Abstract
The phenotypes of neovascular age-related macular degeneration (nAMD) are recognized as differing between Caucasian and Asian patients. Pachychoroid is thought to be more prevalent in Asians than in Caucasians, and may be involved in the development of nAMD in Asian patients. Therefore, we investigated the clinical characteristics and pachychoroid incidence in Japanese patients with nAMD. We retrospectively analyzed 385 eyes of 370 consecutive Japanese patients with treatment naïve nAMD. According to the nAMD nomenclature, type 1 macular neovascularization (MNV) was observed in 132 eyes (34.3%), polypoidal choroidal vasculopathy (PCV) in 137 (35.6%), mixed type 1 and type 2 MNV in 32 (8.3%), type 2 MNV in 43 (11.2%), and type 3 MNV in 41 (10.6%). Pachychoroid was seen in 58.3% of type 1 MNV, 75.2% of PCV, 34.4% of mixed type 1 and type 2 MNV, 14.0% of type 2 MNV, and 0% of type 3 MNV. Compared to nAMD patients without pachychoroid (188 eyes), those who had nAMD with pachychoroid (197 eyes) were significantly younger, had a higher proportion of males, greater central choroidal thickness, and a higher frequency of macular vortex vein anastomoses (all P < 0.001). Furthermore, drusen subtypes differed significantly between the two groups (P < 0.001). These results suggest that most Japanese nAMD patients might have type 1 MNV or PCV. Moreover, in approximately half of patients, nAMD might be associated with pachychoroid, and choroidal congestion may be involved in the development of MNV in these cases.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is a leading cause of visual impairment in developed countries1. Though numerous studies on the pathophysiology and optimal treatment of AMD have been conducted, the terminologies have not been consistent. To facilitate comparison of these diverse studies, a new terminology for neovascular AMD (nAMD) was established by the nAMD nomenclature study group in 20202. Macular neovascularization (MNV) was classified into types 1, 2 and 3, and mixed type 1 and type 2 MNV. Polypoidal choroidal vasculopathy (PCV) was categorized as a variant of type 1 MNV. Type 1 MNV refers to choroidal neovascularization (CNV) that grows into the subretinal pigment epithelium (RPE) space. Type 2 MNV refers to CNV that traverses the RPE and proliferates in the subretinal space. The definition of type 3 MNV is neovascularization that originates from the retinal circulation and grows toward the outer retina. Types 1, 2, and 3 MNV were previously referred to as occult CNV, classic CNV, and retinal angiomatous proliferation, respectively.
The phenotypes of nAMD are recognized as differing between Caucasian and Asian patients3,4,5,6. Drusen are more commonly observed in Caucasian than in Asian patients. On the other hand, the proportions of male and PCV patients are higher among Asians than Caucasians. These findings suggest that the mechanisms of MNV development in nAMD might differ, at least in some respects, between Asian and Caucasian patients. In 2013, the concept of pachychoroid was introduced, describing choroidal thickening associated with dilatation of outer choroidal vessels7. Pachychoroid is thought to be more prevalent in Asians than in Caucasians, and may be involved in the development of nAMD in Asian patients8. Our previous studies revealed that intervortex venous anastomosis is frequently observed in pachychoroid spectrum diseases9,10,11, and that the area of pachyvessels detected by en face optical coherence tomography (OCT) overlapped with the area of choriocapillaris filling delay detected in the early phase of indocyanine green angiography (ICGA)12,13. Therefore, we suggest that chronic ischemia of the choriocapillaris secondary to vortex vein congestion might be involved in the pathogenesis of pachychoroid spectrum diseases.
Soft drusen are sub-RPE deposits, which have been regarded as precursor lesions to nAMD and geographic atrophy3. Reticular pseudodrusen, first described in 199014, and then later in 2010, were proven to be subretinal drusenoid deposits15. Reticular pseudodrusen are also known to be precursor lesions to nAMD and geographic atrophy16. Pachydrusen (pachychoroid-associated drusen) were introduced as new type of sub-RPE deposits in 201817. It has been reported that choroidal thickness is significantly greater in eyes with pachydrusen than in eyes with soft drusen or reticular pseudodrusen17,18.
In this study, we assessed the prevalence of MNV subtypes in Japanese patients diagnosed with nAMD according to the nAMD nomenclature. Then, we investigated the pachychoroid incidence in each MNV subtype. Finally, we compared the demographic and clinical features including intervortex venous anastomosis and drusen subtype between the eyes of patients with nAMD with and without pachychoroid.
Results
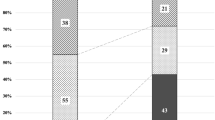
We retrospectively studied 385 eyes of 370 patients (271 eyes of 261 men; 114 eyes of 109 women) with previously untreated nAMD. The average patient age was 75.0 ± 9.9 years. The demographic and clinical characteristics of patients with nAMD are presented in Table 1. The type 1 MNV included 132 eyes of 130 patients (96 eyes of 95 men; 36 eyes of 35 women) with an average age of 72.9 ± 11.3 years (range: 45–96 years). PCV was diagnosed in 137 eyes of 132 patients (106 eyes of 102 men; 31 eyes of 30 women) with an average age of 74.8 ± 8.8 years (range: 52–94 years). Mixed type 1 and type 2 MNV was present in 32 eyes of 32 patients (25 eyes of 25 men; 7 eyes of 7 women) with an average age of 73.0 ± 9.3 years (range: 52–88 years). The type 2 MNV included 43 eyes of 43 patients (28 eyes of 28 men; 15 eyes of 15 women) with an average age of 76.5 ± 7.0 years (range: 59–91 years). Type 3 MNV was the diagnosis in 41 eyes of 35 patients (16 eyes of 13 men; 25 eyes of 22 women) with an average age of 82.3 ± 7.3 years (range: 65–94 years). Two patients showed type 1 MNV in one eye and mixed type 1 and type 2 MNV in the other eye. Of 385 eyes with nAMD, 301 (78.2%) had type 1 MNV or PCV, a variant of type 1 MNV. The average central choroidal thickness (CCT) was 259 ± 103 µm in type 1 MNV, 242 ± 101 µm in PCV, 215 ± 114 µm in mixed type 1 and type 2 MNV, 184 ± 89 µm in type 2 MNV, and 140 ± 61 µm in type 3 MNV, clearly diminishing in this order. Intervortex venous anastomosis was detected in 102 eyes (77.3%) with type 1 MNV, 125 (91.2%) with PCV, 26 (81.3%) with mixed type 1 and type 2 MNV, 26 (60.5%) with type 2 MNV, and 22 (53.7%) with type 3 MNV. As for drusen subtype, soft drusen and reticular pseudodrusen were more common in type 3 MNV. In the other MNV subtypes, pachydrusen were more common and about 30–40% of cases showed no drusen. Pachychoroid was seen in 77 eyes (58.3%) with type 1 MNV, 103 (75.2%) with PCV, 11 (34.4%) with mixed type 1 and type 2 MNV, 6 (14.0%) with type 2 MNV, but none with type 3 MNV.
The comparison between nAMD with and without pachychoroid is presented in Table 2. nAMD without pachychoroid included 188 eyes of 181 patients (113 eyes of 109 men; 75 eyes of 72 women) with an average age of 78.2 ± 8.0 years. The average CCT was 183 ± 90 µm. Intervortex venous anastomosis was detected in 115 eyes (61.2%). Soft drusen were seen in 54 eyes, pseudodrusen in 55, and pachydrusen in 77, while 51 eyes had no drusen. On the other hand, nAMD with pachychoroid was seen in 197 eyes of 189 patients (158 eyes of 152 men; 39 eyes of 37 women) with an average age of 71.9 ± 10.5 years. The average CCT was 272 ± 100 µm. Intervortex venous anastomosis was confirmed in 186 eyes (94.4%). Soft drusen were observed in 9 eyes, pseudodrusen in 4, and pachydrusen in 110, while 82 eyes had no drusen. Compared to those who had nAMD without pachychoroid, patients who had nAMD with pachychoroid were significantly younger, the proportion of males was higher, CCTs were greater, and the frequency of intervortex venous anastomosis was higher (all P < 0.001). Moreover, drusen subtypes differed significantly between the two groups (P < 0.001).
Discussion
We retrospectively studied 385 eyes of 370 patients with previously untreated nAMD. Type 1 MNV was observed in 132 eyes (34.3%), PCV in 137 (35.6%), mixed type 1 and type 2 MNV in 32 (8.3%), type 2 MNV in 43 (11.2%), and type 3 MNV in 41 (10.6%). Pachychoroid was seen in 58.3% of type 1 MNV, 75.2% of PCV, 34.4% of mixed type 1 and type 2 MNV, 14.0% of type 2 MNV, and 0% of type 3 MNV. Compared to those who had nAMD without pachychoroid, patients who had nAMD with pachychoroid were significantly younger, the proportion of males was higher, CCTs were greater, and the frequency of macular vortex anastomoses was higher. Moreover, drusen subtypes differed significantly between the two groups.
PCV reportedly accounts for a higher percentage of nAMD in Asian than in Caucasian patients6. Maruko et al. investigated the clinical characteristics of nAMD in Japanese patients in a hospital-based retrospective study. They reported in 2007 that the proportions of PCV and typical AMD among nAMD cases were 60.2% and 40.8%, respectively, including the patients with binocular nAMD6. However, in the current study, PCV patients accounted for 35.7% (132 of 370 cases), which was obviously a lower proportion than in the previous report. Moreover, type 1, mixed type 1 and type 2, and type 2 MNV, which were previously classified as typical AMD, together accounted for 55.4% (205 of 370 cases), i.e., a higher proportion than in the previous report. In Japan, AMD is the fourth leading cause of visual impairment19, and awareness of the disease has been rising. Therefore, it is possible that patients are seeing ophthalmologists earlier than in the past, leading to earlier detection of nAMD. It is also possible that nAMD is being detected at an earlier stage than before due to the widespread use of OCT and OCT angiography (OCTA). In fact, a multicenter study of Japanese patients with nAMD from 2006 to 2015 demonstrated significantly better visual acuity at initial diagnosis over time20, suggesting that more cases are receiving a diagnosis of nAMD before the disease has progressed. PCV is reportedly categorized as one of the pachychoroid spectrum diseases, and it has been suggested that the disease progresses in the order of central serous chorioretinopathy, pachychoroid neovasculopathy, and PCV10,11,21. Therefore, more cases might be referred to our university hospital before PNV progresses to PCV. PNV was originally defined as type 1 MNV accompanied by pachychoroid22. According to this definition, 58.3% of eyes with type 1 MNV were considered to have PNV in our study. Thus, it can be inferred that the proportion of PCV cases was lower and the proportion of type 1 MNV cases was higher herein than in the previous study. In addition, our previous studies have shown that PNV is characterized by a significantly thicker choroid than PCV (PNV with polypoidal lesions)10,11. This may be the reason for type 1 MNV showing the same choroidal thickness as PCV, even though the incidence of pachychoroid was lower than that of PCV.
It has been suggested that pachychoroid is involved in the development of nAMD in Asians, and various studies have examined this issue in recent years8. However, there is currently no established definition of pachychoroid, and eligibility criteria vary from study to study23. Recently, dilatation of the outer choroidal vessels accompanied by thinning of Sattler’s layer and the choriocapillaris have come to be considered the most important features of pachychoroid24. If these findings are present, pachychoroid is often diagnosed even if there is no obvious choroidal thickening. Therefore, in this study, pachychoroid was diagnosed if B-mode OCT showed dilatation of outer choroidal vessels accompanied by thinning of Sattler’s layer and the choriocapillaris, as well as the presence of MNV directly above them. Thus, pachychoroid was seen in 51.2% of eyes with nAMD in our study. Miyake et al. reported in 2015 that one fourth of Japanese cases had previously been diagnosed as having nAMD associated with pachychoroid25. In their study, subfoveal choroidal thickness and the absence of drusen were also included in the eligibility criteria, which may have lowered the incidence of pachychoroid in Japanese nAMD patients as compared to that in our study. However, they recently reported that 46.2% of Japanese nAMD patients showed pachychoroid-related features using deep phenotype unsupervised machine learning26, observations consistent with our results. Our findings suggest that pachychoroid may play a significant role in the development of nAMD in Japanese. Moreover, pachychoroid spectrum diseases have been found to be more prevalent in males10,11, which may account for the high percentage of males among Japanese nAMD patients.
In this study, intervortex venous anastomosis was detected at a significantly higher rate in nAMD with pachychoroid (94.4%) than in nAMD without pachychoroid (61.2%). Our prior study revealed that 40–50% of normal eyes showed intervortex venous anastomosis using en face OCT images27. Therefore, there may have been tiny anastomotic vessels between the superior and inferior vortex veins prior to the routine detection of any abnormalities. If the vortex veins are congested, the tiny anastomotic vessels might be dilated and easily recognized as intervortex venous anastomosis on en face OCT images. In the current study, intervortex venous anastomosis was frequently detected in nAMD with pachychoroid. However, 61.2% of eyes with nAMD without pachychoroid showed intervortex venous anastomosis, i.e., this finding was more common than in normal eyes. Therefore, mild congestion of vortex veins might be involved in the formation of intervortex venous anastomosis in nAMD without pachychoroid. In our previous study, we demonstrated pachydrusen to frequently be localized within the choriocapillaris filling delay in eyes with CSC28. Therefore, we speculate that circulation impairment in the choriocapillaris due to choroidal congestion might induce the development of pachydrusen. In the present study, 77 of 188 eyes (41.0%) without pachychoroid showed pachydrusen. These results also support the possibility that mild congestion of vortex veins may exist in some eyes with nAMD without pachychoroid.
In recent years, MNV has often been divided into drusen-driven and pachychoroid-driven based on the differences in their developmental mechanisms8,21. In the current study, 197 of 385 (51.2%) eyes with nAMD had associated pachychoroid. However, soft drusen and/or reticular pseudodrusen were also seen in 10 of these 197 (5.1%) eyes with pachychoroid. These cases may have a condition representing an overlap between drusen-driven and pachychoroid-driven MNV. On the other hand, eyes without pachychoroid were considered to have drusen-driven MNV, though, in fact, only 59 of 188 (31.9%) eyes without pachychoroid showed soft drusen and/or reticular pseudodrusen. Therefore, not all eyes without pachychoroid have drusen-driven MNV, which means there are idiopathic MNV cases that are neither pachychoroid-driven nor drusen-driven. However, the choroid is a tissue with high plasticity29. Even in eyes with pachychoroid, remodeling of the choroidal drainage route may reduce dilatation of the outer choroidal vessels over time, resulting in an OCT image that looks as if there is no pachychoroid. It is also possible that there are cases of MNV due to chronic ischemia of the choriocapillaris, although the vortex vein congestion is mild and there is no obvious dilatation of the outer choroidal vessels on OCT images. Such cases may, in this study, have been included among those without pachychoroid, and neither soft nor reticular pseudodrusen.
The limitations of this study include that it was single-center and retrospective, some cases with poor quality images were excluded, CCT was measured manually, pachychoroid and intervortex venous anastomosis were determined subjectively, OCT focused on the posterior pole of the fundus demonstrates only the posterior portion of the choroidal circulation, and all cases were Japanese such that the results may not be generalizable to other racial or ethnic groups.
In conclusion, most Japanese nAMD patients had type 1 MNV or PCV. About half of nAMD patients might have associated pachychoroid, and choroidal congestion may be involved in the development of MNV in these cases.
Methods
We performed this study, in compliance with the Declaration of Helsinki guidelines, after obtaining approval from the Institutional Review Board of Gunma University Hospital. Informed consent was obtained from all individual participants included in the present study. We retrospectively studied consecutive patients diagnosed with treatment naïve nAMD, followed clinically from January 2018 through December 2020 at Gunma University Hospital. We excluded patients with low quality multimodal imaging, under −6.0 diopter of refractive error in the phakic eye, or posterior staphyloma in the pseudophakic eye.
According to our previous studies9,10,11,13,30, all patients underwent a complete ophthalmological examination, including slit-lamp biomicroscopy with a noncontact fundus lens (SuperField lens; Volk Optical Inc., Mentor, OH), color fundus photography and fundus autofluorescence (Canon CX-1; Canon, Tokyo, Japan), fluorescein angiography and ICGA with an angle of 30 degrees (Spectralis HRA + OCT; Heidelberg Engineering, Heidelberg, Germany), as well as swept-source OCT (DRI OCT-1 Triton; Topcon Corp, Tokyo, Japan, and PLEX Elite 9000; Carl Zeiss Meditec, Dublin, CA, USA). The DRI OCT-1 Triton and PLEX Elite 9000 devices incorporate a tunable laser with a 1050 nm central wavelength and acquire 100,000 A-scans/second. The DRI OCT-1 Triton has an axial resolution of 8 μm and a lateral resolution of 20 μm, while the PLEX Elite 9000 has an axial resolution of 6.5 μm and a lateral resolution of 20 μm. We obtained B-mode images of the horizontal and vertical line scans (12 mm) and radial scans (9 mm) through the fovea employing the DRI OCT-1 Triton. Next, cube data were obtained with a raster scan protocol of 1024 (horizontal) × 1024 (vertical) B-scans, which covered the 12 × 12 mm area centered on the fovea by the PLEX Elite 9000. En face images were obtained from the vitreous to the choroidoscleral border with coronal slices from a 3-dimensional dataset included in the inner software. Then, we performed OCTA volume scanning, i.e., 300 × 300 pixels in the 3 × 3 mm area demonstrated by the PLEX Elite 9000. The OCTA thus performed was based on an optical microangiography algorithm.
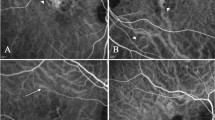
Following the nAMD nomenclature2, we classified nAMD according to MNV subtypes: Type 1 MNV, PCV, mixed type 1 and type 2 MNV, type 2 MNV, and type 3 MNV. Then, we investigated the pachychoroid incidence in each MNV subtype. In the current study, pachychoroid was diagnosed if B-mode OCT showed dilatation of the outer choroidal vessels accompanied by thinning of Sattler’s layer and the choriocapillaris, as well as the presence of MNV directly above them. Finally, we categorized nAMD into two groups, with and without pachychoroid, and compared the demographic and clinical features including age, gender, CCT, incidence of intervortex venous anastomosis, and drusen subtype between the two groups. CCT was measured on B-mode images using the computer-based caliper measurement tool included in the OCT system. CCT was defined as the distance between Bruch’s membrane and the margin of the choroid and sclera under the fovea. Intervortex venous anastomosis was considered to be present if anastomotic vessels connected the superior and inferior vortex veins on en face OCT images. The anastomotic vessels did not show narrowing toward the watershed zone9,10,11. En face OCT images at a depth of every 8 µm in the choroid were assessed. Drusen subtype was determined using fundus photographs according to previous studies15,17. If multiple drusen subtypes existed in the eye, they were counted in duplicate. The presence of pachyvessels on B-mode OCT images and anastomosis between the superior and inferior vortex veins on en face OCT images as well as drusen type were judged by two experienced retinal specialists (H. Matsumoto and J. Hoshino), working together.
For statistical analyses, the Mann–Whitney U test was used to compare unpaired values of age and CCT. The chi-squared independence test was used to determine differences in gender, the incidence of vortex vein anastomosis, and drusen type. The data analyses were performed using Excel (Microsoft, Redmond, WA, USA) with add-in software Statcel431. A P < 0.05 was considered to indicate a statistically significant difference. Age and CCT are presented as the average ± standard deviation.
References
Wong, T. Y. et al. The natural history and prognosis of neovascular age-related macular degeneration: a systematic review of the literature and meta-analysis. Ophthalmology 115, 116–126. https://doi.org/10.1016/j.ophtha.2007.03.008 (2008).
Spaide, R. F. et al. Consensus nomenclature for reporting neovascular age-related macular degeneration data: consensus on neovascular age-related macular degeneration nomenclature study group. Ophthalmology 127, 616–636. https://doi.org/10.1016/j.ophtha.2019.11.004 (2020).
Klein, R., Klein, B. E., Tomany, S. C., Meuer, S. M. & Huang, G. H. Ten-year incidence and progression of age-related maculopathy: the beaver dam eye study. Ophthalmology 109, 1767–1779. https://doi.org/10.1016/s0161-6420(02)01146-6 (2002).
Mitchell, P., Wang, J. J., Foran, S. & Smith, W. Five-year incidence of age-related maculopathy lesions: the blue mountains eye study. Ophthalmology 109, 1092–1097. https://doi.org/10.1016/s0161-6420(02)01055-2 (2002).
Oshima, Y. et al. Prevalence of age related maculopathy in a representative Japanese population: the Hisayama study. Br. J. Ophthalmol. 85, 1153–1157. https://doi.org/10.1136/bjo.85.10.1153 (2001).
Maruko, I., Iida, T., Saito, M., Nagayama, D. & Saito, K. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am. J. Ophthalmol. 144, 15–22. https://doi.org/10.1016/j.ajo.2007.03.047 (2007).
Warrow, D. J., Hoang, Q. V. & Freund, K. B. Pachychoroid pigment epitheliopathy. Retina 33, 1659–1672. https://doi.org/10.1097/IAE.0b013e3182953df4 (2013).
Yanagi, Y. Pachychoroid disease: a new perspective on exudative maculopathy. Jpn. J. Ophthalmol. 64, 323–337. https://doi.org/10.1007/s10384-020-00740-5 (2020).
Matsumoto, H., Kishi, S., Mukai, R. & Akiyama, H. Remodeling of macular vortex veins in pachychoroid neovasculopathy. Sci. Rep. 9, 14689. https://doi.org/10.1038/s41598-019-51268-9 (2019).
Matsumoto, H. et al. Vortex vein anastomosis at the watershed in pachychoroid spectrum diseases. Ophthalmol. Retina 4, 938–945. https://doi.org/10.1016/j.oret.2020.03.024 (2020).
Matsumoto, H. et al. Quantitative measures of vortex veins in the posterior pole in eyes with pachychoroid spectrum diseases. Sci. Rep. 10, 19505. https://doi.org/10.1038/s41598-020-75789-w (2020).
Kishi, S. et al. Geographic filling delay of the choriocapillaris in the region of dilated asymmetric vortex veins in central serous chorioretinopathy. PLoS ONE 13, e0206646. https://doi.org/10.1371/journal.pone.0206646 (2018).
Matsumoto, H. et al. Chronic choriocapillaris ischemia in dilated vortex vein region in pachychoroid neovasculopathy. Sci. Rep. 11, 16274. https://doi.org/10.1038/s41598-021-95904-9 (2021).
Mimoun, G., Soubrane, G. & Coscas, G. Macular drusen. J. Fr. Ophtalmol. 13, 511–530 (1990).
Zweifel, S. A., Spaide, R. F., Curcio, C. A., Malek, G. & Imamura, Y. Reticular pseudodrusen are subretinal drusenoid deposits. Ophthalmology 117, 303–312. https://doi.org/10.1016/j.ophtha.2009.07.014 (2010).
Zweifel, S. A., Imamura, Y., Spaide, T. C., Fujiwara, T. & Spaide, R. F. Prevalence and significance of subretinal drusenoid deposits (reticular pseudodrusen) in age-related macular degeneration. Ophthalmology 117, 1775–1781. https://doi.org/10.1016/j.ophtha.2010.01.027 (2010).
Spaide, R. F. Disease expression in nonexudative age-related macular degeneration varies with choroidal thickness. Retina 38, 708–716. https://doi.org/10.1097/IAE.0000000000001689 (2018).
Cheung, C. M. G., Gan, A., Yanagi, Y., Wong, T. Y. & Spaide, R. Association between choroidal thickness and drusen subtypes in age-related macular degeneration. Ophthalmol. Retina 2, 1196–1205. https://doi.org/10.1016/j.oret.2018.06.014 (2018).
Morizane, Y. et al. Incidence and causes of visual impairment in Japan: the first nation-wide complete enumeration survey of newly certified visually impaired individuals. Jpn. J. Ophthalmol. 63, 26–33. https://doi.org/10.1007/s10384-018-0623-4 (2019).
Sawada, T. et al. Ten-year changes in visual acuity at baseline and at 2 years after treatment in a Japanese population with age-related macular degeneration. Graefes Arch. Clin. Exp. Ophthalmol. 259, 1191–1198. https://doi.org/10.1007/s00417-020-05005-y (2021).
Cheung, C. M. G. et al. Pachychoroid disease. Eye (Lond.) 33, 14–33. https://doi.org/10.1038/s41433-018-0158-4 (2019).
Pang, C. E. & Freund, K. B. Pachychoroid neovasculopathy. Retina 35, 1–9. https://doi.org/10.1097/IAE.0000000000000331 (2015).
Spaide, R. F. The ambiguity of pachychoroid. Retina 41, 231–237. https://doi.org/10.1097/IAE.0000000000003057 (2021).
Castro-Navarro, V. et al. Pachychoroid: current concepts on clinical features and pathogenesis. Graefes Arch. Clin. Exp. Ophthalmol. 259, 1385–1400. https://doi.org/10.1007/s00417-020-04940-0 (2021).
Miyake, M. et al. Pachychoroid neovasculopathy and age-related macular degeneration. Sci. Rep. 5, 16204. https://doi.org/10.1038/srep16204 (2015).
Hosoda, Y. et al. Deep phenotype unsupervised machine learning revealed the significance of pachychoroid features in etiology and visual prognosis of age-related macular degeneration. Sci. Rep. 10, 18423. https://doi.org/10.1038/s41598-020-75451-5 (2020).
Hoshino, J. et al. Variation of vortex veins at the horizontal watershed in normal eyes. Graefes Arch. Clin. Exp. Ophthalmol. https://doi.org/10.1007/s00417-021-05130-2 (2021).
Matsumoto, H. et al. Clinical characteristics of pachydrusen in central serous chorioretinopathy. Graefes Arch. Clin. Exp. Ophthalmol. 257, 1127–1132. https://doi.org/10.1007/s00417-019-04284-4 (2019).
Takahashi, K. & Kishi, S. Remodeling of choroidal venous drainage after vortex vein occlusion following scleral buckling for retinal detachment. Am. J. Ophthalmol. 129, 191–198 (2000).
Matsumoto, H. et al. Pulsation of anastomotic vortex veins in pachychoroid spectrum diseases. Sci. Rep. 11, 14942. https://doi.org/10.1038/s41598-021-94412-0 (2021).
Yanai, H. Statcel: the useful add-in software forms on Excel 4th edn. (OMS, Tokyo, 2015).
Acknowledgements
Neither sponsors nor funding organizations were involved in this study.
Author information
Authors and Affiliations
Contributions
The authors were involved in the following aspects of the study: design and conduct (H.M., S.K.); collection of the data (H.M., J.H., K.N.); management (H.M.); analysis (H.M., J.H.); interpretation (H.M., J.H.); preparation of article (H.M.); review and approval of the manuscript (R.M., S.K., H.A.).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matsumoto, H., Hoshino, J., Mukai, R. et al. Clinical characteristics and pachychoroid incidence in Japanese patients with neovascular age-related macular degeneration. Sci Rep 12, 4492 (2022). https://doi.org/10.1038/s41598-022-08666-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-08666-3
This article is cited by
-
Evaluating photodynamic therapy versus brolucizumab as a second-line treatment for polypoidal choroidal vasculopathy
International Journal of Retina and Vitreous (2024)
-
Predicting treatment outcomes of intravitreal brolucizumab for polypoidal choroidal vasculopathy through noninvasive assessment of polypoidal lesion blood flow with optical coherence tomography angiography
Scientific Reports (2024)
-
One-year visual and anatomical outcomes of intravitreal faricimab injection for neovascular age-related macular degeneration after prior brolucizumab treatment
Scientific Reports (2024)
-
The hypothetical molecular mechanism of the ethnic variations in the manifestation of age-related macular degeneration; focuses on the functions of the most significant susceptibility genes
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Clinical Trials and Future Outlooks of the Port Delivery System with Ranibizumab: A Narrative Review
Ophthalmology and Therapy (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.