Abstract
The emergence of a novel SARS-CoV-2 B.1.1.7 variant sparked global alarm due to increased transmissibility, mortality, and uncertainty about vaccine efficacy, thus accelerating efforts to detect and track the variant. Current approaches to detect B.1.1.7 include sequencing and RT-qPCR tests containing a target assay that fails or results in reduced sensitivity towards the B.1.1.7 variant. Since many countries lack genomic surveillance programs and failed assays detect unrelated variants containing similar mutations as B.1.1.7, we used allele-specific PCR, and judicious placement of LNA-modified nucleotides to develop an RT-qPCR test that accurately and rapidly differentiates B.1.1.7 from other SARS-CoV-2 variants. We validated the test on 106 clinical samples with lineage status confirmed by sequencing and conducted a country-wide surveillance study of B.1.1.7 prevalence in Slovakia. Our multiplexed RT-qPCR test showed 97% clinical sensitivity and retesting 6,886 SARS-CoV-2 positive samples obtained during three campaigns performed within one month, revealed pervasive spread of B.1.1.7 with an average prevalence of 82%. Labs can easily implement this test to rapidly scale B.1.1.7 surveillance efforts and it is particularly useful in countries with high prevalence of variants possessing only the ΔH69/ΔV70 deletion because current strategies using target failure assays incorrectly identify these as putative B.1.1.7 variants.
Similar content being viewed by others
Introduction
In Dec 2020, Rambaut et al.1 reported the genomic characterization of a distinct phylogenetic cluster named lineage B.1.1.7 (also referred to as 20I/501Y.V1 by Nextstrain (https://nextstrain.org/sars-cov-2/), Variant of Concern (VOC) 202012/01, or Alpha by WHO), briskly spreading over the past four weeks in the United Kingdom. The new lineage has 23 mutations: 13 non-synonymous mutations, 4 deletions, and 6 synonymous mutations. The spike protein contains ten mutations at the amino-acid level (ΔH69/ΔV70 and ΔY144 deletions, N501Y, A570D, D614G, P681H, T716I, S982A, D1118H) that could potentially change binding affinity of the virus2,3,4 and consequently virus-host interaction. Indeed, emerging evidence suggests lineage B.1.1.7 has enhanced transmissibility3,5,6,7,8, results in higher viral loads9,10, and causes increased mortality11. These data highlight the need for tools to facilitate enhanced surveillance of lineage B.1.1.7 as well as other variants that may harbour spike gene mutations that alter viral dynamics.
The dominant approach used to putatively detect lineage B.1.1.7 involves conducting multigene RT-qPCR tests that result in positive detection of SARS-CoV-2 in one or more gene sets together with a so-called S gene target failure (SGTF), which is used as a proxy for the B.1.1.7 variant. This approach permits widespread, rapid screening, but is limited by the fact that other variants, in addition to lineage B.1.1.7, produce SGTFs. Thus, the SGTF screening method depends on the presence of other variants in a region and how they vary over time. Whole genome sequencing is the gold-standard for detection of the B.1.1.7 variant. This provides direct confirmation of the variant and identification of emerging variants; however, it is expensive, time consuming, low throughput, and many countries lack a robust genomic surveillance program, making this approach unwieldy to adopt for tracking and mitigating the spread of the B.1.1.7 variant.
Here, we report the development of a novel, multiplexed RT-qPCR test for differentiating lineage B.1.1.7 from all other SARS-CoV-2 lineages. We validated the test using a selected set of 106 clinical samples collected during routine testing with the lineage status verified by sequencing. Unlike other tests that rely on indirect detection via SGTF, this test contains primers that target the ΔH69/ΔV70 and ΔY144 deletions in the spike gene that permit the direct detection of lineage B.1.1.7. This assay was used in three rounds of a country-wide screening of the prevalence of B.1.1.7 in Slovakia, which included 6,886 SARS-CoV-2 positive samples, revealing increasing prevalence of lineage B.1.1.7 over time in Slovakia. This RT-qPCR assay provides a useful tool for countries to rapidly identify hot spots of this new B.1.1.7 variant and implement test, trace, and isolate strategies to prevent this variant from becoming widespread. Countries currently experiencing extensive circulation of variants carrying only the ΔH69/ΔV70 deletion may find this test particularly useful as these would be falsely identified as the B.1.1.7 variant via SGTF tests.
There is also a growing need for more streamlined and sensitive open-source SARS-CoV-2 diagnostic tests. Most open-source protocols rely on singleplex assays that require lengthy workflows (e.g., USA CDC, China CDC) or lack sample quality control assays (e.g., Institut Pasteur, Charité) to ensure proper sample collection and assay performance. Our SARS-CoV-2 S gene assay that is multiplexed with the USA CDC human RNase P assay provides an ultrasensitive, efficient, and affordable solution to supplement current open-source SARS-CoV-2 diagnostic tests.
Results
Identification of RT-qPCR targets by bioinformatic analysis
Our analysis of 1,136 spike gene sequences (spanning 1—21 December 2020) revealed 228 sequences (20%) that contained both the ΔH69/ΔV70 and ΔY144 deletions (for country of origin, see Supplementary Table S1). The shorter deletion (ΔY144) always co-occurred with the longer deletion (ΔH69/ΔV70), whereas the (ΔH69/ΔV70) deletion occurs independently in 17 sequences (1.5%). Pearson’s correlation coefficient of the deletions is 0.953.
We analysed over 900,000 SARS-CoV-2 genomes to determine the prevalence of both ΔH69/ΔV70 and ΔY144 deletions in lineage B.1.1.7 and lineages other than B.1.1.7 and found a total of 257,953 sequences that possess both deletions. Based on the metadata file, we identified SARS-CoV-2 lineages across all called sequences with both deletions. Only 1,230 sequences (0.48%) out of 257,953 sequences are not labelled as B.1.1.7. In other words, 99.52% of sequences containing both deletions belong to lineage B.1.1.7, highlighting the notion that these two deletions are highly specific for the B.1.1.7 variant and make ideal targets for primer/probe design (Table 1).
Development of a multiplexed RT-qPCR assay to distinguish lineage B.1.1.7 from all other SARS-CoV-2 variants
To develop a multiplexed RT-qPCR test to distinguish lineage B.1.1.7, we designed two assays targeting either the wild-type SARS-CoV-2 spike gene or the ΔH69/ΔV70 and ΔY144 deletions that are highly specific to lineage B.1.1.7 (for primer/probe locations and sequences see Fig. 1, Table 2, respectively).
Development and optimization of a general SARS-CoV-2 S gene primer/probe set for all SARS-CoV-2 variants. Schematic illustrates genomic organization of SARS-CoV-2 with an emphasis on the location of both SARS-CoV-2 S gene and B.1.1.7 primer/probe sets relative to the ΔH69/ΔV70 and ΔY144 deletions (red lines with ball points) observed in the spike gene of B.1.1.7 variants.
We began by designing a general S gene primer/probe assay (SARS-CoV-2 S gene) that could be used for screening purposes and would detect the most common strains of SARS-CoV-2 as well as variants containing ΔH69/ΔV70, including lineage B.1.1.7. We assessed the performance of a series of primers flanking the ΔH69/ΔV70 deletion (Supplementary Fig. S1a,b; for primer/probe sequences, see Supplementary Table S2). After selecting the optimal primer/probe combination, we introduced an additional hydrolysis probe, identically labelled with the same reporter and quencher dyes, that would hybridize in tandem (i.e., on the same strand) with the first hydrolysis probe. Consistent with other reports12,13, this dual probe approach enhanced sensitivity and specifity (Supplementary Fig. S1c,d).
For our assay targeting lineage B.1.1.7, we leveraged the highly specific co-occurrence of the ΔH69/ΔV70 and ΔY144 deletions in lineage B.1.1.7 (99.52%, Table 1). By designing a series of forward primers to target the ΔH69/ΔV70 deletion, we differentiated wild type template from ΔH69/ΔV70 template (Supplementary Fig. S2a). Since other SARS-CoV-2 variants share the ΔH69/ΔV70 deletion (e.g., B.1.1.298, B.1.160, B.1.177, B.1.258, B.1.375, B.1.525), we designed a series of reverse primers to target the second, three base pair deletion (bp: 21,991–21,993; ΔY144) and utilized allele-specific PCR approaches14,15,16 and judicious placement of LNA-modified nucleotides to enhance the specificity of the assay (Supplementary Fig. S2b,c). This approach enabled us to differentiate B.1.1.7 variants that contain both the ΔH69/ΔV70 and ΔY144 deletions from SARS-CoV-2 variants that contain only the ΔH69/ΔV70 deletion, provided that a second reaction is ran in parallel using the SARS-CoV-2 S gene set that can be used as a benchmark to assess the relative sensitivity. If the B.1.1.7 primer set amplifies the sample within five Ct cycles of the SARS-CoV-2 S gene primer set, then the sample is B.1.1.7 positive. Alternatively, if the B.1.1.7 primer set amplifies the sample in 8 or more Ct cycles relative to the SARS-CoV-2 S gene primer set, than the sample likely belongs to a variant that contains the ΔH69/ΔV70 deletion, but not the ΔY144 deletion, and hence is B.1.1.7 negative.
We compared three different versions of B.1.1.7 primer/probe sets using a selected set of 46 samples, some of which were sequenced to confirm lineage status. Given our interpretation criterion (Supplementary Table S4), we determined that the V3 primer/probe set performed the best since it correctly identified all B.1.1.7 and ΔH69/ΔV70 deletion samples, with the exception of one ΔH69/ΔV70 deletion sample that was interpreted as inconclusive (Supplementary Fig. S3).
Analytical sensitivity and clinical evaluation of lineage B.1.1.7 S gene primer/probe set
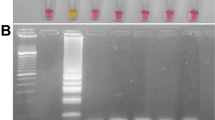
With our final primer/probe sets for SARS-CoV-2 S gene and B.1.1.7 (Table 2), we multiplexed each assay with the US CDC human RNase P primer/probe set (for sequences, see17) as an internal control to assess RNA extraction and assay performance. We then determined the analytical sensitivity using serial dilutions of RNA extracted from a B.1.1.7 positive sample. Both assays displayed high sensitivity (Fig. 2a) with our SARS-CoV-2 S gene and B.1.1.7 assays reliably detecting down to only 2 copies/reaction (0.4 copies/μl) and 10 copies/reaction (2 copies/μl), respectively, placing them among the most sensitive SARS-CoV-2 RT-qPCR assays available.
Analytical sensitivity and clinical validation of SARS-CoV-2 S gene and B.1.1.7 assays. (a) The limit of detection was determined for both SARS-CoV-2 S gene and B.1.1.7 assays by serial dilutions of isolated viral B.1.1.7 RNA. Data depict the mean and SD of eight replicates per each dilution. The dotted line at Ct 40 serves as a threshold after which amplification is considered invalid. (b) Overview of ΔCt values (= B.1.1.7 assay Ct—SARS-CoV-2 S gene assay Ct) for each sample in the clinical validation. Symbols represent the various SARS-CoV-2 lineages that were identified by sequencing. Closed symbols represent samples correctly identified by either the SARS-CoV-2 S gene or B.1.1.7 assays, whereas open symbols denote samples that did not meet the criterion established for variant identification. The shaded background shows ΔCt ranges that correspond with the criterion to report a sample as B.1.1.7 positive (pink), ΔH69/ΔV70 deletion positive (teal), and inconclusive (gray). ND, not detected. (c) Decision tree demonstrating the proper workflow, interpretation criterion, and actions to implement the SARS-CoV-2 S gene and B.1.1.7 assays in a testing regime to identify B.1.1.7 positive samples.
We evaluated the clinical performance of our SARS-CoV-2 S gene and B.1.1.7 assays on 106 clinical samples that underwent sequencing to identify lineage status using interpretation criterion outlined in Supplementary Table S4. A detailed flow chart of the patient samples is depicted in Supplementary Fig. S4. Our SARS-CoV-2 S gene assay detected all 106 clinical samples regardless of lineage (Table 3) confirming its utility as a general screening assay for the most common SARS-CoV-2 variants. Out of 67 clinical samples classified as lineage B.1.1.7 by sequencing, our B.1.1.7 assay positively identified 65 samples, while one sample (Sample 75) was not detected by the B.1.1.7 assay and another sample was deemed inconclusive. The ΔCt of this sample was slightly greater than five cycles (e.g., Sample 40, ΔCt = 5.7) relative to the Ct value for the SARS-CoV-2 S gene assay, which exceeded our cut-off for a positive identification (Fig. 2b).
Notably, our assay was also capable of identifying samples carrying the ΔH69/ΔV70 deletion such as those belonging to the B.1.258 lineage, provided that the sample contains sufficient viral load as other ΔH69/ΔV70 variants yield ΔCt values greater than 8 Ct cycles. For the 24 samples that carry only the ΔH69/ΔV70 deletion and belong to lineage B.1.258, our B.1.1.7 assay correctly identified 20 out of 24 samples. Three samples were not detected by the B.1.1.7 assay possibly due to relatively high Ct values in the SARS-CoV-2 S gene assay for two samples (Sample 33, Ct = 30.1 and Sample 65, Ct = 28.9), making confirmation of the ΔH69/ΔV70 status impossible with our cut-off criterion. One sample had a ΔCt outside the criterion for ΔH69/ΔV70 deletion confirmation and was deemed inconclusive. Neither the B.1.1.7 assay nor the common SARS-CoV-2 S gene assay yielded a positive signal when testing the 94 samples that were previously identified as SARS-CoV-2 negative, while RNase P, in both multiplexed assays, was positive for all 94 samples (Table 3). Both assays did not amplifiy any of the respiratory pathogens that were tested in a cross reactivity experiment (Supplementary Table S6).
Overall, the clinical evaluation confirmed the diagnostic utility of both our SARS-CoV-2 S gene and B.1.1.7 assays, which showed 100% (106/106) and 97% (65/67) diagnostic sensitivity, respectively. The assay also showed diagnostic utility for identifying variants containing only the ΔH69/ΔV70 deletion by detecting 83.3% (20/24) of lineage B.1.258 samples. When considering B.1.258 samples containing high viral loads (Ct ≤ 28), which is necessary to identify variants with only the ΔH69/ΔV70 deletion, the diagnostic sensitivity reached 91.7% (22/24). For an overview of the clinical evaluation data, lineage of each sample, and GISAID information, see Supplementary Table S7. We have provided a decision tree (Fig. 2c) that users may follow to implement this test to directly detect the presence of the B.1.1.7 variant.
Surveillance of lineage B.1.1.7 reveals increasing prevalence throughout the Slovak Republic
To determine the prevalence of lineage B.1.1.7 and its spread throughout the Slovak Republic, regional public health authorities used this test to screen nearly 7,000 samples previously identified as SARS-CoV-2 positive during three screening rounds over a one month period. The first surveillance screening for lineage B.1.1.7 on February 2nd, 2021 revealed a region-specific prevalence of B.1.1.7 ranging from 52% (Žilina) to 85% (Trnava) with an overall B.1.1.7 prevalance of 75% (Fig. 3a–c, Supplementary Table S8). During the second round of screening held on February 17th, 2021, the majority of regions (5 out of 8) showed increased prevalence, although due to reduced prevalence in Banská Bystrica, Košice, and Nitra, the overall prevalence remained at 74%. Closer scrutiny of the data suggests the reduced prevalence in some regions was caused by samples originating from several “non-B.1.1.7 clusters” (e.g., in social care homes), where all positive samples were likely derived from a common infection source. Exclusion of these clusters results in a slight increase in prevalence of 78%. A final screening on March 3rd, 2021 showed increased B.1.1.7 prevalence in all regions and an overall prevalence of 85%. Taking into consideration estimates of growth rates (i.e., reproduction number) for lineage B.1.1.7 in the UK6,8, we used the prevalences obtained on the first screening round (February 2nd, 2021) to estimate historical and future prevalences using a range of two weeks and applying spread factors (3.3 and 5.4) estimated in other countries (Fig. 3d). Although the expected data did not fit with our observed data, a number of factors likely influence regional spread, including the presence and virulence of competing SARS-CoV-2 lineages and selection biases from cluster outbreaks.
Tracking the prevalence of lineage B.1.1.7 in Slovakia. (a) Maps of the prevalence of lineage B.1.1.7 in the eight regions of Slovakia during the three screening rounds held on February 2nd, 2021, February 17th, 2021, and March 3rd, 2021. Regions in red have prevalence > 80%, regions in yellow have prevalence < 60%. (b) Maps of the prevalence of lineage B.1.1.7 in the 79 districts of Slovakia during the three screening rounds held on February 2nd, 2021, February 17th, 2021, and March 3rd, 2021. Regions in red have prevalence > 80%, regions in yellow have prevalence < 60%. (c) Trends in B.1.1.7 prevalence during the three screening rounds in each of the eight regions of Slovakia. (d) Observed trends in B.1.1.7 prevalence during the three screening rounds and expected prevalence given various 2-week spread factors (shown in parentheses) assuming the prevalence of February 2nd, 2021. The prevalence maps in sections (a,b) were generated using Datawrapper (https://www.datawrapper.de/) in version 1.25.0.
Discussion
The recent emergence of a novel SARS-CoV-2 variant called lineage B.1.1.7 has sparked global consternation as it has now been confirmed in over 70 countries and threatens to exacerbate an already dire pandemic. To mitigate the spread of the B.1.1.7 variant, it is imperative that countries have diagnostic tools that can quickly and accurately detect and track the prevalence of the variant in order to implement the appropriate epidemiological measures. Here we report a novel RT-qPCR test to differentiate the B.1.1.7 variant from other SARS-CoV-2 lineages. The test consists of running two S gene target assays, one specific for B.1.1.7 and the other for all SARS-CoV-2 strains, and performing a simple comparison of relative Ct values that allows the user to differentiate the B.1.1.7 variant from other variants that have the ΔH69/ΔV70 deletion. We validated this test on clinical samples that were sequenced to determine the exact SARS-CoV-2 lineage and the results demonstrated a high level of sensitivity in distinguishing the B.1.1.7 variant. Moreover, we retested nearly 7000 samples previously confirmed as SARS-CoV-2 positive by a reference method in three screening rounds over a one month period, revealing widespread and increasing prevalence of lineage B.1.1.7 throughout the Slovak Republic. This RT-qPCR test allows a positive identification of the B.1.1.7 variant, providing countries with a powerful tool to detect and track lineage B.1.1.7, especially countries that have considerable prevalence of variants carrying only the ΔH69/ΔV70 deletion18,19,20,21, which are mistakenly identified as B.1.1.7 variants by currently used SGTF assays.
Although there are hundreds of approved RT-qPCR tests for the detection of SARS-CoV-2, few of them are capable of directly differentiating the B.1.1.7 variant from common variants of SARS-CoV-2. Paradoxically, failed RT-qPCR tests have been instrumental in identifying putative B.1.1.7 positive samples and tracking its prevalence18,20,22,23,24,25. These RT-qPCR tests contain multigene assays, with at least one assay targeting the spike gene, and during routine testing a “drop-out” in the spike gene assay may occur (often termed as S gene target failure, or SGTF), while other gene targets yield positive signals. This SGTF can indicate the presence of the B.1.1.7 variant and flag samples for confirmation by sequencing. It is important to note, however, that SGTPs are produced by other variants that contain the ΔH69/ΔV70 deletion, including the B.1.1, B1.258, B.1.525, and B.1.1.298 (the mink cluster V) lineages, as well7. This highlights the importance of follow up sequencing of SGTF samples to determine lineage status.
Indeed, an analysis of SGTFs and corresponding sequencing data by Public Health England revealed that SGTF assays were poor proxies for the presence of B.1.1.7 in early October with only 3% of SGTFs assays positively identifying a B.1.1.7 variant. The SGTF assays only became useful proxies when the variant spread and became more dominant in late November when the assays then detected over 90% of the variant26. Others have reached a similar conclusion8,19,20,22,23,27, suggesting that the success of SGTF assays depends on the location, time, and frequency of other variants that contain the ΔH69/ΔV70 deletion. This is particularly problematic, since the SGTF assays are the least accurate at the time when the B.1.1.7 variant is at low prevalence, precisely the time when an accurate test is needed most in order to establish effective mitigation strategies. Our test outlined here makes significant strides in this effort by accurately differentiating the B.1.1.7 variant with a test that does not rely on a SGTF, thus providing a rapid, accurate test that eliminates the need to conduct expensive and laborious sequencing to confirm lineage status.
Besides the SGTF tests, a number of commercially available SARS-COV-2 variant tests are emerging and have been used as surveillance strategies to monitor the prevalence of variants such as B.1.1.727,28,29,30,31,32. These tests are largely based on classical SNP genotyping methods using either probe-based genotyping or melting curve analyses and typically focus on mutations that are shared between many variants (e.g., N501Y, E484K, and ΔH69/ΔV70 deletion), making it difficult to distinguish between variants unless running multiple SNP assays and then making complex comparisons of melt curves. Similar to SGTF tests, these approaches, while providing a rapid snapshot of the presence of SARS-CoV-2 variants, often require follow up genomic sequencing to identify the particular variant.
Several groups have described publicly available RT-qPCR protocols for detection of lineage B.1.1.7 that can be divided into SNP genotyping assays using either SYBR33 or probe-based34 melting curve analyses, multiplexed probe-based RT-qPCR35,36,37,39, and a combination of target drop-out tests40. While these open source RT-qPCR protocols offer cost-effective, rapid strategies to directly detect multiple SARS-CoV-2 variants, some are limited by only assessing a small number of mutations that preclude identification of specific variants and most have yet to be tested in real world surveillance scenarios.
To differentiate B.1.1.7, we took an alternative approach by targeting both the ΔH69/ΔV70 and ΔY144 deletions using allele-specific PCR methods combined with judicious placement of LNA oligonucleotides. Together, these modifications provided us with a primer/probe set that retained specificity for B.1.1.7 variants and reduced specificity to other variants containing only the ΔH69/ΔV70 deletion. To highlight the specificity of this assay, our analysis of all GISAID sequences containing both the ΔH69/ΔV70 and ΔY144 deletions revealed that a staggering 99.52% of all these sequences belong to lineage B.1.1.7, ensuring that users can have high confidence that a positive B.1.1.7 assay result is a true positive. Our test, instead of relying on target failures to identify putative variants, provides a positive signal in the presence of B.1.1.7 and ΔH69/ΔV70 deletion variants that can easily be differentiated by comparing their relative Ct values to a common SARS-CoV-2 S gene primer/probe set that serves as a benchmark.
Since this test depends on a relative comparison of Ct values between the B.1.1.7 and common SARS-CoV-2 S gene assays (i.e., B.1.1.7 positive samples must amplify within 5 Ct cycles of the common SARS-CoV-2 S gene), it is important that samples have sufficient viral load to ensure accurate interpretation. For low viral load samples (e.g. Ct > 35), accurate detection may be compromised due to the constraints required by the relative Ct comparison as well as the assay’s limit of detection. This caveat, however, is less stringent than the viral load constraints needed to successfully sequence SARS-CoV-2 samples, which in practice require samples with Ct ≤ 30.
We successfully monitored the dynamics of lineage B.1.1.7 prevalence by retesting nearly 7,000 SARS-CoV-2 positive samples in three successive testing campaigns in Slovakia. This mass surveillance effort provided invaluable information about the spread and prevalence of lineage B.1.1.7 without having to conduct expensive and time-consuming genomic sequencing. Although our observed data did not fit models of previously established replication numbers for lineage B.1.1.76,8, we attribute this discrepancy to region specific presence of other competing SARS-CoV-2 variants. Indeed, a recently described B.1.258 variant that was extensively circulating throughout the Czech Republic and Slovakia21 contains mutations in the spike protein (N439K and ΔH69/ΔV70 deletion) that result in higher viral loads and increased transmissibility7,21,40. It is plausible that the reproduction number of B.1.1.7 is altered in a time and region-dependent manner that is associated with circulation of B.1.258.
The B.1.1.7 RT-qPCR assay described here was also used to screen for B.1.1.7 prevalence in 122 SARS-CoV-2 positive samples in the city of Trenčín, Slovakia in December 2020. While we observed 81–85% prevalence of B.1.1.7 in the region of Trenčín in February 2021, Brejová et al.21 reported only 4% prevalence of B.1.1.7 and 41% prevalence of variants containing only the ΔH69/ΔV70 deletion back in December 2020. This highlights two key points: (1) when considering the B.1.1.7 prevalence in Trenčín in December 2020, the extrapolated historical data using estimated reproduction numbers matches our observed prevalence seen in Trenčín region on February 2nd, 2021 (Fig. 3d). (2) SGTF tests utilized early on in a scenario like Trenčín would result in many false positive B.1.1.7 samples. Overall, these data provide real-world evidence of how this B.1.1.7 RT-qPCR assay can be used in mass surveillance screening to capture critical epidemiological information about the dynamics of B.1.1.7. It is also important to note that the outcome of the B.1.1.7 RT-qPCR assay-based screening and the observed trend is greatly in line with the sequence data from Slovakia available in the GISAID repository (https://www.gisaid.org/). From the clinical samples collected in Slovakia in February 2021, 83.8% (n = 210) were identified as B.1.1.7 lineage while in the samples from March 2021, 97.1% (n = 1,336) belonged to the B.1.1.7 lineage.
Although the assays described here can accurately detect and differentiate the B.1.1.7 variant, a limitation is that it does not detect other emerging variants of concern (VOCs) such as B.1.351 (Beta), P.1 (Gamma), and B.1.617.2 (Delta). This is particularly important in geographical regions where B.1.1.7 is not prevalent or is being superseded by other VOCs. An important future objective will be to design additional assays that could be multiplexed or used in parallel with our B.1.1.7 assay to detect other VOCs (or mutations of concern). These panels could be tailored to specific geographical regions to provide rapid snapshots of VOC prevalence and their dynamics over time in the absence of sequencing. Alternatively, these panels could be used to quickly identify putative variant samples that can be marked for targeted sequencing. As an example of this approach, we recently developed an additional assay targeting the ORF1a (nsp6) ΔS3675/ΔG3676/ΔF3677 deletion that is shared by B.1.1.7, B.1.351, and P.1. By multiplexing this assay with our B.1.1.7 assay, we have developed a multivariant test that can differentiate B.1.1.7 from B.1.351/P.1 (rTEST COVID-19 qPCR Multivariant kit; MultiplexDX) through simply verifying the presence or absence of either the ΔH69/ΔV70 deletion, or ΔS3675/ΔG3676/ΔF3677 deletion, or both deletions. A similar approach utilizing drop out target assays for the same deletions has been used to distinguish multiple variants40.
Although the main use of this assay is to directly detect the B.1.1.7 variant, the multiplexed SARS-CoV-2 S gene and RNase P assay could also be used as an affordable and ultrasensitive diagnostic test. Indeed, with an ultrasensitive LoD of only 0.4 copies/μl, this assay is among the most sensitive open-source and commercial tests with EUA approval41. This notion is in accordance with several independent comparisons of open-source and commercially available SARS-CoV-2 tests that show our S gene/RNase P assay is a highly sensitive test42,42,43,44,46. Given that most open-source protocols either require multiple singleplex reactions and/or lack quality control assays, our multiplexed S gene/RNase P assay can provide a streamlined, affordable, and ultrasensitive alternative to currently available open-source and commercial SARS-CoV-2 diagnostic tests.
We have provided interested users with the primer and probe sequences to implement this B.1.1.7 assay in their own laboratories with the hope this can rapidly scale the ability of countries to identify the B.1.1.7 variant and implement epidemiological measures to mitigate its spread. This test can provide labs with a powerful tool to directly confirm the presence of the B.1.1.7 variant in a sample previously determined SARS-CoV-2 positive by an approved screening test, thus avoiding the use of target gene failure assays that can be plagued with low specificity and obviating the need to conduct burdensome and costly genomic sequencing. This is particularly important for countries that are experiencing extensive circulation of variants harbouring only the ΔH69/ΔV70 deletion as current RT-qPCR assays that rely on SGTFs erroneously classify these samples as presumptive B.1.1.7 variants.
Materials and methods
Identification of RT-qPCR targets by bioinformatic analysis
To identify suitable targets for primer/probe design, we downloaded 1,136 sequences from the GISAID repository filtered during a collection time spanning 1—21 December 2020. We focused on the spike gene because lineage B.1.1.7 contains a number of spike gene mutations, including two deletions (ΔH69/ΔV70 and ΔY144) that are ideal for designing a specific assay. We cut the locus encoding the spike protein and used the MAFFT alignment tool (with the parameter—auto)47 to align all the sequences against the WUHAN reference (NCBI ID: NC_045512.2). Twelve sequences (1.06%) contained ambiguous signal in the loci of deletions and were not used in the downstream analysis. We separated sequences into two groups: (1) those with the ΔH69/ΔV70 and ΔY144 deletions and (2) those without the deletions (Supplementary Table S1). Using SeaView48, we called 95% consensus sequences for the ΔH69/ΔV70 and ΔY144 group and the No deletions group that were subsequently used to design primer and probe sets specific to either B.1.1.7 or all other SARS-CoV-2 variants, respectively.
In a separate analysis to determine the prevalence of the ΔH69/ΔV70 and ΔY144 deletions in lineages other than B.1.1.7, we used the multiple sequence alignment (MSA) dataset from GISAID and the metadata file containing 922,292 sequences (of which 922,190 were determined to be unique) collected from the beginning of the pandemic through 6 April 2021. Using custom python scripts, we searched at the nucleotide level for loci with both ΔH69/ΔV70 and ΔY144 deletions and sorted hits according to Pangolin lineage ID. All commands and scripts are available here: https://github.com/MultiplexDX/B117-RT-qPCR-design/blob/main/B1117.ipynb.
Primer design and synthesis
We designed primers and probes using the 95% consensus sequences to target the S gene of the common SARS-CoV-2 (called SARS-CoV-2 S gene assay). To differentiate the B.1.1.7 variant from all other SARS-CoV-2 variants, we also designed primers and probes to target the S gene of SARS-CoV-2 variants containing either the ΔH69/ΔV70 deletion or the ΔY144 deletion, or both deletions (called B.1.1.7 assay). As an internal control, we synthesized a primer/probe set for human RNase P published by the US CDC17. We incorporated locked nucleic acid (LNA)-modified bases into some primers and probes following general guidelines in order to normalize melting temperatures, increase sensitivity, and enhance specificity49,49,51. Following primer/probe design, we conducted in silico analyses using the IDT OligoAnalyzer™ tool (https://www.idtdna.com/pages/tools/oligoanalyzer) to verify melting temperature (Tm), GC content, and potential to form homo-/hetero-dimers as well as the mFold server52 (http://www.bioinfo.rpi.edu/applications/mfold/) to identify problematic secondary structures or necessary hairpin formation for TaqMan probes. Probes for both SARS-CoV-2 S gene and B.1.1.7 were labelled with a 5’-FAM (6-carboxyfluorescein) reporter dye and 3’-BHQ-1 (black hole quencher 1) dye. In multiplexed reactions, the probe for human RNase P was labelled with a 5’-Cy5 (cyanine 5) reporter dye and 3’-BHQ-3 dye. Primers and probes were synthesized at MultiplexDX, s.r.o. (Bratislava, Slovakia; https://www.multiplexdx.com/). The sequences of primers and probes used in this study are listed in Supplementary Table S2. This test is also available as an in vitro diagnostic (IVD) CE marked kit called rTEST COVID-19 B.1.1.7 qPCR kit (https://www.multiplexdx.com/products/rtest-covid-19-b-1-1-7-qpcr-kit, MultiplexDX, s.r.o.).
Positive controls
For primer/probe set optimization, we used the following positive controls: (1) RNA extracted from a patient confirmed positive for a common variant of SARS-CoV-2 that does not contain any deletions in the spike gene (named wild type template), (2) RNA extracted from a patient confirmed positive for a common variant of SARS-CoV-2 that contains the six base pair deletion (bp: 21,765–21,770) resulting in the deletion of two amino acids at the 69/70 position of the spike protein (named ΔH69/ΔV70 template), and (3) RNA extracted from a patient confirmed positive by whole genome sequencing for the SARS-CoV-2 lineage B.1.1.7 (named B.1.1.7 template). The SARS-CoV-2 control samples were confirmed by whole genome sequencing of tiled ~ 2-kbp long amplicons on a MinION device (Oxford Nanopore Technologies, Oxford, UK) essentially as described by Resende et al.53.
RT-qPCR
We optimized RT-qPCR reactions and conducted clinical validations using both an AriaMx (Agilent, CA, USA) and QuantSudio 5 (ThermoFisher Scientific, MA, USA) real-time PCR system. For all the detected genes, we used the SOLIScript 1-step CoV Kit (Cat. No. 08-65-00250, SOLIS BioDyne, Tartu, Estonia) according to the manufacturer’s recommendations comprised of 4 µl of 5× One-step Probe CoV Mix (ROX), 0.5 µl of 40× One-step SOLIScript CoV Mix, 2 µl of primers/probe mix, 8.5 µl of PCR water, and 5 µl of sample in a 20 µl total volume. One-step RT-qPCR assays were conducted with the following cycling conditions: 55 °C for 10 min for reverse transcription, 95 °C for 10 min for initial denaturation, and 45 cycles of 95 °C for 15 s and 60 °C for 30 s. Concentrations for primers and probes were as follows: SARS-CoV-2 S gene (forward and reverse primer = 500 nM, probes = 200 nM for each probe (single and dual); B.1.1.7: forward primer = 600 nM, reverse primer = 800 nM, probes = 200 nM for each probe (single and dual); RNase P (forward and reverse primer = 250 nM, probe = 80 nM). We used the rTEST COVID-19 qPCR Allplex kit (MultiplexDX) as the reference standard test. This kit utilizes the same master mix and thermocycling conditions as the SARS-CoV-2 S gene and B.1.1.7 assays and contains a single multiplexed reaction targeting the SARS-CoV-2 E and RdRP genes as well as human RNase P.
Analytical sensitivity (limit of detection)
To assess the analytical sensitivity of both our common SARS-CoV-2 S gene (S gene) and B.1.1.7 primer/probe sets, we used RNA isolated from a patient sample infected with the B.1.1.7 variant of SARS-CoV-2 as confirmed by sequencing. This RNA was diluted to 200 copies/μl and then serial dilutions were prepared by diluting the stock with a synthetic matrix “SARS-CoV-2 Negative” (Cat. No. COV000, Exact Diagnostics, TX, USA) containing genomic DNA at a concentration of 75,000 copies/ml, resulting in samples with concentrations of 8 copies/μl (= 40 copies/reaction), 2 copies/μl (= 10 copies/reaction), 0.8 copies/μl (= 4 copies/reaction), 0.4 copies/μl (= 2 copies/reaction) and 0.2 copies/μl (= 1 copy/reaction) that were used in the analytical sensitivity test. The assay was performed in 8 replicates for each prepared dilution.
Clinical performance evaluation
We evaluated the clinical utility of our SARS-CoV-2 S gene and B.1.1.7 primer/probe sets using a selected set of 106 clinical samples, which were collected during December 2020 and January 2021 and confirmed by an RT-qPCR reference method used for routine testing by regional public health authorities of the Slovak Republic. Further sequencing revealed 67 of these samples belonging to the B.1.1.7 lineage, 24 samples belonging to the B.1.258 lineage (contains only the ΔH69/ΔV70 deletion), and 15 samples belonging to other SARS-CoV-2 lineages. The SARS-CoV-2 sequences were determined by sequencing of tiled ~ 2-kbp long amplicons on a MinION device (Oxford Nanopore Technologies, Oxford, UK) as described by Resende et al.53. We also assessed the specificity of our SARS-CoV-2 S gene and B.1.1.7 primer/probe sets by testing 94 samples that were previously classified as SARS-CoV-2 negative. To investigate potential cross-reactivity to other respiratory pathogens, we tested both assays on a battery of respiratory pathogen panels (AmpliRun PCR controls; Vircell Microbiologists) that included complete genomic RNA from Coronavirus OC43 (Cat. No. MBC135-R), Coronavirus (Cat. No. MBC090), Coronavirus SARS (2003; Cat. No. MBC136-R), MERS Coronavirus (Cat. No. MBC132), Influenza A H1N1 (Cat. No. MBC028), Novel Influenza A H1N1 (Cat. No. MBC082), Influenza A H3N2 (Cat. No. MBC029), Influenza A H5N1 (Cat. No. MBC052), Influenza B (Cat. No. MBC030), Human parainfluenza 1 (Cat. No. MBC105), Respiratory syncytial virus subtype A (Cat. No. MBC041), and Rhinovirus (Cat. No. MBC091). All respiratory pathogen panels and positive and negative controls were ran in triplicate.
To ensure our clinical validation was sufficiently powered given the sample size, we conducted a post-hoc sample size estimate using a previously described approach for assessing diagnostic sensitivity and specificity54. The calculation contained the following parameters: expected sensitivity = 0.96; expected specificity = 0.95; prevalence of disease (p) = 0.25; precision (± expected) = 0.10; confidence level 100(1 − α) = 95%; expected drop out rate = 5%. This sample size estimate calculated a sample size for sensitivity, nsen = 64 (with 5% dropout) and a sample size for specifity, nspec = 25, or a total of 89 clinical samples. Therefore, our clinical evaluation of 106 SARS-CoV-2 positive samples, of which 67 samples were classified as B.1.1.7 and 39 samples classified as other lineages, and 94 SARS-CoV-2 negative samples was sufficiently powered.
We conducted a detailed assessment of potential biases and applicability judgements of the clinical validation using the QUADAS-2 tool55 (http://www.bristol.ac.uk/population-health-sciences/projects/quadas/quadas-2/; Supplementary Table S3). Inclusion criteria for the selected set of samples consisted of a positive result from a reference standard RT-qPCR test as well as available sequencing information to confirm lineage.
The clinical validation was conducted by the Biomedical Research Center, Institute of Virology, Slovak Academy of Sciences (BMC SAS). BMC SAS received clinical samples previously identified as SARS-CoV-2 positive by local laboratories, then extracted RNA and performed the reference standard test (rTEST COVID-19 qPCR Allplex kit; MultiplexDX) and the B.1.1.7 test in parallel. All samples were processed and tested in a timely manner to minimize the effects of RNA degradation. For the clinical evaluation, researchers used a prespecified criterion to interpret test results (Supplementary Table S4) and were blind to the sequencing outcome. The results from the B.1.1.7 assay were compared with sequencing outcome to determine the clinical sensitivity, specificity, and positive and negative likelihood ratios, which were calculated using MedCalc’s free online diagnostic test evaluation calculator (for definitions of formulas see, https://www.medcalc.org/calc/diagnostic_test.php)56. Estimates of the prevalence of B.1.1.7 and B.1.258 were derived from sequencing data available in Slovakia during December 2020 and January 2021 and were used to calculate positive and negative predictive values and accuracy. The results of the index test were not made available to the experimenters evaluating the reference standard or sequencing results. Reporting of the clinical evaluation of our B.1.1.7 RT-qPCR test is in accordance with STARD reporting guidelines (Supplementary Table S5).
All experiments were reviewed and approved by the Ethics committee of the Biomedical research Center of the Slovak Academy of Sciences, Bratislava, Slovakia (Ethics committee statement No. EK/BmV-02/2020) and were performed according to their regulations and guidelines. Informed consent was obtained from all subjects.
Surveillance of lineage B.1.1.7 prevalance throughout the Slovak Republic
This test (rTEST COVID-19 B.1.1.7 qPCR kit) was used to assess the prevalence of B.1.1.7 throughout the Slovak Republic over a period of 1 month. Multiple laboratories of the Public Health Authority of the Slovak Republic retested 6,886 samples that were identified as SARS-CoV-2 positive by a standard RT-qPCR test. Retesting occurred over a one month period on February 2nd, 2021 (1,962 samples), February 17th, 2021 (2,382 samples), and March 3rd, 2021 (2,542 samples). To ensure sufficient sample size for smaller geographic regions, we grouped districts based on the jurisdictions of the regional public health offices (there are 36 public health offices each covering 1–8 districts) and distributed tests accordingly. Laboratory personnel determined lineage status using the predefined criteria outlined in Supplementary Table S4. For comparison with our observed B.1.1.7 prevalences, we also used the prevalences obtained on the first screening round (February 2nd, 2021) to estimate historical and future prevalences using a range of 2 weeks and applying spread factors (3.3 and 5.4) that were derived from estimated reproduction numbers from the UK6,8. Data from the surveillance screening can be found on GitHub: https://github.com/Institut-Zdravotnych-Analyz/covid19-data/tree/main/PCR_Tests.
Data availability
Raw data from the clinical validation as well as the names and accession ID of sequences uploaded to GISAID are provided in Supplementary Table S7. All commands and scripts for bioinformatic analyses of GISAID sequences are available here: https://github.com/MultiplexDX/B117-RT-qPCR-design/blob/main/B1117.ipynb. Data from the surveillance screening can be found on GitHub: https://github.com/Institut-Zdravotnych-Analyz/covid19-data/tree/main/PCR_Tests and in Supplementary Table S8.
References
Rambaut, A. et al. Preliminary Genomic Characterisation of an Emergent SARS-CoV-2 Lineage in the UK Defined by a Novel Set of Spike Mutations. Virological (2020). https://virological.org/t/preliminary-genomic-characterisation-of-an-emergent-sars-cov-2-lineage-in-the-uk-defined-by-a-novel-set-of-spike-mutations/563. Accessed 13 January 2021.
GISAID, EpiCoV Data Curation Team. GISAID—UK Reports New Variant, Termed VUI 202012/01. https://www.gisaid.org/references/gisaid-in-the-news/uk-reports-new-variant-termed-vui-20201201/. Accessed 18 January 2021
Luan, B., Wang, H. & Huynh, T. Enhanced binding of the N501Y-mutated SARS-CoV-2 spike protein to the human ACE2 receptor: Insights from molecular dynamics simulations. FEBS Lett. https://doi.org/10.1002/1873-3468.14076 (2021).
Starr, T. N. et al. Deep mutational scanning of SARS-CoV-2 receptor binding domain reveals constraints on folding and ACE2 binding. Cell 182, 1295–1310 (2020).
Davies, N. G. et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science 372, 112 (2021).
Grabowski, F., Preibisch, G., Giziński, S., Kochańczyk, M. & Lipniacki, T. SARS-CoV-2 variant of concern 202012/01 has about twofold replicative advantage and acquires concerning mutations. Viruses 13, 392 (2021).
Meng, B. et al. Recurrent emergence of SARS-CoV-2 spike deletion H69/V70 and its role in the Alpha variant B.1.1.7. Cell Rep. 35, 109292 (2021).
Volz, E. et al. Transmission of SARS-CoV-2 lineage B.1.1.7 in England: Insights from linking epidemiological and genetic data. MedRxiv 37, 1530. https://doi.org/10.1101/2020.12.30.20249034 (2021).
Golubchik, T. et al. Early analysis of a potential link between viral load and the N501Y mutation in the SARS-COV-2 spike protein. MedRxiv. https://doi.org/10.1101/2021.01.12.20249080 (2021).
Kidd, M. et al. S-variant SARS-CoV-2 lineage B.1.1.7 is associated with significantly higher viral load in samples tested by TaqPath polymerase chain reaction. J. Infect. Dis. 223, 1666. https://doi.org/10.1093/infdis/jiab082 (2021).
Horby, P. et al. NERVTAG Paper on COVID-19 Variant of Concern B.1.1.7 (2021).
Yip, S. P. et al. Use of dual TaqMan probes to increase the sensitivity of 1-step quantitative reverse transcription-PCR: Application to the detection of SARS coronavirus. Clin. Chem. 51, 1885–1888 (2005).
Nagy, A. et al. Evaluation of TaqMan qPCR system integrating two identically labelled hydrolysis probes in single assay. Sci. Rep. 7, 41392 (2017).
Gibbs, R. A., Nguyen, P. N. & Caskey, C. T. Detection of single DNA base differences by competitive oligonucleotide priming. Nucleic Acids Res. 17, 2437–2448 (1989).
Tsai, M. Y., Hanson, N. Q., Copeland, K. R., Beheshti, I. & Garg, U. Determination of a T/G polymorphism at nucleotide 3206 of the apolipoprotein C III gene by amplification refractory mutation system. Clin. Chem. 40, 2235–2239 (1994).
Lefever, S., Pattyn, F., Hellemans, J. & Vandesompele, J. Single-nucleotide polymorphisms and other mismatches reduce performance of quantitative PCR assays. Clin. Chem. 59, 1470–1480 (2013).
Centers for Disease Control and Prevention. Research Use Only 2019-Novel Coronavirus (2019-nCoV) Real-Time RT-PCR Primers and Probes (2020). https://www.cdc.gov/coronavirus/2019-ncov/lab/rt-pcr-panel-primer-probes.html. Accessed 4 February 2021
Bal, A. et al. Two-step strategy for the identification of SARS-CoV-2 variant of concern 202012/01 and other variants with spike deletion H69–V70, France, August to December 2020. Eurosurveillance 26, 2100008 (2021).
Larsen, B. B. & Worobey, M. Identification of a Novel SARS-CoV-2 Spike 69–70 Deletion Lineage Circulating in the United States—SARS-CoV-2 coronavirus/SARS-CoV-2 Molecular Evolution. Virological (2020). https://virological.org/t/identification-of-a-novel-sars-cov-2-spike-69-70-deletion-lineage-circulating-in-the-united-states/577. Accessed 29 January 2021
Moreno, G. et al. Detection of Non-B.1.1.7 Spike ∆69/70 Sequences (B.1.375) in the United States—SARS-CoV-2 coronavirus/nCoV-2019 Genomic Epidemiology. Virological (2021). https://virological.org/t/detection-of-non-b-1-1-7-spike-69-70-sequences-b-1-375-in-the-united-states/587. Accessed 4 February 2021
Brejová, B. et al. A SARS-CoV-2 mutant from B.1.258 lineage with ∆H69/∆V70 deletion in the Spike protein circulating in Central Europe in the fall 2020. Virus Genes. https://doi.org/10.1007/s11262-021-01866-5 (2021).
Alpert, T. et al. Early introductions and transmission of SARS-CoV-2 variant B117 in the United States. Cell 184, 2595. https://doi.org/10.1016/j.cell.2021.03.061 (2021).
Gaymard, A. et al. Early assessment of diffusion and possible expansion of SARS-CoV-2 Lineage 20I/501Y.V1 (B.1.1.7, variant of concern 202012/01) in France, January to March 2021. Eurosurveillance 26, 2100133 (2021).
Washington, N. L. et al. S gene dropout patterns in SARS-CoV-2 tests suggest spread of the H69del/V70del mutation in the US. MedRxiv. https://doi.org/10.1101/2020.12.24.20248814 (2020).
Younes, M. et al. B.1.1.7 became the dominant variant in Lebanon. MedRxiv 5, 1403. https://doi.org/10.1101/2021.03.17.21253782 (2021).
Variant Technical Group. Investigation of novel SARS-CoV-2 variant: Variant of concern 202012/01. Technical briefing 4. Public Health England (2021). https://www.gov.uk/government/publications/investigation-of-novel-sars-cov-2-variant-variant-of-concern-20201201 (Accessed 28 January 2021).
Chen, C. et al. Quantification of the spread of SARS-CoV-2 variant B117 in Switzerland. MedRxiv 593, 7858. https://doi.org/10.1101/2021.03.05.21252520 (2021).
Haim-Boukobza, S. et al. Rapid SARS-CoV-2 variants spread detected in France using specific RT-PCR testing. MedRxiv. https://doi.org/10.1101/2021.02.20.21251927 (2021).
Durner, J. et al. Fast and cost-effective screening for SARS-CoV-2 variants in a routine diagnostic setting. Dent. Mater. 37, e95–e97 (2021).
Cabecinhas, A. R. G. et al. SARS-CoV-2 N501Y introductions and transmissions in Switzerland from beginning of October 2020 to February 2021—Implementation of Swiss-wide diagnostic screening and whole genome sequencing. MedRxiv. https://doi.org/10.1101/2021.02.11.21251589 (2021).
Korukluoglu, G. et al. 40 minutes RT-qPCR assay for screening spike N501Y and HV69-70del mutations. BioRxiv. https://doi.org/10.1101/2021.01.26.428302 (2021).
Matic, N. et al. Rapid detection of SARS-CoV-2 variants of concern identifying a cluster of B.1.1.28/P1 variant in British Columbia, Canada. MedRxiv 70, 95. https://doi.org/10.1101/2021.03.04.21252928 (2021).
Sater, F. A., Younes, M., Nassar, H., Nguewa, P. & Hamze, K. A rapid and low-cost protocol for the detection of B.1.1.7 lineage of SARS-CoV-2 by using SYBR green-based RT-qPCR. MedRxiv. https://doi.org/10.1101/2021.01.27.21250048 (2021).
Banada, P. et al. A simple RT-PCR Melting temperature assay to rapidly screen for widely circulating SARS-CoV-2 variants. MedRxiv. https://doi.org/10.1101/2021.03.05.21252709 (2021).
Nörz, D. et al. Evaluation of a fully automated high-throughput SARS-CoV-2 multiplex qPCR assay with built-in screening functionality for del-HV69/70- and N501Y variants such as B.1.1.7. J. Clin. Virol. 141, 104894 (2021).
Vogels, C.B.F. et al. Multiplex qPCR discriminates variants of concern to enhance global surveillance of SARS-CoV-2. PLoS Biol. 19, e3001236. https://doi.org/10.1371/journal.pbio.3001236 (2021).
Yaniv, K., Ozer, E., Plotkin, N., Bhandarkar, N. S. & Kushmaro, A. RT-qPCR assay for detection of British (B.1.1.7) and South Africa (B.1.351) variants of SARS-CoV-2. MedRxiv. 9, 1900. https://doi.org/10.1101/2021.02.25.21252454 (2021).
Wurtzer, S. et al. Monitoring the propagation of SARS CoV2 variants by tracking identified mutation in wastewater using specific RT-qPCR. MedRxiv. https://doi.org/10.1101/2021.03.10.21253291 (2021).
Perchetti, G. A., Nalla, A. K., Huang, M.-L., Jerome, K. R. & Greninger, A. L. Multiplexing primer/probe sets for detection of SARS-CoV-2 by qRT-PCR. J. Clin. Virol. 129, 104499 (2020).
Thomson, E. C. et al. Circulating SARS-CoV-2 spike N439K variants maintain fitness while evading antibody-mediated immunity. Cell. https://doi.org/10.1016/j.cell.2021.01.037 (2021).
MacKay, M. J. et al. The COVID-19 XPRIZE and the need for scalable, fast, and widespread testing. Nat. Biotechnol. 38, 1021–1024 (2020).
Freire-Paspuel, B. & Garcia-Bereguiain, M. A. Analytical and clinical evaluation of “AccuPower SARS-CoV-2 Multiplex RT-PCR kit (Bioneer, South Korea)” and “Allplex 2019-nCoV assay (Seegene, South Korea)” for SARS-CoV-2 RT-PCR diagnosis: Korean CDC EUA as a quality control proxy for developing countries. Front. Cell. Infect. Microbiol. https://doi.org/10.3389/fcimb.2021.630552 (2021).
Freire-Paspuel, B. & Garcia-Bereguiain, M. A. Clinical performance and analytical sensitivity of three SARS-CoV-2 nucleic acid diagnostic tests. Am. J. Trop. Med. Hyg. 104, 1516 (2021).
Nalla, A. K. et al. Comparative performance of SARS-CoV-2 detection assays using seven different primer-probe sets and one assay kit. J. Clin. Microbiol. https://doi.org/10.1128/JCM.00557-20 (2020).
Wang, X. et al. Limits of detection of 6 approved RT–PCR kits for the novel SARS-coronavirus-2 (SARS-CoV-2). Clin. Chem. https://doi.org/10.1093/clinchem/hvaa099 (2020).
Vogels, C. B. F. et al. Analytical sensitivity and efficiency comparisons of SARS-CoV-2 RT–qPCR primer–probe sets. Nat. Microbiol. 5, 1299–1305 (2020).
Nakamura, T., Yamada, K. D., Tomii, K. & Katoh, K. Parallelization of MAFFT for large-scale multiple sequence alignments. Bioinformatics 34, 2490–2492 (2018).
Gouy, M., Guindon, S. & Gascuel, O. SeaView version 4: A multiplatform graphical user interface for sequence alignment and phylogenetic tree building. Mol. Biol. Evol. 27, 221–224 (2010).
McTigue, P. M., Peterson, R. J. & Kahn, J. D. Sequence-dependent thermodynamic parameters for locked nucleic acid (LNA)−DNA duplex formation. Biochemistry 43, 5388–5405 (2004).
Latorra, D., Arar, K. & Michael Hurley, J. Design considerations and effects of LNA in PCR primers. Mol. Cell. Probes 17, 253–259 (2003).
Levin, J. D., Fiala, D., Samala, M. F., Kahn, J. D. & Peterson, R. J. Position-dependent effects of locked nucleic acid (LNA) on DNA sequencing and PCR primers. Nucleic Acids Res. 34, e142 (2006).
Zuker, M. Mfold web server for nucleic acid folding and hybridization prediction. Nucleic Acids Res. 31, 3406–3415 (2003).
Resende, P. C. et al. SARS-CoV-2 genomes recovered by long amplicon tiling multiplex approach using nanopore sequencing and applicable to other sequencing platforms. BioRxiv. https://doi.org/10.1101/2020.04.30.069039 (2020).
Buderer, N. M. Statistical methodology: I. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad. Emerg. Med. 3, 895–900 (1996).
Whiting, P. F. et al. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 155, 529–536 (2011).
MedCalc Software Ltd. Diagnostic Test Evaluation Calculator. https://www.medcalc.org/calc/diagnostic_test.php (Accessed 19 July 2021).
Acknowledgements
We gratefully acknowledge the authors from the submitting and originating laboratories that shared genetic sequencing data with the GISAID initiative. We acknowledge the contribution of the oligonucleotide synthesis and production team at MultiplexDX for synthesizing the primers and probes in this study, the laboratory staff of the Slovak regional public health authorities and diagnostic laboratories for screening samples during surveillance of B.1.1.7, and the team at the Institute for Healthcare Analyses for processing the surveillance data. Surveillance of lineage B.1.1.7 using MuliplexDX tests was funded by the Ministry of Health of Slovakia. This project was supported by the European Union’s Horizon 2020 research and innovation program [EVA-GLOBAL project, grant agreement number 871029] (BK) and grants from the Slovak Research and Development Agency: PP-COVID-20-0017 (BK) and PP-COVID-20-0116 (PC, BK). The funding sources had no role in the design and conduct of the study, interpretation of the data, writing of the manuscript, and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
B.K., P.C., V.K., K.B., M.M. and E.D.P. conceptualized and planned the study. V.K. conducted bioinformatic analyses for primer/probe design and inclusivity. P.C. designed and synthesized primers/probes. M.R., R.H., K.B. and V.C. optimized primer/probe sets on positive controls and clinical samples. A.B., L.Ro., M.K., A.L., L.M., M.S., L.Re., E.N., P.S. and A.K. collected and provided clinical samples and associated metadata. K.B., V.C., B.B., J.N. and T.V., performed genomic sequencing and bioinformatics to determine sample lineage status. B.K., K.B., V.C., M.S., M.L. and L.L. performed clinical validation and analysed clinical data. M.M. and E.S. collected and evaluated samples from the B.1.1.7 lineage surveillance and analysed the data. E.D.P., M.M., B.K. and P.C. verified the underlying data. E.D.P., B.K., P.C., M.M., E.S., V.K., M.R., R.H. and K.B. analysed and interpreted the data and wrote the manuscript. All authors had full access to the data, provided critical comments and feedback on the manuscript, and accept responsibility to submit the manuscript for publication.
Corresponding authors
Ethics declarations
Competing interests
VK, EDP, MR, RH, and PC are employees of MultiplexDX, a biotechnology company which has commercialized a kit called rTEST COVID-19 B.1.1.7 qPCR kit (https://www.multiplexdx.com/products/rtest-covid-19-b-1-1-7-qpcr-kit, MultiplexDX, Inc., Bratislava, Slovakia) that is based on this research. BK is a Head of the Department of Virus Ecology, Institute of Virology, Biomedical Research Center of the Slovak Academy of Sciences (BMC SAS). MM is a Head of the Insititute for healthcare analyses at the Slovak Ministy of Health. BMC SAS has entered into collaboration with MultiplexDX, Inc. for development and validation of RT-qPCR tests for routine detection of SARS-CoV-2 and the test for detection of B.1.1.7 variant described in this study. The Ministry of Health procured said tests for the B.1.1.7 lineage surveillance. All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boršová, K., Paul, E.D., Kováčová, V. et al. Surveillance of SARS-CoV-2 lineage B.1.1.7 in Slovakia using a novel, multiplexed RT-qPCR assay. Sci Rep 11, 20494 (2021). https://doi.org/10.1038/s41598-021-99661-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99661-7
This article is cited by
-
Development of multiplex allele-specific RT-qPCR assays for differentiation of SARS-CoV-2 Omicron subvariants
Applied Microbiology and Biotechnology (2024)
-
Vivid COVID-19 LAMP is an ultrasensitive, quadruplexed test using LNA-modified primers and a zinc ion and 5-Br-PAPS colorimetric detection system
Communications Biology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.