Abstract
In clinical practice, most patients with monoclonal gammopathy of undetermined significance (MGUS) undergo long-term follow-up without disease progression. There is insufficient real-world data about how closely and whether anything other than disease progression should be monitored. Herein, we performed a nationwide study of 470 patients with MGUS with a 10-year follow-up to determine the patterns of disease progression and other comorbidities. During the follow-up period, 158 of 470 patients with MGUS (33.62%) progressed to symptomatic monoclonal gammopathies. Most of these were multiple myeloma (134/470 patients, 28.51%), and those diagnosed within 2 years after diagnosis of MGUS was high. Approximately 30–50% of patients with MGUS had hypertension, diabetes, hyperlipidemia, and osteoarthritis at the time of diagnosis, and these comorbidities were newly developed during the follow-up period in approximately 50% of the remaining patients with MGUS. Approximately 20–40% of patients with MGUS have acute or chronic kidney failure, thyroid disorders, disc disorders, peripheral neuropathy, myocardial infarction, stroke, and heart failure during the follow-up period. Altogether, when MGUS is diagnosed, close follow-up of the possibility of progression to multiple myeloma is required, especially within 2 years after diagnosis; simultaneously, various comorbidities should be considered and monitored during the follow-up of patients with MGUS. Continuous research is needed to establish appropriate follow-up guidelines.
Similar content being viewed by others
Introduction
Monoclonal gammopathy of undetermined significance (MGUS) is defined as serum monoclonal protein level < 3 g/dL, bone marrow plasma cells < 10%, and absence of end-organ damage (e.g., hypercalcemia, renal insufficiency, anemia, and bone lesions), or other lymphoproliferative malignancies1,2. MGUS is a well-known premalignant phase that can progress to multiple myeloma (MM), Waldenström macroglobulinemia (WM), AL amyloidosis, or other lymphoproliferative disorders at approximately 1% per year3,4,5. Therefore, to detect disease progression, the current guidelines recommend the quantification of monoclonal protein along with monitoring of related symptoms in patients with MGUS at 3–6 month intervals for the first 1–2 years, and then at 6–24 months intervals if stable4,6,7,8.
However, according to data from previous studies, the majority of patients with MGUS do not progress to symptomatic monoclonal gammopathy9,10. In addition, patients with MGUS have been shown to have an increased risk of bacterial infections, ischemic heart disease, renal disease, rheumatic diseases, skeletal fractures, and arterial or venous thrombosis11,12,13,14,15,16. Patients with MGUS have a shorter overall survival times compared to the matched control population17. Although progression to symptomatic monoclonal gammopathy is an important cause of death in patients with MGUS, it does not entirely explain the shorter overall survival time18. Other comorbidities may be associated with shorter overall survival times in patients with MGUS11,19,20, it is necessary to reconsider whether it is sufficient to focus solely on disease progression during follow-up and testing according to the recommendations of the guidelines mentioned above.
In this study, we performed a nationwide study with patients diagnosed with MGUS with a follow-up period of 10 years using the Health Insurance Review and Assessment Service (HIRA). This study aimed to determine the occurrence patterns of disease progression and other comorbidities during a 10-year follow-up period in the real world.
Methods
Data source
In South Korea, the National Health Insurance (NHI), which is a universal health coverage system, covers approximately 98% of the population21,22. Those insured by NHI pay insurance contributions and receive medical services from their health care providers, and then the NHI pays costs based on the claims data. The claims data consist of patients’ diagnosis, treatment, procedures, surgical history, and prescription drugs, and this information is anonymized and provided for healthcare service research in the form of the HIRA database. The data used in this study were extracted from patient information in the HIRA database and were approved by the Institutional Review Board of Korea University Anam Hospital (No. 2020AN0135). Since this study was conducted with anonymized patient data from the HIRA database, the need for informed consent was waived by the institutional review board.
Patients
In general, the healthcare provider files claims for patient's medical services to the NHI according to the patient's main diagnosis, sub-diagnosis, and rule-out diagnosis. The main diagnosis describes the primary complaint or disease requiring the greatest treatment or examination; the sub-diagnosis was defined as the disease that was present or occurred secondary to the main diagnosis and had an impact on patient care. A rule-out diagnosis was defined as a previously considered disease that was excluded after examination.
To analyze patients with MGUS who had undergone long-term follow-up for 10 years, the claims data for patients diagnosed with MGUS (D472 code of Korea Classification of Disease, 7th edition) as the main diagnosis or sub-diagnosis (excluding rule-out diagnosis) from January 1, 2007, to August 31, 2009, were extracted from January 1, 2007, to August 31, 2019. If a patient progressed to symptomatic monoclonal gammopathy during the follow-up period with MGUS stated as the diagnosis on the first claim data within the recruitment period of this study, it is possible that the two claim codes (MGUS as the main diagnosis and symptomatic monoclonal gammopathy as sub-diagnosis, or vice versa) could be claimed on the same date. These patients were not suitable for this study; therefore, patients with MM, plasma cell leukemia (PCL), plasmacytoma, WM, amyloidosis, and any lymphoproliferative diseases or hematologic malignancies at the date of diagnosis of MGUS were excluded (Supplementary Table 1).
This study aimed to determine the prevalence and occurrence patterns of disease progression and other comorbidities of MGUS in the real world. Therefore, all patients who met the inclusion criteria were presented without limitations, such as age.
Clinical endpoints
We aimed to confirm the prevalence of MGUS in South Korea and to determine the occurrence patterns of disease progression and other comorbidities during the 10-year follow-up period.
The prevalence of MGUS was calculated by dividing the number of patients with MGUS by the mid-year population (Table 1 and Supplementary Table 2). The HIRA only provides claim data for the patient population that the researcher intends to study (HIRA policy due to database serving capacity limitations). Instead, information on the number of patients with specific diseases (excluding details about that population) is disclosed to the general public as public data. In this study, we analyzed the claims data extracted from January 1, 2007, to August 31, 2019, for patients who were diagnosed with MGUS from January 1, 2007, to August 31, 2009. To present the number of patients with MGUS from 2007 to 2019, the number of patients with MGUS in 2007 and 2008 was derived from the HIRA database, and the data after 2009 were derived from the public data provided by HIRA (Fig. 1).
Disease progression was defined as the occurrence of MM, PCL, plasmacytoma, WM, amyloidosis, and any lymphoproliferative disease or hematologic malignancies after the date of diagnosis of MGUS. The incidence of disease progression was presented as the number of new patients in the year normalized to the number of patients with MGUS in this study. The prevalence was presented as the number of total patients in the year normalized to the number of patients MGUS in this study.
Comorbidities included chronic diseases known to be common in South Korea23 or diseases commonly associated with patients with MGUS in existing studies11,12,13,16. For solid malignancies, the seven most common cancers in South Korea were selected24. The prevalence of comorbidities at the diagnosis of MGUS was defined as comorbidities diagnosed from January 1, 2007, to the date of MGUS diagnosis. Newly developed comorbidities were defined as newly developed diseases in patients with MGUS who did not have any comorbidities at the time of MGUS diagnosis. As mentioned above, the HIRA provided claims data for patients who were diagnosed with MGUS from January 1, 2007, to August 31, 2009. To determine the prevalence of comorbidities in patients with MGUS compared to the entire population, the prevalence data for each comorbidity in the entire population (determined from public data from the HIRA database) were presented as reference data. The prevalence calculation method for each comorbidity in the entire population is presented as a figure legend in Supplementary Figure 1. The incidence and prevalence of newly developed comorbidities were presented as the number of new patients in the year and total number of patients in the year, respectively.
Statistical analysis
Categorical data are presented as frequencies and percentages. Continuous data are described as the mean with standard deviation. Statistical analyses were performed using SAS v9.4 (SAS Institute Inc., Cary, NC, USA) and R Statistical Software v3.3.3 (Foundation for Statistical Computing, Vienna, Austria).
Results
Patients with MGUS in South Korea
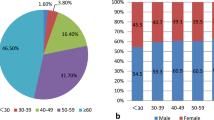
Between January 1, 2007, and August 31, 2009, 643 patients with MGUS were identified. A total of 470 patients were analyzed in this study, after excluding patients with MM, PCL, plasmacytoma, WM, amyloidosis, lymphoproliferative diseases, and hematologic malignancies at the time of diagnosis of MGUS (Supplementary Table 1). Among 470 patients with MGUS, bone marrow examination, spinal computed tomography (CT), or spinal magnetic resonance imaging (MRI) was performed within 30 days before the date of diagnosis with MGUS in 20.2% (95/470), 1.5% (7/470), and 0.9% (4/470) of cases, respectively. None of the patients with MGUS underwent positron emission tomography.
The prevalence rate per 100,000 people in South Korea between January 1, 2007, and August 31, 2009, was 0.37–0.50 overall and 1.11–1.52 in those aged 50 years or older. The prevalence of MGUS was higher in individuals aged 50 years and older and in men (Table 1). The prevalence has been shown to increase annually, and from around 2015, the trend of increase has become steeper (Fig. 1).
The occurrence patterns of disease progression during the follow-up period
Disease progression after the date of MGUS diagnosis during the follow-up period is summarized in Table 2. MM occurred in 28.51% (134 patients) of the 470 patients with MGUS. PCL, extramedullary plasmacytoma, and solitary plasmacytoma occurred in 0.43% (2 patients), 0.64% (3 patients), and 0.43% (2 patients), respectively. WM and amyloidosis occurred in 1.7% (7 patients) and 2.5% (10 patients), respectively. Lymphoma occurred in 4.68% (22 patients) and leukemia in 3.62% (17 patients).
The occurrence patterns of disease progression during the follow-up period of MM, PCL, extramedullary plasmacytoma, solitary plasmacytoma, WM, and amyloidosis are shown in Fig. 2. In the case of MM, WM, and amyloidosis, the probability of occurrence within 2 years of initial diagnosis of MGUS tended to be high. PCL, extramedullary plasmacytoma, and solitary plasmacytoma showed a tendency to occur sporadically throughout the follow-up period. In patients who progressed to MM, the median duration from the date of diagnosis of MGUS to the date of diagnosis of MM was 2.5 months (range: 0.1–147.4 months) (Supplementary Figure 2).
The occurrence patterns of disease progression during the follow-up period. The incidence of disease progression was presented as the number of new patients in the year in patients with MGUS in this study. The prevalence was presented as the number of total patients in the year in patients with MGUS in this study.
The occurrence patterns of comorbidities during the follow-up period
The prevalence of comorbidities and newly developed comorbidities during the follow-up period are summarized in Tables 3 and 4. Population-wide prevalence data for each comorbidity are presented as reference data in Table 3. The prevalence calculation method for each comorbidity is presented as a figure legend in Supplementary Figure 1. At the time of diagnosis of MGUS, 54.04% (254/470 patients), 40.64% (191/470 patients), 42.55% (200/470 patients), and 29.57% (139/470 patients) had accompanying hypertension (HTN), diabetes mellitus (DM), hyperlipidemia (HLD), and osteoarthritis (OA), respectively. During the follow-up period, HTN, DM, HLD, and OA were newly developed (i.e., not present at the time of diagnosis of MGUS) in 54.17% (117/216 patients), 54.48% (152/279 patients), 61.11% (165/270 patients), and 53.47% (177/331 patients) of patients, respectively. The occurrence pattern of these comorbidities appeared to occur within 5 years after the date of MGUS diagnosis (Fig. 3). Solid malignancies occurred in 5% of the patients during the follow-up period.
Discussion
In this study, the prevalence rate of MGUS was 1.11–1.52 in individuals aged 50 years or older per 100,000 population in South Korea between January 1, 2007, and August 31, 2009, and this has been gradually increasing. During a 10-year follow-up of patients with MGUS, 158 of 470 patients (33.62%) progressed to symptomatic monoclonal gammopathies. Most of these were MM (134/470 patients, 28.51%), and the number of cases diagnosed within 2 years after the diagnosis of MGUS was high. Approximately half of MGUS patients already had HTN, DM, HLD, and OA at the time of MGUS diagnosis, and these comorbidities occurred in approximately half of the remaining MGUS patients during the follow-up period.
The prevalence of MGUS in those older than 50 years has been reported to be 3.6–3.9% in Western countries10,25 and 0.8–3.3% in Eastern countries26,27,28. In this study, the prevalence rate per 100,000 was 0.37–0.50 overall and 1.11–1.52 in those aged 50 years or older in South Korea between January 1, 2007, and August 31, 2009. Considering that the world standardized incidence rate for MGUS was 3.76 ± 0.26 per 100,000 inhabitants reported in a population-based study in France29, the prevalence of MGUS in South Korea between January 1, 2007, and August 31, 2009, is thought to be relatively low compared to other countries. However, it is difficult to directly compare the prevalence of previous studies with those of the present study. In this study, we calculated the period prevalence by dividing the total number of patients with MGUS by the mid-year population. In other words, this study determined prevalence using the claim data for MGUS as a numerator and the mid-year population as the denominator, which is an arbitrary number representing the population. During the recruitment period, asymptomatic cases or cases in which the individual did not receive treatment could not be captured by this method; thus, the prevalence of MGUS could be somewhat underreported. In addition, since the mid-year population could be larger than the actual population, there is a possibility that the prevalence of MGUS in this study was somewhat underreported. In contrast, previous studies conducted screening tests for M-protein in all subjects regardless of symptoms, and these studies were conducted in limited participant groups recruited in community practices, hospitals, or regions, rather than the entire population.
It should be noted that the number of patients with MGUS is increasing every year compared to the patient registration period of this study (January 1, 2007, to August 31, 2009). This trend has not only been seen in South Korea, but also in other Asian countries, including Japan, Taiwan, and Hong Kong27,28,30. The reasons for this increase could be related to rapid industrialization and increased life span, which are common trends among Asian countries. Since aging is associated with the incidence of MGUS, increased life span may have increased the prevalence of MGUS. Alternatively, as interest in MGUS and diseases related to MGUS increases, more cases are assessed for MGUS, which may lead to greater detection of MGUS cases. Additionally, the prevalence of MGUS decreased in those over 80 years of age in this study, contrary to what it has been widely demonstrated in previous studies that indicated that prevalence of MGUS increases with increasing age10,25. Considering that this study was based on analysis of insurance claims data, it is possible that people in this age group had more passive hospital visits and treatment compared to younger people. Alternatively, this trend may be due to limited access to medical services in older patients.
In this study, a total of 158 of 470 patients with MGUS (33.62%) progressed to MM (28.51%), PCL (0.43%), extramedullary plasmacytoma (0.64%), solitary plasmacytoma (0.43%), WM (1.49%), and amyloidosis (2.13%) during a 10-year follow-up period. MM, WM, and amyloidosis showed a tendency to occur within 2 years after the initial diagnosis of MGUS; in contrast, PCL, extramedullary plasmacytoma, and solitary plasmacytoma occurred sporadically throughout the follow-up period. The molecular basis of MGUS progression to symptomatic monoclonal gammopathy remains poorly understood; however, several genetic aberrations may be involved in its mechanism. Taking this into account, the genetic factors involved in the mechanism of progression of symptomatic monoclonal gammopathy may differ from each other, which may have led to the above epidemiological pattern3,31,32,33,34. The 10-year cumulative probability of progression to MM in this study was higher than previously known (approximately 10%)1,7,18,35, which may also be due to racial and genetic differences. Alternatively, it could be due to insufficient work-up to exclude symptomatic monoclonal gammopathy at the time of diagnosis of MGUS in the real world because routine bone marrow examination or CT in all patients with MGUS was a controversial guideline in 20104,6,7,36. In fact, in the present study, bone marrow examination, spinal CT, and spinal MRI were performed in only 20.2%, 1.5%, and 0.9% of 470 patients with MGUS, respectively. In addition, approximately 50% of patients progressed to MM within 3 months from the date of MGUS diagnosis. Based on the results of this study, it can be suggested that when diagnosing patients with MGUS, sufficient tests should be performed to differentiate symptomatic monoclonal gammopathy, especially MM. If sufficient testing is not performed, close follow-up within three months of diagnosis is necessary. Another important consideration is that since this study selected patients with MGUS based on insurance claims data, patients without symptoms or specific clinical abnormalities may have been excluded. Therefore, the higher 10-year cumulative probability of progression reported in this study may have been due to the under-diagnosis of low-risk cases of MGUS with a low risk of disease progression.
Interestingly, approximately 30–50% of patients with MGUS had HTN, DM, HLD, and OA at the time of diagnosis of MGUS, and these comorbidities were newly developed during the follow-up period in approximately 50% of patients who did not have any comorbidities at the time of diagnosis of MGUS. According to data from the Korean National Health and Nutrition Examination Survey, the prevalence of HTN, DM, HLD, and OA in the population aged 50 years and older in South Korea is reported to be approximately 35%, 15%, 50%, and 35%, respectively37,38,39,40,41. Although direct comparison is impossible, it is deemed a significant number, considering that out of the total 470 patients with MGUS, the probability of already having or someday having these comorbidities is up to 80%. This may be because MGUS might be associated with the pathophysiology of HTN, DM, HLD, and OA. Alternatively, it may have been found that the chances of visiting the hospital and undergoing tests increased during the follow-up period for MGUS, considering the high incidence of these comorbidities within 5 years of MGUS diagnosis (Fig. 3). Conversely, a population that has already been diagnosed with HTN, DM, HLD, OA or belonging to a high-risk group that could proceed to these conditions have higher healthcare utilization and are therefore more likely to be tested for MGUS, that may have led to the results of this study.
Monitoring for kidney disease in patients with MGUS is important because it is one of the end-organ damages that can be caused by disease progression. In contrast, monoclonal gammopathy of renal significance (MGRS), in which one or more kidney lesions related to the produced monoclonal immunoglobulin occur without disease progression42. In this study, approximately 30% of 470 patients with MGUS had existing or newly developed acute or chronic kidney disease. This is a fairly high number compared to the pooled incidence of acute kidney disease in the general hospitalized population, which is 19.4% in Eastern Asia according to KDIGO-equivalent criteria43. The total prevalence estimate of chronic kidney disease in adults aged over 20 years in South Korea was 8.2%44. Supplementary Figures 3 and 4 present cases of newly occurring acute or chronic kidney disease in patients with MGUS divided according to disease progression. In this study, 15/470 patients (3.19%) and 13/470 patients (2.77%) were diagnosed with acute or chronic kidney disease, respectively, several months before disease progression. Additionally, 52/470 patients (11.06%) and 63/470 patients (13.40%) were diagnosed with acute or chronic kidney disease, respectively, without evidence of disease progression. These patients may have had MGRS. MGRS-associated kidney diseases do not respond well to the immunosuppressive regimens, and may necessitate clone-directed therapy. Affected patients have an approximately 90% recurrence after kidney transplantation if monoclonal gammopathy is not eliminated before or immediately after transplantation45,46,47. Therefore, it is necessary to raise awareness for these patients and actively consider kidney biopsy if MGRS is suspected.
In addition, approximately 20–40% of all MGUS patients in this study had pre-existing or newly diagnosed comorbidities such as thyroid disorders, disc disorders, peripheral neuropathy, myocardial infarction, stroke, and heart failure. These prevalence and incidence rates are higher than previously known48,49,50,51,52,53,54. However, it is difficult to conclude whether MGUS or underlying comorbidities may be risk factors for these diseases. Nevertheless, according to the results of this study, it is considered necessary to monitor not only disease progression but also the comorbidities mentioned above in the follow-up of patients with MGUS. In the case of solid malignancies, less than 5% of patients with MGUS were newly identified within the follow-up period. This is similar to the previously known average risk55,56,57,58,59; therefore, it is reasonable to perform cancer screening in MGUS patients in the same manner as in the general population.
This study analyzed claims data using the HIRA database; therefore, the present study has several limitations. First, because information on risk factors, including individual patient's type of MGUS and blood test at the time of diagnosis cannot be identified, detailed risk groups cannot be classified. Second, it was impossible to directly analyze the risk compared to the matched general population because HIRA only provided data concerning the population with MGUS claims data rather than the entire population (HIRA policy due to database capacity limitations). For example, this study showed that the prevalence of the aforementioned comorbidities in patients with MGUS was higher than the prevalence data for each comorbidity in the entire population provided by the public HIRA database (2010). However, it was not possible to determine whether this was due to MGUS or other combined comorbidities, as the comparison was not made with the general population, which was corrected for several factors that could influence these results. Third, we defined the prevalence of comorbidities at diagnosis of MGUS as comorbidities from January 1, 2007, to the date of diagnosis with MGUS, and newly developed comorbidities were defined as newly developed diseases in MGUS patients who did not have any comorbidities at the time of diagnosis of MGUS. There is a limitation in that the follow-up period, according to the date of diagnosis of MGUS, differed in determining the prevalence of comorbidities or the number of newly developed cases in this study. Although the distribution of the date of diagnosis with MGUS was relatively even except for January 2007, and the median follow-up duration for the definition of prevalence was 15.61 months, which was close to the average patient enrollment period (Supplementary Figure 5), it is necessary to be cautious in interpreting the prevalence of comorbidities or newly developed diseases presented in this study. Nevertheless, it is considered to be important because this study presented the prevalence of MGUS in South Korea and information on the occurrence patterns of disease progression and comorbidities during a 10-year follow-up period of patients with MGUS in the real world.
In conclusion, in this study, 33.62% of the patients with MGUS experienced disease progression to symptomatic monoclonal gammopathies during a 10-year follow-up in the real world. Most patients had MM, and the incidence rate was high within 2 years of the diagnosis of MGUS. In addition, approximately 80% of patients with MGUS were diagnosed with HTN, DM, HLD, and OA at the time of diagnosis or during the follow-up period. Taken together, when MGUS is diagnosed, close follow-up of the possibility of progression to MM is required, especially within 2 years after diagnosis; at the same time, various comorbidities should be considered and monitored during the follow-up of patients with MGUS, especially HTN, DM, HLD, and OA. Since this study was performed by analyzing insurance claims data, it must be taken into account that the prevalence of MGUS and its correlative comorbidities could have been underestimated from the actual prevalence, and more studies are needed to transition from the current disease progression detection-centered guidelines to those that can improve overall patient care.
References
Kyle, R. A. Monoclonal gammopathy of undetermined significance. Natural history in 241 cases. Am. J. Med. 64, 814–826 (1978).
Rajkumar, S. V. et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 15, e538-548 (2014).
van Nieuwenhuijzen, N., Spaan, I., Raymakers, R. & Peperzak, V. From MGUS to multiple myeloma, a paradigm for clonal evolution of premalignant cells. Cancer Res. 78, 2449–2456 (2018).
Kyle, R. A. et al. Monoclonal gammopathy of undetermined significance (MGUS) and smoldering (asymptomatic) multiple myeloma: IMWG consensus perspectives risk factors for progression and guidelines for monitoring and management. Leukemia 24, 1121–1127 (2010).
Cosemans, C. et al. Prognostic biomarkers in the progression from MGUS to multiple myeloma: A systematic review. Clin. Lymphoma Myeloma Leuk. 18, 235–248 (2018).
Bird, J. et al. UK myeloma forum (UKMF) and Nordic Myeloma Study Group (NMSG): Guidelines for the investigation of newly detected M-proteins and the management of monoclonal gammopathy of undetermined significance (MGUS). Br. J. Haematol. 147, 22–42 (2009).
Berenson, J. R. et al. Monoclonal gammopathy of undetermined significance: a consensus statement. Br. J. Haematol. 150, 28–38 (2010).
van de Donk, N. W. et al. The clinical relevance and management of monoclonal gammopathy of undetermined significance and related disorders: recommendations from the European Myeloma Network. Haematologica 99, 984–996 (2014).
Landgren, O. et al. Monoclonal gammopathy of undetermined significance (MGUS) consistently precedes multiple myeloma: A prospective study. Blood 113, 5412–5417 (2009).
Kyle, R. A. et al. Prevalence of monoclonal gammopathy of undetermined significance. N. Engl. J. Med. 354, 1362–1369 (2006).
Kristinsson, S. Y. et al. Patterns of survival and causes of death following a diagnosis of monoclonal gammopathy of undetermined significance: A population-based study. Haematologica 94, 1714–1720 (2009).
Kristinsson, S. Y. et al. Monoclonal gammopathy of undetermined significance and risk of skeletal fractures: A population-based study. Blood 116, 2651–2655 (2010).
Kristinsson, S. Y. et al. Arterial and venous thrombosis in monoclonal gammopathy of undetermined significance and multiple myeloma: A population-based study. Blood 115, 4991–4998 (2010).
Gregersen, H. et al. The risk of bacteremia in patients with monoclonal gammopathy of undetermined significance. Eur. J. Haematol. 61, 140–144 (1998).
Raposo, A., Peixoto, D. & Bogas, M. Monoclonal gammopathy and rheumatic diseases. Acta Reumatol. Portug. 39, 12–18 (2014).
Lomas, O. C., Mouhieddine, T. H., Tahri, S. & Ghobrial, I. M. Monoclonal gammopathy of undetermined significance (MGUS)-not so asymptomatic after all. Cancers (Basel) 12, 1554 (2020).
Kyle, R. A. et al. Long-term follow-up of monoclonal gammopathy of undetermined significance. N. Engl. J. Med. 378, 241–249 (2018).
Kyle, R. A. et al. Long-term follow-up of 241 patients with monoclonal gammopathy of undetermined significance: The original Mayo Clinic series 25 years later. Mayo Clin. Proc. 79, 859–866 (2004).
Gregersen, H. et al. Mortality and causes of death in patients with monoclonal gammopathy of undetermined significance. Br. J. Haematol. 112, 353–357 (2001).
Kristinsson, S. Y., Björkholm, M. & Landgren, O. Survival in monoclonal gammopathy of undetermined significance and Waldenström macroglobulinemia. Clin. Lymphoma Myeloma Leuk. 13, 187–190 (2013).
Cheol Seong, S. et al. Data resource profile: The national health information database of the national health insurance service in South Korea. Int. J. Epidemiol. 46, 799–800 (2017).
Kim, L., Kim, J.-A. & Kim, S. A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol. Health 36, e2014008–e2014008 (2014).
Kim, E. J., Yoon, S. J., Jo, M. W. & Kim, H. J. Measuring the burden of chronic diseases in Korea in 2007. Public Health 127, 806–813 (2013).
Hong, S. et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2017. Cancer Res. Treat. 52, 335–350 (2020).
Wadhera, R. K. & Rajkumar, S. V. Prevalence of monoclonal gammopathy of undetermined significance: A systematic review. Mayo Clin. Proc. 85, 933–942 (2010).
Park, H. K. et al. Prevalence of monoclonal gammopathy of undetermined significance in an elderly urban Korean population. Am. J. Hematol. 86, 752–755 (2011).
Wu, S. P. et al. MGUS prevalence in an ethnically Chinese population in Hong Kong. Blood 121, 2363–2364 (2013).
Iwanaga, M., Tagawa, M., Tsukasaki, K., Kamihira, S. & Tomonaga, M. Prevalence of monoclonal gammopathy of undetermined significance: Study of 52,802 persons in Nagasaki City, Japan. Mayo Clin. Proc. 82, 1474–1479 (2007).
Cabrera, Q. et al. Epidemiology of Monoclonal Gammopathy of Undetermined Significance (MGUS): The experience from the specialized registry of hematologic malignancies of Basse-Normandie (France). Cancer Epidemiol. 38, 354–356 (2014).
Watanaboonyongcharoen, P., Nakorn, T. N., Rojnuckarin, P., Lawasut, P. & Intragumtornchai, T. Prevalence of monoclonal gammopathy of undetermined significance in Thailand. Int. J. Hematol. 95, 176–181 (2012).
Bladé, J., Rosiñol, L., Cibeira, M. T. & de Larrea, C. F. Pathogenesis and progression of monoclonal gammopathy of undetermined significance. Leukemia 22, 1651–1657 (2008).
Zingone, A. & Kuehl, W. M. Pathogenesis of monoclonal gammopathy of undetermined significance and progression to multiple myeloma. Semin. Hematol. 48, 4–12 (2011).
Jiménez, C. et al. MYD88 L265P is a marker highly characteristic of, but not restricted to, Waldenström’s macroglobulinemia. Leukemia 27, 1722–1728 (2013).
Seckinger, A. et al. AL Amyloidosis—Pathogenesis and prognosis are determined by the amyloidogenic potential of the light chain and the molecular characteristics of malignant plasma cells. Blood 132, 187–187 (2018).
Kyle, R. A. et al. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N. Engl. J. Med. 346, 564–569 (2002).
Bustoros, M. et al. Bone marrow biopsy in low-risk monoclonal gammopathy of undetermined significance reveals a novel smoldering multiple myeloma risk group. Am. J. Hematol. 94, E146-e149 (2019).
Kim, H. C. et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: Part I-epidemiology of hypertension. Clin. Hypertens. 25, 16 (2019).
Noh, J. The diabetes epidemic in Korea. Endocrinol. Metab. 31, 349–353 (2016).
2018 Guidelines for the management of dyslipidemia FAU - Rhee, Eun-Jung FAU - Kim, Hyeon Chang FAU - Kim, Jae Hyeon FAU - Lee, Eun Young FAU - Kim, Byung Jin FAU - Kim, Eun Mi FAU - Song, YoonJu FAU - Lim, Jeong Hyun FAU - Kim, Hae Jin FAU - Choi, Seonghoon FAU - Moon, Min Kyong FAU - Na, Jin Oh FAU - Park, Kwang-Yeol FAU - Oh, Mi Sun FAU - Han, Sang Youb FAU - Noh, Junghyun FAU - Yi, Kyung Hee FAU - Lee, Sang-Hak FAU - Hong, Soon-Cheol FAU - Jeong, In-Kyung. Korean J. Intern. Med. 34, 723–771 (2019).
Lee, S. et al. The prevalence of osteoarthritis and risk factors in the Korean population: The sixth Korea National health and nutrition examination survey (VI-1, 2013). Korean J. Fam. Med. 40, 171–175 (2019).
Hong, J. W., Noh, J. H. & Kim, D.-J. The prevalence of and demographic factors associated with radiographic knee osteoarthritis in Korean adults aged ≥ 50 years: The 2010–2013 Korea National Health and Nutrition Examination Survey. PLoS ONE 15, e0230613 (2020).
Leung, N. et al. The evaluation of monoclonal gammopathy of renal significance: A consensus report of the International Kidney and Monoclonal Gammopathy Research Group. Nat. Rev. Nephrol. 15, 45–59 (2019).
Mehta, R. L. et al. International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): A human rights case for nephrology. Lancet (London, England) 385, 2616–2643 (2015).
Park, J. I., Baek, H. & Jung, H. H. Prevalence of chronic kidney disease in Korea: the Korean National Health and Nutritional Examination Survey 2011–2013. J. Korean Med. Sci. 31, 915–923 (2016).
Leung, N., Bridoux, F. & Nasr, S. H. Monoclonal gammopathy of renal significance. N. Engl. J. Med. 384, 1931–1941 (2021).
Fermand, J.-P. et al. How I treat monoclonal gammopathy of renal significance (MGRS). Blood 122, 3583–3590 (2013).
Wang, C. H. & Hogan, J. J. Monoclonal gammopathies and kidney disease. Search. Signif. 13, 1781–1782 (2018).
Kwon, H. et al. Prevalence and annual incidence of thyroid disease in Korea from 2006 to 2015: A nationwide population-based cohort study. Endocrinol. Metab. (Seoul) 33, 260–267 (2018).
Battié, M.C., Videman, T. & Parent, E. Lumbar disc degeneration: Epidemiology and genetic influences. Spine 29 (2004).
Won, J. C., Kim, S. S., Ko, K. S. & Cha, B.-Y. Current status of diabetic peripheral neuropathy in Korea: Report of a hospital-based study of type 2 diabetic patients in Korea by the diabetic neuropathy study group of the korean diabetes association. Diabetes Metab. J. 38, 25–31 (2014).
Kim, H. et al. Prevalence and incidence of atherosclerotic cardiovascular disease and its risk factors in Korea: A nationwide population-based study. BMC Public Health 19, 1112 (2019).
Kim, J. Y. et al. Executive summary of stroke statistics in Korea 2018: A report from the epidemiology research council of the Korean Stroke Society. J. Stroke 21, 42–59 (2019).
Hwang, S. et al. Changes in acute kidney injury epidemiology in critically ill patients: A population-based cohort study in Korea. Ann. Intensive Care 9, 65–65 (2019).
Lee, J. H., Lim, N. K., Cho, M. C. & Park, H. Y. Epidemiology of heart failure in Korea: Present and future. Korean Circ. J. 46, 658–664 (2016).
Kim, G. H., Liang, P. S., Bang, S. J. & Hwang, J. H. Screening and surveillance for gastric cancer in the United States: Is it needed?. Gastrointest. Endosc. 84, 18–28 (2016).
Hampton, J. S., Sharp, L., Craig, D. & Rees, C. J. Colorectal cancer screening and surveillance for non-hereditary high-risk groups—Is it time for a re-think?. Curr. Treat. Options Gastroenterol. 19, 48–67 (2021).
Vecchio, M. M. Breast cancer screening in the high-risk population. Asia Pac. J. Oncol. Nurs. 5, 46–50 (2018).
Hayes, J. H. & Barry, M. J. Screening for prostate cancer with the prostate-specific antigen test: A review of current evidence. JAMA 311, 1143–1149 (2014).
Croswell, J. M., Ransohoff, D. F. & Kramer, B. S. Principles of cancer screening: Lessons from history and study design issues. Semin. Oncol. 37, 202–215 (2010).
Acknowledgements
This study was supported by grants from the Celltrion Pharm (Grant Number: CR 2020-7).
Author information
Authors and Affiliations
Contributions
B. S. K. and K. W. K. designed the study. K. W. K. and J. E. S. analyzed the data and summarized the results. K. W. K. wrote the manuscript. B. H. L., M. J. J., E. S. Y., D. S. K., S. R. L., H. J. S., C. W. C., Y. P., and B. S. K. reviewed the data analysis. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kang, KW., Song, J.E., Lee, BH. et al. A nationwide study of patients with monoclonal gammopathy of undetermined significance with a 10-year follow-up in South Korea. Sci Rep 11, 18449 (2021). https://doi.org/10.1038/s41598-021-97664-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-97664-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.