Abstract
An update on the trends in maxillofacial traumatology provides additional information on the actual and changing needs. This retrospective study aimed to review all patient records of patients treated for isolated midface fractures in the Department of Cranial- and Maxillofacial Surgery at the Dortmund General Hospital between 2007 and 2017. The patient radiographs and patient files were reviewed. The safety and efficacy of the applied methods were controlled by assessing complications based on the Clavien-Dindo classification system. The statistical analysis included descriptive methods including regression analysis and χ2-test. In eleven years, 3474 isolated midface fracture sites have been identified in 2868 patients. The yearly trend is slightly increasing, in elderly clearly worsening, in children and youth decreasing. The male-to-female ratio was 2.16:1 for the whole study population, in the age group 18–25 y.o. 6.95:1 while in elderly above 80 y.o. 1:2.51, the age group specific incidence reflects this result, too. The most common fractures were nasal bone fractures (1405), zygomatic fractures (832) and orbital floor fractures (700). The average hospital stay was 2.7 days, the most fractures were operated within 24 h. The complication rate was 2.02% (Clavien-Dindo class II–V). The incidence of midfacial fractures is increasing in the total population and especially in elderly, but decreasing in children. Development of injury prevention measures is needed in this population. The diagnostic and therapeutic procedures are appropriate, as there is a low complication rate and short inpatient stay observed.
Similar content being viewed by others
Introduction
The head and face are exposed to injuries. Facial fractures are common injuries as results of road traffic accidents, falls, interpersonal violence, sports or work-related accidents1,2,3,4,5,6,7. The most common fractures are nasal bone fractures6. Upper jaw fractures, on the other hand, are common in high-energy trauma, therefore often as part of panfacial fractures8. The number of cases of isolated fractures of the central midface (except for the isolated nasal bone fractures, which occur most frequently) is reported in these papers as significantly lower.
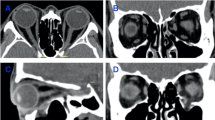
The development of diagnostics and treatment of midface fractures have been an important topic since 1895 the introduction of the first osteosynthesis system by Lane9 and 1896 the first dental radiograph by Walkhoff10. After decades of development, computed tomography (CT) became the “gold standard” for diagnostics, even three dimensional virtual applications are used after 200011,12. Different osteosynthesis materials, methods and implant designs have been introduced13. Titanium alloy implants have proven their superiority in osteosynthesis14,15,16. The latest improvements include digital workflows, usage of finite element methods and individual implant planning that allows more accurate diagnostics and osteosynthesis in maxillofacial surgery12,17,18.
Patient safety, treatment outcome and economic factors have become of increasing importance during these decades16,19,20,21,22. The complication rates after facial bone fractures are reported between 4.67 and 17%22. These have a negative impact on the length of hospital stay, operations in cases with complications generally take longer and patients are longer disabled and need much rehabilitation efforts to be able to return to normal life activites22. The removal of the osteosynthesis implants is a matter of discussion23, however, if a removal is indicated or requested by the patient, the best time to avoid implant osteointegration is 4–6 months time after surgery22.
Based on the continuously evolving knowledge, different fracture treatment guidelines have been established. The current and widely accepted fracture classification and treatment system is presented by the AO (AO Foundation, Clavadelerstrasse 8, 7270 Davos, Switzerland)24,25,26. This is the most comprehensive consensus guidline that has been implemented in maxillofacial traumatology. If these guidelines are correctly applied, the quality of patient care is good. This workflow is supported by good economic decisions and adequate management of patients and resources19,20,27,28,29,30. The continuous review of the treatment outcome provides feedback about treatment quality.
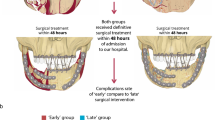
Figure 1 represents the summary of the workflow applied at the Department of Oral and Maxillofacial Surgery at Dortmund General Hospital. This workflow is based on actual literature and guidelines and is updated regularly. Patients are initially seen in the Outpatient Department of the Clinics or in the Interdisciplinary Emergency Room. After the initial assessment of injuries, a complex diagnostic procedure is completed to determine the therapeutic needs. After this, a treatment plan is prepared and the surgical therapy is carried out as soon as possible. Postoperatively antibiotics is administered (ampicillin-sulbactam 2 g/1 g iv. 3 times a day or clindamycin 600 mg 3 times a day in case of allergies), analgesics is adapted as per WHO-guidelines, cryotherapy is administered. The wound management is performed by trained personnel. In case of need, an early logopedic treatment or physiotherapy are applied. If needed, a further treatment in a rehabilitation unit is initiated. The emissions take place at least after 2 days after surgery, but this period is prolonged individually, if needed. Clinical examinations and radiographs are performed postoperatively. If a complication is diagnosed, the necessary therapy is addressed.
Postoperative follow-up visits are planned mostly 7–10 days after surgery. After less severe injuries, most patients are referred to a follow-up visit to the general practitioner’s or maxillofacial surgeon at the office. Complicated cases or patients with complications are referred to our Outpatient Department. Late complications are addressed in this phase of treatment as per need. As many follow-up visits take place, as needed. The removal of osteosynthesis implants (except for orbita meshes) is planned after 4–6 months time.
Our study aimed to retrospectively assess the safety and efficacy of the current treatment protocols and osteosynthesis procedure by analyzing patient cases with isolated midfacial fractures, who received inpatient care for their injuries at the Department for Oral- and Maxillofacial Surgery and Facial Plastic Surgery at General Hospital Dortmund between 01.01.2007 and 31.12.2017.
Materials and methods
The Ethics Commission of the University of Witten–Herdecke has approved this study (No. 152/2017).
This study was conducted in accordance with the Helsinki Declaration, the laws and regulations of the European Union, the Federal Republic of Germany, the State North-Rhine-Westfalia and the General Hospital Dortmund.
This study included patients with isolated midface fractures, who have been treated in our department from 1.1.2007 to 12.31.2017. All patients that had any other associated facial fractures have been excluded from this study. The initial patient examination is performed by the attending maxillofacial surgeon. If this is required, a close cooperation with the trauma surgeon, neurosurgeon or other specialities are round the clock available. If the attending surgeon is not yet a specialist, a specialist support is also always available. Patients after admission are reviewed, the diagnosis and treatment plan are discussed and corrected, if needed.
Second, third and fourth Author have reviewed patient documentation, last Author has provided support and has monitored the data collection with an overall source data verification rate of 44% and 100% for cases with complications.
Patients with midface fractures are seen in the outpatient department or in the emergency room (out of office hours). Patients are primarily admitted to the hospital. The diagnostics is performed immediately and the decision for the treatment option is taken as soon as the diagnostic results are available. Patients are diagnosed and operated—in case of dislocated fractures—based on the AO criteria24,25. Antibiotics (amoxicillin-clavulanic acid or clindamycin) are administered peri- and 3 days postoperatively, pain medication and cryotherapy is proven. In case of orbital involvement, an examination by eye specialists is mandatory. Patients are regularly discharged 2 days after surgery. The removal of the osteosynthesis implants is mostly offered for the patients to reduce late complications that could result from a foreign body. In these cases, osteosynthesis implants are standard titanium alloy materials that have been marketed in 2003.
The below list contains the fracture sites that have been assessed in this study.
-
Fractures of the central midface
-
Nasal bone fracture
-
Naso-orbito-ethmoid fracture (Markovitz Type I, II and III)
-
Medial orbital wall (orbito-ethmoid) fracture
-
Le Fort I type fracture
-
Le Fort II type fracture
-
Palatal fracture
-
Isolated fracture of the anterior sinus wall
-
-
Fractures of the lateral midface
-
Orbital floor fracture
-
Zygomatic arch fracture (only isolated cases)
-
Zygomatic bone fracture
-
Le Fort III type fracture
-
Orbital roof fracture
-
The complications are evaluated as per the classification of Clavien-Dindo31. Class I complications have not been evaluated. Any Class II–V complications were identified in patient documentation and were analyzed. Safety was assessed based on the WHO Guidelines for Safe Surgery. If an adverse consequence (complication, permanent disability) was detected, the procedure is considered as unsafe. In contrary, a completed treatment without complications or permanent disability is considered as safe32.
The main study hypothesis was that adopting the latest improvements of maxillofacial traumatology and supporting specialties leads to improvement in complication rate and other measures of care. Further hypothesis was that shortening of the time frame between injury and surgery decreases the rate of complications.
Based on the electronic data, the Dortmund Cranio-Maxillofacial Trauma Registry was created. The suitable patients have been identified in this databank. The radiographs, discharge and surgery reports of these patients have been analyzed. The data were analyzed with Microsoft Excel 2013 (® Microsoft Corp., Redmond, USA). The statistical analysis included descriptive methods including regression analysis and χ2-test to verify significance in case of gender and age differences. The confidence interval was p < 0.05.
Ethical approval
The Ethics Committee of the University of Witten–Herdecke has approved this study (No. 152/2017).
Informed consent for study participation and publication
Informed consent was obtained from all individual participants included in the study.
Results
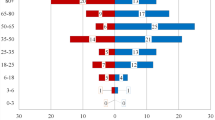
In eleven years from 1.1.2007 to 12.31.2017, a total number of 2868 patients have been admitted to our Department with isolated midface fractures (this makes 40.9% of the 7010 total hospitalizations for maxillofacial traumas). Table 1 reports the demographic data of the patients. A total of 1961 males and 907 females have been admitted (respectively 68.4% and 31.6% of isolated midface cases), the overall male-to-female ratio was 2.16:1, however, this rate shows a high variance between 6.95:1 in 18 to 25-year-old males and 1:2.54 in female older than 80 years old. The yearly number of patients is shown in Fig. 2, the trend is stable. To avoid bias resulting from differently sized population groups, the yearly average incidence rates have been counted based on the city population report33. The incidence is the highest in 18–25-year-old males and is generally higher in males before the age of 65 years. In the elderly (65 y.o. and above), the incidence is higher in females (Fig. 3).
Yearly average incidence of midface fractures in different age groups. (The incidence is given N/100,0000/year, the reference is the city population given in Table 1).
The analysis of the etiologies revealed that falls, interpersonal violence, road traffic accidents, sport and free time-related accidents and work-related accidents are the most common causes. Alcohol usage is very common, lately the use of drugs is an emerging issue.
The analysis of fracture sites (Table 2) has shown that the most exposed areas are the nasal bone, the zygomatic bone and the orbital floor (respectively 1405, 832 and 700 fracture sites). Also, in the case of zygomatic bone fractures and orbital floor fractures, there is a significant difference in the number of left and right-sided fractures. This difference results of the high number of interpersonal violence as a cause for these fractures, especially among young males. Classic Le Fort-fractures (a total of 178 in all three levels) or fractures in the nasoethmoid regions (a total of 53 fracture sites) are in comparison less common. Differently from the referred AO-classification, where this is not listed—in 40 cases, we found isolated fracture of the frontal maxillary sinus wall resulting mostly from falls or interpersonal violence.
The surgical treatment is performed mostly within 24 h after the injury (Fig. 4), 1.0 (SD = ± 0.3) days in case of first surgeries and 0.1 (SD = ± 0.7) days in case of secondary surgeries. The patients are observed 2.7 (SD = ± 4.9) days in case of first surgeries and 2.0 (SD = ± 0.7) days after secondary surgeries thereafter until discharge. The average surgery in the central midface area took 21 (SD = ± 26.2) minutes, in the lateral midface area 33 (SD = ± 27.4) minutes. Respectively the average anesthesia durations were 63 (SD = ± 78.6) and 90 (SD = ± 67.7) minutes. This grouping was performed to differentiate between different surgical technics applied in the nasal and periorbital regions.
Table 3 provides a summary of the most frequently used osteosynthesis implants. The 2.0 mm straight plate without bar is mostly used (37.6%), this one is used in many zygomatic bone fractures (23.9% of all fractures) at the frontozygomatic suture. The table lists modified and not modified length implants. The analysis of complications (see below) showed no difference in risk of complications after adaptations.
The complications are rare: we observed a total of 58 patients with severe complications. There were no lethal or life-threatening ones observed. The list of the complications e.g. their combinations are listed in Table 4. The majority of the complications are related to the procedure and a few of them are related to the osteosynthesis implants. In case of midface fractures, the complication rate (Clavien-Dindo Class II–IV) was 2.02%.
Discussion
The patient treatment protocol follows the AO guidelines24,25. This is the first study—as per authors’ information—that reports clinical results with the Medartis Modus® system. As new device designs and materials are marketed since osteosynthesis became a proven method34, re-evaluation of the novel developments is to be examined. This study is a retrospective assessment of 11 years of the treatment period in 2868 patients.
Most fractures are nasal bone, zygomatic bone and orbital floor fractures. Generally, the etiology and fracture distribution are similar to those in the international literature3,7,35,36,37. Some authors report more mandibular fractures than midfacial ones, in our registry midface fractures dominate (2868 vs. 1096 patients)38. The complication rate was 2.2%, which is below the international average22,39,40. The average time to the first surgery and the total inpatient stay is also shorter than it was reported by other authors19,20,41,42. This also helps to reduce the complication rate and is only possible with an experienced and well-managed team. In our opinion, immediate interdisciplinary diagnosis and therapy planning, early surgery and adequate postoperative care, including sufficient intensive care units and short hospital stay help reducing the overall complication rates. The midface is more stable and biomechanically less stressed than for example the mandibular angle or paramedian area. The aforementioned improvement in three-dimensional diagnostics and implant quality allows clearly easier surgery for orbital injuries, too. All these explain the better results in midface area than the overall complication rates, too. The osteosynthesis implants showed excellent stability, failures were in just a few cases reported. Most of these cases have not lead to a non-union, pseudoarthrosis, or osteomyelitis. Thus, the safety and efficacy of the methods and materials that are used in our surgery are proven.
The high incidence rate in young male and old female patients is alarming. At young age interpersonal violence and road traffic accidents are important etiologies. In older females, most cases are related to falls, less to road traffic accidents. Interpersonal violence is much rarely reported. Alcoholic influence is in both cases an important factor but in people older than 75 y.o. most falls are related to poor medical conditions. It is important, to apply more prevention in both patient groups to decrease the occurrence of facial fractures. As the number of admissions varies around yearly 260 ± 40 cases during the whole study period with a slightly worsening trend. In the whole registry, the yearly number of underage patients is decreasing, while in the elderly, the situation is getting worse. In younger men and older females more specific preventive work should be performed in order to reduce injury rates and consequences.
The limitation of the study is its retrospective nature. Some data, including radiographs, was missing. This was < 1% and missing data was mostly reproducible from the existing parts of the patient documentation. This retrospective nature of the study also carries advantages. The concept is the same during the study, the operations are carried out or supervised by the same, experienced surgeons. The treatment follows the above concept, but is highly individualized, thus a bias by using non-adaptable study protocols is reduced.
In conclusion, we can state, that the diagnostic and treatment protocols are appropriate, both these and sufficient experience supports good results and low complication rates. The novel osteosynthesis implants are safe and the surgeries can be performed on time.
The study covers a long time frame that is among the longest periods that have been reviewed. Another limitation of this study is that it is a monocentric one. A multicentric, prospective extension of this study (for example in Germany or in Europe) would bring still more scientific value. This requires, however, continuous efforts at all research centers that can increase long-term bias due to non-reporting cases. Due to the high work load with analyzing all radiographs and thorough monitoring, the study duration was long, the results, however, more standardized.
In conclusion, this study has shown that the three most common fractures of the midface area, nasal bone fractures, zygomatic bone fractures and orbital floor fractures (40.1%, 23.9% and 20.1% respectively) make 84.1% of all midface fractures. Due to improvement of diagnostics, therapy and materials used for surgery, the complication rate can be decreased to 2.2%, which is well below the internationally reported complication rates. This proves our hypothesis that the current guidelines and workflows contribute to improvement to patient safety and better treatment outcome.
Data availability
Data availability is ruled by the Data Protection laws of the European Union, the Federal Republic of Germany, the State North-Rhine-Westphalia and the regulations of Dortmund General Hospital. Data is therefore on purpose on-site available.
References
Eggensperger, N., Smolka, K., Scheidegger, B., Zimmermann, H. & Iizuka, T. A 3-year survey of assault-related maxillofacial fractures in central Switzerland. J. Craniomaxillofac. Surg. 35, 161–167 (2007).
Kontio, R., Suuronen, R., Ponkkonen, H., Lindqvist, C. & Laine, P. Have the causes of maxillofacial fractures changed over the last 16 years in Finland? An epidemiological study of 725 fractures. Dent. Traumatol. 21, 14–19 (2005).
Kraft, A. et al. Craniomaxillofacial trauma: Synopsis of 14,654 cases with 35,129 injuries in 15 years. Craniomaxillofac. Trauma Reconstr. 5, 41–50 (2012).
Lee, K. Global trends in maxillofacial fractures. Craniomaxillofac. Trauma Reconstr. 05, 213–222 (2012).
Louis, M., Agrawal, N. & Truong, T. A. Midface fractures II. Semin. Plast. Surg. 31, 94–99 (2017).
Hwang, K., Ki, S. J. & Ko, S. H. Etiology of nasal bone fractures. J. Craniofac. Surg. 28, 785–788 (2017).
Hwang, K. & You, S. H. Analysis of facial bone fractures: An 11-year study of 2,094 patients. Indian J. Plast. Surg. 43, 42–48 (2010).
Ali, K. & Lettieri, S. Management of panfacial fracture. Semin. Plast. Surg. 31, 108–117 (2017).
Oral and Maxillofacial Surgery for the Clinician (2021).
Riaud, X. First dental radiograph (1896). Dent. Hist. 59, 87–88 (2014).
Scarfe, W. C. Imaging of maxillofacial trauma: Evolutions and emerging revolutions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 100, S75–S96 (2005).
Lisiak-Myszke, M. et al. Application of finite element analysis in oral and maxillofacial surgery—A literature review. Materials 13, 3063 (2020).
Fonseca, R. J. & Fonseca, R. J. Oral and Maxillofacial Trauma (Elsevier Saunders, 2012).
Gilardino, M. S., Chen, E. & Bartlett, S. P. Choice of internal rigid fixation materials in the treatment of facial fractures. Craniomaxillofac. Trauma Reconstr. 2, 49–60 (2009).
de Viteri, V. S. & Fuentes, E. Titanium and titanium alloys as biomaterials. In Tribology—Fundamentals and Advancements (ed. Gegner, J.) 10.5772/55860 (InTech, 2013).
Rana, M. et al. Surgical treatment of zygomatic bone fracture using two points fixation versus three point fixation-a randomised prospective clinical trial. Trials 13, 1–10 (2012).
Pugachev, A. et al. Application of patient-specific simulation workflow for obstructive sleep apnea diagnosis and treatment with a mandibular advancement device. Int. J. Numer. Methods Biomed. Eng. 36, e3350 (2020).
Thayaparan, G. K., Lewis, P. M., Thompson, R. G. & D’Urso, P. S. Patient-specific implants for craniomaxillofacial surgery: A manufacturer’s experience. Ann. Med. Surg. 66, 102 (2021).
Czerwinski, M., Ma, S., Motakis, D. & Lee, C. Economic analysis of open approach versus conventional methods of zygoma fracture repair. Can. J. Plast. Surg. 16, 153–156 (2008).
Czerwinski, M., Martin, M. & Lee, C. Quantitative comparison of open reduction and internal fixation versus the Gillies method in the treatment of orbitozygomatic complex fractures. Plast. Reconstr. Surg. 115, 1848–1854 (2005) (discussion 1855–1857).
Bertram, A., Hyam, D. & Hapangama, N. Out-of-hours maxillofacial trauma surgery: A risk factor for complications?. Int. J. Oral Maxillofac. Surg. 42, 214–217 (2013).
Bicsák, Á. et al. Complications after osteosynthesis of craniofacial fractures-an analysis from the years 2015–2017. Oral Maxillofac. Surg. https://doi.org/10.1007/s10006-020-00903-1 (2020).
Sukegawa, S. et al. Maxillofacial trauma surgery patients with titanium osteosynthesis miniplates: Remove or not?. J. Craniofac. Surg. 31, 1338–1342 (2020).
Cornelius, C.-P. et al. The comprehensive AOCMF classification system: Midface fractures—Level 3 tutorial. Craniomaxillofac. Trauma Reconstr. 07, S068–S091 (2014).
Kunz, C. et al. The comprehensive AOCMF classification system: Orbital fractures—Level 3 tutorial. Craniomaxillofac. Trauma Reconstr. 07, S092-S102 (2014).
Audigé, L., Cornelius, C.-P., Kunz, C., Buitrago-Téllez, C. & Prein, J. The comprehensive AOCMF classification system: Classification and documentation within AOCOIAC software. Craniomaxillofac. Trauma Reconstr. 07, S114–S122 (2014).
Barrett, D. M., Halbert, T. W., Fiorillo, C. E., Park, S. S. & Christophel, J. J. Cost-based decision analysis of postreduction imaging in the management of mandibular fractures. JAMA Fac. Plast. Surg. 17, 28 (2015).
Geisler, B. P., Ji, Y. D. & Peacock, Z. S. Value in oral and maxillofacial surgery: A systematic review of economic analyses. J. Oral Maxillofac. Surg. 75, 2287–2303 (2017).
Lee, K. C., Chuang, S.-K. & Eisig, S. B. The Characteristics and cost of le fort fractures: A review of 519 cases from a nationwide sample. J. Oral Maxillofac. Surg. 77, 1218–1226 (2019).
Nalliah, R. P. et al. Economics of facial fracture reductions in the United States over 12 months. Econ. Fac. Fract. Reduct. Dent. Traumatol. 29, 115–120 (2013).
Monteiro, E. et al. Assessment of the Clavien–Dindo classification system for complications in head and neck surgery: The Clavien–Dindo classification system. Laryngoscope 124, 2726–2731 (2014).
WHO Guidelines for Safe Surgery 2009: Safe Surgery Saves Lives (2009).
Yearly report of the City of Dortmund (2018).
Brown, J. S., Grew, N., Taylor, C. & Millar, B. G. Intermaxillary fixation compared to miniplate osteosynthesis in the management of the fractured mandible: An audit. Br. J. Oral Maxillofac. Surg. 29, 308–311 (1991).
Allareddy, V., Allareddy, V. & Nalliah, R. P. Epidemiology of facial fracture injuries. J. Oral Maxillofac. Surg. 69, 2613–2618 (2011).
Manodh, P., Prabhu Shankar, D., Pradeep, D., Santhosh, R. & Murugan, A. Incidence and patterns of maxillofacial trauma-a retrospective analysis of 3611 patients-an update. Oral Maxillofac. Surg. 20, 377–383 (2016).
Motamedi, M. H. K. et al. Pattern of maxillofacial fractures: A 5-year analysis of 8,818 patients. J. Trauma Acute Care Surg. 77, 630–634 (2014).
Bicsák, Á., Abel, D., Berbuesse, A., Hassfeld, S. & Bonitz, L. Evaluation of mandibular fractures in a German nationwide trauma center between 2015 and 2017. J. Maxillofac. Oral Surg. https://doi.org/10.1007/s12663-021-01513-4 (2021).
Bossert, R. P. & Girotto, J. A. Blindness following facial fracture: Treatment modalities and outcomes. Craniomaxillofac. Trauma Reconstr. 2, 117–124 (2009).
Maqusi, S., Morris, D. E., Patel, P. K., Dolezal, R. F. & Cohen, M. N. Complications of pediatric facial fractures. J. Craniofac. Surg. 23, 1023–1027 (2012).
Cabalag, M. S. et al. Epidemiology and management of maxillofacial fractures in an Australian trauma centre. J. Plast. Reconstr. Aesthet. Surg. 67, 183–189 (2014).
Moses, H. et al. Opportunity cost of surgical management of craniomaxillofacial trauma. Craniomaxillofac. Trauma Reconstr. 09, 076–081 (2015).
Acknowledgements
We acknowledge Medartis AG, and especially Dr. Annika Cattin and Dr. Adrian Spiegel for their support. We acknowledge our colleagutes Mr Alexander Rost and Mr Frank Niemeier for their support. We thank for all our colleagues supporting our work with injured people.
Funding
Open Access funding enabled and organized by Projekt DEAL. Medartis AG (Hochbergerstr. 60E, CH-4057 Basel, Switzerland) has financially supported this study (no grant Nr. available).
Author information
Authors and Affiliations
Contributions
L.B.: study design, communication with EC, data collection, data management and analysis, text writing. D.A.: data collection, management and analysis. V.W.: data collection. E.P.: data collection. S.H.: study design, communication with EC, text review. Á.B.: corresponding author, study design, communication with EC, data collection, data management and analysis, text writing.
Corresponding author
Ethics declarations
Competing interests
S.H. and L.B. are design surgeons at Medartis AG, they declare no non-financial competing interest. Á.B., D.A., V.W. and E.P. declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bonitz, L., Wruck, V., Peretti, E. et al. Long-term evaluation of treatment protocols for isolated midfacial fractures in a German nation-wide craniomaxillofacial trauma center 2007–2017. Sci Rep 11, 18291 (2021). https://doi.org/10.1038/s41598-021-97858-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-97858-4
This article is cited by
-
Impact of the COVID-19 pandemic on maxillofacial trauma surgery in Germany - implications from the national DRG database
Oral and Maxillofacial Surgery (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.