Abstract
Childhood pneumonia is common in developing countries, with significant morbidity and mortality. Taking the significance of the problem and variability of risk factors into account, a study was needed to identify the potential determinants of pneumonia in under-five children. A facility-based unmatched case–control study was conducted among 435 children (145 cases and 290 controls) aged 2–59 months at public health facilities in Worabe town from December 28, 2016, to January 30, 2017. Data were collected using interviewer-administered questionnaire and analysed using SPSS version 22. Bivariable and multivariable binary logistic regression were used to determine association between dependant and independent variables. Among the factors assessed, stunting [AOR = 3.6,95% CI: 1.9–6.9], carrying the child on the back during cooking [AOR = 2.0,95% CI: 1.2–3.2], absence of chimney in the cooking room [AOR = 2.2, 95% CI: 1.3–3.7], having a history of asthma [AOR = 5.0,95% CI: 2–12], and a previous acute upper respiratory tract infection [AOR = 3.7,95% CI:2.3–6.1] were significantly associated with pneumonia.
Similar content being viewed by others
Introduction
Pneumonia is a respiratory tract infection that affects children. Streptococcus pneumoniae, Haemophilus influenzae type b (Hib), and respiratory syncytial virus are among the common pathogens involved1. S. pneumoniae is the most common cause of bacterial pneumonia during childhood in the developing countries. Microbes that are commonly found in upper respiratory tract can cause lower respiratory tract infection. They may also spread via air-borne droplets at the time of cough or sneeze or may spread through blood, especially during and shortly after birth2. Pneumonia is the major killer of under-five children than any other disease known to affect children. Childhood pneumonia causes substantial mortality and morbidity among under-five children, with developing nations carrying the highest pneumonia burden3,4.
Every year, nearly 1 million children die of pneumonia worldwide and approximately about 15% of all deaths occur in children under age of five. This means a loss of over 2500 children’s lives every day or 100 children every hour. It is the most prevalent in sub-Saharan Africa and South Asia, Nigeria, Pakistan, the Democratic Republic of Congo, and Ethiopia, accounting for 50% of total deaths5,6,7. In Ethiopia, pneumonia is the leading cause of death, accounting for 18% of all under-five mortality burdens8. As a result, Ethiopia ranks fifth (62 deaths in 1000) among 15 countries in the world and has the highest death rate from clinical pneumonia in under five children9. It also causes millions of morbidity and adds costs to the health services program; as health services are passed on to cure high pneumonia morbidity cases, with an estimated 3,370,000 children encountering pneumonia annually10,11.
Ethiopia follows the same strategy and has adopted the World Health Organization (WHO) Integrated Management of Childhood Illness (IMNCI) guidelines since 2001. Moreover, with the objective of increasing access to life-saving interventions, Ethiopia made a policy breakthrough of introducing community-based treatment of pneumonia through health extension workers in 201012. Since then, 38,000 health extension workers from nearly 15,000 health posts have been equipped with the skills and supplies to treat pneumonia at the community level using the integrated community case management (ICCM) approach13.
Previous studies indicated that some of most determinants for pneumonia include the educational status of parents, age of the mother, family child caring practice, family income, age and sex of the child, parental smoking or indoor air pollution from biomass fuel smoke, absence window in the kitchen, overcrowding, parental asthma, household history of pneumonia, malnutrition, lack exclusively breastfeeding, lack of zinc supplementation, comorbidity condition such as diarrhoea, measles, acute upper respiratory infection (AURTI), and previous history of asthma1,10,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37.
Contributing factors of pneumonia need to be studied to better inform health care providers and policy-makers to consider pneumonia prevention strategies. Although there are studies conducted in Ethiopia, the risk factors for pneumonia differ in different societies and study populations37. Taking the high burden of pneumonia and variability of risk factors into account, this study is envisaged to identify the potential determinants of pneumonia in under-five children. Above all, there was no previous study in the study area that could show the determinants of pneumonia.
Methods
Study setting and study design
An unmatched case–control study was conducted from December 28, 2016, to January 30, 2017, in public health facilities located in Worabe town, Silte zone, Southern Nation Nationalities, and People’s Region. Worabe town is the capital town of Silte zone. The town has a total population of 29,600, of which 4618 are under-five children. There are two public health facilities in Worabe town and 6 private clinics38.
Study population
Children who were 2–59 months old, and those who visited the selected health facilities during the study period.
Cases were children aged 2–59 months who visited pediatric units, registered and diagnosed with pneumonia as defined by the Federal Democratic Republic of Ethiopian Ministry of Health Integrated Management of Childhood Illness (IMNCI) guideline that is adapted from WHO39.
The control group was defined as children aged 2–59 months without pneumonia and attended the public health facilities in Worabe town.
Sample size determination and sampling technique
A sample size of 435(145 cases and 290 controls) was determined using Epi-Info version 3.5.4 statistical software assumingtwo side confidence level (Cl) of 95%, power = 80%, ratio control to case 2:1, and taking a history of AURTI as a predictor of pneumonia with 22.4% prevalence among control group; 1.80 Odds ratio from a case–control study21 and an estimated non-response rate of 10%. All public health facilities in the town were purposively included based on patient load and the presence of accessible trained staff on IMNCI. The sample size was distributed to each health facility based on the average daily caseload. According to the zonal health bureau Health Management Information System report, the average daily pneumonia patients among under-five children at Worabe comprehensive specialized hospital (WCSH) was seven and it was two at Worabe Health Centre40. Based on this, the sample size allocated for the Worabe health centre was one case and two controls on a daily basis with a total of 21 cases and 42 controls. The sample size allocated for WCSH was six cases and twelve controls on a daily basis with a total of 124 cases and 248 controls.
Selection of cases
All cases (diagnosed and recorded as pneumonia/severe pneumonia) were considered in the study until the required sample size was reached/fulfilled.
Selection of controls
As the control-to-case ratio was 2:1, two children who did not have pneumonia and visited selected health facilities for different services at the time of data collection were randomly selected by systematic random sampling after the cases were identified.
Eligibility criteria
The study included children who were between 2 and 59 months of age, those who were residents of Worabe town for a minimum of six months, and visited the pediatric unit of WCSH and Worabe Health Center during the study period.
Children with the following conditions were excluded from the study: cardiac disease, cough that lasted for > 15 days (suspected of pulmonary tuberculosis), cough because of the recent history of aspiration of a liquid or a foreign body, and caregiver who did not have any information about the child at the time of data collection.
Study variables
Dependent variables
Presence of pneumonia.
Independent variables
Socio-demographic factors: Parental factors such as educational and occupational status, parental cigarette smoking, age of the mother, family size, and family caring practice (parental/home maid, place of child during cooking, and family income).
Child factors: age and sex, immunization status, a pre-existing illness such as a history of diarrhoea, AURTI, and acute lower respiratory tract infection/pneumonia in the last 2 weeks and asthma.
Environmental factors: type of fuel used for cooking, crowding status, place of cooking, parental asthma, and household history of tuberculosis and pneumonia.
Nutritional condition of the child: undernutrition, breastfeeding status of the child for the first 6 months and duration of breastfeeding, age of complementary feeding started, and zinc supplementation.
Operational definitions
Pneumonia
A child aged 2–59 months with cough and/or difficulty in breathing for less than two weeks of duration plus fast breathing and/or chest in drawing15,16,17,18,19.
Fast breathing is defined as:
-
For children in the age interval of 2–11 months, 50 breaths per minute or more
-
For children in the age interval of 12 months to 5 years, 40 breaths per minute or more39,40,41.
History of acute upper respiratory tract infection(AURTI): a child who had a history of ear infection, common cold, tonsillitis, or pharyngitis in the last fifteen days prior to data collection42.
Underweight: Weight at the birth of less than 2500 g43,44.
Stunting: Chronic undernutrition condition in which a child is short for his or her age44.
Wasting: Unintended loss of weight which makes children too thin and weak45.
Data collection tools and procedures
A structured questionnaire was developed based on a review of previously published studies and adapted for the current study with certain modifications17,18,19,20,21,22,23,24,25,26,27,28. The questionnaires included information on the possible risk factors for pneumonia, including socio-demographic factors, environmental/home-based factors, nutritional factors, immunization status, pre-existing illness and child care practices. Data were collected by IMNCI-trained nurses working in under-five clinics who received two days of training regarding the research. After the study participants were identified as cases and controls, mothers/primary caretakers were interviewed based on the interviewer-administered pretested structured questionnaire.
Anthropometric measurements
The weight and height of the child were taken at the beginning of the interview by data collectors. A suspended scale of 25 kg capacity graduated at 0.1 kg was used for weighing infants and children. The reading was recorded to the nearest 0.1 kg. Length measurements in the lying position were taken for children less than two years of age, and height measurements were taken for children 2–5 years of age. The anthropometric data were analysed in terms of weight for age, length for age, and weight for length using WHO Anthrosoftware to prepare for SPSS. The WHO (2006) growth standard was used to report anthropometric measurements result by Z-score, and the global acute malnutrition standard was used to classify the child’s nutritional status as normal, stunted, wasted, or underweight.
Data quality management
The questionnaire was pretested on a 5% sample size at Kbit Primary Hospital to ensure the validity and reliability of the survey tools. After collecting the pre-test data, it was checked for potential problems related to the tool, such as any difficult question that was understandable or unclear to reply and corrective measures were taken.
Data processing and analysis
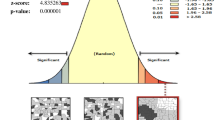
The collected data were checked for completeness, coded and entered into Epi Info version 7 and exported to the statistical package for social sciences (SPSS) version 22 for analysis. The entered data were cleaned and checked for consistency and extent of outliers. Different statistical assumptions and appropriate corrections were made prior to analysis. Descriptive analyses were carried out for each of the independent variables. Bivariable and multivariable binary logistic regression analysis was used to test the association between the independent and dependent variables. Bivariable analysis was performed for each of the independent variables with the outcome variable. Variables that had a p-value < 0.2 on bivariate analysis were taken as candidates for multivariable binary logistic regression model analysis to identify predictors of the outcome variables. Variables with a p-value less than 0.05 on multivariable logistic regression analysis were considered statically significant factors for the outcome variables. The strength of the association between the dependent variable and independent variables was expressed using adjusted odds ratio (AOR) with 95% confidence intervals.
Ethical approval and consent to participant
The study was ethically approved by the Institutional Review Board of Saint Paul’s Millennium Medical College Department of Public Health. An official permission letter was obtained from the study site. The objectives, expected outcomes, benefits, and risks of the study were explained to mothers/guardians/caregivers of the study participants. Data were collected after written informed consent was obtained. The study was conducted in accordance with the Declaration of Helsinki.
Results
Socio-demographic characteristics
A total of 435 (145 cases and 290 controls) children aged 2–59 months participated in the study, making the response rate 100% for both groups. The highest proportion of cases (57.2%) and controls (62.4%) were in the age group of 2–11 months, with mean ages of 14.6(SD ± 12.8) and 12.6 months (SD ± 12.7) for cases and controls respectively. Approximately 52% of cases and 51% of controls were males (Table 1).
Nutritional, pre-existing illness and vaccination status of the children
The majority (79.3%) of cases and 85.5% of controls were exclusively breastfed for the 1st six months of life. Regarding the nutritional status of the children, 11.9% cases and 9% controls, 26.9% cases and 18.6% controls were underweight and stunted respectively. More than 90% of cases and 95% of controls received pentavalent and pneumococcal conjugate vaccines.
The study indicated that; variables such as Zinc supplementation (p = 0.01), stunting (p = 0.001), wasting (p = 0.06), exclusive breastfeeding for the first 6 months (p = 0.1), a child with the previous history of AURTI (p < 0.001), and diarrhoea (p = 0.06) in the past two weeks and history of asthma (p < 0.001) were associated with the occurrence of pneumonia in the bivariate logistic regression at p < 0.2 (Table 2).
Environmental factors associated with pneumonia
More than half of the cases (57.2%) and controls (54.8%) lived in households that used wood as a source of energy for cooking. The highest proportion of cases (63.4%) and controls (63.8%) had mothers cooking their food in the kitchen. Approximately 61% of cases and 44% of controls stayed near or on their mothers'/care takers back while she was cooking. The bivariate logistic regression analysis revealed that crowding (p = 0.04), type of energy source for cooking (p = 0.02), absence of chimneys in the cooking room (p < 0.01), and place of a child during cooking (p < 0.01) had significant associations with pneumonia among children (Table 3).
Factors associated with pneumonia among children aged 2–59 months
All variables analysed by bivariable binary logistic regression showed a p-value less than 0.2. Multivariable binary logistic regression analysis showed that stunting, previous history of asthma diagnosis in the child, place of the child during cooking, absence of chimney in the cooking room and history of AURTI in the last 2 weeks prior to data collection were determinants of pneumonia. The findings revealed that the odds of stunting were 3.6 times higher among children with pneumonia than controls (AOR = 3.6, 95% CI: 1.8, 7; p < 0.001). On the other hand,the odds of carrying the child on the back while cooking/beside the cooking mother were twice as high as those of compared to children outside of the cooking room among cases than controls (AOR = 2, 95% CI: 1.2, 3.3; p = 0.006).
Similarly, the odds of children living in households with no chimney in the cooking room were 2.2 times higher among cases than controls (AOR = 2, 95% CI: 1.3, 3.7; p = 0.003). The odds of having a previous history of asthma were fivefold higher among cases than controls (AOR = 5, 95% CI: 2, 12; p < 0.001). Likewise, the odds of having a history of AURIT in the last 2 weeks prior to data collection were 3.7 times higher among children with pneumonia than among children without pneumonia (AOR = 3.7, 95% CI: 2.3, 6.1; p < 0.001) (Table 4).
Discussion
In this study, pre-existing respiratory illnesses, such as a history of asthma in the child and a previous history of AURTI, undernutrition (stunting), absence of chimney in the cooking room, and carrying the child on the back during cooking, were found to be significant risk factors associated with the occurrence of pneumonia among children aged 2–59 months.
The odds of carrying the child on the back while cooking was 2 times greater than that of children who pass outside of the cooking room among cases than controls. This could be due to indoor pollution as a result of unsafe energy sources such as charcoal, wood, and biomass. This result is consistent with a cross-sectional study conducted in northwest Ethiopia found that a child who was carried on the back of mother during cooking was five times more likely to develop pneumonia than their counterparts17. Similar findings were obtained in different countries that reported indoor air pollution as a risk factor for pneumonia15,25,28,29,30. However, two studies conducted in Ethiopia did not report a significant association between the place of the child during cooking and the occurrence of pneumonia in children18,23. The variation of the results could be due to differences in study setting and methodology used.
Stunting was another factor identified to be significantly associated with pneumonia, indicating that the odds of stunting were 3.6 times higher among children with pneumonia than controls, which is in line with a study conducted in Northwest Ethiopia and Bangladesh17,19. The possible reason might be that stunting shows long-term malnutrition, which weakens the child’s immunity and makes the child vulnerable to pneumonia. From different prospects of different studies, malnutrition (undernutrition) weakens the respiratory muscles needed to clear secretions in the respiratory tract, which intern predisposes to pneumonia1,24,41.
In this study, there was the strongest association between pneumonia and a history of asthma, indicating that children who had a previous history of asthma had approximately fivefold increased odds of developing pneumonia compared to their counterparts. According to the WHO 2008 bulletin report, concomitant diseases such as asthma were likely to be the risk factors for the occurrence of childhood pneumonia15. Several findings from other areas also indicated the relationship between asthma and pneumonia episodes21,36. In a study conducted in the Philippines, 55.4% of children who developed consolidated pneumonia had asthma as an underlying illness27. In the current study, we are unable to conclude whether asthma or other asthmatic condition was a predisposing factor for pneumonia. Further study is needed to define a causal relationship between asthma and pneumonia.
A history of AURTI in a child in the last two weeks preceding the current pneumonia was identified to put a child 3.7 times at risk of pneumonia compared to their counterpart. This is in line with the study conducted in southwest Ethiopia, which indicates that the risk of pneumonia is more than 5 times for children who had previous AURTIs23, and a similar finding in the Netherlands showed a strong relationship between the occurrences of community- acquired pneumonia and an increasing number of previous AURTIs21. However, a study conducted in Ethiopia reported no significant association between occurrences of pneumonia and preceding infection of AURTI in children22. A possible explanation might be that AURTI increases susceptibility to infections that subsequently predisposes patients to pneumonia or that there might be descending infection from the upper to lower respiratory tract.
Limitations of the study
The diagnosis of pneumonia was based on the clinical WHO IMNCI classification guidelines, which introduced misclassification recall bias; the study did not consider privates health facilities and did not consider the complete population.
Conclusions
This study indicated stunting, a previous history of asthma and upper respiratory tract infection, the absence of chimney in the cooking room and carrying the child on the back during cooking are strongly associated with an increased risk of childhood pneumonia. Therefore, the zonal health bureau, in collaboration with the agricultural office needs to improve the nutritional status of children, and the town administrative health office, in collaboration with the health facilities may provide health education to the community about the health risk of child exposure to biomass fuel smoke and to have chimneys in the cooking room.
Data availability
All necessary raw data used for analysis in this study is available from corresponding author with reasonable request.
Abbreviations
- AURTI:
-
Acute upper respiratory tract infection
- ICCM:
-
Integrated community case management
- IMNCI:
-
Integrated management of neonatal and childhood illness
- WCSH:
-
Worabe comprehensive specialized hospital
- WHO:
-
World Health Organization
References
WOH and UNICEF. Pneumonia and diarrhea: tackling the deadliest diseases for the world' poorest children. New York, June 2012.
United nation children's fund: world pneumonia day, facts about childhood pneumonia. New York (2015).
Liu, L. et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379, 2151–61 (2012).
Wang, H. et al. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 957–79 (2014).
World pneumonia day: universal access for pneumonia prevention and care (2014).
WHO media centre: pneumonia fact sheet, Sep 2016.
UNICEF: EVERY BREATH COUNTS, Every 35 seconds, a child dies from pneumonia. Addis Ababa, Ethiopia—January 31, 2016.
World Health Organization and UNICEF. Fulfilling the health agenda for the women and children countdown to 2015: maternal, newborn and child survival. The 2014 report. Geneva, WHO (2014).
United Nations Children’s Fund. Pneumonia and diarrhea progress report: IVAC, Bangladesh (2013).
Christa, L. et al. Childhood pneumonia and diarrhoea global burden of childhood pneumonia and diarrhoea. Lancet 381, 1405–1416 (2013).
World Health Organization and UNICEF. Handbook: IMCI, integrated management of childhood illness. Geneva: WHO (2005).
Federal ministry of health (FMOH): national plans on integrated community case management of common childhood illness. Ethiopia (2010).
United nation children's fund, Ethiopia: central data base, October 2014.
Levine, O. & Dinleyici, E. C. Pneumonia: the forgotten killer of children. Annotated 4(10), 27–28 (2010).
Rudan, I., Boschi-Pinto, C., Biloglav, Z., Mulholland, K. & Campbell, H. Epidemiology and etiology of childhood pneumonia. Bull. World Health Org. 86(5), 408–416 (2008).
Rudan, I. et al. Epidemiology and aetiology of childhood pneumonia in 2010: estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogen in192 countries. J. Glob. Health 3(1), 1–14. https://doi.org/10.7189/jogh.03.010401 (2013).
Abeje, G., Wubshet, M. & Asres, G. Prevalence of pneumonia among under- five children in Este town and the surrounding rural Kebele, Northwest Ethiopia: a community based cross-sectional study. Sci. J. Public Health 2(3), 150–155 (2014).
Teshome, A. Prevalence of pneumonia and factors associated among children 2–59 months old in Wondo Genet district, Sidama zone, SNNPR, Ethiopia. Curr. Pediatr. Res. 21(1), 19–25 (2017).
Azad, K. Risk factors for acute respiratory infections (ARI) among children under five years in Bangladesh. J. Sci. Res. 1(1), 72–81 (2009).
Fatmi, Z. & White, F. A comparison of ‘cough and cold’ and pneumonia: risk factors for pneumonia in children under 5 years revisited. Int. J. Infect. Dis. 6(4), 295–301 (2002).
Teepe, J., Grigoryan, L. & Verheij, T. J. Determinants of community-acquired pneumonia in children and young adults in primary care. Eur. Respir. J. 35(5), 1113–1117 (2010).
Dadi, A. F., Kebede, Y. & Birhanu, Z. Determinants of pneumonia in children aged two months to five years in urban areas of Oromia Zone, Amhara Region, Ethiopia. Open Access Libr. J. 1–10, e1044. https://doi.org/10.4236/oalib.1101044 (2014).
Geleta, D., Tessema, F. & Ewnetu, H. Determinants of community acquired pneumonia among children in Kersa District, Southwest Ethiopia: facility based case control study. J. Pediatr. Neonatal Care 5(2), 00179. https://doi.org/10.15406/jpnc.2016.05.00179 (2014).
Pore, P. D., Ghattargi, C. H. & Rayate, M. V. Study for risk factors for acute respiratory infection (ARI) in under five in solapur. Natl. J. Community Med. 1(2), 64–67 (2010).
Taksande, A. M. & Yeole, M. Risk factors for acute respiratory infection (ARI) in under-fives in a rural hospital of Central India. J. Pediatr. Neonatal Individ. Med. 5(1), e050105 (2016).
Gedefaw, M., Berhe, R., Gedefaw, M. & Berhe, R. Determinates of childhood pneumonia and diarrhea with special emphasis to exclusive breastfeeding in north Achefer district, northwest Ethiopia: a case control study. Open J. Epidemiol. 5(2), 107–112 (2015).
Kosai, H. et al. Incidence and risk factors for childhood pneumonia-like episodes in Biliran Island, Philippines a community-based study. PLoSOne 10(5), e0125009. https://doi.org/10.1371/journal.pone.0125009 (2015).
Dherani, M. et al. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under- five years: a systematic review and meta-analysis. Bull. World Health Org. 86, 390–398 (2008).
Bautista, L., Correa, A., Baumgartner, J., Breysse, P. & Matanoski, G. Indoor charcoal smoke and acute respiratory infections in young children in the Dominican Republic. Am. J. Epidemiol. 169, 572–580 (2009).
Bruce, N. et al. Pneumonia case-finding in the RESPIRE Guatemala indoor air pollution trial: standardizing methods for resource-poor settings. Bull. World Health Org. 85, 535–544 (2007).
Roux, D. M., Myer, L., Nicol, M. P. & Zar, H. J. Incidence and severity of childhood pneumonia in the first year of life in a South African birth cohort: the Drakenstein Child Health Study. Lancet Glob. Health 3, e95-103 (2015).
Maliha, N., Zafar, F. & Arif, A. Effect of behavioral risk factors on development of pneumonia among children under-5 years of age: a case-control study. Malays. J. Paediatr. Child Health Online Early 1(07), 1–13 (2011).
Zheng, X. H. et al. Home risk factors for childhood pneumonia in Nanjing, China. Chin. Sci. Bull. 58, 4230–4236. https://doi.org/10.1007/s11434-013-5686-5 (2013).
Schmidt, W. P., Cairncross, S., Barreto, M. L., Clasen, T. & Genser, B. Recent diarrhoeal illness and risk of lower respiratory infections in children under the age of 5 years. Int. J. Epidemiol. 38, 766–72 (2009).
Rahman, S. S., Khatun, A., Azhar, B. S., Rahman, H. & Hossain, S. A study on the relationship between nutritional status and prevalence of pneumonia and diarrhoea among preschool children in Kushtia. Pediatr. Res. Int. J. 2014, i1-10 (2014).
Hoving, M. F. & Brand, P. L. Causes of recurrent pneumonia in children in a general hospital. J. Paediatr. Child Health 49, E208-212. https://doi.org/10.1111/jpc.12114 (2013) (PMID: 23438187).
Horta, B. L., & Victora, C. G. Short-term effects of breastfeeding: a systematic review on the benefits of breastfeeding on diarrhoea and pneumonia mortality (2013).
Worabe Town Administrative Health Unit: Annual plan performance report, 2008 EFY.
Integrated management of newborn and childhood illness (IMNCI): chart booklet for health workers. Ministry of Health (2015).
Silte Zone Health Department: Health Management Information System report from Hamle (July) to Sane (June) 2008 EFY.
Mathew, J. L. et al. Acute respiratory infection and pneumonia in India: a systematic review of literature for advocacy and action: UNICEF-PHFI series on newborn and child health, India. Indian Pediatr. 48, 191–218 (2011).
Time-to-recovery from severe pneumonia and its determinants among children under-five admitted to university of Gondar Comprehensive Specialized Hospital in Ethiopia: a retrospective follow-up study; 2015–2020. Pediatr. Health Med. Ther. 12, 189–196 (2021).
Sutan, R., Mohtar, M., Mahat, A. N. & Tamil, A. M. Determinant of low birth weight infants: a matched case control study. Open J. Prev. Med. 4, 91–99. https://doi.org/10.4236/ojpm.2014.43013 (2014).
Amaha, D. N. & Woldeamanue, T. B. Maternal factors associated with moderate and severe stunting in Ethiopian children:analysis of some environmental factorsbased on 2016 demographic health survey. Nutr. J. 20, 18. https://doi.org/10.1186/s12937-021-00677-6 (2021).
Ferreira, N. C. et al. Detection of chronic wasting disease in mule and white-tailed deer by RT-QuIC analysis of outer ear. Sci. Rep. 11, 7702. https://doi.org/10.1038/s41598-021-87295-8 (2021).
Acknowledgements
We would like to thank the Zone Health Bureau, Worabe Health Centre, Worabe Comprehensive Specialized Hospital, Saint Paul’s Hospital Millennium Medical College Department of Public Health for facilitating the study. We also acknowledge all study participants for their willingness to take part in the study.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
R.K.S. Designed the study, was involved in data collection, data analysis and interpretation, wrote the paper and prepared the manuscript for publication. Y.A.W. & M.M.A. Data analysis; and interpretation and prepared the initial draft of the manuscript for publication. S.M.A. Had oversight of all the stages of the research, critically reviewed the final draft of the paper and the prepared manuscript for publication. The final manuscript was read and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seramo, R.k., Awol, S.M., Wabe, Y.A. et al. Determinants of pneumonia among children attending public health facilities in Worabe town. Sci Rep 12, 6175 (2022). https://doi.org/10.1038/s41598-022-10194-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10194-z
This article is cited by
-
Determinants of pneumonia among under-five children in Oromia region, Ethiopia: unmatched case-control study
Archives of Public Health (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.