Abstract
Cataract is the leading cause of blindness worldwide, and advanced cataract techniques such as femtosecond laser-assisted cataract surgery (FLACS) have been commercially available. Corneal refractive surgery (CRS) is one of the most popular surgeries for the correction of refractive errors. CRS changes the cornea not only anatomically but also pathophysiologically. However, there has been no clinical research analyzing the refractive and safety outcomes of FLACS after CRS. The aim of this retrospective chart review and comparative study is to evaluate the effect and safety of FLACS after CRS comparing with conventional PCS. Participants with a previous CRS history who underwent FLACS or conventional PCS were included in this study. The visual outcomes and the refractive outcomes including refractive, corneal, and ocular residual astigmatism were compared. The safety outcomes were then studied intraoperatively and postoperatively. A total of 102 patients with age-related cataract were enrolled. At 3 months postoperatively, UCVA, BCVA, and predictive error were not significantly different between the FLACS and conventional PCS groups. Reduction of refractive astigmatism was higher in FLACS. Postoperative ORA was significant lower in FLACS. Reduction of ORA was higher in FLACS. The intraoperative and postoperative complications were also not significantly different between the two groups. FLACS could effectively change refractive astigmatism and ORA; without more complications than conventional PCS. FLACS’ competitive edge in postoperative ORA may provide better visual quality than conventional PCS in patients with a previous history of CRS.
Similar content being viewed by others
Introduction
Cataract is the leading cause of blindness worldwide1, and cataract surgery is one of the most commonly performed operations, with more than 30 million operations per year in the United States2. Phacoemulsification cataract surgery (PCS) became the standard method of cataract treatment1. Advanced cataract techniques such as multifocal intraocular lens (IOL), toric IOL, and femtosecond laser-assisted cataract surgery (FLACS) have been commercially available for over 10 years3,4,5. FLACS enables a well-centered and predetermined capsulotomy compared with the conventional method. This machine-controlled capsulorhexis can minimize IOL tiltation6,7, resulting in fewer higher-order aberrations8.
Corneal refractive surgery (CRS) is one of the most popular surgeries for correcting refractive errors, especially myopia9. In the United States, approximately 800,000 laser in situ keratomileuses (LASIK) procedures were performed annually.
Accurate IOL calculation for cataract surgery after CRS is a major challenge10. CRS alters the anterior corneal curvature and anterior to posterior corneal relationships, causing difficulty in predicting the effective lens position11. CRS also affects corneal thickness, integrity, and irregularity12. Because these changes cause an unpredictable deterioration of visual quality, accurate prediction, and intended outcome are important in patients with a previous history of CRS and must be confirmed.
To date, there has been no clinical research analyzing the refractive and safety outcomes of FLACS after CRS. Only a few case reports suggested the benefit of FLACS in patients with a previous history of CRS13,14. This study aimed to evaluate the effect and safety of FLACS after CRS comparing with conventional PCS.
Results
A total of 102 eyes of 102 patients with age-related cataracts and a previous history of CRS were included in this study. The mean follow-up period was 90.7 days [86–94 days]. Table 1 shows the baseline characteristics of the study population according to FLACS and conventional PCS. The baseline characteristics of FLACS and conventional PCS were not significantly different.
Table 2 shows the 3-month postoperative outcomes with indices of the Alpins method. There were no significant differences between FLACS and conventional PCS in terms of uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), and predictive error (p = 1.000, 1.000, and 0.796, respectively). The proportions of preoperative and postoperative refractive astigmatism ≤ 0.50 D were changed from 20 to 49% in FLACS and 18 to 49% in conventional PCS, and the changes in proportion were not significantly different between the two groups (p = 0.787). In the Alpins method, none of the indices differed between the two groups after adjustment for target-induced astigmatism (TIA). Postoperative ORA was 0.20 D (95% CI 0.05–0.35) lower in FLACS than in conventional PCS (p = 0.018).
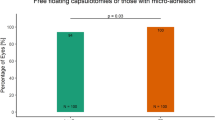
Figure 1 shows the changes in preoperative and postoperative refractive astigmatism and ORA after adjusting preoperative corneal astigmatism. In both FLACS and conventional PCS, postoperative refractive astigmatism was significantly reduced from 1.12 ± 0.56 to 0.86 ± 0.46 (p = 0.001) and 1.10 ± 0.79 to 0.76 ± 0.59 (p = 0.018), respectively. The reduction of refractive astigmatism was significantly higher in FLACS than in conventional PCS (p = 0.026). Postoperative ORA was significantly lower in FLACS than in conventional PCS (p = 0.018). The reduction of ORA was significantly higher in FLACS than in conventional PCS (p = 0.012).
Preoperative and postoperative refractive astigmatism (a), corneal astigmatism (b), and ocular residual astigmatism (c) in FLACS and conventional phacoemulsification cataract surgery. In the process of repeated measure ANOVA, preoperative corneal astigmatism significantly affected refractive astigmatism. *p < 0.05, †adjustment for preoperative corneal astigmatism.
Table 3 shows the intraoperative and postoperative complications according to the groups; no significant differences were observed between the groups (p = 0.727 and 0.647, respectively).
Discussion
The results of this study suggest that FLACS for patients with a previous history of CRS was more effective in the change of refractive astigmatism at the 3-month follow-up, which comes from postoperative ORA significantly lower in FLACS than in conventional PCS. FLACS was not accompanied by more complications compared with conventional PCS.
Because the target IOL (D) had been set not only for far vision or emmetropia but also for near vision, UCVA, BCVA, and prediction error were analyzed. UCVA, BCVA, and prediction error were not significantly different between FLACS and conventional PCS. The Barrett True-K formula is one of the most accurate IOL calculation formulas for patients with a previous history of CRS15, and the prediction error of the Barrett True-K formula was − 0.24, which was similar to those of our study.
Postoperative ORA was lower, and reduction of refractive astigmatism and ORA were significantly higher in FLACS than in conventional PCS. A multicenter, randomized study showed that FLACS had no advantage in corneal astigmatism, as in our study16, but it did not analyze the effect of FLACS on refractive astigmatism and ORA. ORA is composed of posterior corneal astigmatism, lens astigmatism, and retinal astigmatism17. The preoperative and postoperative posterior corneal astigmatism was not significantly different in this study. In a previous report, ORA, which also included a part of retinal astigmatism, was found to be inversely correlated with axial length and positively correlated with SE and corneal astigmatism18. In our study, axial length, SE, and both anterior and posterior corneal astigmatism were not significantly different between the two groups. Therefore, the difference in ORA between the two groups may be explained by lens astigmatism owing to lens tilt and decentration caused by the different capsulotomy methods between FLACS and conventional PCS6,7. Previous studies have reported that horizontal and vertical IOL tilt and decentration were significantly higher in manual capsulotomy and that the results showed a correlation with changes in refraction values between 1 month and 1 year after surgery. IOL tilt and decentration influence visual acuity, dysphotopsia, and coma-like aberrations19,20,21,22. Moreover, CRS also induced aberrations in a previous study23: the root-mean-square wavefront error increased 1.9-fold in a 6.5 mm pupil and significantly in a 3.0 mm pupil, and positive spherical aberration was increased fourfold after myopic LASIK. Oblate corneas that underwent myopic correction benefited from aspheric IOLs with negative spherical aberration, which compensates the positive corneal spherical aberration24, and aspheric IOLs are shown to produce more optical quality degradation if tilted or decentered25. Considering the visual impacts of the capsulotomy method and CRS, femtosecond laser may provide a higher quality of vision and have a greater impact on patients after CRS.
Trauma vulnerability is a concern in patients with a history of CRS26,27. The physical and thermal energy in the process of FLACS could damage the previous CRS-operated tissue28,29,30. However, the complication rates between FLACS and conventional PCS for patients with a history of CRS were not different intraoperatively and postoperatively in our study. The overall intraoperative and postoperative complication rates were 2.8% and 12.5% in FLACS in a previous study5, similar to ours. Specifically, posterior capsule tear rates were 0% for FLACS, as in the previous UK reports5,31. An intraoperative pupil contracture of 3.9% and incomplete laser capsulotomy of 5.9% were the challenges of FLACS5,32,33. There were two incomplete capsulotomy cases in FLACS, and they could be finished with manual capsulorhexis without any complications, their ORAs were not significantly high, within 95% CIs, compared with other FLACS cases. The focus size and pulse separation of laser system are the issue of this complication34. The LenSx femtosecond laser platform, which was used in this study, utilizes high energy and low frequency of laser pulse and relatively larger focus size, and this causes larger pulse separation than other femtosecond laser platforms. In this study, 1/102 participants developed postoperative anterior uveitis. In the UK reports, 9.7% of the FLACS group and 8.2% of the PCS group experienced postoperative anterior uveitis, which was higher than our study5. The 4-week steroid applied for a month of our protocol may decrease the complication.
There are certain limitations to our study. First, the results of this study did not involve the patients' subjective symptoms. In a Chinese report, FLACS resulted in the dry eye at postoperative day 1, week 1, and month 135. However, in the UK reports, the health-related quality of life and vision questionnaires did not show a significant difference between FLACS and conventional PCS5,36. After CRS, there was a possibility of visual disturbance, and other subjective dissatisfaction37, and the additional laser treatment could affect the subjective outcomes. Second, our study showed that FLACS had an advantage on ORA and that refractive astigmatism in FLACS was lower than that in conventional PCS after adjustment for preoperative corneal astigmatism. The influence of IOL-induced astigmatism on ORA and aberration was estimated and not directly measured. Further assessment of the patients’ subjective outcomes and analyses for ORA and aberration is required to investigate the effectiveness of FLACS after CRS. Third, the number of detailed complications was too small, and the follow-up period was relatively short to conduct the detailed analysis of FLACS complications. Therefore, we conducted the overall analysis. For example, zonule dialysis was about 4% of patients, which was different from the previous large-scale study, which reported zonule dialysis was about 0.5%38. This study could not determine that CRS increases the risk of zonule dialysis because the number of this complication was only one or two.
In conclusion, at the 3-month follow-up, FLACS was effective in terms of the change of refractive astigmatism and ORA. Moreover, FLACS was not accompanied by more complications compared with conventional PCS. The competitive edge of FLACS in postoperative ORA may provide better visual quality than conventional PCS in patients with a previous history of CRS.
Methods
The Severance Hospital Clinical Research Ethics Committee approved the study protocol (YUHS-SH-IRB-4-2021-0774). The study was conducted in accordance with the tenets of the Declaration of Helsinki, and informed consent was obtained from the subjects after an explanation of the nature and possible consequences of the study.
Study design and patients
This retrospective comparative study was performed at the Severance Hospital, Yonsei University College of Medicine, between June 2018 and December 2020. The patients with a history of the CRS (LASIK, laser epithelial keratomileusis [LASEK], and photorefractive keratectomy [PRK]) and conducted 3-month follow-up were enrolled. Exclusion criteria were as follows: (a) significant visual impairing diseases such as central corneal opacity, diabetic retinopathy, macular degeneration, and advanced glaucoma, (b) previous history of the complication of CRS (i.e., corneal ectasia), and (c) corneal astigmatism > 1.25 D with any of astigmatism correcting procedures (i.e., arcuate keratotomy and toric IOL insertion). The patients were classified into two groups of 51 patients each: FLACS and conventional PCS. The participants in the conventional PCS group were selected by the computerized matched sampling of age, sex, types of CRS, surgeons, preoperative spherical equivalent and refractive astigmatism, and preoperative corneal power and astigmatism by using Python version 3.8 (https://www.python.org).
Procedures
All participants underwent a detailed preoperative ophthalmological evaluation, including slit-lamp and fundus examinations. IOL power calculation was performed using optical biometry (IOLMaster 700, Carl Zeiss Meditec AG). Corneal measurement was based on Scheimpflug tomography (Pentacam, Oculus Inc.) simulated K performed within 2 weeks before the surgery. All participants underwent FLACS or conventional PCS with the femtosecond system (LenSx, Alcon Laboratories, Inc.) under topical anesthesia.
The surgical procedures of FLACS and conventional PCS after the femtosecond laser procedure were similar. The clear corneal incision on the temporal side was created using a 2.65–2.80 mm keratome, and the anterior capsule button was removed. In the conventional PCS group, capsulotomy was performed using a capsulotomy needle or forceps. Phacoemulsification was performed using the Centurion vision system (Alcon Laboratories, Inc.). Patients with a single aspherical lens, Tecnis 1-piece intraocular lens (Johnson & Johnson), were enrolled in this study. All operations were performed by experienced surgeons (I.J., K.Y.S., and T.I.K). Postoperative care, including empirical antibiotics and anti-inflammatory medications, was administered as per standard unit practice for cataract surgery for a month.
Outcomes
The primary outcomes were best-corrected visual acuity (BCVA, decimal scaled), and the refractive outcomes were postoperative spherical equivalent (SE), prediction error, refractive astigmatism, corneal power, corneal astigmatism with vector analysis by the Alpins method in the ACRS website, and ocular residual astigmatism (ORA) at the 3-month follow-up39. Prediction error was calculated as the difference of target IOL [diopters (D)] using the Barrett True-K formula and postoperative SE. The vector analysis includes eight indices: TIA, defined as the astigmatic change that the surgery was intended to induce or preoperative astigmatism; surgically induced astigmatism vector (SIA), defined as the astigmatic change that the surgery actually induced; and difference vector (DV), defined as the induced astigmatic change that would enable the initial surgery to achieve its intended target or postoperative astigmatism, the magnitude of error (SIA minus TIA), angle of error (AE, angle between TIA vector and SIA vector), the absolute value of AE, correction index (SIA divided by TIA), and index of success (DV divided by TIA). ORA was calculated using refractive astigmatism and corneal anterior astigmatism values40,41. The secondary outcomes were the safety outcomes of intra- and postoperative complications5.
Statistical analysis
The study was framed as a comparative design focusing on BCVA, predictive error, refractive outcomes, and safety outcomes. Because TIA is known to affect SIA and other indices of the Alpins method42, a comparative analysis was performed using the Alpins method with the adjustment of TIA. Comparisons of preoperative and postoperative values in each group were analyzed using the paired t test. Comparative analyses for change of continuous and categorical values between the two groups were analyzed using the repeated measures ANOVA after adjustment with statistically significant parameters among age, sex, laterality, types of CRS, surgeon, preoperative SE, preoperative corneal power and astigmatism, axis group of preoperative corneal astigmatism, axial length and anterior chamber depth. A p value < 0.05 was considered statistically significant, and a 95% confidence interval (CI) was calculated.
References
Bourne, R. R. et al. Causes of vision loss worldwide, 1990–2010: A systematic analysis. Lancet Glob. Health 1(6), e339–e349 (2013).
CY 2019 Top 200 Level II HCPCS Codes Ranked by Charges (PDF) (Centers for Medicare & Medicaid Services) (2021).
Khandelwal, S. S., Jun, J. J., Mak, S., Booth, M. S. & Shekelle, P. G. Effectiveness of multifocal and monofocal intraocular lenses for cataract surgery and lens replacement: A systematic review and meta-analysis. Graefes Arch. Clin. Exp. Ophthalmol. 257(5), 863–875 (2019).
Kessel, L. et al. Toric intraocular lenses in the correction of astigmatism during cataract surgery: A systematic review and meta-analysis. Ophthalmology 123(2), 275–286 (2016).
Day, A. C. et al. Femtosecond laser-assisted cataract surgery versus phacoemulsification cataract surgery (FACT): A randomized noninferiority trial. Ophthalmology 127(8), 1012–1019 (2020).
Nagy, Z. Z. et al. Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. J. Refract. Surg. 27(8), 564–569 (2011).
Kránitz, K. et al. Intraocular lens tilt and decentration measured by Scheimpflug camera following manual or femtosecond laser-created continuous circular capsulotomy. J. Refract. Surg. 28(4), 259–263 (2012).
Miháltz, K. et al. Internal aberrations and optical quality after femtosecond laser anterior capsulotomy in cataract surgery. J. Refract. Surg. 27(10), 711–716 (2011).
Jabbour, S. & Bower, K. S. Refractive surgery in the US in 2021. JAMA 326(1), 77–78 (2021).
Savini, G. & Hoffer, K. J. Intraocular lens power calculation in eyes with previous corneal refractive surgery. Eye Vis. 5(1), 1–10 (2018).
Gimbel, H., Sun, R. & Kaye, G. B. Refractive error in cataract surgery after previous refractive surgery. J. Cataract Refract. Surg. 26(1), 142–144 (2000).
Pinheiro, M. N. Jr. et al. Corneal integrity after refractive surgery: Effects of radial keratotomy and mini-radial keratotomy. Ophthalmology 102(2), 297–301 (1995).
Huang, P.-W., Huang, W.-H., Tai, Y.-C. & Sun, C.-C. Femtosecond laser-assisted cataract surgery in a patient with traumatic cataract and corneal opacity after LASIK: A case report. BMC Ophthalmol. 20(1), 1–4 (2020).
Wang, W. et al. Femtosecond laser-assisted cataract surgery with implantation of a diffractive trifocal intraocular lens after laser in situ keratomileusis: A case report. BMC Ophthalmol. 18(1), 1–5 (2018).
Yeo, T. K., Heng, W. J., Pek, D., Wong, J. & Fam, H. B. Accuracy of intraocular lens formulas using total keratometry in eyes with previous myopic laser refractive surgery. Eye 35(6), 1705–1711 (2021).
Schweitzer, C. et al. Femtosecond laser-assisted versus phacoemulsification cataract surgery (FEMCAT): A multicentre participant-masked randomised superiority and cost-effectiveness trial. Lancet 395(10219), 212–224 (2020).
Alpins, N., Ong, J. K. & Stamatelatos, G. New method of quantifying corneal topographic astigmatism that corresponds with manifest refractive cylinder. J. Cataract Refract. Surg. 38(11), 1978–1988 (2012).
Liu, Y. et al. Evaluating internal and ocular residual astigmatism in Chinese myopic children. Jpn. J. Ophthalmol. 61(6), 494–504 (2017).
Madrid-Costa, D. et al. Visual simulation through different intraocular lenses using adaptive optics: Effect of tilt and decentration. J. Cataract Refract. Surg. 38(6), 947–958 (2012).
Hayashi, K., Yoshida, M. & Hayashi, H. All-distance visual acuity and contrast visual acuity in eyes with a refractive multifocal intraocular lens with minimal added power. Ophthalmology 116(3), 401–408 (2009).
Tester, R., Pace, N. L., Samore, M. & Olson, R. J. Dysphotopsia in phakic and pseudophakic patients: Incidence and relation to intraocular lens type. J. Cataract Refract. Surg. 26(6), 810–816 (2000).
Taketani, F., Matuura, T., Yukawa, E. & Hara, Y. Influence of intraocular lens tilt and decentration on wavefront aberrations. J. Cataract Refract. Surg. 30(10), 2158–2162 (2004).
Moreno-Barriuso, E. et al. Ocular aberrations before and after myopic corneal refractive surgery: LASIK-induced changes measured with laser ray tracing. Invest. Ophthalmol. Vis. Sci. 42(6), 1396–1403 (2001).
Kohnen, T., Mahmoud, K. & Bühren, J. Comparison of corneal higher-order aberrations induced by myopic and hyperopic LASIK. Ophthalmology 112(10), 1692.e1-1692.e11 (2005).
Lawu, T., Mukai, K., Matsushima, H. & Senoo, T. Effects of decentration and tilt on the optical performance of 6 aspheric intraocular lens designs in a model eye. J. Cataract Refract. Surg. 45(5), 662–668 (2019).
Jabbur, N. S., Sakatani, K. & O’Brien, T. P. Survey of complications and recommendations for management in dissatisfied patients seeking a consultation after refractive surgery. J. Cataract Refract. Surg. 30(9), 1867–1874 (2004).
Dudenhoefer, E. J., Vinger, P. F. & Azar, D. T. Trauma after refractive surgery. Int. Ophthalmol. Clin. 42(3), 33–45 (2002).
De Medeiros, F. W. et al. Effect of femtosecond laser energy level on corneal stromal cell death and inflammation. J. Refract. Surg. 25(10), 869–874 (2009).
Shimmura, S. et al. Excimer laser-induced hydroxyl radical formation and keratocyte death in vitro. Invest. Ophthalmol. Vis. Sci. 40(6), 1245–1249 (1999).
Maatz, G. et al. Chemical and physical side effects at application of ultrashort laser pulses for intrastromal refractive surgery. J. Opt. A Pure Appl. Opt. 2(1), 59 (2000).
Roberts, H. W. et al. A randomized controlled trial comparing femtosecond laser-assisted cataract surgery versus conventional phacoemulsification surgery. J. Cataract Refract. Surg. 45(1), 11–20 (2019).
Abell, R. G. et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: Outcomes and safety in more than 4000 cases at a single center. J. Cataract Refract. Surg. 41(1), 47–52 (2015).
Diakonis, V. F. et al. Effects of femtosecond laser-assisted cataract pretreatment on pupil diameter: A comparison between three laser platforms. J. Refract. Surg. 32(2), 84–88 (2016).
Latz, C., Asshauer, T., Rathjen, C. & Mirshahi, A. Femtosecond-laser assisted surgery of the eye: Overview and impact of the low-energy concept. Micromachines 12(2), 122 (2021).
Yu, Y. et al. Evaluation of dry eye after femtosecond laser-assisted cataract surgery. J. Cataract Refract. Surg. 41(12), 2614–2623 (2015).
Lundström, M. et al. Risk factors for refractive error after cataract surgery: Analysis of 282 811 cataract extractions reported to the European Registry of Quality Outcomes for cataract and refractive surgery. J. Cataract Refract. Surg. 44(4), 447–452 (2018).
Fan-Paul, N. I., Li, J., Miller, J. S. & Florakis, G. J. Night vision disturbances after corneal refractive surgery. Surv. Ophthalmol. 47(6), 533–546 (2002).
Trikha, S., Agrawal, S., Saffari, S., Jayaswal, R. & Yang, Y. Visual outcomes in patients with zonular dialysis following cataract surgery. Eye 30(10), 1331–1335 (2016).
Reinstein, D. Z., Archer, T. J. & Randleman, J. B. JRS Standard for Reporting Astigmatism Outcomes of Refractive Surgery (SLACK Incorporated Thorofare, 2014).
Alpins, N. A. New method of targeting vectors to treat astigmatism. J. Cataract Refract. Surg. 23(1), 65–75 (1997).
Lin, J. The contribution of ocular residual astigmatism to anterior corneal astigmatism in refractive astigmatism eyes. Sci. Rep. 11(1), 1–6 (2021).
Chan, T. C. et al. Vector analysis of corneal astigmatism after combined femtosecond-assisted phacoemulsification and arcuate keratotomy. Am. J. Ophthalmol. 160(2), 250-255.e2 (2015).
Author information
Authors and Affiliations
Contributions
H.A. conception or design of the work, data collection, data analysis and interpretation, writing the manuscript; I.J., K.Y.S., E.K.K. critical revision of the article; T.K. conception or design of the work, data analysis and interpretation, critical revision of the article. All authors have approved the final version of to be published. All persons designated as authors qualify for authorship.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahn, H., Jun, I., Seo, K.Y. et al. Femtosecond laser-assisted cataract surgery after corneal refractive surgery. Sci Rep 12, 4263 (2022). https://doi.org/10.1038/s41598-022-08297-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-08297-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.