Abstract
The benefit of percutaneous coronary intervention (PCI) has been reported to be associated with functional stenosis severity defined by fractional flow reserve (FFR). This study aimed to investigate the predictive ability of preprocedural transthoracic Doppler echocardiography (TDE) for increased coronary flow. A total of 50 left anterior descending arteries (LAD) that underwent TDE examinations were analysed. Hyperaemic LAD diastolic peak velocity (hDPV) was used as a surrogate of volumetric coronary flow. The increase in coronary flow was evaluated by the metric of % hDPV-increase defined by 100× (post-PCI hDPV-pre-PCI hDPV)/pre-PCI hDPV. The two groups divided by the median value of % hDPV-increase were compared, and the determinants of a significant coronary flow increase defined as more than the median % hDPV-increase were explored. After PCI, FFR values improved in all cases. hDPV significantly increased from 53.0 to 76.0 mm/s (P < 0.01) and the median % hDPV-increase was 45%, while hDPV decreased in 10 patients. On multivariable analysis, pre-PCI FFR and hDPV were independent predictors of a significant coronary flow increase. Preprocedural TDE-derived hDPV provided significant improvement of identification of lesions that benefit from revascularisation with respect to significant coronary flow increase.
Similar content being viewed by others
Introduction
Fractional flow reserve (FFR) can be used as an invasive marker to identify epicardial lesions that may benefit from revascularisation. FFR has shown prognostic efficacy and a continuous and independent relationship with subsequent outcomes1,2. An increase in coronary flow to the ischaemic region is the most fundamental reason for revascularisation because the severity and extent of stress-induced myocardial ischaemia have been proposed to be the most important contributing factors of a better prognosis3,4. These findings suggest that the benefit of percutaneous coronary intervention (PCI) may be greater in patients with lesions showing lower FFR values5, wherein a greater increase in coronary flow might be expected. PCI that provides no benefit with respect to coronary flow increase is a questionable indication and may even harm patients by exposing them to procedure- and stent-related risks, including the high bleeding risk of dual antiplatelet therapy. However, limited data are available regarding the relationship between physiological indices, such as FFR, coronary flow reserve (CFR), the index of microcirculatory resistance (IMR), hyperaemic peak coronary flow velocity, and changes in volumetric coronary blood flow after PCI. Furthermore, there are currently no preprocedural non-invasive markers that show predictive efficacy for a significant coronary flow increase after PCI.
Stress transthoracic Doppler echocardiography (S-TDE) is a cost-effective modality that provides diagnostic and prognostic information on coronary flow velocity and coronary flow velocity reserve (CFVR) without the need for ionising radiation, radioactive tracers, gadolinium, or intravascular catheterisation6. The CFVR value obtained by S-TDE represents useful quantitative information on the functional status of coronary artery circulation7,8. However, few S-TDE studies have documented changes in hyperaemic diastolic peak velocity (hDPV) after elective PCI. Vasodilator S-TDE, when performed after PCI, is likely to overcome most of the limitations of the wire-based, invasive, approach for measuring intracoronary pressure, such as under- or over-estimation of CFR and FFR because of reactive resting hyperaemia and microvascular injury7,9,10. Therefore, the three-fold aim of the present study, using hDPV as a surrogate of volumetric coronary flow, was to (1) investigate the early changes in S-TDE-derived indices, such as hDPV and CFVR, in the left anterior descending coronary artery (LAD) after successful and uncomplicated PCI; (2) explore the determinants of the changes in LAD hDPV; and (3) assess whether preprocedural S-TDE-derived physiological indices can predict increased coronary flow after PCI, independent of FFR.
Materials and methods
Study design and patient population
This study prospectively included 57 patients with stable coronary artery disease who were scheduled to undergo elective PCI of de novo, single, functionally significant LAD lesions at a single tertiary-care centre between June 10, 2020 and September 30, 2020. All patients had anginal symptoms (Canadian Cardiovascular Society class 1–3) and de novo, functionally significant, proximal LAD lesions (FFR ≤ 0.80). Patients with acute coronary syndrome or angiographically visible collateral flow were excluded. Other exclusion criteria were the inability to provide consent, history of myocardial infarction in the LAD territory, coronary intervention or coronary artery bypass graft surgery, occluded target vessels, left main coronary artery disease, reduced systolic function (ejection fraction < 50%), chronic renal disease, congestive heart failure, atrial fibrillation, and contraindications to adenosine administration. Optimal medical therapy with high-dose statins, dual antiplatelets, and antihypertensives was initiated immediately after diagnostic catheterisation in all patients. According to the study protocol, no ad hoc PCI was performed in this study.
The present study was approved by an institutional ethics committee (reference #955/Tsuchiura Kyodo General Hospital; 9 June, 2020) and was conducted in compliance with the tenets of the Declaration of Helsinki for human studies. All patients provided written informed consent for the study and future data utilisation.
Invasive coronary angiography
Each patient initially underwent standard diagnostic coronary angiography via the radial artery using a 6F system to assess the coronary anatomy and the severity of functional stenosis. Quantitative coronary angiography (QCA) analyses were performed using a CMS-MEDIS system (Medis Medical Imaging Systems, Leiden, Netherlands). All patients received a bolus injection of heparin (5000 IU) before the procedure. Intracoronary bolus injections of nitroglycerin (0.2 mg) were administered at the start of the procedure and before functional measurements.
Physiological measurements
Physiological measurements were performed in the LAD using a Radi Analyzer Xpress instrument with a single 0.014-inch PressureWire™ (Abbott Vascular, St. Paul, MN, USA). The FFR, mean transit time, CFR, and IMR were determined using a RadiAnalyzer Xpress instrument with a pressure–temperature sensor-chipped wire (Abbott Vascular), as per previously described methods. The FFR value was calculated as the ratio of the mean distal coronary pressure to the mean aortic pressure during stable hyperaemia, which was induced by the intravenous administration of adenosine (140 μg/kg/min through a central vein). After calibration, the wire was advanced, and the intracoronary pressure distal to the coronary stenosis was measured. After FFR measurement, when the pressure sensor reached the tip of the guiding catheter during hyperaemia via a pull-back manoeuvre, a mean Pd–Pa pressure drift of ≤ 2 mmHg was confirmed and documented. The institutional standard protocol mandated repeat assessment if the pressure drift was > 2 mmHg. All patients were instructed to strictly refrain from ingesting caffeinated beverages for > 24 h before catheterisation. CFR was calculated as resting mean transit time (Tmn) divided by hyperemic Tmn using a thermodilution technique11. Maximal hyperemia was induced by a continuous infusion at a rate of 140 μg/kg per min until a steady state hyperemia.
Percutaneous coronary intervention
PCI was performed according to the latest guidelines12. All patients underwent coronary stent implantation (2nd or 3rd generation drug-eluting stent) with pre-dilatation. The type of stent was selected at the operator’s discretion, and the strategy was determined by the interventionist. To avoid aggressive stent expansion, online QCA was performed to determine the proper stent size. Successful and uncomplicated PCI was defined as residual stenosis of < 20%, Thrombolysis in Myocardial Infarction flow grade of 3, no side branch occlusion or distal embolisation, and no PCI-related myocardial infarction according to the fourth universal definition of myocardial infarction13.
Measurement of coronary flow velocity
Eligible patients underwent pre- (1 day before) and post-procedural (3 days after) LAD coronary flow assessments by S-TDE. Echocardiographic studies were performed according to the American Society of Echocardiography guidelines14 using a commercially available digital ultrasound system (GE Vivid E95; GE Vingmed Ultrasound, Horten, Norway) with a multifrequency transducer and second-harmonic technology. After the standard examination, coronary flow in the mid-distal portion of the LAD was visualised in a modified three-chamber view. For colour flow mapping, the velocity range was set as 16–24 cm/s. A sample volume (3–5 mm wide) was selected at the distal LAD to measure blood flow velocity. The peak diastolic coronary flow velocity was measured at basal conditions (bDPV) and during maximal hyperaemia (hDPV), which was induced by intravenous adenosine (140 μg/kg per min through a central vein). All data were digitally stored for offline review and measurements. Three optimal flow signal profiles at rest and during hyperaemia were obtained offline from the recorded data. The CFVR was calculated as the ratio of the hyperaemic peak diastolic flow velocity to the basal peak diastolic flow velocity6 using the software package of the ultrasound system. Coronary flow increase was evaluated by the metric of % hDPV-increase, defined as (post-PCI hDPV-pre-PCI hDPV)/pre-PCI hDPV × 100. Two groups categorised by the median value of % hDPV-increase were compared (significant increase group and non-significant increase group), and the determinants of a significant coronary flow increase, defined as an increase greater than the median % hDPV-increase, were investigated. The mean diastolic coronary flow velocity and velocity–time integral were measured at basal conditions (bDMV and bVTI, respectively) and during maximal hyperaemia (hDMV and hVTI, respectively). Both hDPV and hDMV showed significant predictive values in the univariate analysis. The AUCs of ROC analyses of hDPV and hDMV were 0.761 [95% CI 0.628–0.894] and 0.736 [95% CI 0.598–0.874], respectively (Supplemental Fig. S1). There were no significant differences in AUCs of ROC curves for these two different velocity measurements to predict significant coronary flow increase. Thus, hDPV, which showed a numerically larger AUC, was used for further analyses. Two experts who were blinded to the clinical data separately analysed all stored data at a 1-week interval and performed the analyses twice to evaluate the reproducibility of the S-TDE-derived data. Figure 1 shows a representative case of coronary flow velocity recording and measurement before and after LAD PCI.
Representative images of coronary flow velocity measurements by transthoracic Doppler echocardiography. A representative case of a LAD lesion that underwent TDE examinations before and after successful PCI. (A) Pre-PCI hDPV, (B) post-PCI hDPV. LAD left anterior descending artery, TDE transthoracic Doppler echocardiography, PCI percutaneous coronary flow intervention, hDPV hyperaemic diastolic peak velocity.
Statistical analysis
Statistical analyses were performed using R version 3.5.3. Categorical data are expressed as numbers and percentages and were compared using the chi-square or Fisher’s exact tests, as appropriate. The normality of the distributed values was assessed using Shapiro–Wilk statistics. Continuous variables are expressed as medians (25th–75th percentile) since all of the variables showed non-normal distributions and were compared using the Mann–Whitney U test. Associations were evaluated by analysing Spearman’s correlation for non-normally distributed data. Univariable linear regression analysis was performed to identify significant predictors of % hDPV-increase after PCI. Also, univariable logistic regression analyses were performed to predict a significant coronary flow increase. The associated variables with a P-value < 0.05 in the univariate analyses were entered in the multivariable model, and a forward stepwise regression method was used to fit the multivariable model. The Akaike information criterion was applied to test the model fitness to avoid over-fitting. Receiver operating characteristic (ROC) curve analysis was performed to assess the best cut-off values of pre-PCI FFR and pre-PCI hDPV to predict a significant coronary flow increase after PCI. The optimal cut-off value was calculated using the Youden index. A prediction model for significant coronary flow increase was constructed to determine the incremental discriminatory and reclassification performance of pre-PCI hDPV when it was added to the model including pre-PCI FFR; this involved the use of relative integrated discrimination improvement (IDI) and the category-free net reclassification index (NRI). A level of P < 0.05 was considered significant.
Results
Baseline patient characteristics and physiological findings
Of the 57 initially enrolled patients who underwent PCI for LAD lesions and S-TDE before and after PCI, five patients were excluded due to insufficient TDE data acquisition. Furthermore, one patient was excluded because they showed a type 4A myocardial infarction, and another patient withdrew their consent before completing the postprocedural S-TDE. Thus, the final analysis included 50 patients who underwent successful PCI and had complete TDE flow data.
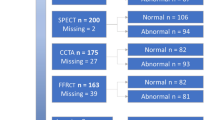
Table 1 summarises the baseline characteristics and angiographic and physiological data of 50 patients in the two groups divided by the median value of % hDPV-increase after PCI. The median % hDPV-increase was 45%. The FFR and pre-PCI hDPV were significantly lower in the significant coronary flow increase group (FFR: 0.65 vs 0.73, P = 0.005; pre-PCI hDPV: 46.0 vs 67.0 cm/s, P = 0.001). After successful PCI, hDPV significantly increased from 53.0 (39.8–69.8) cm/s to 76.0 (55.8–96.3) cm/s; however, 10 patients (20.0%) showed decreased hDPV despite of an increase in FFR (Fig. 2).
Serial changes in hDPV after PCI. hDPV significantly increased from 53.0 to 76.0 mm/s (P < 0.01), while hDPV decreased in 10 patients (20.0%). Red lines indicate cases with increased hDPV after PCI, and blue lines indicate cases with decreased hDPV after PCI. Abbreviations as in Fig. 1.
Predictors of a significant coronary flow increase and determinants of a change in hDPV after PCI
Predictors of a significant coronary flow increase were assessed using univariate and multivariate logistic regression analyses (Table 2). The pre-PCI FFR and pre-PCI hDPV were independently associated with a significant coronary flow increase. The results of univariable and multivariable linear regression analyses for predicting % hDPV-increase after PCI are shown in Table 3. Pre-PCI FFR and pre-PCI hDPV were independently and significantly associated with a % hDPV-increase after PCI. ROC analyses revealed the best cut-off values of pre-PCI FFR and pre-PCI hDPV for a significant coronary flow increase as follows: FFR = 0.68 (AUC: 0.729, 95% confidence interval [CI] 0.558–0.870) and hDPV = 52.0 cm/s (AUC, 0.761; 95% CI 0.628–0.894) (Fig. 3A,B). Table 4 shows that adding pre-PCI hDPV to the FFR model can increase predictability for a significant coronary flow increase (NRI: 0.560, 95% CI 0.044–1.075, P = 0.033 and IDI: 0.119, 95% CI 0.028–0.210, P = 0.009).
ROC analyses to determine the optimal cut-off values to predict a significant coronary flow increase. (A) ROC analysis of pre-PCI FFR to predict a significant coronary flow increase. (B) ROC analysis of pre-PCI hDPV to predict a significant coronary flow increase. FFR fractional flow reserve, ROC receiver operating characteristic; other abbreviations as in Fig. 1.
When patients were divided into four groups based on the best cut-off values of FFR and pre-PCI hDPV (0.68 and 52.0 cm/s, respectively), the degree of % hDPV-increase and the prevalence of a significant coronary flow increase were significantly different between these four groups (Fig. 4A,B).
The degree of % hDPV-increase and the prevalence of a significant coronary flow increase in four groups stratified by the best cut-off values of pre-PCI FFR and pre-PCI hDPV (pre-PCI FFR = 0.68 and pre-PCI hDPV = 52.0 cm/s). (A) The degree of % hDPV-increase was significantly different between the four groups. (B) The prevalence of a significant coronary flow increase was significantly different between the four groups. Abbreviations as in Figs. 1 and 3.
S-TDE measurement reproducibility
The inter- and intra-observer agreements for the identification of impaired CFVR (≤ 2.0) were 93% and 96%, respectively. The mean difference in CFVR values between the two observers was 6.8%.
Discussion
The current study investigated the predictive ability of preprocedural TDE for increased coronary flow after elective PCI. The essential findings were as follows: (1) PCI increased hyperaemic coronary flow, documented by S-TDE-derived hDPV, in 80% of the study patients, while FFR improvement was observed in all patients; (2) the median coronary flow velocity increase was 45%; (3) pre-PCI FFR, pre-PCI CFR, QCA reference diameter, and pre-PCI hDPV were associated with a significant coronary flow increase; and (4) pre-PCI hDPV predicted a significant coronary flow increase independent of the pre-PCI FFR value. To the best of our knowledge, the present study is the first to demonstrate that non-invasive S-TDE examination can predict a significant coronary flow increase after PCI for functionally significant LAD lesions.
Rationale of revascularisation
The aim of revascularisation by PCI is to increase coronary blood flow in an ischaemic region by modifying the epicardial lesion. A previous study using positron emission tomography (PET) showed a significant increase in regional stress myocardial blood flow (MBF) and myocardial flow reserve in the region with revascularisation15. However, limited data are available on the prediction of increased coronary flow after PCI or even on the relationship between baseline patient data, including those of functional lesion assessment, and coronary flow increase.
The FFR has rapidly gained consensus as the gold standard for representing induced regional ischaemia due to epicardial coronary artery stenosis for revascularisation decision-making in patients with stable coronary artery disease. The FFR has also been demonstrated to show a continuous and independent relationship with subsequent outcomes in patients with stable coronary artery disease (CAD)2. Based on these studies, a physiological rationale is increasingly required before decision-making for revascularisation in patients with chronic coronary syndrome. In addition, considering that the existence, extent, and severity of induced myocardial ischaemia have been proposed to be the most important contributing factors for a better prognosis3,4, coronary intervention without a corresponding increase in coronary flow or a reduction in ischaemia would not be expected to improve patient outcomes. Indeed, this could even be harmful due to the exposure of patients to procedure-related, stent-related, and high bleeding risks owing to dual antiplatelet therapy or a combination of anticoagulation therapies. Therefore, reliable and widely available methods are necessary to identify or predict a significant coronary flow increase after PCI, preferably by non-invasive pre-PCI testing.
Determinants of coronary flow increase after PCI
Recently, Driessen et al. and Knaapen et al. reported that successful coronary revascularisation has a significant and positive impact on absolute myocardial perfusion as assessed by serial PET. Notably, the improvement in the FFR after PCI was directly related to the increase in hyperaemic MBF16. Kanaji et al., using cardiac magnetic resonance imaging, showed that FFR-guided PCI was associated with increased absolute hyperaemic coronary sinus flow and that increased flow was associated with pre-PCI FFR values5. In the present study, we demonstrated that using S-TDE, pre-PCI S-TDE-derived hDPV had a powerful ability for predicting coronary flow increase by multiple linear regression analysis independent of pre-PCI FFR values. Furthermore, we defined a significant coronary flow increase after PCI as an increase greater than the median improvement in hDPV (45%); this value was in line with that reported in a previous PET study, which showed an average increase of 46% in absolute coronary flow after PCI17. A significant coronary flow increaser could also be predicted independent of pre-PCI FFR values by multivariate analysis.
Potential clinical implication of pre-PCI S-TDE examination
Our results indicated that the pre-PCI FFR is one of the most important determinants of increased coronary flow. However, ROC analysis showed that the best cut-off value of pre-PCI FFR for predicting a significant coronary flow increase was 0.68. This finding supports that of the prior study by Nijjer et al.18, in which the pre-PCI FFR predicted an increase in coronary flow velocity after PCI; the greatest increments in hyperaemic flow velocity were seen in territories where the pre-PCI FFR was ≤ 0.70. The present study strongly suggests that in addition to pre-PCI FFR values obtained invasively at the catheterisation laboratory, the non-invasive pre-PCI S-TDE-derived metric of hDPV could yield incremental predictive information for coronary flow increase after PCI. These findings support our decision-making regarding revascularisation, although further investigations are required.
Limitations
This study has several limitations, which should be considered when interpreting the results. First, the present study evaluated only 50 patients for the final analysis and carried the inherent limitations due to its small sample size, single-centre study, and observational nature; therefore, precluded extensive subgroups analyses and a selection bias can not be canceled. Second, in the Doppler echocardiographic examination of LAD coronary flow, pre- and post-PCI LAD flow data were comparable only at identical measurement positions and constant vessel diameters under similar haemodynamics. These issues were carefully addressed by ensuring the exact positioning of the echo probe, performing functional assessments, and maintaining the specified time frame for examination (around 10 am). Nevertheless, we cannot exclude the possibility of a change in the diameter of the LAD after non-LAD PCI or a difference in the functional measurement position. Third, the absolute coronary flow volume was not assessed in this study. The limited coronary flow volume in the ischaemic region depends on the downstream myocardial mass subtended by the lesion, and the impact of PCI on the coronary flow of the LAD might be affected by restoration of coronary flow volume following revascularisation. However, the main strength of the present study was the paired comparison performed for serial TDE examinations of the proximal LAD lesions for each patient, which might at least partially alleviate this limitation. Fourth, coronary flow may serially change after PCI, and our results are based on one time window of 3 days after the procedure. Further studies are needed to serially quantify the changes in coronary flow if the S-TDE data obtained in the present study are shown to be able to predict flow characteristics at a later follow-up date. Fifth, no prognostic data was provided in the present study. Sixth, the post-PCI TDE measurement was performed at more than 24 h after PCI, which may have influenced on the results. Subsequent mid- and long-term changes in coronary flow should be further studied. Seventh, approximately 10% of patients were not adequately evaluated by echocardiography, which might have resulted in a certain bias for the results. Finally and most importantly, future studies should test whether changes in coronary flow in ischaemic regions after PCI could provide prognostic information.
Conclusions
The noninvasively obtained pre-PCI S-TDE-derived hDPV could yield incremental predictive information over pre-PCI FFR values for a significant increase in coronary flow after PCI, which might support our decision to perform revascularisation.
References
Gotberg, M. et al. Instantaneous wave-free ratio versus fractional flow reserve to guide PCI. N. Engl. J. Med. 376, 1813–1823. https://doi.org/10.1056/NEJMoa1616540 (2017).
Johnson, N. P. et al. Prognostic value of fractional flow reserve: Linking physiologic severity to clinical outcomes. J. Am. Coll. Cardiol. 64, 1641–1654. https://doi.org/10.1016/j.jacc.2014.07.973 (2014).
Hachamovitch, R., Hayes, S. W., Friedman, J. D., Cohen, I. & Berman, D. S. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 107, 2900–2907. https://doi.org/10.1161/01.CIR.0000072790.23090.41 (2003).
Pijls, N. H. et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (fractional flow reserve versus angiography for multivessel evaluation) study. J. Am. Coll. Cardiol. 56, 177–184. https://doi.org/10.1016/j.jacc.2010.04.012 (2010).
Kanaji, Y. et al. Impact of elective percutaneous coronary intervention on global absolute coronary flow and flow reserve evaluated by phase-contrast cine-magnetic resonance imaging in relation to regional invasive physiological indices. Circ. Cardiovasc. Interv. 11, e006676. https://doi.org/10.1161/CIRCINTERVENTIONS.118.006676 (2018).
Ciampi, Q. et al. Functional, anatomical, and prognostic correlates of coronary flow velocity reserve during stress echocardiography. J. Am. Coll. Cardiol. 74, 2278–2291. https://doi.org/10.1016/j.jacc.2019.08.1046 (2019).
Uren, N. G. et al. Reduced coronary vasodilator function in infarcted and normal myocardium after myocardial infarction. N. Engl. J. Med. 331, 222–227. https://doi.org/10.1056/NEJM199407283310402 (1994).
Tesic, M. et al. Prognostic value of transthoracic doppler echocardiography coronary flow velocity reserve in patients with nonculprit stenosis of intermediate severity early after primary percutaneous coronary intervention. J. Am. Soc. Echocardiogr. 31, 880–887. https://doi.org/10.1016/j.echo.2018.02.011 (2018).
Kern, M. J. et al. Abnormal coronary flow velocity reserve after coronary artery stenting in patients: Role of relative coronary reserve to assess potential mechanisms. Circulation 100, 2491–2498. https://doi.org/10.1161/01.cir.100.25.2491 (1999).
van de Hoef, T. P. et al. Impact of coronary microvascular function on long-term cardiac mortality in patients with acute ST-segment-elevation myocardial infarction. Circ. Cardiovasc. Interv. 6, 207–215. https://doi.org/10.1161/CIRCINTERVENTIONS.112.000168 (2013).
Fearon, W. F. et al. Novel index for invasively assessing the coronary microcirculation. Circulation 107, 3129–3132. https://doi.org/10.1161/01.CIR.0000080700.98607.D1 (2003).
Levine, G. N. et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J. Am. Coll. Cardiol. 58, e44–e122. https://doi.org/10.1016/j.jacc.2011.08.007 (2011).
Thygesen, K. et al. Fourth universal definition of myocardial infarction (2018). J. Am. Coll. Cardiol. 72, 2231–2264. https://doi.org/10.1016/j.jacc.2018.08.1038 (2018).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 28, 1-39.e14. https://doi.org/10.1016/j.echo.2014.10.003 (2015).
Aikawa, T. et al. Improved regional myocardial blood flow and flow reserve after coronary revascularization as assessed by serial 15O-water positron emission tomography/computed tomography. Eur. Heart J. Cardiovasc. Imaging 21, 36–46. https://doi.org/10.1093/ehjci/jez220 (2020).
Driessen, R. S. et al. Impact of revascularization on absolute myocardial blood flow as assessed by serial [(15)O]H2O positron emission tomography imaging: A comparison with fractional flow reserve. Circ. Cardiovasc. Imaging 11, e007417. https://doi.org/10.1161/CIRCIMAGING.117.007417 (2018).
Johnson, N. P. & Gould, K. L. Physiological basis for angina and ST-segment change PET-verified thresholds of quantitative stress myocardial perfusion and coronary flow reserve. JACC Cardiovasc. Imaging 4, 990–998. https://doi.org/10.1016/j.jcmg.2011.06.015 (2011).
Nijjer, S. S. et al. Change in coronary blood flow after percutaneous coronary intervention in relation to baseline lesion physiology: Results of the JUSTIFY-PCI study. Circ. Cardiovasc. Interv. 8, e001715. https://doi.org/10.1161/CIRCINTERVENTIONS.114.001715 (2015).
Author information
Authors and Affiliations
Contributions
Contributions of authors: M.Y., conception, design, analysis of data, and drafting the manuscript; M.H., design and critical revision of the manuscript; T.S., data collection and critical revision of the manuscript; Y.K., data collection and critical revision of the manuscript; K.N., data collection and critical revision of the manuscript; T.N., data collection and critical revision of the manuscript; T.M., data collection and critical revision of the manuscript; M.H., data collection and critical revision of the manuscript; R.H., data collection and critical revision of the manuscript; M.A., data collection and critical revision of the manuscript; E.U., data collection and critical revision of the manuscript; T.M., data collection and critical revision of the manuscript; T.L., data collection and critical revision of the manuscript; T.Y., data collection and critical revision of the manuscript; T.S., data collection and critical revision of the manuscript; T.K., analysis of data, critical revision of the manuscript, and final approval of submission. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yamaguchi, M., Hoshino, M., Sugiyama, T. et al. Preprocedural transthoracic Doppler echocardiography to identify stenosis associated with increased coronary flow after revascularisation. Sci Rep 12, 1667 (2022). https://doi.org/10.1038/s41598-022-05683-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-05683-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.