Abstract
There is a lack of information highlighting the possible association between the genomic subtypes of enteropathogenic Escherichia coli (EPEC) on environmental enteric dysfunction (EED) and on linear growth during childhood. Genomic subtypes of EPEC from stool samples collected from 1705 children enrolled in the MAL-ED birth cohort were detected by TaqMan Array Cards. We measured site-specific incidence rate by using Poisson regression models, identified the risk factors and estimated the association of genomic subtypes of EPEC with the composite EED score and linear growth at 24 months of age. In general, the highest incidence rate (39%) was found among children having aEPEC infection, which was the greatest in Tanzania (54%). Exclusive breastfeeding and having an improved sanitation facility were found to be protective factors against EPEC infection. In the multivariate models, in overall effect after adjusting for the potential covariates aEPEC showed strong positive associations with the EED scores and tEPEC showed a positive association with poor linear growth at 24 months of age. Our analyses may lay the cornerstone for a prospective epidemiologic investigation for a potential vaccine development aimed at reducing the burden of EPEC infections and combat childhood malnutrition.
Similar content being viewed by others
Introduction
Diarrhea is responsible for the death of approximately 900,000 children per year worldwide, with the majority of cases of mortality occurring in developing countries1. Host factors such as: immunocompromisation, enteropathy and dysbiosis of the gut microbiome, which are commonly attributing to childhood malnutrition may in turn predispose malnourished young children to greater severity of diarrheal and other enteric diseases and their long-term sequelae2,3. Diarrheal diseases in combination with malnutrition have also been reported to hinder the cognitive development of millions of young children worldwide, with persistent infections occurring in their most formative early childhood when critical brain synaptogenesis occurs4.
Findings from the Global Enteric Multicenter Study (GEMS) report enteropathogenic Escherichia coli (EPEC) to be the leading contributor of diarrheal mortality among children in low and middle income countries (LMICs) aged less than 12 months5. EPEC does not possess the technology for the production of heat-labile or heat-stable enterotoxin and is classified based on a lesion known as the attaching-and-effacing (A/E) phenotype to the EPEC adherence factor (EAF) plasmid due to the eae gene located on the chromosomal pathogenicity island called the locus of enterocyte effacement (LEE locus) and produces the intimin adhesin6. EPEC is equipped with the locus of enterocyte effacement (LEE) pathogenicity island, which comprises of 41 open reading frames (ORFs) and codes for a distinct type III secretion system that is involved in the pathogenesis of these organisms7.
On the basis of the presence of the EAF plasmid encoding bundle-forming pili (BFP), EPEC can be sub-grouped into typical EPEC (tEPEC) and atypical EPEC (aEPEC)8. Typical EPEC is usually linked to incidences of gastroenteritis, even severe diarrhea among infants, while atypical EPEC is associated with a wide array of clinical manifestations, ranging from asymptomatic colonization to prolonged diarrhea, based on different settings8,9,10. Findings from studies carried out across 13 developing countries showed that isolates of aEPEC accounted for 78% of all EPEC associated diarrheal cases among children aged less than 5 years11. Additionally, EPEC may lead to severe nutrient malabsorption, resulting in nutritional consequences and eventual persistence of diarrhea12.
Results from a cross-sectional case–control study conducted among Brazilian aged between 2 and 36 months reported a higher association of tEPEC infections with clinical severity of diarrhea and undernutrition compared to aEPEC infections13. Later on, a recent study conducted in Bangladesh reported higher detection rates of both tEPEC and aEPEC among severely malnourished infants with diarrhea aged less than 6 months, compared to their age-matched well-nourished counterparts, although the detection of tEPEC was greater than the detection of aEPEC in both the severely malnourished and well-nourished groups14. Moreover, a reanalysis of the data from the Global Enteric Multicenter Study reported that tEPEC was significantly associated with higher incidences of moderate-to-severe diarrhea (MSD) among children aged 6–11 months and suffering from acute malnutrition15.
However, a thorough understanding of the epidemiology of infection by the EPEC subtypes is yet to be established, owing to the lack of proper discrimination in many studies16. The main goal of our study was to estimate the site-specific incidence rates of the two genomic subtypes of EPEC (tEPEC and aEPEC) and their possible associations with the composite EED (environmental enteric dysfunction) scores and the consequent growth failure among children at 24 months of age.
Results
General characteristics of the study population and incidence rates of virulence-related genes associated with EPEC
A total of 34,622 monthly stool samples were collected from 1715 participants who completed the follow-up to 24 months. All the stool samples collected over this time from all the participants at the different study sites were assessed for the presence of virulence-related genes associated with EPEC using TaqMan Array Cards (TAC). The general characteristics of the study children are presented in Table 1.
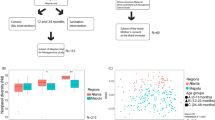
The incidence rates of the two genomic subtypes of EPEC (tEPEC and aEPEC) in the stool samples collected across all the 8 study sites over the 24 months study period have been shown in Fig. 1. The overall incidence rate of the aEPEC was the highest (39%). The incidence of virulence-related genes associated with aEPEC was highest in Tanzania (54%). It was also observed that the overall incidence of tEPEC virulence gene was lowest among all the sites (3%). The incidence of aEPEC infection was higher than the incidence of tEPEC infection, across all the study sites (Supplementary Table 1).
Factors associated with the two genomic subtypes of EPEC
Factors associated with infections by the two genomic subtypes of EPEC across all study sites were identified using Poisson regression (Table 2). The incidence rate for infection of EPEC in female children was comparable with male children. Additionally, exclusive breastfeeding status with infections by the aEPEC [IRR:0.99 (95%CI: 0.99–1.00); p < 0.001] and improved sanitation among children infected with tEPEC [IRR: 0.90 (95%CI: 0.81–0.99); p = 0.026] were associated and found to be statistically significant. The incidence rate of aEPEC was higher for the sites of Brazil, Nepal, South Africa, and Peru, while that of the aEPEC was the greatest in Peru. Consequently, the incidence rate of tEPEC infection was the lowest in Brazil and that of aEPEC was the lowest in Pakistan. The incidence rate of tEPEC infection was higher in India and Peru (Table 2).
Association between the different virulence genes of EPEC and child growth
Infections with tEPEC were associated with poor linear growth (difference in 24 months LAZ: length-for-age z score), with a stronger association being observed for overall all the study sites (Table 3). In Nepal, infection with tEPEC [− 2.44 difference in 24 months LAZ (95% CI: − 4.36, −0.52); p = 0.013] had a statistically significant negative association with LAZ. In India, aEPEC [− 0.96 difference in 24 months LAZ (95% CI: − 1.87, − 0.05); p = 0.040] was negatively associated with LAZ which was also statistically significant. For the other countries (except Bangladesh) infections with tEPEC were negatively associated with LAZ and for the other three countries (Tanzania, Brazil, South Africa) infections with aEPEC were negatively associated with LAZ but were not statistically significant.
Association between genomic subtypes of EPEC and enteric inflammation
After adjusting for the potential covariates like age, sex, WAMI index (water/sanitation, assets, maternal education, and income); enrollment length-for-age z score; maternal BMI; the number of children in the household, presence of poultry/cattle in the household, seasonality, serum zinc level, AGP (alpha-1-acid glycoprotein), presence of co-pathogens (Campylobacter, LT-ETEC, ST-ETEC, Shigella/EIEC, and Giardia), site for the overall estimate and age as the time variable in GEE (generalized estimating equations) model for the genomic subtypes of EPEC, aEPEC was also clearly and consistently associated with increased EED score with the overall [Coef. 0.15 (95% CI: 0.07, 0.23); p < 0.001] effect for all sites. The same findings were observed in India [Coef. 0.19 (95% CI: 0.01, 0.37); p = 0.043] and Nepal [Coef. 0.31 (95% CI: 0.11, 0.50); p = 0.002] individually for aEPEC infection (Table 4).
Discussion
To our knowledge, this is the first study investigating the associations between the two prominent genomic subtypes of EPEC (tEPEC and aEPEC) with enteric inflammation and linear growth in children from birth up until 2 years of age. Several EPEC virulence genes have been used in case–control and epidemiological studies in recent years, with eae and bfpA being among the most common for detection of the prominent subtypes of EPEC17.
We found that exclusive breastfeeding and having an improved sanitation facility had a very small protective effect against both tEPEC and aEPEC. Concurrent observation from a study conducted among Tanzanian children have described the same findings, most of the children younger than 6 months were exclusively breastfeed whose stool specimens were negative for EPEC18. Another study conducted in University Hospital, Sao Paulo, Brazil over 46 women who had given birth to normal term babies found that, the human colostrum IgA antibodies reacting to enteropathogenic E. coli antigens and their persistence in the gastrointestinal tract was shown by the strong reactivity to the 94-kDa band in the Western blot analysis. These data confirm the role of colostrum antibodies in protecting the neonate against infections caused by EPEC19. Hands, soil, and water could all be key sources of exposure to EPEC. The most important reservoirs of pathogens are the ones that children come in contact with most often. Overall, the sanitation intervention seems to have a limited effect on the presence of EPEC in hands, soil, and water20. Such assessments of different factors that may be associated with EPEC infections may in turn enhance in devising new treatment strategies against EPEC infections.
We documented high incidence rates of both tEPEC and aEPEC in Tanzania. The Global Enteric Multicenter Study (GEMS) determined that the diarrheal death of children can largely be attributed to a mere few infectious agents5. In particular, diarrhea caused by tEPEC is associated with a 2.6-fold higher hazard of death, the largest reported in the GEMS5. In our study, the lowest incidence rate of tEPEC has been found in Brazil. Other studies reported aEPEC to have a significant association with diarrhea in several countries, including Brazil21,22,23, where aEPEC was more prevalent than tEPEC. These observations indicate that aEPEC infections have significant clinical pertinence regarding the burden of EPEC infections and demand greater vigilance through epidemiologic and virulence studies.
In diarrheal animal models, positive culture or qPCR results for atypical EPEC (aEPEC) had significantly higher small intestinal and colonic lesion scores than a healthy animal. The increase in colonic lesion scores in animals with diarrhea and aEPEC infections was due to increased amounts of inflammatory infiltrate in the lamina propria24. In our study, the presence of aEPEC was more strongly associated with EED scores, implying a higher intestinal inflammation. The relevance of elevated intestinal inflammation associated with this particular genomic subtype of EPEC is not yet clear and no evidence indicates a particular genomic subgroup of EPEC to be associated with elevated intestinal inflammatory biomarkers and subsequently increased EED score. Henceforth, our study is the first attempt undertaken towards the generation of evidence-based knowledge of the contribution of the different genomic subgroups of EPEC with regards to enteric inflammation and poor child growth in LMIC settings.
Our study findings also illustrate that the presence of tEPEC and aEPEC was negatively associated with childhood linear growth in Nepal and India, respectively. However, in Norwegian children a significant association was observed with diarrhea lasting 14 days or more, a finding that may indicate a role for atypical EPEC in prolonged diarrhoeal episode25 and which might cause chronic malnutrition. When the different genomic subgroups of EPEC adhere to epithelial cells in vitro or in vivo they cause characteristic changes known as Attaching and Effacement (A/E) lesions. Decrease in number and height of microvilli, blunting of borders of enterocytes, loss of the glycocalyx, shortening of villi, and presence of a mucus pseudo membrane coating the mucosal surface were the abnormalities observed in the majority of children12. These ultrastructural derangements may be due to a mechanism where the different subgroups of EPEC trigger diarrhea as a response to contamination of food or water, which in turn if persistent may, in turn, result in chronic malnutrition in an early phase of life.
Although antibiotic therapy is not recommended for cases of mild acute diarrhea26, studies on the determination of the antibiotic resistance profile of aEPEC are necessary, due to cases of persistent diarrhea associated with aEPEC being reported25,26,27. Henceforth, under such clinical manifestations, the administration of antimicrobial therapy may be useful28.
Despite some potentially promising nature of our study findings, there are several possible limitations associated with our analysis. As an observational cohort study, the causality of the associations between infection with various genomic subgroups of EPEC and both intestinal inflammation and linear growth cannot be proven but can be hypothesized based on several factors, including the appropriate adjustment of the models for possible confounders, the strength and consistency of the associations, and the biological plausibility. We were unable to establish a temporal relationship between infections and the outcomes, which would require structured longitudinal models. Moreover, our analysis lacked data of the host gut microbiome and host diet, which have been found to be linked with infection by a wide range of enteropathogens.
The present study concludes that exclusive breastfeeding and improved sanitation facility are the possible protective factors for EPEC infections by different virulence genes and thereby leading to a compromised linear growth in childhood. The burden of both tEPEC and aEPEC was associated with increased enteric inflammation among children in the first 2 years of life.
Method
Study design and participants
MAL-ED (Etiology, Risk Factors, and Interactions of Enteric Infections and Malnutrition and the Consequences for Child Health) was a birth cohort study performed across 8 sites in South America, sub-Saharan Africa, and South Asia. The MAL-ED study design and methodology have been described elsewhere29. Briefly, 1715 children were enrolled from November 2009 to February 2012 from the community within 17 days of birth across eight different sites, namely: Bangladesh, India, Nepal, Pakistan, South Africa, Tanzania, Brazil, and Peru. In our current analysis, data from all 1715 participants were available from enrolment soon after birth up to 24 months of age.
Ethical consideration
The study was approved by the ethical committees at each of the participating institutes across each of the 8 study sites29. The study was approved by the Research Review Committee and the Ethical Review Committee, icddr,b (BGD); Committee for Ethics in Research, Universidade Federal do Ceara; National Ethical Research Committee, Health Ministry, Council of National Health (BRF); Institutional Review Board, Christian Medical College, Vellore; Health Ministry Screening Committee, Indian Council of Medical Research (INV); Institutional Review Board, Institute of Medicine, Tribhuvan University; Ethical Review Board, Nepal Health Research Council; Institutional Review Board, Walter Reed Army Institute of Research (NEB); Institutional Review Board, Johns Hopkins University; PRISMA Ethics Committee; Health Ministry, Loreto (PEL); Ethical Review Committee, Aga Khan University (PKN); Health, Safety and Research Ethics Committee, University of Venda; Department of Health and Social Development, Limpopo Provincial Government (SAV); Medical Research Coordinating Committee, National Institute for Medical Research; Chief Medical Officer, Ministry of Health and Social Welfare (TZH)30. Written informed consent was obtained from the parents or legal guardians of every child.
All 8 of the MAL-ED sites contributed their expertise, explained the challenges unique to their site, debated vigorously, compromised, and created 1 set of consensus standard operating procedures (SOPs), which was then implemented at the sites prior to study recruitment. All methods and procedures that have been used in this study were performed in accordance with the relevant guidelines and regulations31,32,33,34.
Data collection
Anthropometric measurements were taken at monthly intervals up to the age of 24 months using standard scales (Seca gmbh & co. kg., Hamburg, Germany). Length-for-age z score (LAZ), weight-for-age z score (WAZ), and weight-for-length z score (WLZ) were calculated through the use of the 2006 WHO standards for children35. Details of illness and child feeding practices were collected during household visits, conducted twice weekly32. Additionally, household demographics, presence of siblings, maternal characteristics, and other data on the child’s birth and anthropometry were obtained at enrollment29. Beginning at 6 months of age, socioeconomic data were collected every 6 months. The WAMI score (Water, sanitation, hygiene, Asset, Maternal education, and Income index, ranging from 0 to 1) is a socioeconomic status index. It includes access to improved water and sanitation, eight selected assets, maternal education, and household income as a representative of the socioeconomic status of the households36. A better socioeconomic status is indicated by a higher WAMI score37. Improved water and sanitation were defined following World Health Organization guidelines38. Treatment of drinking water was defined as filtering, boiling, or adding bleach39.
Collection of stool and blood samples
Non-diarrheal stool samples were collected monthly (at least 3 days before or after a diarrheal episode) from birth to age 2 years and peripheral blood was collected at 7, 15, and 24 months of age40. Raw stool aliquots and blood samples were processed at all sites using harmonized protocols and stored at − 80 °C freezers before subsequent laboratory analyzes31.
In this study, plasma zinc was assessed as the measure of zinc status at the age of 7, 15, and 24 months. Plasma zinc concentration is a proxy marker and recommended for assessment of population zinc status, especially for children in low-income countries41. Plasma alpha-1-acid glycoprotein (AGP) level was considered as a biomarker for systemic inflammation and was also assessed at 7, 15, and 24 months42.
Assessment of enteropathogens by TaqMan Array Cards (TAC)
Total nucleic acid (both DNA and RNA) was extracted from the fecal samples using the QIAamp Fast DNA Stool Mini kit (Qiagen), following the manufacturer’s guidelines. Two external controls, namely: MS2 bacteriophage and Phocine herpesvirus (PhHV) were added to the samples for the confirmation of nucleic acid extraction and amplification efficiency43.
For the detection of enteropathogens, a quantitative polymerase chain reaction (qPCR) with the use of a customized TaqMan Array Card (TAC) involving compartmentalized probe-based real-time PCR assays was used for the detection of a possible 29 pathogens from each of the samples44. Ct (quantification cycle) value of 35 was set as a threshold for analysis, whereby a Ct > 35 was considered as negative, as mentioned elsewhere43. In our current study, we investigated the occurrence of putative virulence-related genes (VRG) of EPEC, namely: bfpA for tEPEC, and eae for aEPEC.
Assessment of biomarkers of intestinal inflammation
Intestinal inflammation was evaluated by measuring the levels of the biomarkers: alpha-1-anti-trypsin (Biovendor, Chandler, NC), neopterin (GenWay Biotech, San Diego, CA), and myeloperoxidase (Alpco, Salem, NH) in the stool samples collected from the study participants at the 3, 6, 9, 15, and 24 months of age time points by quantitative ELISA, using manufacturer’s guidelines45.
Statistical analysis
All statistical analyses were performed in STATA 15 (Stata Corporation, College Station, TX). Descriptive statistics such as proportion, mean and standard deviation (SD) for symmetric data, and median with inter‐quartile range (IQR) for asymmetric quantitative variables were used to summarize the data. Chi-square and proportion test were used to determine the association between two categorical variables and t-test was used to assess the mean difference between two groups for symmetric distribution. Incidence rates were calculated using Poisson regression where outcome variables were the number of infections of EPEC (different genomic strain) and offset variables were a log of a number of follow-up visits. The factors associated with virulence-related genes associated with EPEC in the monthly stool samples were calculated using Poisson regression models. In the final multiple Poisson regression model, the following variables were considered for inclusion using stepwise forward selection: child sex, birth weight, duration of exclusive breastfeeding in months, enrollment weight for age z-score, length for age z score, maternal age in years, maternal education, mother having less than 3 living children, maternal BMI, routine treatment of drinking water, improved sanitation, household ownership of cattle/poultry, and less than 2 people live in per room. We excluded children from the Pakistan site for growth analysis, owing to bias noted in a subset of this cohort within the study period. Myeloperoxidase (MPO), neopterin (NEO), and alpha-1-antitrypsin (AAT) values were log‐transformed before the analysis. At each time point, the composite EED score ranging from 0 to 10 was calculated from the three fecal markers, as described in the previous literature by MAL-ED researchers46,47. Categories were assigned values as 0 (low), 1 (medium), or 2 (high). The formula for the composite EED score is as follows48:
Associations between virulence-related genes linked with EPEC and composite EED score were estimated using generalized estimating equations (GEE) to fit regression models after adjusting for sex, age, water/sanitation, assets, maternal BMI, and (WAMI) index; enrollment length-for-age and weight-for-age z score, maternal height; poultry/cattle in house, serum zinc level, inflammatory biomarker AGP (alpha-1-acid glycoprotein), presence of co-pathogens (Campylobacter, LT-ETEC, ST-ETEC, Shigella/EIEC, and Giardia), seasonality, and site for overall estimate and age in the month as time variable49. To assess and compare the associations of virulence-related genes linked with EPEC infection burden on growth at 24 months of age, we used multivariable linear regression after adjusting for the site and the necessary covariates. To detect multicollinearity, the variance inflation factor (VIF) was calculated, and no variable producing a VIF value > 5 was found in the final model. We calculated the strength of association by estimating the coefficient and its 95% CI (confidence interval) during the multivariable analysis. A p value of < 0.05 was considered statistically significant.
Data availability
A publicly available MAL-ED dataset was analyzed in this study. This data can be obtained from here: ClinEpiDB [https://clinepidb.org/ce/app/record/dataset/DS_841a9f5259].
References
Liu, L. et al. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet 379(9832), 2151–2161 (2012).
Rytter, M. J. H., Kolte, L., Briend, A., Friis, H. & Christensen, V. B. The immune system in children with malnutrition—A systematic review. PLoS ONE 9(8), e105017 (2014).
Jones, K. D., Thitiri, J., Ngari, M. & Berkley, J. A. Childhood malnutrition: Toward an understanding of infections, inflammation, and antimicrobials. Food Nutr. Bull. 35(2_suppl1), S64–S70 (2014).
Dipasquale, V., Cucinotta, U. & Romano, C. Acute malnutrition in children: Pathophysiology, clinical effects and treatment. Nutrients. 12(8), 2413 (2020).
Kotloff, K. L. et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): A prospective, case–control study. Lancet 382(9888), 209–222 (2013).
Deborah Chen, H. & Frankel, G. Enteropathogenic Escherichia coli: Unravelling pathogenesis. FEMS Microbiol. Rev. 29(1), 83–98 (2005).
Elliott, S. J. et al. The complete sequence of the locus of enterocyte effacement (LEE) from enteropathogenic Escherichia coli E2348/69. Mol. Microbiol. 28(1), 1–4 (1998).
Donnenberg, M. S. et al. Bacterial factors associated with lethal outcome of enteropathogenic Escherichia coli infection: Genomic case–control studies. PLoS Negl. Trop. Dis. 9(5), e0003791 (2015).
Hernandes, R. T., Elias, W. P., Vieira, M. A. & Gomes, T. A. An overview of atypical enteropathogenic Escherichia coli. FEMS Microbiol. Lett. 297(2), 137–149 (2009).
Nataro, J. P. & Kaper, J. B. Diarrheagenic Escherichia coli. Clin. Microbiol. Rev. 11(1), 142–201 (1998).
Ochoa, T. J., Barletta, F., Contreras, C. & Mercado, E. New insights into the epidemiology of enteropathogenic Escherichia coli infection. Trans. R. Soc. Trop. Med. Hyg. 102(9), 852–856 (2008).
Fagundes-Neto, U. & Scaletsky, I. C. A. The gut at war: The consequences of enteropathogenic Escherichia coli infection as a factor of diarrhea and malnutrition. Sao Paulo Med. J. 118, 21–29 (2000).
Santos, A. K. S. et al. Virulence-related genes and coenteropathogens associated with clinical outcomes of enteropathogenic Escherichia coli infections in children from the Brazilian semiarid region: A case–control study of diarrhea. J. Clin. Microbiol. 57(4), e01777-e11718 (2019).
Palit, P. et al. Use of TaqMan Array Cards to investigate the etiological agents of diarrhea among young infants with severe acute malnutrition. Trop. Med. Int. Health 26 (12), 1659–1667 (2021).
Tickell, K. D. et al. The effect of acute malnutrition on enteric pathogens, moderate-to-severe diarrhoea, and associated mortality in the Global Enteric Multicenter Study cohort: A post-hoc analysis. Lancet Glob. Health 8(2), e215–e224 (2020).
Gomes, T. A. et al. Diarrheagenic Escherichia coli. Braz. J. Microbiol. 47, 3–30 (2016).
Abe, C. M. et al. Virulence features of atypical enteropathogenic Escherichia coli identified by the eae+ EAF-negative stx− genetic profile. Diagn. Microbiol. Infect. Dis. 64(4), 357–365 (2009).
Moyo, S. J., Maselle, S. Y., Matee, M. I., Langeland, N. & Mylvaganam, H. Identification of diarrheagenic Escherichia coli isolated from infants and children in Dar es Salaam, Tanzania. BMC Infect. Dis. 7(1), 92 (2007).
Carbonare, S. B., Silva, M. L. M., Palmeira, P. & Carneiro-Sampaio, M. M. S. Human colostrum IgA antibodies reacting to enteropathogenic Escherichia coli antigens and their persistence in the faeces of a breastfed infant. J. Diarrhoeal Dis. Res. 15(2), 53–58 (1997).
Fuhrmeister, E. R., Ercumen, A., Pickering, A. J. et al. Effect of Sanitation Improvements on Pathogens and Microbial Source Tracking Markers in the Rural Bangladeshi Household Environment. Environmental science & technology. 54(7), 4316–4326 (2020).
Afset, J. E., Bergh, K. & Bevanger, L. High prevalence of atypical enteropathogenic Escherichia coli (EPEC) in Norwegian children with diarrhoea. J. Med. Microbiol. 52(11), 1015–1019 (2003).
Bueris, V. et al. Detection of diarrheagenic Escherichia coli from children with and without diarrhea in Salvador, Bahia, Brazil. Mem. Inst. Oswaldo Cruz. 102, 839–844 (2007).
Scaletsky, I. C. A., Fabbricotti, S. H., Silva, S. O. C., Morais, M. B. & Fagundes-Neto, U. HEp-2–adherent Escherichia coli strains associated with acute infantile diarrhea, São Paulo, Brazil. Emerg. Infect. Dis. 8(8), 855 (2002).
Watson, V. E. et al. Association of atypical enteropathogenic Escherichia coli with diarrhea and related mortality in kittens. J. Clin. Microbiol. 55(9), 2719–2735 (2017).
Afset, J. E., Bevanger, L., Romundstad, P. & Bergh, K. Association of atypical enteropathogenic Escherichia coli (EPEC) with prolonged diarrhoea. J. Med. Microbiol. 53(11), 1137–1144 (2004).
Marcos, L. A. & DuPont, H. L. Advances in defining etiology and new therapeutic approaches in acute diarrhea. J. Infect. 55(5), 385–393 (2007).
Nguyen, R. N., Taylor, L. S., Tauschek, M. & Robins-Browne, R. M. Atypical enteropathogenic Escherichia coli infection and prolonged diarrhea in children. Emerg. Infect. Dis. 12(4), 597 (2006).
Ochoa, T. J., Salazar-Lindo, E. & Cleary, T. G. Management of children with infection-associated persistent diarrhea. Seminars in Pediatric Infectious Diseases. 15(4), 229–236 (2004).
The MAL-ED Network Investigators. The MAL-ED Study: A Multinational and Multidisciplinary Approach to Understand the Relationship Between Enteric Pathogens, Malnutrition, Gut Physiology, Physical Growth, Cognitive Development, and Immune Responses in Infants and Children Up to 2 Years of Age in Resource-Poor Environments. Clinical Infectious Diseases. 59(suppl_4): S193–S206 (2014).
Rogawski, E. T. et al. Epidemiology of enteroaggregative Escherichia coli infections and associated outcomes in the MAL-ED birth cohort. PLoS Negl. Trop. Dis. 11(7), e0005798 (2017).
Houpt, E. et al. Microbiologic methods utilized in the MAL-ED cohort study. Clin. Infect. Dis. 59(suppl_4), S225–S232 (2014).
Richard, S. A., Barrett, L. J., Guerrant, R. L., Checkley, W. & Miller, M. A. Disease surveillance methods used in the 8-site MAL-ED cohort study. Clin. Infect. Dis. 59(suppl_4), S220–S224 (2014).
Platts-Mills, J. A. et al. Methods of analysis of enteropathogen infection in the MAL-ED cohort study. Clin. Infect. Dis. 59(suppl_4), S233–S238 (2014).
Murray-Kolb, L. E. et al. The MAL-ED cohort study: Methods and lessons learned when assessing early child development and caregiving mediators in infants and young children in 8 low-and middle-income countries. Clin. Infect. Dis. 59(suppl_4), S261–S272 (2014).
de Onis, M. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 85(9), 660–667 (2007).
Das, R. et al. Evaluating association of vaccine response to low serum zinc and vitamin D levels in children of a birth cohort study in Dhaka. Vaccine 39(1), 59–67 (2021).
Das, S., Alam, M. A., Mahfuz, M., El Arifeen, S. & Ahmed, T. Relative contributions of the correlates of stunting in explaining the mean length-for-age z-score difference between 24-month-old stunted and non-stunted children living in a slum of Dhaka, Bangladesh: Results from a decomposition analysis. BMJ Open 9(7), e025439 (2019).
Unicef, W. H. O. Progress on Drinking Water and Sanitation: 2014 Update (Joint Monitoring Programme for Water Supply and Sanitation) (WHO, 2012).
Amour, C. et al. Epidemiology and impact of campylobacter infection in children in 8 low-resource settings: Results from the MAL-ED study. Clin. Infect. Dis. 63(9), 1171–1179 (2016).
Rogawski, E. T. et al. Use of quantitative molecular diagnostic methods to investigate the effect of enteropathogen infections on linear growth in children in low-resource settings: Longitudinal analysis of results from the MAL-ED cohort study. Lancet Glob. Health 6(12), e1319–e1328 (2018).
De Benoist, B., Darnton-Hill, I., Davidsson, L., Fontaine, O. & Hotz, C. Conclusions of the joint WHO/UNICEF/IAEA/IZiNCG interagency meeting on zinc status indicators. Food Nutr. Bull. 28(3_suppl 3), S480–S484 (2007).
Gannon, B. M. et al. A point-of-care assay for alpha-1-acid glycoprotein as a diagnostic tool for rapid, mobile-based determination of inflammation. Curr. Res. Biotechnol. 1, 41–48 (2019).
Liu, J. et al. Development and assessment of molecular diagnostic tests for 15 enteropathogens causing childhood diarrhoea: A multicentre study. Lancet Infect. Dis. 14(8), 716–724 (2014).
Rogawsk, E. T. et al. Use of quantitative molecular diagnostic methods to investigate the effect of enteropathogen infections on linear growth in children in low-resource settings: Longitudinal analysis of results from the MAL-ED cohort study. Lancet Glob. Health 109(18), 30351 (2018).
The MAL-ED Network Investigators. The MAL-ED study: A multinational and multidisciplinary approach to understand the relationship between enteric pathogens, malnutrition, gut physiology, physical growth, cognitive development, and immune responses in infants and children up to 2 years of age in resource-poor environments. Clin. Infect. Dis. 59(suppl_4), S193–S206 (2014).
Kosek, M. et al. Fecal markers of intestinal inflammation and permeability associated with the subsequent acquisition of linear growth deficits in infants. Am. J. Trop. Med. Hyg. 88(2), 390–396 (2013).
Arndt, M. B. et al. Fecal markers of environmental enteropathy and subsequent growth in Bangladeshi children. Am. J. Trop. Med. Hyg. 95(3), 694–701 (2016).
Fahim, S. M. et al. Association of fecal markers of environmental enteric dysfunction with zinc and iron status among children at first two years of life in Bangladesh. Am. J. Trop. Med. Hyg. 99(2), 489–494 (2018).
Sanin, K. I. et al. Micronutrient adequacy is poor, but not associated with stunting between 12–24 months of age: A cohort study findings from a slum area of Bangladesh. PLoS ONE 13(3), e0195072 (2018).
Acknowledgements
We acknowledge with gratitude the commitment of The Etiology, Risk Factors, and Interactions of Enteric Infections and Malnutrition and the Consequences for Child Health and Development Project (MAL-ED) as a collaborative project supported by the Bill and Melinda Gates Foundation, the Foundation for the National Institutes of Health, and the National Institutes of Health, Fogarty International Center. The authors are grateful to MAL-ED staff, parents, and children for their contributions. We acknowledge the contribution of icddr,b’s core donors including the Government of the People’s Republic of Bangladesh, Global Affairs Canada, Canada; Swedish International Development Cooperation Agency and the Commonwealth and Development Office (FCDO), UK for their continuous support and commitment to icddr,b’s research efforts.
Funding
This work was supported, in whole or in part, by the Bill & Melinda Gates Foundation [Grant Number: OPP47075]. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission.
Author information
Authors and Affiliations
Contributions
T.A. conceptualized and designed the study. R.D., P.P., M.A.H., and A.S.G.F. conceived the hypothesis. M.A.H. managed the data set and provided technical support. R.D. analyzed the data. R.D. developed the tables/graphs presented here and wrote the first draft of the manuscript. P.P. wrote the methodology part on laboratory investigations of stool samples. P.P., M.A.H., M.M., A.S.G.F., and T.A. critically reviewed the manuscript and provided intellectual inputs. T.A. gave the final approval for publication. All authors contributed to the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Das, R., Palit, P., Haque, M.A. et al. Site specific incidence rate of genomic subtypes of enteropathogenic Escherichia coli and association with enteric inflammation and child growth. Sci Rep 12, 5724 (2022). https://doi.org/10.1038/s41598-022-09730-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-09730-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.