Abstract
Subjects with comorbidities are at risk for neurodegeneration. There is a lack of a direct relationship between comorbidities and neurodegeneration. In this study, immunomagnetic reduction (IMR) assays were utilized to assay plasma Aβ1–42 and total tau protein (T-Tau) levels in poststroke (PS, n = 27), family history of Alzheimer’s disease (ADFH, n = 35), diabetes (n = 21), end-stage renal disease (ESRD, n = 41), obstructive sleep apnea (OSA, n = 20), Alzheimer’s disease (AD, n = 65). Thirty-seven healthy controls (HCs) were enrolled. The measured concentrations of plasma Aβ1–42 were 14.26 ± 1.42, 15.43 ± 1.76, 15.52 ± 1.60, 16.15 ± 1.05, 16.52 ± 0.59, 15.97 ± 0.54 and 20.06 ± 3.09 pg/mL in HC, PS, ADFH, diabetes, ESRD, OSA and AD groups, respectively. The corresponding concentrations of plasma T-Tau were 15.13 ± 3.62, 19.29 ± 8.01, 17.93 ± 6.26, 19.74 ± 2.92, 21.54 ± 2.72, 20.17 ± 2.77 and 41.24 ± 14.64 pg/mL. The plasma levels of Aβ1–42 and T-Tau in were significantly higher in the PS, ADFH, diabetes, ESRD and OSA groups than controls (Aβ1–42 in PS: 15.43 ± 1.76 pg/mL vs. 14.26 ± 1.42 pg/mL, p < 0.005; T-Tau in PS: 19.29 ± 8.01 vs. 15.13 ± 3.62 pg/mL, p < 0.005, Aβ1–42 in ADFH: 15.52 ± 1.60 pg/mL vs. 14.26 ± 1.42 pg/mL, p < 0.001; T-Tau in ADFH: 17.93 ± 6.26 vs. 15.13 ± 3.62 pg/mL, p < 0.005, Aβ1–42 in diabetes: 16.15 ± 1.05 pg/mL vs. 14.26 ± 1.42 pg/mL, p < 0.001; T-Tau in diabetes: 19.74 ± 2.92 vs. 15.13 ± 3.62 pg/mL, p < 0.001, Aβ1–42 in ESRD: 16.52 ± 0.59 pg/mL vs. 14.26 ± 1.42 pg/mL, p < 0.001; T-Tau in ESRD: 21.54 ± 2.72 vs. 15.13 ± 3.62 pg/mL, p < 0.001, Aβ1–42 in OSA: 15.97 ± 0.54 pg/mL vs. 14.26 ± 1.42 pg/mL, p < 0.001; T-Tau in OSA: 20.17 ± 2.77 vs. 15.13 ± 3.62 pg/mL, p < 0.001). This evidence indicates the high risk for dementia in these groups from the perspective of plasma biomarkers.
Similar content being viewed by others
Introduction
In 2020, the global prevalence of dementia was approximately 8%, i.e., 30 million patients1. Alzheimer’s disease (AD) is the most common dementia. With the aging of society, the number of dementia patients is expected to be more than 100 million in 20502,3,4. Management and health care for dementia are definitely a large economic burden at present. This burden will become more serious in the future if there is no action taken to cure or prevent dementia. Unfortunately, no curative treatment is currently available for dementia. Several pharmaceutical companies continue to develop new drugs for the treatment of dementia. On the other hand, prevention efforts for dementia attract the attention of medical doctors or researchers. Exciting results have been reported to demonstrate the feasibility of delaying the onset of dementia using aerobic exercise, nutrition adjustments, or sleeping quality improvement5,6,7,8. The delay could effectively reduce the population of dementia in the future.
People with risk factors are strongly suggested to take such preventive actions when they are still cognitively normal. These people are referred to as high risk for dementia (HRD). Most of these risk factors are similar to those for cardiovascular disease, such as hypertension, hyperlipidemia, diabetes, and obesity9,10,11,12,13. According to published papers, people with these risk factors at midlife have relatively higher possibilities of suffering from dementia when aged more than 65 years9,10,11,12,13. In addition to increasing cardiovascular risk, family history, hypoxia, and other comorbidities are potential risk factors for neurodegeneration14,15,16. Some models using scores of these risk factors at midlife to predict the occurrence of dementia with aging have been developed for clinical assessments9,17. However, there is a lack of a direct relationship between these risk factors and dementia pathology.
Amyloid positron emission tomography (PET) is the most direct assessment of dementia pathology, especially AD18,19,20. Due to its low availability and high cost, amyloid PET examinations in HRD are difficult to perform. Significant correlations between biomarkers in cerebrospinal fluid (CSF) and amyloid PET results have been demonstrated21,22,23. CSF biomarker assays are an alternative way to explore dementia pathology in HRD. Lumbar puncture for sampling CSF, however, has side effects, which limit the utility of CSF biomarkers in clinical practice. Recently, assays for dementia biomarkers in plasma have become available24,25,26,27,28,29. Significant correlations between plasma amyloid β (Aβ) levels and amyloid PET results have been reported30,31,32. This implies that dementia pathology in HRD could be explored using plasma biomarker assays. In this study, immunomagnetic reduction (IMR) assays were utilized to assess plasma Aβ1–42 and total Tau protein (T-Tau) levels in HRD. The enrolled HRD included poststroke (PS) subjects, individuals with a family history of AD (ADFH), and patients with diabetes, end-stage renal disease (ESRD) and obstructive sleep apnea (OSA).
Methods
Recruitment of subjects
In this study, there were 246 subjects enrolled at six hospitals in Taiwan, and all studies were approved by the hospital institutional review boards. Thirty-seven heathy controls (HCs) were enrolled. There was no hypertension, hyperlipidemia, diabetes, obesity, cardiovascular disease, metabolic disease, brain ischemia, or renal disease in any of the HCs. There were 27 PS patients with normal cognition33. Thirty-five cognitively normal people had a first-degree family history of AD. Twenty-one subjects had diabetes mellitus (diabetes). Forty-one patients had end-stage renal disease (ESRD)34. Twenty subjects suffered from obstructive sleep apnea (OSA). Sixty-five patients with AD were enrolled35. The AD patients were diagnosed according to NIA-AA 2011 guidelines. The institutional review boards of all the joining hospitals approved this study. All participants provided written informed consent prior to study enrollment.
Plasma preparation
A 6-mL EDTA blood collection tube was used for blood draw, followed by centrifugation of the collected blood at a speed ranging from 1500 to 2500 g for 15 min at room temperature with the aid of a swing-bucket rotor. From each EDTA tube, 1 mL of plasma was transferred to 0.5-mL microcentrifuge tubes and stored at − 80 °C until biomarker assays were performed. Plasma was frozen no later than 4.5 h after blood draw. All plasma samples were shipped in a dry-ice package to MagQu Co., Ltd. in New Taipei City, Taiwan, for the blind assessment of plasma biomarkers.
Plasma biomarker assays
Plasma biomarkers were assayed with immunomagnetic reduction (IMR). IMR kits (MF-AB2-0060, MF-TAU-0060, MagQu) and the IMR analyzer (XacPro-S, MagQu) were used for assaying Aβ1–42 and T-Tau. For assaying Aβ1–42/T-Tau, 60/80 μL reagent was mixed with 60/40 μL plasma for each measurement. Duplicated measurements were conducted for each biomarker per sample. The mean value of the duplicated measurements was reported for each biomarker for a subject. The mean, repeatability coefficient of variation (%CV), within-lab %CV and lowest limit of quantification (LLOQ) of Aβ1–42 and T-Tau IMR assay are shown in Table 1.
Statistical methods
Continuous variables for each measurement are presented as the mean ± standard deviation. Continuous variables were compared using t-tests, and the p values were determined.
Ethical standards
The study was started and conducted after approval of the study protocol by the regional ethical committee in all the joined hospitals, including National Cheng Kung University Hospital, National Taiwan University Hospital, Cardinal Tien Hospital, Kaohsiung Chang Gung Memorial Hospital, Taipei City Hospital, and Shuang Ho Hospital, approved the study protocol, and the study was carried out in accordance with relevant guidelines and regulations, including the World Medical Association (WMA) Declaration of Helsinki. Since the patients could not themselves consent to the study, a written informed consent was obtained from the patient’s closest relative.
Results
The subjects with diabetes had an AC sugar level of 127.6 ± 26.7 g/dL and HbA1c level of 6.51 ± 0.52%. The individuals with OSA had an apnea–hypopnea index (AHI) of 54.6 ± 17.5.
Demographic information of the enrolled subjects is listed in Table 1. The ages of the HC, PS, ADFH, diabetes, ESRD, OSA and AD groups were 63.1 ± 12.4, 70.7 ± 6.9, 59.75 ± 4.7, 75.8 ± 7.3, 62.5 ± 7.8, 40.3 ± 8.7 and 78.8 ± 7.3 years, respectively. Except for ADFH and ESRD, all other groups had significant differences in age compared to the HC. Although the ages among groups were not matched, this was not a crucial point in exploring the differences in plasma biomarker levels among groups because the plasma Aβ1–42 and T-Tau levels measured with immunomagnetic reduction were not significantly age dependent36.
The subjects in the HC, PS, ADFH, ESRD and OSA groups were cognitively normal, had a clinical dementia ranking (CDR) of zero and a Mini-Mental State Examination (MMSE) score higher than 26. The CDR of every subject with AD was equal to or higher than 0.5 (1.11 ± 0.63). The MMSE score of the AD patients was 18.7 ± 4.1. The AD group clearly showed cognitive impairment.
The measured concentrations of plasma Aβ1–42 were 14.26 ± 1.42 pg/mL in HC, 15.43 ± 1.76 pg/mL in PS, 15.52 ± 1.60 pg/mL in ADFH, 19.74 ± 2.92 pg/mL in diabetes, 16.52 ± 0.59 pg/mL in ESRD, 15.97 ± 0.54 pg/mL in OSA and 20.06 ± 3.09 pg/mL in AD groups. Notably, the HC group showed relatively low levels of plasma Aβ1–42 (Fig. 1). The levels gradually increase across groups from HC to PS to ADFH to OSA to ESRD and to AD. Through t-test analyses using Aβ1–42 levels in HCs as a reference, the PS group showed a p value lower than 0.05, while the other groups showed p values lower than 0.001. This implied that groups, such as the PS, ADFH, ESRD and OSA groups, had significantly higher concentrations of plasma Aβ1–42 than the HC group but lower concentrations than the AD group of patients. According to the results in published papers, elevations in plasma Aβ1–42 levels were shown to be associated with amyloid pathology in the brain30,31,37,38. Thus, PS, ADFH, ESRD and OSA are high-risk factors for the accumulation of amyloid in the brain. Unfortunately, amyloid PET imaging was not available to explore amyloid deposition in the brain for the subjects in the PS, ADFH, ESRD and OSA groups in this study.
Dot plot of measured levels of Aβ1–42 in the plasma of healthy control (HC), poststroke subjects (PS), individuals with a family history of Alzheimer’s disease (ADFH), and patients with end-stage renal disease (ESRD), obstructive sleep apnea (OSA) and Alzheimer’s disease (AD). *p < 0.05 and **p < 0.01 versus healthy control.
Another typical biomarker for dementia, especially for AD, is tau protein. The levels of plasma total tau protein (T-Tau) were determined for all subjects. As listed in Table 2, the T-Tau level in the HC group was 15.13 ± 3.62 pg/mL; PS, 19.29 ± 8.01 pg/mL; ADFH, 17.93 ± 6.26 pg/mL; diabetes 19.74 ± 2.92 pg/mL; ESRD, 21.54 ± 2.72 pg/mL; OSA, 21.54 ± 2.72 pg/mL; and AD, 41.24 ± 14.64 pg/mL. The results showed that all PS (p < 0.05), ADFH (p < 0.001), diabetes (p < 0.001), ESRD (p < 0.001) and OSA (p < 0.001) patients had significantly higher levels of plasma T-Tau than HCs but significantly lower levels than AD patients. Hence, from the perspective of plasma biomarkers, these groups are at high risk for neurodegeneration.
Discussion
As shown in Table 1, the PS, ADFH, diabetes, ESRD, and OSA groups had higher levels of plasma Aβ1–42 and T-Tau than the HC group but lower levels than the AD group. This implied that there is a high suspicion of individuals in these groups progressing to dementia. Other previous analytic platforms show lower Aβ1–42 concentrations in AD compared with other diagnostic groups39,40. However, the different results may result from differences in detection principles and target proteins. Most of detection systems mainly recognizes Aβ42 monomer and a small amount of oligomer, but because it requires paired antibodies, the signal of oligomers may be underestimated. However, immunomagnetic reduction (IMR) uses only a single antibody and could identify both Aβ42 monomers and oligomers, allowing more target proteins to be captured. Several countries, including Sweden, Taiwan, United Kingdom and the United States, have used IMR to obtain similar data41,42,43. The above data prove that the results are reproducible and reproducible. According to studies by other labs, increased plasma Aβ oligomers level was measured in AD patients37,44. These results are similar to the IMR measurement results, so IMR may be mainly recognized to Aβ42 oligomer. The recognized Aβ categories still need to be further studied.
A follow-up study is needed to investigate the occurrence of dementia in these groups. It would be better to simultaneously observe the changes in plasma biomarker levels in the context of a longitudinal study. In fact, several papers have revealed the relatively high occurrence of dementia in PS individuals or those with ADFH, diabetes, ESRD, or OSA. For example, Pendlebury et al. reported that PS dementia occurs in 7% of PS patients 1 year after a stroke45. The incidence of cognitive impairment was 10–40% among those with ESRD46. As reported by Tufik et al., OSA has been associated with several comorbidities, including cognitive impairment47. A previous study showed that OSA patients exhibited significantly higher serum Aβ1–42 levels than age- and sex-matched controls48. Scarabino et al. showed that a family history of dementia was associated with an increased risk of AD, with an odds ratio of 2.71 (p < 0.05)15. Furthermore, an individual having a first-degree relative with dementia was significantly associated with risk of AD (odds ratio = 2.9, p < 0.05). Although the associations between these diseases and dementia have been discussed, the results of plasma Aβ1–42 and T-Tau levels reported in this study demonstrate the high risk for dementia with biological evidence.
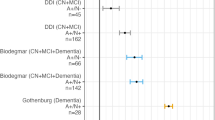
Plasma biomarkers are promising for assessing the risk of AD. The values of Aβ1–42xT-Tau in plasma have been validated as a clinical index for assessing AD35,42,49. Several research groups announced that the cutoff values of plasma Aβ1–42xT-Tau levels for discriminating amnesic mild cognitive impairment and AD patients from cognitively normal controls range from 382 to 455 pg2/mL235,42,49. The difference in the cutoff levels among reports might be due to some possible causes such as AD severity of enrolled subjects, subjective assessments on neuropsychological tests, plasma preparation, etc. In this study, the subjects showing plasma Aβ1–42xT-Tau levels higher than 382 pg2/mL2 were referred to subhealth.
The concentrations of Aβ1–42 in plasma for individuals in different high-risk group using IMR are shown in Fig. 1. The concentrations of Aβ1–42 in the high-risk group were lower than that in AD group (20.06 ± 3.09 pg/mL), but higher than that in HC group (14.26 ± 1.42 pg/mL). This indicates that the microenvironment of the brain has changed compared to normal individuals, resulting in an increase in the amount of Aβ1–42. The concentrations of plasma Tau for individuals in high-risk group are shown in Fig. 2. The concentrations of Tau in the high-risk group were lower than that in AD group (15.13 ± 3.62 pg/mL), but higher than that in HC group (41.24 ± 14.64 pg/mL). This suggests that the high-risk group has some neurological damage compared to the HC group, leading to an increase in the amount of Tau expression. The dot plot of plasma Aβ1–42xT-Tau for individuals in each group is shown in Fig. 3. The value of 382 pg2/mL2 is indicated with the dashed line. There were no individuals with plasma Aβ1–42xT-Tau levels higher than 382 among the HCs. However, some proportion of subjects in the PS, ADFH, diabetes, ESRD and OSA groups showed Aβ1–42xT-Tau levels higher than 382 pg2/mL2. The prevalence of subhealth in each group was analyzed and plotted with the gray background in Fig. 3. There were 37% of PS subjects and 11.4% of ADFH subjects considered subhealth. In the diabetes and ESRD groups, the prevalence of subhealth was 28.6% and 29.3%, respectively. The subhealth occurrence in the OSA group was found to be 15%. Based on the results in Fig. 1, PS is the riskiest factors for dementia. The fact that 37% of PS subjects were classified as subhealth may explain why the occurrence of poststroke dementia is so high45. Notably, ADFH showed a lower prevalence of subhealth than OS. Moreover, the ADFH group had only one-third of the subhealth prevalence observed in the PS group and half the prevalence observed in the diabetes and ESRD groups. This might imply that biological causes such as hypertension, hypoxia or electrolyte imbalance frequently found in PS, diabetes, ESRD and OSA patients are more dominant in relation to the risk for dementia than family history.
Dot plot of measured levels of Aβ1–42xT-Tau in the plasma of healthy controls (HCs), poststroke subjects (PS), individuals with a family history of Alzheimer’s disease (ADFH), and patients with end-stage renal disease (ESRD), obstructive sleep apnea (OSA) and Alzheimer’s disease (AD). The prevalence of subhealth (Aβ1–42xT-Tau ≥ 382) in each group is plotted with a gray background.
Limitation
The total numbers of enrolled subjects in each group are relatively limited. More subjects should be enrolled for validating the percentages of high-risk dementia in each group.
Conclusion
The plasma levels of Aβ1–42 and T-Tau in the PS, ADFH, diabetes, ESRD, and OSA groups were relatively high compared to those in the HC group but were lower than those in the AD group. On average, the prevalence of subhealth in these groups was 16.7%. This evidence indicated the high risk for dementia in these groups from the perspective of plasma biomarkers.
Data availability
The dataset generated and analyzed in the current study is available from the corresponding author on reasonable request.
References
Norton, S. et al. A commentary on studies presenting projections of the future prevalence of dementia. BMC Public Health 13, 1–5 (2013).
Ferri, C. P. et al. Global prevalence of dementia: A Delphi consensus study. Lancet 366, 2112–2117 (2005).
Brookmeyer, R. et al. Forecasting the global burden of Alzheimer’s disease. Alzheimers Dement. 3, 186–191 (2007).
Cao, Q. et al. The prevalence of dementia: A systematic review and meta-analysis. J. Alzheimers Dis. 73, 1157–1166 (2020).
McDonnell, M. N. et al. Aerobic exercise to improve cognitive function in adults with neurological disorders: A systematic review. Arch. Phys. Med. Rehabil. 92, 1044–1052 (2011).
Canevelli, M. et al. Nutrition and dementia: Evidence for preventive approaches? Nutrients 8, 144 (2016).
Ford, A. H. Preventing delirium in dementia: Managing risk factors. Maturitas 92, 35–40 (2016).
Iuliano, E. et al. Physical exercise for prevention of dementia (EPD) study: Background, design and methods. BMC Public Health 19, 659 (2019).
Kivipelto, M. et al. Risk score for the prediction of dementia risk in 20 years among middle aged people: A longitudinal, populationbased study. Lancet Neurol. 5, 735–741 (2006).
Chen, J. H. et al. Risk factors for dementia. Formos. Med. Assoc. 108, 754–764 (2009).
Norton, S. et al. Potential for primary prevention of Alzheimer’s disease: An of population-based data. Lancet Neurol. 13, 788–794 (2014).
Lipnicki, D. M. et al. Risk factors for mild cognitive impairment, dementia and mortality: The Sydney memory and ageing study. J. Am. Med. Dir. Assoc. 18, 388–395 (2017).
Sibbett, R. A. et al. Risk factors for dementia in the ninth decade of life and beyond: A study of The Lothian birth cohort 1921. BMC Psychiatry 17, 205 (2017).
Fox, C. et al. The importance of detecting and managing comorbidities in people with dementia? Age Ageing 43, 741–743 (2014).
Scarabino, D. et al. Influence of family history of dementia in the development and progression of late-onset Alzheimer’s disease. Neuropsychiatr. Genet. 171, 250–256 (2016).
Hassan, H. & Chen, R. Hypoxia in Alzheimer’s disease: Effects of hypoxia inducible factors. Neural Regen. Res. 16, 310–311 (2021).
Tsai, P. H. et al. Development and validation of a dementia screening tool for care in Taiwan: Brain health test. PLoS ONE 13, e0196214 (2018).
Furukawa, K. et al. Amyloid PET in mild cognitive impairment and Alzheimer’s disease with BF-227: Comparison to FDG-PET. J. Neurol. 257, 721–727 (2010).
Morbelli, S. & Bauckneht, M. Amyloid PET imaging: Standardization and integration with other Alzheimer’s disease biomarkers. Methods Mol. Biol. 1750, 203–212 (2018).
Suppiah, S. et al. The who, when, why, and how of PET amyloid imaging in management of Alzheimer’s disease-review of literature and interesting images. Diagnostics 9, 65 (2019).
Palmqvist, S. et al. Detailed comparison of amyloid PET and CSF biomarkers for identifying early Alzheimer disease. Neurology 85, 1240–1249 (2015).
Spallazzi, M. et al. CSF biomarkers and amyloid PET: Concordance and diagnostic accuracy in A MCI cohort. Acta Neurol. Belg. 119, 445–452 (2019).
Reimand, J. et al. Amyloid-β PET and CSF in an autopsy-confirmed cohort. Ann. Clin. Transl. Neurol. 7, 2150–2160 (2020).
Xia, W. et al. A specific enzyme-linked immunosorbent assay for measuring beta-amyloid protein oligomers in human plasma and brain tissue of patients with Alzheimer disease. Arch. Neurol. 66, 190–199 (2009).
Oh, E. S. et al. Comparison of conventional ELISA with electrochemiluminescence technology for detection of amyloid-β in plasma. J. Alzheimer’s Dis. 21, 769–773 (2010).
Birkmann, E. et al. Counting of single prion particles bound to a capture-antibody surface (surface-FIDA). Vet. Microbiol. 123, 294–304 (2007).
Kim, J. S. et al. Detection and quantification of plasma amyloid-β by selected reaction monitoring mass spectrometry. Anal. Chim. Acta 840, 1–9 (2014).
Mondello, S. et al. CSF and plasma amyloid-β temporal profiles and relationships with neurological status and mortality after severe traumatic brain injury. Sci. Rep. 4, 6446–6511 (2014).
Chiu, M. J. et al. Multi-channel SQUID-based ultrahigh-sensitivity in-vitro detections for bio-markers of Alzheimer’s disease via immunomagnetic reduction. IEEE Trans. Appl. Supercond. 21, 477–480 (2011).
Tzen, K. Y. et al. Plasma Aβ but not tau is related to brain PiB retention in early Alzheimer’s disease. ACS Chem. Neurosci. 5, 830–836 (2014).
Fan, L. Y. et al. The relation between brain amyloid deposition, cortical atrophy, and plasma biomarkers in amnesic mild cognitive impairment and Alzheimer’s disease. Front. Aging Neurosci. 10, 175 (2018).
Lin, S. Y. et al. Plasma amyloid assay as a pre-screening tool for amyloid positron emission tomography imaging in early-stage Alzheimer’s disease. Alzheimers Res. Therapy 11, 111 (2019).
Tang, S. C. et al. Plasma β-amyloids and tau proteins in patients with vascular cognitive impairment. Neuromol. Med. 20, 498–503 (2018).
Hou, Y. C. et al. The role of plasma neurofilament light protein for assessing cognitive impairment in patients with end-stage renal disease. Front. Aging Neurosci. 13, 657794 (2021).
Chiu, M. J. et al. Nanoparticle-states based immunomagnetic assay of plasma biomarkers for differentiating dementia and prodromal of Alzheimer’s disease—A cross-validation study. Nanomed. Nanotechnol. Biol. Med. 26, 10218 (2020).
Lue, L. F. et al. Age-dependent relationship between plasma Aβ40 And Aβ42 and total tau levels in cognitively normal subjects. Front. Aging Neurosci. 11, 222 (2019).
Zhou, L. et al. Plasma amyloid-β oligomers level is a biomarker for Alzheimer’s disease diagnosis. Biochem. Biophys. Res. Commun. 423, 697–702 (2012).
Assini, A. et al. Plasma levels of amyloid beta-protein 42 are increased in women with mild cognitive impairment. Neurology 63, 828–831 (2004).
De, W. F. et al. Plasma tau, neurofilament light chain and amyloid-β levels and risk of dementia: A population-based cohort study. Brain 43, 1220–1232 (2020).
Pesaresi, M. et al. Plasma levels of beta-amyloid (1–42) in Alzheimer’s disease and mild cognitive impairment. Neurobiol. Aging 27, 904–905 (2006).
Teunissen, C. E. et al. Plasma amyloid-β (Aβ42) correlates with cerebrospinal fluid Aβ42 in Alzheimer’s disease. J. Alzheimers Dis. 62, 1857–1863 (2018).
Lue, L. F. et al. Plasma levels of Aβ42 and tau identified probable Alzheimer’s dementia: Findings in two cohorts. Front. Aging Neurosci. 9, 226 (2017).
Chiu, M. J. et al. Synergistic association between plasma Aβ1–42 and p-tau in Alzheimer’s disease but not in Parkinson’s disease or frontotemporal dementia. ACS Chem. Neurosci. 21, 1376–1383 (2021).
Lim, C. Z. J. et al. Subtyping of circulating exosome-bound amyloid β reflects brain plaque deposition. Nat. Commun. 10, 1144 (2019).
Pendlebury, S. T. & Rothwell, P. M. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: A systematic review and meta-analysis. Lancet Neurol. 8, 1006–1018 (2009).
Drew, D. A. et al. Cognitive impairment in CKD: Pathophysiology, management, and prevention. Am. J. Kidney Dis. 74, 782–790 (2019).
Tufik, S. et al. Obstructive sleep apnea syndrome in the Sao Paulo epidemiologic sleep study. Sleep Med. 1, 441–446 (2010).
Bu, X. L. et al. Serum amyloid-beta levels are increased in patients with obstructive sleep apnea syndrome. Sci. Rep. 5, 13917 (2015).
Jiao, F. et al. The validation of multifactor model of plasma Aβ42 and total-tau in combination with MoCA for diagnosing probable Alzheimer disease. Front. Aging Neurosci. 12, 212 (2020).
Acknowledgements
We thank the MagQu company (New Taipei City, Taiwan) for detecting neurological biomarkers in plasma using the immunomagnetic reduction technique.
Funding
This work was supported by the Taiwan Ministry of Science and Technology under Grant Numbers 105-2314-B-002-001, 107-2321-B-039-004, 106-2314-B-038-001, 107-2314-B-038-050, 108–2314-B-303-029, and 109-231-B-002-029.
Author information
Authors and Affiliations
Contributions
This study was designed by S.Y.Y. and M.C.P. and run by C.C.W., Y.C.H., J.S.J., S.C.T., W.C.L., C.H.L., M.J.C., T.F.C., S.H.Y. and C.J.H. S.Y.Y. prepared the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
SY Yang is an employee and a shareholder of MagQu Co., Ltd. The other authors do not have competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pai, MC., Wu, CC., Hou, YC. et al. Evidence of plasma biomarkers indicating high risk of dementia in cognitively normal subjects. Sci Rep 12, 1192 (2022). https://doi.org/10.1038/s41598-022-05177-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-05177-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.