Abstract
Psychological intimate partner violence (IPV), a global public health problem, affects mothers during pregnancy. We evaluated its relationship with preterm birth. We established a cohort of 779 consecutive mothers receiving antenatal care and giving birth in 15 public hospitals in Spain. Trained midwives collected IPV data using the Index of Spouse Abuse validated in the Spanish language. Preterm was defined as birth before 37 completed weeks of gestation. Gestational age was estimated by early ultrasound. With multivariate logistic regression we estimated the relative association of IPV with preterm birth as adjusted odds ratios (AOR), with 95% confidence intervals (CI). In propensity score analysis, using weighting by inverse probability of exposure to IPV, the whole sample was used for estimating the absolute difference in probability of preterm amongst offspring born to mothers with and without IPV. Socio-demographic and other pregnancy characteristics served as covariates in both analyses. Preterm occurred in 57 (7.3%) pregnancies. Psychological IPV, experienced by 151 (21%) mothers, was associated with preterm birth (11.9% vs 6.5%; AOR = 2.4; 95% CI = 1.1–5.0; p = 0.01). The absolute preterm difference in psychological IPV compared to normal was 0.08 (95% CI = 0.01–0.16; p = 0.04). The probability of preterm birth was 8% higher on average in women with psychological IPV during pregnancy. As our analysis controlled for selection bias, our findings give credence to a causal inference. Screening and management for psychological IPV during pregnancy is an important step in antenatal care to prevent preterm birth.
Similar content being viewed by others
Introduction
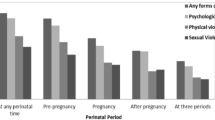
Violence against women including intimate partner violence (IPV) is one of the most pervasive human rights abuses worldwide. IPV refers to behaviour within an intimate relationship that causes physical, sexual or psychological harm, including acts of physical aggression, sexual coercion, psychological abuse and controlling behaviours. This definition covers violence by both current and former spouses and partners1,2. Globally, the lifetime prevalence of IPV against women perpetrated by a male partner is around 30%3. In Europe, 32% of women reported experiencing psychological IPV and 43% reported psychological IPV including other forms of violence as controlling behavior, economic violence and blackmail with children4.
The consequences of IPV are magnified when the victim of violence is pregnant because of additional health risks to both the woman and her unborn child1,5. During pregnancy most women are in contact with the health care system making antenatal care a window of opportunity for identifying IPV. Violence during pregnancy is higher than many common obstetric conditions6 differing across countries and cultural settings3,7,8,9. In a European wide-survey, women who were pregnant during the relationship with their partner and who experienced violence in the relationship, 20% of the victims of current partner violence and 42% of victims of previous partner violence say that physical or sexual violence also took place during pregnancy4. A recent Spanish study documented that psychological IPV in pregnancy was reported by 21.0% of the women by using validated screening tools10. The awarness of this problem is high in Spain as political agreement to reduce gender violence (2017) was obtained with unanimity among all the political parties and supported by consistent provision of an annual budget. The Spanish agreement emphasizes that doctors, midwives and other allied healthcare professionals must act as active screeners, and that this should happen within a system where early detection is followed by proper multidisciplinary input11.
A worldwide estimation of 12.9 million children are born before 37 gestational weeks, which implies that 9.6% of all children being born preterm12 with devastating effects on the child's health13. IPV during pregnancy might contribute to preterm birth through an association with obstetric complications, e.g. preeclampsia, gestational diabetes14,15,16,17,18,19. Physical IPV during pregnancy has been most linked to preterm birth20,21,22,23,24. In a recent meta-analysis study, the psychological IPV was assessed in only 2 of the 30 articles14. However, psychological violence is also an important form of IPV but inadequate standardization of its measurement might difficult to quantify the health effects of this type of violence16. The deficiency of valid and reliable evaluations of IPV16 with frequent studies aiming exclusively on physical IPV25 have the result that the matter of psychological IPV during pregnancy mainly unnoticed.
It is increasingly being recognised that psychological victimization during pregnancy contributes to poorer overall health and temperament of the child. Psychological IPV during pregnancy have been linked to psychological outcomes such as high levels of stress, anxiety, and posttraumatic stress disorder17,19. Women who are victims of psychological IPV during pregnancy have been found to have more severe family/social problems and higher rates of psychiatric problems and comorbidity9,15. Consequently, psychological IPV may be a risk factor for negative pregnancy health experiences and behaviors including substance use and inadequate weight gain and prenatal care utilization, suggesting pathways by which psychological IPV may impact pregnancy and birth outcomes15,17. Continuous and improved investigation has been requested, especially because the harmful effects of non-physical IPV are underestimated20,21,26,27.
Observational studies13,14,16,17,21 of the link between psychological IPV and preterm birth are vulnerable to selection bias, a situation where certain characteristics related to the likelihood of exposure, e.g. socioeconomic status, can lead to an inaccurate estimate of the association, making a causal inference impossible. A thorough search of the literature showed that propensity score analysis has not been used to evaluate the relationship, reducing the risk of bias in the estimation of the association.
Considering the public health importance of IPV and preterm birth as important risk factors for maternal and infant morbidity, we examined if the experience of psychological IPV, perpetrated by current or former male partners, and captured with validated tools in pregnancy may be associated with preterm birth in a propensity score analysis to allow for evaluation of a causal inference.
Methods
Population, sample size and study subjects
A population-based study was designed for all public hospitals (n = 28) in Andalusia, Spain (number of births = 76,336). A cluster sampling approach was adopted to select 15 hospitals to represent service type (regional, n = 5; specialized, n = 10; and district, n = 13). A sample of 750 women, consecutively enrolling 50 women per hospital8, provided an accuracy of ± 2.5% with 99% confidence for IPV detection, assuming an IPV prevalence of 7.5%16 and an intraclass correlation coefficient of 5%28. Participants were women who received routine antenatal care giving birth in the hospital. Exclusion criteria were women with miscarriages, inability to converse in the Spanish language, and the presence of cognitive disease preventing collection. The study protocol was approved by the research ethics committees of all participating hospitals (Research Ethics Committees of Healthcare Hospitals, Healthcare Counselling, Andalusian Healthcare Service, Andalusian Government, Spain. Protocol code: VIO-EMB-AP-2017) in accordance with the “Ethical Principles for Medical Research Involving Human Subjects” adopted in the Declaration of Helsinki by the World Medical Association (64thWMA General Assembly, Fortaleza, Brazil, October 2013). All participants provided written informed consent prior to enrolment.
Data collection procedures
Data were gathered during the immediate postpartum period by midwives at each hospital who were given specific training for participation in the study. Women were enrolled on successive days until the sample size per hospital was achieved (n = 50), preventing any day without sampling. Data were gathered in a room other than the ward in which the woman was hospitalized, where the study objective was explained, with guarantee that partner was not present. The strict anonymity and confidentiality of the information collected was guaranteed. Women participating signed informed consent. If the questionnaire responses evidenced IPV, the women were given comprehensive information on the police, judicial, and social resources available.
Data collection instruments
Preterm birth
Preterm was defined as birth before 37 completed weeks of gestation. Gestational age was estimated by early ultrasound.
IPV Exposure
IPV was defined as physical, sexual, coercion or psychological violence, and controlling behaviours perpetrated by a current or past male partner1,2 during 12 months before giving birth. It was identified in the immediate postpartum period using Index of Spouse Abuse (ISA), a 30-item self-report instrument measuring the severity and frequency of abuse by weighted items (Supplementary Method)29. ISA (ranging from 0 to 100 points) measured two different types of violence: an ISA-P score that represents the severity of physical violence and an ISA-NP score that represents the severity of nonphysical or psychological violence. The higher scores reflect more severe IPV. Recommended cut-off scores were 10 for physical violence and 25 for psychological violence as at these thresholds the sum of false positives and false negatives was minimized29. The instrument was validated for application in Spanish30.
Socio-demographic measures
Data collected were age, nationality, schooling history, employment, relationship status, number of children, cohabitation with partner/family, and the availability of next of kin support (i.e. a relative who could be turned to when needed). Relationship status was coded as “married”, “committed relationship” but not married and “non-committed relationship” considered between individuals who may have casual sex without demanding or expecting the commitment of a formal relationship10.
Pregnancy intendedness
The women were asked: “At the time you became pregnant, did you want to become pregnant then, did you want to wait until later, did you want no (more) children, or did you not mind either way?” A pregnancy was considered unintended if the respondent stated that at the time, she became pregnant she would have liked to have waited until later to become pregnant (mistimed pregnancy) or that she did not want any (more) children (unwanted pregnancy)31.
Perinatal outcomes
Data was extracted from the prospectively documented individual health records during the pregnancy. Outcomes collected were: anaemia (< 10.5 g/dL), vaginal bleeding (threatened abortion and antepartum haemorrhage), stillbirth, urinary tract infection, vaginal infections (bacterial vaginosis, sexually transmitted infection, candidiasis, etc.), gestational diabetes (confirmed by glucose tolerance test at 24–28 weeks), gestational hypertension (> 140/90 mmHg), spontaneous preterm labour, low birth weight, others (e.g. hyperemesis, placental disorders, mental disorders, hypothyroidism and intrauterine growth retardation) and smoking in pregnancy.
Statistical analysis
Multiple logistic regression analysis determined the relative association between IPV and preterm birth. The results were summarized as crude (COR) and adjusted odds ratios (AORs) with 95% confidence intervals (CIs). The absolute difference in probability of preterm amongst those with and without IPV was estimated using propensity score analysis32. Weighting by inverse probability of exposure to IPV was applied to the whole sample. The Average Treatment Effect (ATE) of psychological IPV vs no IPV on preterm birth was estimated for the entire sample. The covariates in both analyses (multiple regression analysis and propensity score analysis) were socio-demographic characteristics (age, relationship status, educational level, employment status, nationality, cohabitation, and kin support), desired pregnancy, number of children different from the actual birth, stillbirth, obstetric pathologies (any pathology during pregnancy except anemia or infections), infections during pregnancy and smoking in pregnancy. The covariates were selected based on previous results predicting IPV and on preterm birth theory8. The numbers of cases of physical IPV were too small for a reliable multivariate analysis.
Results
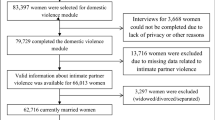
The flow diagram of participants in this dataset shown in Fig. 1. The response rate amongst those invited to take part was 92.2% and the data loss was 4.3%: 28 women who refused to participate in the study and 11 who refused to fill out the ISA questionnaire (the latter were included in the study). IPV in pregnancy was reported by 21.3% (n = 153) of the women, including physical and psychological IPV, with no duplication of cases. Physical IPV was reported by 26 (3.6%) and psychological by 151 (21.0%).
The maternal socio-demographic characteristics and outcomes are shown in Tables 1 and 2. Preterm was observed in 57 (7.3%) of newborns; 11.9% among women who reported psychological IPV versus 6.5% among those who did not (COR = 1.9; 95% CI = 1.1–3.5; p = 0.02). The odds of preterm birth were higher in women with obstetric complications (COR = 4.3; 95% CI = 2.4–7.5) and those with a previous stillbirth (COR = 2.0; 95% CI = 1.1–4.5). In the adjusted analysis, the relative association of exposure to psychological IPV, compared to normal, with preterm birth remained significant (AOR = 2.4; 95% CI = 1.1–5.0; p = 0.01) (Table 2). The absolute difference in the probability of preterm birth among pregnant women who suffered psychological IPV vs those without exposure was 0.08 (95% CI = 0.01–0.16; p = 0.04), using propensity score analysis (Table 2).
Discussion
In this study, psychological IPV, reported by 1 in 5 mothers, was associated with preterm birth. As the probability of preterm birth was 8% higher in women with psychological IPV, health care professionals should be alert about the risk to the offspring of women with psychological IPV exposure in pregnancy.
The strength of our investigation is based on the propensity score analysis that was used for the first time to draw causal inference between psychological IPV during pregnancy and preterm birth. The individual sampling weight contributes to the analysis using observed covariates in the whole sample32 to balance on average the measured socio-demographic and obstetric covariates among those with and without IPV. This reduced the risk of confounding in the relationship between the IPV exposure and preterm birth outcome. Even though this approach cannot control for unknown and unmeasured confounding it raises the possibility of a causal inference that metrics consideration. In future studies with larger samples, sensitivity analysis should be recommended to explore the bias due to unmeasured confounding variables. A key strength of our work is that it was a population-based study to identify psychological IPV during pregnancy with a validated tool (ISA) in the local language and midwives trained for data collection. Continuous ISA scores could be used in the logistic regression as an alternative approach in future research. The use of ultrasound scanning for gestational age determination was another strength of the study. This study presented data with a high response rate (> 90%). Despite the small figures, rejection to fill out the IPV instruments should always be considered methodological issues. Nevertheless, the low loss of ISA data (< 5%) should support the minimal influence on the validity of our results8. Further strength is that socio-demographic characteristics had no effect on preterm birth in the adjusted multivariate model. Perinatal outcomes, such as obstetric pathologies and a previous stillbirth were associated to preterm birth.
Although IPV has been also assessed in postpartum period27, that may be considered as one limitation of the study, since women tend to feel particularly vulnerable and may have induced an underreporting of the violence33. Another limitation is that the findings of this study may not generalize to non-Spanish populations, particularly to populations of pregnant women in countries with differing access to healthcare and/or quality of healthcare.
We found the prevalence of preterm 7.3% (< 37 weeks), the small numbers of extreme (< 28 weeks) and early (< 32 weeks) premature births did not allow us to draw any conclusion about preterm subgroups. Similar prevalence rates have been reported confirmed also by ultrasound scan21. However, maturity in a multi-country study, including 184 countries, showed that 11.1% of all deliveries were preterm13. The reported differences may reflect that pregnant women are exposed to different living conditions and also how accurately gestational age is determined34.
Women experiencing IPV during pregnancy were at increased risk for preterm birth 14,16,17,21,22,27 that is well established leading causes of neonatal morbidity and mortality13. However, it is important to note that several studies have not found a significant relationship between IPV and delivering preterm23,35,36. The lack of associations between IPV during pregnancy and preterm birth may be attributable to the small size of the sample studies. Similarly, generalizations are difficult to state among studies finding positive associations owing to different populations sampled, assessments, methods, and data analysis17.
The association between psychological IPV during pregnancy and preterm birth that we documented was adjusted for other known obstetric pathologies or a previous stillbirth. The causal inference, in addition to our inverse probability weighting analysis, is strengthened by several biological mechanisms. Psychological IPV during pregnancy may increase the risk of preterm birth through psychosocial or physical stress, depression, anxiety, isolation, decreased social support, and low self-esteem14,16,17,37. Indeed, psychological stress may induce pregnancy complications including such as preeclampsia or preterm labor or may aggravate preexisting conditions such as hypertension and gestational diabetes17,37. Psychosocial stress may also reflect in unhealthy behaviours during pregnancy such as smoking, or alcohol and drug consume, or may affect the adequate use of antenatal care services14,16,17,37,38. Regarding to the unhealthy behaviours, we found that smoking during pregnancy was not significantly associated to preterm birth. Besides, the stress of experiencing IPV during pregnancy may increase hypothalamic–pituitary–adrenal (HPA) activity. Higher levels of HPA hormones, including corticotrophin-releasing hormone (CRH), could initiate labor as well as restrict utero-placental perfusion16,17. Endothelial dysfunction and inflammatory cytokines all seem to be implicated in the pathogenesis of placental insufficiency, abruptio placentae and preterm birth16. Additional studies are needed to disentangle the independent and joint effect of IPV exposure and these risk factors on preterm risk.
Based on our findings, experiencing psychological IPV during pregnancy has a significant positive effect on premature birth. Thus, screening for non-physical IPV during pregnancy is an important step. There is a need for strengthening health care provision by involving other stakeholders who can support victims of psychological IPV by securing social and psychological support. Antenatal care represents an important opportunity to engage in preterm birth prevention through psychological IPV identification and management.
References
Garcia-Moreno, C., Jansen, H., Ellsberg, M., Heise, L. & Watts, C. WHO Multi-country study on women’s health and domestic violence against women (World Health Organization, 2005).
Stark, E. Coercive control: How men entrap women in personal life (Oxford University Press, 2007).
Garcia-Moreno, C. et al. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner violence (World Health Organization, 2013).
European Union Agency for Fundamental Rights (FRA). Violence against women: an EU-wide survey. Luxembourg: Publications Office of the European Union; 2015. [Available from: https://fra.europa.eu/en/publication/2014/violence-against-women-eu-wide-survey-main-results-report]
Jasinski, J. L. Pregnancy and domestic violence: a review of the literature. Trauma Violence Abuse. 5, 47–64 (2004).
Gazmararian, J. A. et al. Violence and reproductive health: current knowledge and future research directions. Matern Child Health J. 4, 79–84 (2000).
Gartland, D. et al. The case for early intervention to reduce the impact of intimate partner abuse on child outcomes: results of an Australian cohort of first-time mothers. Birth 41(4), 374–383 (2014).
Velasco, C., Luna, J. D., Martin, A., Caño, A. & Martin-de-las-Heras, S. Intimate partner violence against Spanish pregnant women: application of two screening instruments to assess prevalence and associated factors. Acta Obstet. Gynecol. Scand. 93, 1050–1058 (2014).
Tavoli, Z., Tavoli, A., Amirpour, R., Hosseini, R. & Montazeri, A. Quality of life in women who were exposed to domestic violence during pregnancy. BMC Pregnancy Childbirth. 16, 19 (2016).
Martin-de-Las-Heras, S., Velasco, C., Luna-Del-Castillo, J. D. & Khan, K. S. Breastfeeding avoidance following psychological intimate partner violence during pregnancy: a cohort study and multivariate analysis. BJOG 126, 778–783 (2019).
Martin-de-las-Heras, S. & Khan, K. Healthcare professionals should be actively involved in gender violence reduction: political consensus emerges in Spain. BJOG 125(1), 80 (2017).
Beck, S. et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull. World Health Organ. 88, 31–38 (2010).
Blencowe, H. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379, 2162–2172 (2012).
Donovan, B. M., Sprackelen, C. N., Schweizer, M. L., Ryckman, K. K. & Saftlas, A. F. Intimate partner violence during pregnancy and the risk for adverse infant outcomes: a systematic review and meta-analysis. BJOG 123, 1289–1299 (2016).
Martin-de-Las-Heras, S., Velasco, C., Luna-Del-Castillo, J. D. & Khan, K. S. Maternal outcomes associated to psychological and physical intimate partner violence during pregnancy: a cohort study and multivariate analysis. PLoS ONE 14, e0218255 (2019).
Hill, A., Pallitto, C., McCleary-Sills, J. & Garcia-Moreno, C. A systematic review and meta-analysis of intimate partner violence during pregnancy and selected birth outcomes. Int. J. Gynaecol. Obstet. 133(3), 269–276 (2016).
Alhusen, J. L., Ray, E., Sharps, P. & Bullock, L. Intimate partner violence during pregnancy: maternal and neonatal outcomes. J. Womens Health. 24(1), 100–106 (2015).
Chisholm, C. A., Bullock, L. & Ferguson, J. E. J. Intimate partner violence and pregnancy: screening and intervention. Am. J. Obstet. Gynecol. 217(2), 145–149 (2017).
Chisholm, C. A., Bullock, L. & Ferguson, J. E. J. Intimate partner violence and pregnancy: epidemiology and impact. Am. J. Obstet. Gynecol. 217(2), 141–144 (2017).
Abdollahi, F., Rezaie Abhari, F., Yazdani Charati, J. & Rouhani, S. Impact of psychological violence on pregnancy outcomes in a prospective study. Iran J. Psychiatry Behav. Sci. 8(3), 22–27 (2014).
Sigalla, G. N. et al. Intimate partner violence during pregnancy and its association with preterm birth and low birth weight in Tanzania: a prospective cohort study. PLoS ONE 12(2), e0172540 (2017).
Berhanie, E., Gebregziabher, D., Berihu, H., Gerezgiher, A. & Kidane, G. Intimate partner violence during pregnancy and adverse birth outcomes: a case-control study. Reprod. Health. 16, 22 (2019).
Abujilban, S., Mrayan, L., Al-Modallal, H. & Isaa, E. Effects of intimate partner physical violence on newborns’ birth outcomes among Jordanian birthing women. J. Interpers. Violence 32, 3822–3838 (2017).
Maciel, M. N. A., Blondel, B. & Saurel-Cubizolles, M. J. Physical violence during pregnancy in France: Frequency and impact on the health of expectant mothers and newborns. Matern. Child Health J. 23, 1108–1116 (2019).
Bell, H., Bush-Armendariz, N. B., Sanchez, E. & Tekippe, A. Pregnant and parenting battered women speak out about their relationships and challenges. J. Aggress. Maltreat. Trauma 17, 318–335 (2008).
Coker, A. L. et al. Physical and mental health effects of intimate partner violence for men and women. Am. J. Prev. Med. 23, 260–268 (2002).
Sanchez, S. E. et al. Risk of spontaneous preterm birth in relation to maternal exposure to intimate partner violence during pregnancy in Peru. Matern. Child Health J. 17, 485–492 (2013).
Eldridge, S. K. S. Practical guide to cluster randomized trials in health services research (Wiley, 2012).
Hudson, W. W. & Mcintosh, S. R. The assessment of spouse abuse: two quantifiable dimensions. J. Marriage Fam. 43(4), 873–885 (1981).
Observatorio de Salud de las Mujeres, Escuela Andaluza de Salud Pública. Adaptación española de un instrumento de diagnóstico y otro de cribado para detectar la violencia contra la mujer en la pareja desde el ámbito sanitario [Spanish adaptation of a diagnostic and a screening tool for detecting intimate partner violence violence against women in the health system] (in Spanish. No abstract available). Madrid, Spain: Ministerio de Sanidad y Consumo, 2006. Available online at: http://www.msc.es/organizacion/sns/planCalidadSNS/pdf/equidad/genero_vg_02.pdf. Accessed 13 July 2017.
Pallitto, C. C. et al. Intimate partner violence, abortion, and unintended pregnancy: results from the WHO multi-country study on women’s health and domestic violence. Int. J. Gynecol. Obstet. 120(1), 3–9 (2013).
Lee, J. & Little, T. D. A practical guide to propensity score analysis for applied clinical research. Behav. Res. Ther. 98, 76–90 (2017).
McFarlane, J., Campbell, J. C., Sharps, P. & Watson, K. Abuse during pregnancy and femicide: urgent implications for women’s health. Obstet. Gynecol. 100(1), 27–36 (2002).
Urquia, M. L., O’Campo, P. J., Heaman, M. I., Janssen, P. A. & Thiessen, K. R. Experiences of violence before and during pregnancy and adverse pregnancy outcomes: an analysis of the Canadian Maternity Experiences Survey. BMC Pregnancy Childbirth. 11, 42 (2011).
Janssen, P. A. et al. Intimate partner violence and adverse pregnancy outcomes: a population-based study. Am. J. Obstet. Gynecol. 188, 1341–1347 (2003).
Grimstad, H., Schei, B., Backe, B. & Jacobsen, G. Physical abuse and low birthweight: A case-control study. Br. J. Obstet. Gynaecol. 104, 1281–1287 (1997).
Bailey, B. A. Partner violence during pregnancy: prevalence, effects, screening, and management. J. Womens Health 2, 183–197 (2010).
Martin-de-las-Heras, S., Velasco, C., Caño, A., Luna-del-Castillo, J. D. & Khan, K. S. Poor antenatal care attendance is associated with intimate partner violence: multivariate analysis of a pregnancy cohort. Eur. J. Obstet. Gynecol. Reprod. Biol. 237, 204–208 (2019).
Acknowledgements
The authors are grateful to all of the midwives who participated in this study and to all of the women who shared their experiences.
Funding
This study was funded by the Ministry of the Economy and Competitiveness of Spain (National Project I + D + I: FEM2016-79049-R).
Author information
Authors and Affiliations
Contributions
S.M.H,. C.V. and A.C. conceived and designed the study. C.V., L.R. and AC extracted and prepared the data for the analysis. J.D.L. provided statistical analysis. S.M.H., K.K. and L.R. conducted the data analysis. S.M.H. and K.K. were responsible for the writing of the manuscript. All authors were involved in the drafting and revising of the article and approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martín-de-las-Heras, S., Khan, K.S., Velasco, C. et al. Propensity score analysis of psychological intimate partner violence and preterm birth. Sci Rep 12, 2942 (2022). https://doi.org/10.1038/s41598-022-06990-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-06990-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.