strain-derived myocardial work at rest and during exercise in patients with cardiac amyloidosis. J. Am. Soc. Echocardiogr. 33(5), 573–582. https://doi.org/10.1016/j.echo.2019.11.018 (2020).
Halabi, A., Wright, L. & Marwick, T. H. Measurement of global myocardial work with exercise testing. J. Am. Soc. Echocardiogr. 33(5), 631–632. https://doi.org/10.1016/j.echo.2020.01.021 (2020).
Borrie, A., Goggin, C., Ershad, S., Robinson, W. & Sasse, A. Noninvasive myocardial work index: Characterizing the normal and ischemic response to exercise. J. Am. Soc. Echocardiogr. 33(10), 1191–1200. https://doi.org/10.1016/j.echo.2020.05.003 (2020).
Sengupta, S., Jain, R., Burkule, N., Olet, S. & Khandheria, B. K. Myocardial work index: A novel method for assessment of myocardial function in south Asian recreational athletes. J. Patient Cent. Res. Rev. 7(2), 147–156. https://doi.org/10.17294/2330-0698.1730 (2020).
Mehrotra, P., Labib, S. B. & Schick, E. C. Differential effects of dobutamine versus treadmill exercise on left ventricular volume and wall stress. J. Am. Soc. Echocardiogr. 25(8), 911–918. https://doi.org/10.1016/j.echo.2012.05.002 (2012).
Albouaini, K., Egred, M., Alahmar, A. & Wright, D. J. Cardiopulmonary exercise testing and its application. Postgrad. Med. J. 83(985), 675–682. https://doi.org/10.1136/hrt.2007.121558 (2007).
Author information
Authors and Affiliations
Contributions
M.L.—writing of the manuscript; Y.B.—data collection; O.B.—figure preparation, data acquisition; V.T.—data analysis, intellectual input; S.F.—a critical review, intellectual input; All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leitman, M., Balboul, Y., Burgsdorf, O. et al. Myocardial work index during normal dobutamine stress echocardiography. Sci Rep 12, 6813 (2022). https://doi.org/10.1038/s41598-022-10903-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10903-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.