Abstract
To the authors’ knowledge, no study has been conducted on life expectancy for aged care facility residents with hip fracture. We assessed life expectancy of 240 residents of aged care facilities in Australia who experienced recent hip fracture treated with surgery. 149 deaths occurred over a mean follow-up of 1.2 years. Being female and having better cognition were associated with longer life expectancy. Increased age was associated with shorter life expectancy. The cumulative mortality rate within three months after hip fracture was 25.0% while the cumulative mortality rate for the whole study period was 62.1%. Life expectancy was 8.2 years, 4.8 years and 2.8 years for 70, 80 and 90-years old female patients. Life expectancy was 3.8 years, 2.2 years and 1.3 years for 70, 80 and 90 years old male patients, respectively. In conclusion, age, gender and cognition level were associated with life expectancy of hip fracture patients living in aged care facilities and their life expectancy was much shorter than that of the general Australian population.
Similar content being viewed by others
Introduction
Hip fracture has a substantial impact on survival and health-related quality of life of older people1,2. It is estimated that 1.6 million hip fractures occur worldwide each year and by 2050 this number could reach between 4.5 million and 6.3 million3,4. Hip fracture poses a significant economic burden worldwide5. Across Australian and New Zealand, more than 25,000 people break their hip each year with an estimated cost of 1 billion dollar annually6. Life expectancy is a statistical measure of the number of years that a human expects to live based on one’s current age and other demographic factors. Life expectancy is a key indicator used to assess mortality trends, disease burden, overall health status of a population and monitor trends in health care over time used by the World Health Organization (WHO)7. In Australia people who are 65 years of age or older (50 years or older if identified as an Aboriginal or Torres Strait Islander person) are eligible for aged care services, the Australian government pays aged care service providers to deliver aged care through subsidies and supplements, capital grants for residential aged care and program funding8. In 2017–18, 7% Australian aged 65 and over were in residential aged care facilities and about one-quarter (27%) hip fractures occurred in aged care facilities9. While it is well known that hip fracture is associated with increased mortality in both sexes10,11,12, to the authors’ knowledge, no study has been conducted on life expectancy for aged care facility residents with hip fracture. For hip fracture patients living in aged care facilities knowing his/her life expectancy many help patients, family members and health care providers make plans and decisions for patients’ care over the remaining lifespan.
The Southern Adelaide Co-ordinated Regional Hip and Debility Rehabilitation Programme to Improve Quality of Life (SACRED) was a randomised clinical trial which examined whether providing rehabilitation in aged care facilities for people who were recovering from hip fracture surgery improved quality of life and mobility at 4 weeks and 12 months. The primary outcomes of the trial were mobility and quality of life. The main study was conducted between June 2012 and December 2014, for mortality, the last follow up was extended to December 2015. The detailed descriptions of the trial, intervention methods and main results were reported elsewhere13,14. The objective of this analysis is to assess the life expectancy of people 70 and older after hip fracture and identify factors influencing the survival time.
Methods
Study design and participants
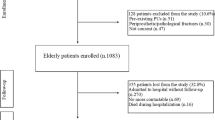
We performed secondary analyses using the data from the Southern Adelaide Co-ordinated Regional Hip and Debility Rehabilitation Programme to Improve Quality of Life trial (SACRED). The trial was conducted between June 2012 and December 2014; for mortality data, the last follow up was 18 December 2015. Participants were medically stable residential aged care facility residents aged 70 years or older who had experienced a new, surgically treated hip fracture and were ambulant prior to their fracture either without assistance, with aids, or with the assistance of one other person. Participants unable to provide informed consent or obtain consent from a suitable proxy, had pathological and peri-prosthetic fractures, had a terminal illness and were receiving palliative care, had a hip fracture treated non-surgically or were unable to follow a one-step command due to cognitive impairment at recruitment were excluded from the study13.
Outcomes
The outcome variable was survival time after hip fracture, calculated as date of death (all cause) or date of last follow up minus date of hip fracture. For patients surviving past 18 December 2015, the censored follow up time was calculated as 18 December 2015 minus the date of hip fracture. For patients who were lost to follow up or withdrew, survival time was calculated as date of last contact minus date of hip fracture.
Covariates
All covariates were measured at baseline: age; BMI; cognition as measured by Mini-Mental State Examination (MMSE); delirium; any previous fractures; previous hip fractures; surgery types and randomised group. All measurements and data collection were performed by the researchers or trained nurses for the trial.
Statistical analyses
Kaplan–Meier plots and log-rank tests were used to compare survival distributions across different groups. Weibull accelerated failure time (AFT) regression was chosen to investigate the associations between covariates and the survival time. Weibull AFT model was used to calculate life expectancy as it can produce robust results in ageing research15. The Weibull AFT model was specified as:
where subject i \( (\mathrm{i}=\mathrm{1,2},\dots \mathrm{n})\) had \(\mathrm{p}\) covariates \({x}_{i1,} {x}_{i2,}\) …\({x}_{ip}\) and possibly censored survival time \({t}_{i}\), \(\upsigma \) was the scale parameter, \({\varvec{\beta}}=\left ({\beta }_{0},\dots , {\beta }_{p}\right)\) were the regression coefficients of covariates, \({\varepsilon }_{1}\dots {\varepsilon }_{n}\) were independent and identically distributed according to the Gumbel distribution16,17. Life expectancy was calculated as the expected value of survival time \(,\mathrm{ E}\left (\mathrm{T}\right)=\mathrm{exp} ({{\varvec{x}}}_{{\varvec{i}}}^{\boldsymbol{^{\prime}}}{\varvec{\beta}})\Gamma (\sigma +1)\) where the Gamma function has the form \(\Gamma \left (\mathrm{z}\right)={\int }_{0}^{+\infty }{x}^{z-1}{e}^{-x}dx\)18.
For sensitivity analysis, a Cox proportional hazards regression model was used to investigate the associations between covariates and mortality and results were compared with the results of the Weibull AFT model.
Analyses were performed using SAS 9.4 (SAS Institute, Cary, NC) and RStudio 1.2.5001 with R 3.6.3 (RStudio, Inc. Boston, MA).
Ethics approval
The SACRED trial was registered on the Australian and New Zealand Clinical Trials Registry, registration number: ACTRN12612000112864. The Southern Adelaide Clinical Human Research Ethics Committee granted ethics approval for the secondary analysis of the trial and granted a waiver of informed consent (Application Number: 276.20). All research activities were carried out in accordance with the guidelines and regulations of the Australian National Health and Medical Research Council (NHMRC).
Results
A total of 240 participants of whom 178 (74.2%) were female and 62 (25.8%) were male were included in the study. The mean baseline age of participants was 88.6 (SD, 5.6) years, ranging from 70 to 101 years. The mean baseline mini-mental state examination (MMSE) score was 8.0 (SD, 7.8); 7.8% of participants had normal cognition or mild cognitive impairment, 33.8% suffered moderate cognitive impairment and 58.7% suffered severe cognitive impairment. 34.6% participants had delirium at baseline. The mini-nutritional assessment score was 5.3 (SD, 2.3). The mean BMI was 25.2 (SD, 4.9) kg/m2 with 5.4% underweight, 46.6% normal, 31.2% overweight and 16.7% obese. Ninety-four participants had experienced a previous fracture of any type and 32 had experienced a previous hip fracture. The most common surgery was intramedullary nailing (36.3%) and three participants had total hip replacement. Table 1 shows the baseline characteristics of participants.
The mean follow-up time for participants was 1.2 years, median was 1.1 years with range from 0.06 to 3.6 years. In total, 149 deaths occurred during the follow-up period. Kaplan–Meier curves (Fig. 1) showed that being female (log rank test: p = 0.0071), being of younger age (log rank: 0.0214) and having a higher MMSE score (log rank test: p = 0.0045) were associated with better survival. The survival curves were steeper (i.e. faster decline) early in the follow up period indicating that mortality rate was highest close to the time of hip fracture. The cumulative death rate within three months was 25.0% (60/240) and the cumulative death rate during the whole study period was 62.1% (149/240). Mortality rate was 118 deaths per 100 person-years within 3 months while the mortality rate of the whole study period (3.6 years) was 51.3 deaths per 100 person-years.
Table 2 showed being female indicated longer life expectancy (coefficient (β) = 0.86, 95% confidence interval (CI):0.39 to 1.34, p = 0.0004). Older age was associated with shorter life expectancy (β = − 0.06, 95% CI: − 0.10 to − 0.02, p = 0.0043). Relative to severe cognitive impairment, normal or mild-cognitive impairment (β = 1.18, 95% CI: 0.05 to 2.31, p = 0.0414) and moderate cognitive impairment (β = 0.56, 95% CI: 0.07 to 1.04, p = 0.0237) were associated with longer life expectancy. Randomisation groups, nutritional status, BMI, previous fractures of any type, previous hip fracture, and different surgery types were not associated with life expectancy.
Using the Weibull AFT model, we calculated life expectancy for different ages by sex. For females who underwent surgical treatment for hip fracture, estimated life expectancy would be 8.2 years for those aged 70 years, 4.8 years for those aged 80 years, and 2.8 years for those aged 90 years. For male patients, estimated life expectancy was 3.8 years for those aged 70 years, 2.2 years for those aged 80 years and 1.3 years for those aged 90 years. (Fig. 2).
Results of sensitivity analysis testing the same covariates in the Weibull AFT model in a multivariable Cox regression model did not yield different results. All estimates were consistent with the Weibull AFT model (in terms of association, direction and significance) (Table 3).
Discussion
In this longitudinal study of 240 hip fracture patients, we found that older age, male gender and greater impairment of cognition were associated with reduced life. Life expectancy of hip fracture patients living in aged care facilities was lower than in the general Australian population especially for those younger patients. This study also found that mortality rate was much higher immediately following the hip fracture.
Life expectancy is defined as the average number of years a group of people is expected to live at a certain age, comparing hip fracture patients’ life expectancy with that of the general population could show a straightforward impact of hip fracture on the population and the disease burden. The Treasurer of the Commonwealth of Australia estimated that in 2015 for a 70 year old female the life expectancy was 19.3 years (i.e. at 70 years old she was expected to live to 89.3 years) and for a 70 year old male the life expectancy was 16.9 years19. Therefore, the life expectancy of a 70 year old female hip fracture patient living in an aged care facility could be 11 (19.3–8.2 = 11.1) years shorter than that of the Australian general population, and it could be 13 years (16.9–3.8 = 13.1) shorter for a 70 year old man.
Studies have shown that women had a much higher risk for hip fracture than men, but men had much higher mortality than women after hip fractures20,21,22,23,24. In our study we observed that men’s hazard rate for death was about twice that of women (HR = 1.98). Our study also found that if a hip fracture happened at a younger age, males would have much shorter life expectancy than females, however the difference decreased at older ages. Previous studies have found cognitive impairment to be a major risk factor for mortality after hip fracture and this was confirmed by our study25,26. Studies showed MMSE cannot be used to detect delirium but can be used to ruling out delirium as shown by several studies27,28. Our data also support that MMSE can be used to rule out delirium, such as with normal cognitive (MMSE > 24) none of the patients had delirium, however among severe cognitive impairment (MMSE < 10) patients about 50% patients had delirium which means high MMSE will be useful to rule out delirium. However, to avoid collinearity, we did not put delirium variable into the final model since the delirium was highly correlated with MMSE (Spearman correlation coefficient = − 0.87, p < 0.0001). The relationship between mortality and BMI after hip fracture was not consistent; some studies suggested that being overweight or obese were protective factors for mortality after hip fracture29,30, however, Akinleye et al. followed 15,108 patients who underwent surgery for hip fracture over a 5 year period and found that either extreme of the BMI spectrum had the highest mortality rates31. In our study we did not find an association between BMI and mortality after hip fracture in these older patients. We did not find any association between the type of hip surgery and life expectancy, this result was consistent with a retrospective registry-based cohort study of 14,932 patients undergoing hip fracture surgery in Sweden32.
Mortality rate after hip fracture is associated with time since injury. Kanis et al. showed that mortality rate after a hip or vertebral fracture is non-linear; the rate slows down significantly with time33,34,35. We found the same phenomenon as the mortality rate within three months was much higher than the whole study period. However, a study showed that death rate was increasing in the first 6 to 9 months after hip fracture due to infection and cardiovascular disease36. Interventions at which stage and what kind of interventions can more effectively prevent excessive deaths warrant further studies.
This study had several strengths. The commencements of follow up and baseline characteristics of the patients were well defined and accurately measured. The follow-up rate was high and patients who were lost follow-up and withdrew from the study were well documented. Our study directly calculates the survival time which is the most natural measure of life for both clinicians and patients. This study had limitations. Firstly, for the clinical trial, 2210 patients were aassessed for eligibility, 1766 were not meeting inclusion criteria and 114 declined to participate which made our sample size as 240, this inclusion/exclusion procedures made our study lack of generalisability and our results might not be generalized to broader hip fracture patients. Secondly, the life expectancy in this study was calculated by parametric method while the life expectancy of Australian population was calculated by life table method, the parametric method could overestimate the life expectancy of the patients and cause extra bias when comparing the life expectance between the specific population and the general population37. Thirdly, our sample size was small and we did not provide confidence intervals for the life expectancies, further studies with bigger sample size might provide more accurate life expectancies for hip fracture patients. Finally, the follow up time of this study was short, our model parameters derived from the short period of follow up time might not fit long term mortality of the population.
Conclusions
Overall, our data suggested that age, gender and cognition were associated with life expectancy of hip fracture patients. The life expectancy of hip fracture patients living in aged care facilities was much lower than that of the general Australian population as would be expected with this very disabled group of older people. Hip fracture occurring at a younger age in this population could cause more loss of life expectancy. Interventions at which stage and what kind of interventions can more effectively prevent excessive deaths warrant further studies.
Data availability
The data that support the findings of this study are available from Dr. Enwu Liu or Professor Maria Crotty (Maria.Crotty@sa.gov.au), upon reasonable request and ethnic approval from the Southern Adelaide Clinical Human Research Ethics Committee.
References
Svedbom, A. et al. Quality of life for up to 18 months after low-energy hip, vertebral, and distal forearm fractures-results from the ICUROS. Osteoporos. Int. 29 (3), 557–566 (2018).
Civinini, R. et al. Functional outcomes and mortality in geriatric and fragility hip fractures—Results of an integrated, multidisciplinary model experienced by the “Florence hip fracture unit”. Int. Orthop. 43 (1), 187–192 (2019).
Gullberg, B., Johnell, O. & Kanis, J. World-wide projections for hip fracture. Osteoporos. Int. 7 (5), 407–413 (1997).
Cooper, C., Campion, G. & Melton, L. J. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 2 (6), 285–289 (1992).
Williamson, S. et al. Costs of fragility hip fractures globally: A systematic review and meta-regression analysis. Osteoporos. Int. 28 (10), 2791–2800 (2017).
ANZHFR Annual Report of Hip Fracture Care 2019. Australian and New Zealand Hip Fracture Registry. (2019).
Teeraananchai, S., Kerr, S., Amin, J., Ruxrungtham, K. & Law, M. Life expectancy of HIV-positive people after starting combination antiretroviral therapy: A meta-analysis. HIV Med. 18 (4), 256–266 (2017).
AIHW. Aged care [Internet]. (Australian Institute of Health and Welfare, 2019). https://www.aihw.gov.au/reports/australias-welfare/aged-care.
AIHW. Australian Institute of Health and Welfare 2018. Hip Fracture Incidence and Hospitalisations in Australia 2015–16. Cat. No. PHE 226. (AIHW, 2018).
Katsoulis, M. et al. Excess mortality after hip fracture in elderly persons from Europe and the USA: The CHANCES project. J. Intern. Med. 281 (3), 300–310 (2017).
Kilci, O. et al. Postoperative mortality after hip fracture surgery: a 3 years follow up. PLoS ONE 11 (10), e0162097 (2016).
Farahmand, B. Y., Michaelsson, K., Ahlbom, A., Ljunghall, S. & Baron, J. A. Survival after hip fracture. Osteoporos. Int. 16 (12), 1583–1590 (2005).
Crotty, M. et al. Should we provide outreach rehabilitation to very old people living in Nursing Care Facilities after a hip fracture? A randomised controlled trial. Age Ageing 48 (3), 373–380 (2019).
Killington, M. et al. People living in nursing care facilities who are ambulant and fracture their hips: Description of usual care and an alternative rehabilitation pathway. BMC Geriatr. 20 (1), 128 (2020).
Swindell, W. R. Accelerated failure time models provide a useful statistical framework for aging research. Exp. Gerontol. 44 (3), 190–200 (2009).
Lai, C.-D. Generalized Weibull Distributions 23–75 (Springer, 2014).
Liu, E. & Lim, K. Using the Weibull accelerated failure time regression model to predict time to health events. bioRxiv 2018:362186.
Artin, E. The Gamma Function. (Courier Dover Publications, 2015).
2015 Intergenerational Report, Australia in 2055. (Hockey, J., Australia, T., eds.) (A.C.T: Treasury, 2015).
Lobo, E. et al. Gender differences in the incidence of and risk factors for hip fracture: A 16-year longitudinal study in a southern European population. Maturitas 97, 38–43 (2017).
Sullivan, K. J., Husak, L. E., Altebarmakian, M. & Brox, W. T. Demographic factors in hip fracture incidence and mortality rates in California, 2000–2011. J. Orthop. Surg. Res. 11, 4 (2016).
Alvarez-Nebreda, M. L., Jiménez, A. B., Rodríguez, P. & Serra, J. A. Epidemiology of hip fracture in the elderly in Spain. Bone 42 (2), 278–285 (2008).
Kannegaard, P. N., van der Mark, S., Eiken, P. & Abrahamsen, B. Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing. 39 (2), 203–209 (2010).
Kristensen, P. K., Johnsen, S. P., Mor, A., Thillemann, T. M. & Pedersen, A. B. Is the higher mortality among men with hip fracture explained by sex-related differences in quality of in-hospital care? A population-based cohort study. Age Ageing 46 (2), 193–199 (2017).
Schaller, F. et al. Mild to moderate cognitive impairment is a major risk factor for mortality and nursing home admission in the first year after hip fracture. Bone 51 (3), 347–352 (2012).
Tarazona-Santabalbina, F. J. et al. Severity of cognitive impairment as a prognostic factor for mortality and functional recovery of geriatric patients with hip fracture. Geriatr. Gerontol. Int. 15 (3), 289–295 (2015).
Mitchell, A. J., Shukla, D., Ajumal, H. A., Stubbs, B. & Tahir, T. A. The mini-mental state examination as a diagnostic and screening test for delirium: Systematic review and meta-analysis. Gen. Hosp. Psychiatry. 36 (6), 627–633 (2014).
Ringdal, G. I. et al. Using the mini-mental state examination to screen for delirium in elderly patients with hip fracture. Dement. Geriatr. Cogn. Disord. 32 (6), 394–400 (2011).
Prieto-Alhambra, D. et al. Relationship between mortality and BMI after fracture: A population-based study of men and women aged≥ 40 years. J. Bone Miner. Res. 29 (8), 1737–1744 (2014).
Flodin, L., Laurin, A., Lökk, J., Cederholm, T. & Hedström, M. Increased 1-year survival and discharge to independent living in overweight hip fracture patients. Acta Orthop. 87 (2), 146–151 (2016).
Akinleye, S. D., Garofolo, G., Culbertson, M. D., Homel, P. & Erez, O. The role of BMI in hip fracture surgery. Geriatr. Orthop. Surg. Rehabil. 9, 2151458517747414 (2018).
Åhman, R. et al. Determinants of mortality after hip fracture surgery in Sweden: A registry-based retrospective cohort study. Sci. Rep. 8 (1), 15695 (2018).
Johnell, O. et al. Mortality after osteoporotic fractures. Osteoporos. Int. 15 (1), 38–42 (2004).
Kanis, J. et al. Correspondence in response to OSIN-D-18-00831 quantifying imminent risk. Osteoporos. Int. 30 (2), 525–526 (2019).
Kanis, J. et al. Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporosis Int. 31, 1–12 (2019).
Cameron, I. D. et al. Hip fracture causes excess mortality owing to cardiovascular and infectious disease in institutionalized older people: A prospective 5-year study. J. Bone Miner. Res. 25 (4), 866–872 (2010).
Fledelius, P., Guillen, M., Nielsen, J.P. & Petersen, K.S. A comparative study of parametric and nonparametric estimators of old-age mortality in Sweden (2004).
Acknowledgements
The authors thank Dr Karen Lim for the editing of this manuscript.
Funding
The SACRED trial was supported by funding provided by the National Health and Medical Research Council (NHMRC) Partnership Centre on Dealing with Cognitive and Related Functional Decline in Older People (grant no. GNT9100000). There was no funding for the secondary analysis of the trial.
Author information
Authors and Affiliations
Contributions
E.L., I.D.C., S.K. and M.C. designed the study. E.L. had full access to the dataset and analysed the data. M.K. provided the data had full access to the dataset. E.L. and R.L. drafted the manuscript and all authors provided critical revisions and approved the final submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author (s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, E., Killington, M., Cameron, I.D. et al. Life expectancy of older people living in aged care facilities after a hip fracture. Sci Rep 11, 20266 (2021). https://doi.org/10.1038/s41598-021-99685-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99685-z
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.