Abstract
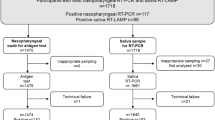
The COVID-19 pandemic has resulted in significant diversion of human and material resources to COVID-19 diagnostics, to the extent that influenza viruses and co-infection in COVID-19 patients remains undocumented and pose serious public-health consequences. We optimized and validated a highly sensitive RT-PCR based multiplex-assay for the detection of SARS-CoV-2, influenza A and B viruses in a single-test. This study evaluated clinical specimens (n = 1411), 1019 saliva and 392 nasopharyngeal swab (NPS), tested using two-assays: FDA-EUA approved SARS-CoV-2 assay that targets N and ORF1ab gene, and the PKamp-RT-PCR based assay that targets SARS-CoV-2, influenza viruses A and B. Of the 1019 saliva samples, 17.0% (174/1019) tested positive for SARS-CoV-2 using either assay. The detection rate for SARS-CoV-2 was higher with the multiplex assay compared to SARS-specific assay [91.9% (160/174) vs. 87.9% (153/174)], respectively. Of the 392 NPS samples, 10.4% (41/392) tested positive for SARS-CoV-2 using either assay. The detection rate for SARS-CoV-2 was higher with the multiplex assay compared to SARS-specific assay [97.5% (40/41) vs. 92.1% (39/41)], respectively. This study presents clinical validation of a multiplex-PCR assay for testing SARS-CoV-2, influenza A and B viruses, using NPS and saliva samples, and demonstrates the feasibility of implementing the assay without disrupting the existing laboratory workflow.
Similar content being viewed by others
Introduction
The outbreak of COVID-19 (caused by SARS-CoV-2) is currently a raging pandemic and has led to major socio-economic disruption worldwide. Since the identification of SARS-CoV-2 in the region of Wuhan, China, 77,343,652 confirmed cases with over 1,702,293 COVID-19 related deaths have been reported globally (https://coronavirus.jhu.edu/map.html, last accessed December 21, 2020). In an attempt to curtail the spread of the disease, testing for SARS-CoV-2 has been identified as the single most important measure. Substantial emergency policy changes as well as state-sponsored funding have facilitated implementation of testing for the virus in the USA and around the world1,2. However, due to the diversion of personnel, resources, and supplies to SARS-CoV-2 testing, the testing of viral pathogens that normally cause seasonal respiratory tract infections has been marginalized. Acute respiratory tract infections (ARTIs) remain the leading cause of morbidity and mortality from infectious diseases. The Global Burden of Disease (2017) data has demonstrated that influenza contributed 11.5% of the total lower respiratory tract infections (LRTIs), leading to over 9 million hospitalizations and 145,000 deaths across all age groups in a single calendar year3. Further, co-infection with bacterial, fungal, or viral pathogens has been associated with disease severity and death in the current pandemic. A report originating from Wuhan, China, identified that 80% of COVID-19 patients had co-infection with at least one respiratory pathogen, with the most common being influenza viruses A and B (60% and 53.30% respectively)4. The neglect of these co-circulating pathogens, especially influenza A and B viruses has generated serious public health gaps both at a clinical and epidemiological level. The potential impact of co-circulating respiratory viral pathogens during the ongoing influenza season is of major concern at both local and international public health levels. Further, with the COVID-19 vaccination already in use, testing for pathogens, especially the influenza viruses in addition to SARS-CoV-2, is already becoming the next diagnostic testing emergency.
We must remain cognizant of the fact that the pandemic has caused a significant change in routine clinical diagnostic laboratories at the level of re-directing workflow, workforce, supplies, and validating new diagnostic tests5. It is only in the last few months that laboratories have streamlined testing for SARS-CoV-2, and therefore shifting to a new workflow and implementing new diagnostic tests, would only unsettle the already exhausted laboratory staff. To address these clinical and technical challenges, we have optimized and validated a highly sensitive RT-PCR based multiplex assay for the detection of SARS-CoV-2, influenza A and B viruses in a single test, using the same workflow, instruments, sample types, supplies, and laboratory personnel currently utilized for SARS-CoV-2 testing (Fig. 1). Additionally, the assay was validated for both nasopharyngeal swab (NPS) and saliva samples and demonstrated higher sensitivity in detecting SARS-CoV-2 virus compared to the FDA-EUA comparator assay (SARS-CoV-2 detection only). We contend that this novel multiplex assay can be used to screen for influenza viruses along with the detection of SARS-CoV-2 and can be readily implemented in laboratories across the globe, using essentially the same workflow and rapid turnaround time (TAT).
Material and methods
Study site and ethics
This single-center diagnostic study was conducted at Augusta University, GA, USA. This site is a Clinical Laboratory Improvement Amendments (CLIA) accredited laboratory for high complexity testing and is one of the main SARS-CoV-2 testing centers in the State of Georgia. The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board A- BIOMEDICAL I (IRB REGISTRATION #00000150), Augusta University. HAC IRB # 611298. Based on the IRB approval, the need for consent was waived, all PHI was removed and all data was anonymized before accessing for the study.
Patient specimens and setting
The study evaluated 1411 clinical specimens that included 1019 saliva and 392 NPS samples collected in either healthcare or community setting, tested using both the FDA-EUA approved SARS-CoV-2 and the PKamp RT-PCR based assays. As a standard protocol, NPS samples were collected by a healthcare worker using a sterile flocked swab placed in a sterile tube containing the viral transport medium (VTM) (Becton Dickinson, USA, cat no. 22053). The saliva samples were collected under the supervision of a healthcare worker in Omni tubes (Omni International, USA, SKU: 19-628D) without adding any media. All samples were stored at 4 °C temperature and transported to the SARS-CoV-2 testing facility at Augusta University, GA, within 24 h of sample collection, for further processing.
FDA-EUA approved assay for the detection of SARS-CoV-2 (SARS-specific assay)
The assay is based on nucleic acid extraction followed by TaqMan-based RT-PCR assay to conduct in vitro transcription of SARS-CoV-2 RNA, DNA amplification, and fluorescence detection (FDA-EUA assay by PerkinElmer Inc. Waltham, USA). The assay targets specific genomic regions of the SARS-CoV-2: nucleocapsid (N) gene and ORF1ab. The TaqMan probes for the two amplicons are labeled with FAM and ROX fluorescent dyes, respectively, to generate target-specific signals. The assay includes an RNA internal control (IC, bacteriophage MS2) to monitor the processes from nucleic acid extraction to fluorescence detection. The IC probe is labeled with VIC fluorescent dye to differentiate its fluorescent signal from SARS-CoV-2 targets. The samples were resulted as positive or negative based on the Ct values specified by the manufacturer (Supplementary file 1). For a detailed method, please refer to Sahajpal, NS, et al.6.
PKamp assay for the detection of SARS-CoV-2, influenza A and B viruses (Multiplex assay)
The PKamp Respiratory SARS-CoV-2 RT-PCR Panel assay (PerkinElmer Inc. Waltham, USA) is a real-time reverse transcription-polymerase chain reaction (RT -PCR) multiplexed test intended for the simultaneous qualitative detection and differentiation of SARS-CoV-2, influenza A, influenza B, and respiratory syncytial virus (RSV). The oligonucleotide primers and probes for the detection of SARS-CoV-2 include the virus nucleocapsid (N) gene and ORF1ab gene. The primers and probes for the detection of influenza A and RSV target regions of matrix protein. The primers and probes for the detection of influenza B target the regions of the nuclear export protein (NEP) and nonstructural protein 1 (NS1) genes. An additional primer/probe set to detect the endogenous control targets the RNase P gene and is included in the test. Qualitative assessment is based on fluorescence detections with TaqMan probes labeled as SARS-CoV-2 (FAM), influenza A (ROX), influenza B (Cy5), Respiratory syncytial virus (Cy5.5), and RNase P (HEX/VIC). The protocol for extraction and RT-PCR was described previously7. The samples were resulted as positive or negative based on the Ct values specified by the manufacturer (Supplementary file 1).
Limit of detection studies
The limit of detection (LoD) studies were conducted as per the FDA guidelines (https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/vitro-diagnostics-euas). Briefly, SARS-CoV-2 reference control material (SARS-CoV-2: SeraCare (Mat. No. 0505-0159; influenza A and B: SeraCare (Mat. No. 0515-0001) was spiked into the negative saliva and NPS samples to serve as positive samples at 540 copies/ml, 180 copies/ml, 60 copies/ml and 20 copies/ml concentrations. The lowest concentration detected in all three triplicates was determined as the preliminary LoD. To confirm the LoD, 20 replicates of preliminary LoD were analyzed and deemed as confirmed if at least 19/20 replicates were detected.
Data analysis
Data were analyzed for descriptive statistics and presented as a number (%) for categorical variables and mean ± standard deviation (SD) for continuous variables. Ct values were compared using Paired T-test.
Results
Clinical performance: saliva samples
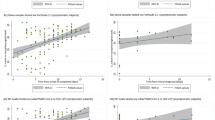
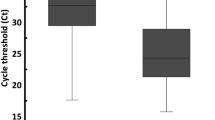
Of the 1019 saliva samples, 17.0% (174/1019) tested positive for SARS-CoV-2 using either assay. The detection rate for SARS-CoV-2 was higher with multiplex assay compared to SARS-specific assay [91.9% (160/174) vs. 87.9% (153/174)], respectively. The concordance for positive results between the two tests was 80.4% (140/174) (Table 1). The Ct values for SARS-CoV-2 were comparable between the two assays (SARS-CoV-2: 29.2 ± 7.2 vs. N: 29.8 ± 6.4, ORF1ab: 28.0 ± 7.1), whereas the Ct values of housekeeping gene was significantly lower with multiplex assay compared to SARS-specific assay [RNaseP: 20.6 ± 2.05 vs. IC: 32.5 ± 2.0 (p < 0.001)], respectively (Fig. 2). Further, the number of tests resulting as invalid was significantly less with the multiplex assay compared to the SARS-specific assay [1.7% (18/1019) vs. 5.6% (58/1019) (p < 0.001)]. No samples were positive for either influenza A or B.
Clinical performance: NPS samples
Of the 392 saliva samples, 10.4% (41/392) tested positive for SARS-CoV-2 using either assay. The detection rate for SARS-CoV-2 was higher with our multiplex assay compared to the SARS-specific assay [97.5% (40/41) vs. 95.1% (39/41)], respectively. The concordance for positive results between the two tests was 92.6% (38/41) (Table 2). The Ct values for SARS-CoV-2 were comparable between the two assays (SARS-CoV-2: 30.8 ± 8.8 vs. N: 31.3 ± 8.6, ORF1ab: 28.8 ± 8.6), whereas the Ct values of housekeeping gene was significantly lower with multiplex assay compared to SARS-specific assay [RNaseP: 23.1 ± 1.77 vs. IC: 31.3 ± 1.5 (p < 0.001)], respectively (Fig. 3). No samples were positive for either influenza A or B.
Limit of detection studies: saliva samples
In the preliminary LoD study using saliva samples, all replicates were detected at 60, 180, and 540 copies/ml for SARS-CoV-2 and the LoD was determined at 60 copies/ml, with 20/20 replicates being detected. The preliminary LoD evaluation for influenza A and B identified all replicates at the four concentrations for influenza B, whereas all replicates at 180 and 540 copies/ml were positive for influenza B. The LoD was established at 180 copies/ml for both influenza A, and B viruses, with 20/20 replicates being detected (Table 3).
Limit of detection studies: NPS samples
In the preliminary LoD study using NPS samples, all replicates at the four tested concentrations (20, 60, 180, and 540 copies/ml) were detected for SARS-CoV-2, and the LoD was determined at 60 copies/ml, with 20/20 replicates being detected. The preliminary LoD evaluation for influenza A and B identified all replicated at the four concentrations for influenza B, whereas all replicates at 180 and 540 copies/ml were detected for influenza B. The LoD was established at 180 copies/ml for both influenza A, and B viruses, with 20/20 replicates being detected (Table 4).
Discussion
This undocumented health loss due to seasonal influenza viruses has posed severe public health deficiencies, both at a clinical and epidemiological level8,9,10. Further, poorly documented co-infections in patients with COVID-19 continue to amplify the morbidity and mortality associated with the pandemic4,11. In an attempt to address these clinical and technical challenges, we propose a simplified protocol for the detection of SARS-CoV-2 along with common co-infections. We have optimized and validated a highly sensitive, RT-PCR based multiplex assay for detecting SARS-CoV-2, influenza A, and B viruses in a single test, using the same workflow, instruments, sample types, supplies, and laboratory personnel needed for the testing of SARS-CoV-2 virus (Fig. 1). The clinical evaluation of 1411 specimens that included 1019 saliva samples and 392 NPS samples demonstrated comparable performance of the multiplex assay to the SARS-specific FDA-EUA assay. Of the 1019 saliva samples evaluated with both assays, the detection rate was higher with the proposed multiplex assay compared to the SARS-specific assay (91.9% (160/174) vs. 87.9% (153/174). Ct values for SARS-CoV-2 with the multiplex assay were comparable to N and ORF1ab genes with the SARS-specific assay. The marginally higher performance of the multiplex assay compared to the SARS-specific assay might be attributed to the fact that in the multiplex assay, the amplification from two regions of the SARS-CoV-2 genome (N and ORF1ab genes) are detected with a single dye (FAM) for fluorescence detection. Thus, very weak positive samples that do not amplify sufficiently for the respective targets individually (N: FAM, ORF1ab: ROX) in the SARS-specific assay are being amplified to cross the threshold collectively in the multiplex assay [SARS-CoV-2 (N, ORF1ab): FAM). The concordance between the two assays was found to be 80.4% (140/174). Upon manual inspection of the Ct values, it was found that the discrepant results between the assays emerged for samples that show low viral loads with high Ct values, and only one gene detected (N or ORF1ab) with the SARS-specific assay. The findings were similar with NPS samples, with a slightly higher detection rate with multiplex assay compared to SARS-specific assay [97.5% (40/41) vs. 95.1% (39/41)], with a concordance of 92.6% (38/41) between the two assays. The Ct values for SARS-CoV-2 with the multiplex assay were comparable to N and ORF1ab gene with the SARS-specific assay. Further, the LoD studies performed with the SeraCare reference material demonstrated high sensitivity of the assay with LoD of 60 copies/ml for SARS-CoV-2 and 180 copies/ml for influenza A and B viruses, for both saliva and NPS samples. Notably, no samples resulted positive for influenza viruses A and B in this study. These results are in alignment with the prevalence of flu in this state, as reported by the Georgia Department of Public Health. The baseline levels were reported as 0–3%, with an incidence of 0.6% in the second week of December 2020 (https://dph.georgia.gov/epidemiology/influenza/flu-activity-georgia). Recently, in another single-center evaluation study, the LoD for SARS-CoV-2, influenza A and B were reported to be 5 copies/reaction, but the LoD was not validated as per FDA guidelines, and remains to be validated12.
We have previously discussed saliva samples that resulted as inconclusive and have argued that the rate of these invalid results would decrease with assays that include RNaseP gene as a housekeeping control7,13. Herein, the number of invalids significantly decreased with the multiplex assay compared to the SARS-specific assay [1.7% (18/1019) vs. 5.6% (58/1019): p < 0.001], and Ct values for the housekeeping gene was significantly lower (p < 0.001) with the multiplex assay compared to the SARS-specific assay. The RNase P gene is abundant in both the NPS and saliva samples, leading to a definitive result, whereas the addition of an external control (5 µl IC in SARS-specific assay) might be difficult to extract in complex samples contributing to inconclusive results. It is recommended that inconclusive samples be re-processed, and if the results still remain inconclusive, then patients need to be re-tested on a fresh sample. A major advantage of this multiplex assay has been that it did not cause any significant workflow changes in our laboratory. Existing platforms and even procedures remained essentially the same as those in use for the last eight months for COVID-19 testing. The only change was in the PCR master mix composition, which does not cause any change in workflow or TAT. The TAT with SARS-specific assay has been ~ 14 h for reporting ~ 800 samples/day, and the TAT to report results with the multiplex assay was found to be similar as assessed by an independent, blinded protocol.
However, the study is limited by the fact that none of our clinical samples were known positive for influenza A and B viruses. To address this limitation, we obtained the SeraCare reference material for influenza A and B viruses. We performed the LoD studies by spiking saliva and NPS samples to validate the assay for the detection of influenza viruses. The second limitation was that Respiratory Syncytial Virus (RSV) was not validated in this study as the RT-PCR instruments available in the laboratory do not have the channel on which the dye for RSV detection was labeled. The manufacturers have appropriately provided the procedure for RT-PCR master mix preparation, where, TE (Tris-EDTA) was added instead of RSV probes in the solution. The laboratories that have instruments that can detect RSV can easily include the detection of RSV in addition to SARS-CoV-2, influenza A, and B viruses. The third limitation was that it would have been ideal to sequence the non-concordant samples between the assays to resolve the discrepant results. However, due to exhaustion of the sample, additional experiments could not be performed. Nonetheless, despite these limitations, this study presents a significant and clinically validated assay that can be implemented for testing of SARS-CoV-2, influenza A and B viruses, using NPS and saliva samples for population screening.
References
Taipale, J., Romer, P., Linnarsson, S. Population-scale testing can suppress the spread of COVID-19. medRxiv. 2020.04.27.20078329 (2020).
Bedford, J. et al. COVID-19: Towards controlling of a pandemic. Lancet 395(10229), 1015–1018 (2020).
GBD 2017 Influenza Collaborators. Mortality, morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: An analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 7(1), 69–89 (2019).
Xing, Q. et al. Precautions are needed for COVID-19 patients with co-infection of common respiratory pathogens. MedRxiv https://doi.org/10.1101/2020.02.29.20027698 (2020).
Posteraro, B., Marchetti, S., Romano, L., Santangelo, R., Morandotti, G.A., Sanguinetti, M., Cattani, P. FPG COVID Laboratory Group. Clinical microbiology laboratory adaptation to COVID-19 emergency: experience at a large teaching hospital in Rome, Italy. Clin. Microbiol. Infect. 26(8), 1109–11 (2020).
Sahajpal, N. S. et al. Proposal of RT-PCR-based mass population screening for severe acute respiratory syndrome coronavirus 2 (coronavirus disease 2019). J Mol Diagn. 22(10), 1294–1299 (2020).
Sahajpal, N. S. et al. SalivaAll: Clinical validation of a sensitive test for saliva collected in healthcare and community settings with pooling utility for SARS-CoV-2 mass surveillance. J. Mol. Diagn. S1525–1578(21), 00114–00118 (2021).
Fischer, W. A., Bhagwanjee, S. & Sevransky, J. Global burden of influenza: Contributions from resource limited and low-income settings. Glob. Heart 9(3), 325 (2014).
Gordon, A. & Reingold, A. The burden of influenza: A complex problem. Curr. Epidemiol. Rep. 5(1), 1–9 (2018).
Bresee, J. et al. Progress and remaining gaps in estimating the global disease burden of influenza. Emerg. Infect. Dis. 24(7), 1173 (2018).
Lansbury, L., Lim, B., Baskaran, V. & Lim, W. S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 81(2), 266–275 (2020).
Shu, B. et al. Multiplex real-time reverse transcription PCR for influenza A virus, influenza B virus, and severe acute respiratory syndrome Coronavirus 2. Emerg. Infect. Dis. 27(7), 1821–1830 (2021).
Sahajpal, N. S. et al. SalivaSTAT: Direct-PCR and pooling of saliva samples collected in healthcare and community setting for SARS-CoV-2 mass surveillance. Diagnostics 11(5), 904 (2020).
Funding
This project has been funded by the National Institute of Allergy and Infectious Diseases, a component of the NIH, Department of Health and Human Services, under contract 75N93019C00052.
Author information
Authors and Affiliations
Contributions
Conceptualization, N.S.S., A.K.M., and R.K.; Data curation, N.S.S., A.K.M., S.A., K.J., P.A.; Formal analysis, N.S.S., A.K.M., A.N., E.A., and R.K.; Funding acquisition, R.K.; Investigation, N.S.S., A.K.M., A.N., S.A and R.K.; Methodology, N.S.S., A.K.M., and R.K.; Resources, R.K.; Software, N.S.S., A.K.M., A.N.; Supervision, R.K.; Validation, N.S.S. and A.K.M.; Visualization, N.S.S., A.K.M.; Writing—original draft, N.S.S.; Writing—review & editing: T.M.R., V.K., A.K., S.F., M.H., A.C., A.M.R., and R.K. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
RK has received honoraria, travel funding, and research support from Illumina, Asuragen, Perkin Elmer Inc., Bionano Genomics Inc, QIAGEN, and BMS. AK and MH are salaried employees of PerkinElmer Inc and MH hold stock options at PerkinElmer Inc. AC is salaried employee of Bionano Genomics Inc. All the other authors do not have any competing interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sahajpal, N.S., Mondal, A.K., Ananth, S. et al. Clinical validation of a multiplex PCR-based detection assay using saliva or nasopharyngeal samples for SARS-Cov-2, influenza A and B. Sci Rep 12, 3480 (2022). https://doi.org/10.1038/s41598-022-07152-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-07152-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.