Abstract
The Coronavirus Disease (COVID-19) pandemic imposed a high burden of morbidity and mortality. In COVID-19, direct lung parenchymal involvement and pulmonary microcirculation dysfunction may entail pulmonary hypertension (PH). PH and direct cardiac injury beget right ventricular dysfunction (RVD) occurrence, which has been frequently reported in COVID-19 patients; however, the prevalence of RVD and its impact on outcomes during COVID-19 are still unclear. This study aims to evaluate the prevalence of RVD and associated outcomes in patients with COVID-19, through a Systematic Review and Meta-Analysis. MEDLINE and EMBASE were systematically searched from inception to 15th July 2021. All studies reporting either the prevalence of RVD in COVID-19 patients or all-cause death according to RVD status were included. The pooled prevalence of RVD and Odds Ratio (OR) for all-cause death according to RVD status were computed and reported. Subgroup analysis and meta-regression were also performed. Among 29 studies (3813 patients) included, pooled prevalence of RVD was 20.4% (95% CI 17.1–24.3%; 95% PI 7.8–43.9%), with a high grade of heterogeneity. No significant differences were found across geographical locations, or according to the risk of bias. Severity of COVID-19 was associated with increased prevalence of RVD at meta-regression. The presence of RVD was found associated with an increased likelihood of all-cause death (OR 3.32, 95% CI 1.94–5.70). RVD was found in 1 out of 5 COVID-19 patients, and was associated with all-cause mortality. RVD may represent one crucial marker for prognostic stratification in COVID-19; further prospective and larger are needed to investigate specific management and therapeutic approach for these patients.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its associated disease (COVID-19), plagued the world during 2020, with the World Health Organization declaring a pandemic state earlier in the year1. By 13th July 2021, an estimated 4 million deaths were attributed to COVID-19 worldwide2, with an extremely high healthcare, social, and economic burden. Most of the disease’s mortality and severity have been attributed to respiratory complications of the disease; indeed, patients may develop severe pneumonia up to Acute Respiratory Distress Syndrome (ARDS). Beyond direct alveolar involvement, also lung microcirculation seems to be affected in these patients. Autopsies studies revealed a pattern of pulmonary endothelial dysfunction with increased inflammatory infiltrate and microvascular thrombosis3. All the conditions mentioned above may lead to the development of increased pulmonary pressures and right ventricle overload.
On the other hand, cardiovascular complications have been early addressed as one concern in these patients4. While several factors may influence the severity and clinical course of the disease5, cardiovascular disease, including arrhythmia, myocardial disfunction and myocardial injury, have been repeatedly identified as potential key detrimental factors in patients with COVID-196,7,8. Lung parenchymal involvement, pulmonary microvascular pathologic changes, right ventricular pressure overload, and direct myocardial injury exert a synergic detrimental effect on the right ventricular function.
Indeed, right ventricular dysfunction (RVD)9 has been described as a potential predictor of poor outcomes in small preliminary studies, but its prevalence and associated outcomes in patients with COVID-19 are far from being elucidated. Clarification of the prevalence of RVD, and its associated outcomes in patients with COVID-19, may promote the implementation of tailored strategies for the screening, prevention, and treatment of right ventricular impairment.
Amid this pandemic, systematic review and meta-analysis have been depicted as essential tools to provide a timely and comprehensive synthesis of evidence during the COVID-19 pandemic10. Moving from this, this systematic review and meta-analysis aimed to estimate the prevalence of RVD among patients with COVID-19 and to explore its impact on all-cause mortality.
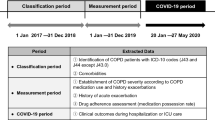
Materials and methods
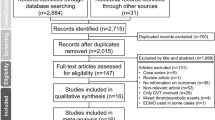
This systematic review has been performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and recommendations. The protocol was registered into the international register of systematic reviews PROSPERO, N. CRD42021227946.
Search strategy
Systematic and comprehensive literature research was performed on MEDLINE and EMBASE databases, from inception to 15th July 2021. The search strategy included a combination of terms related to the research question, including ‘right ventricular dysfunction’, ‘COVID-19’, and ‘SARS-CoV-2’. The full search strategy is available in Supplementary Material, Table S1.
Study selection
All records retrieved from the database search were systematically assessed by two independent authors (BC and GFR) according to titles and abstracts; articles included after this phase were subsequently screened for full-text eligibility. Study selection was performed with the use of a standardized web-based platform (Covidence). Any disagreement during each phase was discussed collegially. Inclusion criteria were: (i) any study reporting the prevalence of RVD; or (ii) any study reporting outcomes in patients with COVID-19 according to the RVD status (i.e., number of patients with and without RVD who died). Exclusion criteria were: (i) case reports, conference abstracts, editorial, comments, systematic reviews, meta-analyses and guidelines, (ii) studies that enrolled less than 30 COVID-19 patients, and (iii) articles in languages other than English, Italian or Spanish.
References of the included studies were additionally searched for other relevant articles that were not retrieved from the literature search. In the case of two or more studies based on the same cohort of subjects and exploring the same outcome(s), only the most recently published were selected and included.
Outcomes definition
Primary outcomes were defined as (i) prevalence of RVD, as defined in the original studies, and (ii) all-cause death according to RVD status. When RVD was not clearly defined in the original studies or multiple definitions were reported, we considered RVD according to the study-defined TAPSE cut-off, if available, to increase the homogeneity of RVD definition among studies included. Among the “all-cause death” definition, we also included the in-hospital mortality and 30-day mortality, as defined in the original studies.
Data extraction and quality assessment
Data from the studies included were independently extracted by two co-authors (BC and GFR) using a standardized electronic form. Data on sample size, number of individuals with and without RVD, mortality, and follow-up time were extracted. We collected data about study design and cohort baseline characteristics (i.e., age, sex, associated comorbidities including hypertension, diabetes mellitus, congestive heart failure (CHF)), and data on the severity of the disease or intensity of care received (i.e. intensive care unit (ICU), mechanically ventilated patients), when available. Proportion of patients with severe COVID-19 disease enrolled was also extracted; we defined severity according to the original studies definitions, when available, or according to a diagnosis of ARDS, or need for mechanical ventilation.
All studies included were independently evaluated by two co-authors (BC and GFR) to evaluate their quality and assess the risk of bias. We assessed the risk of bias separately for the two primary outcomes of the study. For studies reporting the prevalence of RVD, we used a customized version of the Newcastle–Ottawa Scale (NOS) for cross-sectional studies, composed of 5 items across 3 domains (selection, comparability, outcomes), with a maximum of 5 points. Each study with a score ≤ 3 was considered at high risk of bias. We used a customized version of the NOS for cohort studies for studies reporting outcomes, composed of 8 items across 3 domains (selection, comparability, outcomes), with a maximum of 9 points. Each study with a score ≤ 6 was considered at high risk of bias.
Publication bias was assessed for studies reporting outcomes according to RVD status. Funnel plots were visually inspected for asymmetricity; furthermore, Egger’s test was also performed and reported.
Statistical analysis
Pooled prevalence of RVD, 95% confidence intervals (CI) and 95% prediction intervals (PI) were estimated using a generalized linear mixed model11. 95% PI represents a predicted range of the true effect in an individual or new study and provide useful information on the variability of the effect in different clinical settings12,13.
Outcomes from the original studies and according to RVD status were pooled and compared using random-effect models; restricted maximum likelihood was used to estimate tau for this outcome.
Pooled estimates were reported as Odds Ratios (OR) and 95% confidence intervals (CI). The inconsistency index (I2) was calculated to measure heterogeneity. According to pre-specified cut-offs, low heterogeneity was defined as an I2 of < 25%, moderate heterogeneity when I2 falls between 25 and 75%, and high heterogeneity when I2 was > 75%.
For each primary outcome, a “leave-one-out” sensitivity analysis was performed, by iteratively removing 1 study at a time to analyse their influence on pooled estimate and heterogeneity.
We also performed two subgroup analyses for the prevalence of RVD, according to the geographical location of the included studies, and the risk of bias. No subgroup analysis was performed for the all-cause death, according to the low number of studies included in this analysis. To evaluate the potential impact of COVID-19 severity on the prevalence of RVD, we also performed an univariable meta-regression analysis.
All the statistical analyses were performed using R version 4.1.0 (The R Foundation, 2021), with the use of ‘meta’, ‘metafor’ and ‘dmetar’ packages.
Results
A total of 350 studies were retrieved from the literature search (146 from MEDLINE and 204 from EMBASE). After the selection process, a total of 29 articles were included in the analysis14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42 (Fig. S1 in Supplementary Materials).
Systematic review of the included studies
Table 1 shows the baseline characteristics of the studies included in the meta-analysis. 29 studies reported data about the prevalence of RVD14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42, while 7 reported about all-cause mortality according to RVD status17,19,20,30,33,35,36. 11 studies were held in Europe16,18,19,20,21,33,34,35,36,38,40, 8 in North America23,25,26,28,29,37,41,42, 3 in Asia30,31,32, and 7 in other geographical locations14,15,17,22,24,27,39, including 2 multinational studies24,27. Cohorts included were quite homogeneous in terms of mean age of the included patients (ranging from 52 years old to 68 years old); among sex, males were generally more represented than females (up to 84%). Among studies reporting outcome, the definition of all-cause mortality comprised ICU-death17, in-hospital mortality35, 30-day mortality36, 90-day mortality19 or unspecified all-cause death20,30,33.
The definition of RVD was heterogeneous across studies, both in terms of parameters and cut-offs used to defined RVD. 13 studies used a combination of several parameters15,18,19,21,24,28,30,33,34,35,38,40,42, 8 studies defined RVD according to TAPSE cut-off14,16,22,23,31,32,36,39, while other or unclear definitions of RVD was used in 8 studies17,20,25,26,27,29,37,41. In one study, a surrogate of Right Ventricular-Arterial uncoupling, which in turn relates the degree of RVD to the increase of pulmonary pressure, was addressed20. For 4 studies, we assumed RVD according to the reported TAPSE cut-offs, to mitigate heterogeneity in the RVD definition among studies14,16,22,39.
The risk of bias for each study was reported in Tables S2 and S3 in Supplementary Materials, respectively for studies assessing the prevalence of RVD, and for studies reporting outcomes. Among studies reporting prevalence, 13 were defined at high risk of bias, while 5 studies were defined at high risk of bias among those reporting outcomes. Selection bias and definition of RVD were the most common concerns among the included studies.
Meta-analysis of the included studies
Prevalence of RVD
Among 3813 patients included in the analysis, pooled prevalence of RVD was found as high as 20.4%, with a high degree of heterogeneity between studies. PI was between 7.8% and 43.9% (Fig. 1). No significant differences were observed in the prespecified subgroup analysis according to geographical location or bias risk (Table S4).
The prespecified leave-one-out sensitivity analysis showed overall consistency of the main results, with little to no influence of individual studies on pooled estimates or heterogeneity (Fig. S2).
To evaluate the impact of COVID-19 severity (defined as the proportion of patients defined as “severe” or “critical” in the original study, or when a stratification was not available, as those patients with ARDS or mechanically ventilated) on the prevalence of RVD, we performed an univariable meta-regression analysis. The results are graphically reported in Fig. 2; the proportion of patients with severe COVID-19 disease was significantly associated with the prevalence of RVD in the cohorts included (p = 0.040, R2 = 22.4%).
All-cause death according to RVD
Seven studies reported all-cause death occurrence according to RVD status, with a total of 847 patients included in the analysis. RVD was associated with a significantly increased likelihood of all-cause death (OR 3.32, 95% CI 1.94–5.70), with a moderate grade of heterogeneity between studies (Fig. 3). The leave-one-out analysis showed that excluding the study from D’Alto et al.20 reduces the pooled estimate, with no heterogeneity among the 6 remaining studies (I2 = 0%, Fig. S3). No publication bias was detected (Egger’s test p = 0.446, Fig. S4).
Discussion
COVID-19 disease was defined as the third leading cause of death in the United States by October 202043. At this stage of the pandemic, early identification of patients at higher risk of clinical deterioration is critical for proper prognostic stratification and delivering the best care. Cardiovascular complications, including myocardial dysfunction, has been described as a potential predictor of adverse outcomes44; although most studies focused on left ventricular impairment, some reports clearly underlines a potential detrimental role of RVD in patients with COVID-19.
Our study reports a comprehensive and updated systematic review and meta-analysis on the prevalence of RVD and associated outcomes in patients with COVID-19. Overall, we found that the prevalence of RVD may be as high as almost 1 out of 5 patients. Among the studies included, we observed a largely ranging prevalence of RVD, possibly reflecting the heterogeneity in the sensitivity of the methods used to define RVD. Bleakley et al.16 observed that specific phenotypes of RVD may be present in patients with COVID-19, and that definition according to TAPSE may have low sensitivity to detect RVD in this clinical scenario. The severity of the disease may also represent one key factor influencing the prevalence of RVD among COVID-19 patients, although evidence is limited. In our meta-analysis, we reported a large variation of PI, up to 44%; this information may be particularly useful to interpret the findings of our study: our results indicates that, depending on the method used to define RVD and the clinical setting, the prevalence of RVD in patients with COVID-19 may be higher than expected. This hypothesis is confirmed by our meta-regression, which found that the proportion of severe COVID-19 patients enrolled was a significant predictor for higher prevalence of RVD in the studies included. The relatively low R2 found for this association suggests that other factors are important in determining the prevalence of RVD, but we were unfortunately unable to analyze them, and to perform multivariable meta-regressions, due to data availability. Beyond that, and although this analysis has some clear limitation (the heterogeneous definition of severe disease, and the study-level nature of this association), the results of our meta-regression may support a mechanistic link between severe disease and RVD. However, further studies are needed to confirm this association, and to evaluate the impact of other risk factors on the risk of RVD in COVID-19 patients.
Several physiopathological hypotheses sustain association between COVID-19 and RVD. COVID-19 related ARDS is likely to be often complicated by RVD, given the direct alveolar injury and the associated ventilatory strategies such as hyper-inflated lungs and permissive hypercapnia45. Moreover, a direct detrimental viral effect on pulmonary microcirculation up to a pattern of endothelium with endothelial dysfunction46 and increased vascular inflammatory infiltrate was reported in autopsies from COVID-19 patients3. As a matter of fact, an interplay between COVID-19, angiotensin-converting enzyme 2, and pulmonary hypertension have been postulated47,48.
Furthermore, COVID-19 has been linked to an increased risk of venous thromboembolism (VTE) and pulmonary embolism49, with the highest risk for patients with severe disease; moving from these evidence, VTE may represent a critical cause of deterioration of RV function and performance50. Taken all pathophysiological mechanisms together (parenchymal involvement, endothelial damage, and pulmonary embolism), right ventricular overload with increased pulmonary pressures is likely to occur frequently. Furthermore, COVID-19 is associated with direct myocardial injury through many different mechanisms, including inflammation, microvascular dysfunction, hypoxia, and ischemia44, with also a COVID-19 related myocarditis described51. Although these manifestations may be more frequently causing left ventricular dysfunction, it is possible that they also have a role, although often overlooked, in the onset of RVD.
Beyond these hypotheses, our findings demonstrated that patients with COVID-19 and RVD are exposed to an excess of mortality than patients without RVD. Our results are in line to what has been observed in other clinical settings characterized by respiratory infectious diseases; indeed, reduced right ventricular function was reported as a risk factor for adverse events in community-acquired pneumonia52, as well as in patients with ARDS45. This information may be crucial for clinicians dealing with patients with COVID-19. In fact, bedside ultrasound examination has become increasingly important in this pandemic, for the assessment of disease progression, lung-heart interactions, and hemodynamic instability53, in a context where access to second-line diagnostics tools is often reduced by logistic constraints or severity of the disease, as in the critically ill patients. According to our data, careful assessment of RV function, which is often undervalued and overlooked in a fast approach to cardiac ultrasound, may provide useful information and may drive specific therapeutic approaches. Since most of the included cohorts reported about patients in ICU settings, these findings may not be immediately translated to all patients with COVID-19; however, further studies are required to confirm these results, and to explore whether a standardized screening program for RVD dysfunction, as well as tailored therapeutic approaches, may significantly improve the prognosis of these patients.
Limitations
This study has several limitations. First, most of the studies included in this meta-analysis are retrospective or based on small cohorts, some of which were found at high risk of bias. This limitation, which may have affected our results and estimates, is mainly due to the nature of the research question, and the pandemic scenario in which these studies were conducted. Moreover, the heterogeneity in the definition of RVD may have distorted our estimates on the pooled prevalence of the disease. To overcome these limitation (at least partially), we reported PI, which gave a broader sense of the possible distribution of the actual prevalence in patients with COVID-19. Furthermore, our leave-one-out analysis showed consistency of our results after excluding one study at a time. Our study was not designed to assess factors that may influenced the association between COVID-19 and RVD; also, some baseline characteristics were missing or not reported in the original studies, and most studies did not provide details on the severity or grade of RVD. This limited our ability to evaluate the influence of specific variables on the prevalence of RVD, or stratify our results according to RVD grading. We attempted to estimate the impact of COVID-19 severity on RVD prevalence through a meta-regression analysis, which may help in understanding the association between severity of COVID-19 and burden of RVD. However, we were not able to perform multivariable meta-regression with other risk factors, due to data availability; therefore, the results of the meta-regression analysis should be interpreted with caution. Most of the patients were recruited in ICUs and/or underwent mechanical ventilation, and these factors may have influenced the assessment of RVD in the original studies and, in turn, our results. However, these patients represent a relevant part of individuals with COVID-19, so that these findings are highly relevant to everyday practice. We were only able to analyse the association between RVD and all-cause mortality in COVID-19 patients, since the original studies did not report sufficient data on the causes of death observed. Further studies are required to analyse the impact of RVD on different cause of mortality, including cardiovascular and COVID-19 related mortality.
Conclusion
Among patients with COVID-19, RVD can be found in almost 1 out of 5 patients; the prevalence may be influenced by the severity of COVID-19 disease, but these results need confirmation in further studies. Patients with RVD showed a threefold higher likelihood of all-cause death, compared to patients with normal RV function. RVD may represent one important and often overlooked marker for prognostic stratification in COVID-19; further studies are needed to clarify this association and investigate the specific management and therapeutic approach for these patients.
References
World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020 (WHO, 2021).
World Health Organization. Weekly Epidemiological Update on COVID-19—13 July 2021 (WHO, 2021).
Varga, Z. et al. Endothelial cell infection and endotheliitis in COVID-19. The Lancet 395, 1417–1418 (2020).
Long, B., Brady, W. J., Koyfman, A. & Gottlieb, M. Cardiovascular complications in COVID-19. Am. J. Emerg. Med. 38, 1504–1507 (2020).
Jordan, R. E., Adab, P. & Cheng, K. K. Covid-19: Risk factors for severe disease and death. BMJ 368, 1–2 (2020).
Shi, S. et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 5, 802–810 (2020).
Gupta, A. K. et al. Current perspectives on coronavirus disease 2019 and cardiovascular disease: A white paper by the JAHA editors. J. Am. Heart Assoc. 9, e017013 (2020).
Romiti, G. F., Corica, B., Lip, G. Y. H. & Proietti, M. Prevalence and impact of atrial fibrillation in hospitalized patients with COVID-19: A systematic review and meta-analysis. J. Clin. Med. 10, 2490 (2021).
D’Andrea, A. et al. Right ventricular function and pulmonary pressures as independent predictors of survival in patients with COVID-19 pneumonia. Cardiovasc. Imaging 13, 2467–2468 (2020).
Romiti, G. F., Corica, B., Cangemi, R., Basili, S. & Raparelli, V. Need for innovative and timely synthesis of evidence during Covid-19 outbreak. Eur. J. Intern. Med. 77, 165–166 (2020).
Stijnen, T., Hamza, T. H. & Özdemir, P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat. Med. 29, 3046–3067 (2010).
IntHout, J., Ioannidis, J. P. A., Rovers, M. M. & Goeman, J. J. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 6, e010247 (2016).
Riley, R. D., Higgins, J. P. T. & Deeks, J. J. Interpretation of random effects meta-analyses. BMJ 342, 964–967 (2011).
Barman, H. A. et al. Echocardiographic features of patients with COVID-19 infection: A cross-sectional study. Int. J. Cardiovasc. Imaging. https://doi.org/10.1007/s10554-020-02051-9 (2020).
Bitar, Z. I., Shamsah, M., Bamasood, O. M., Maadarani, O. S. & Alfoudri, H. Point-of-care ultrasound for COVID-19 pneumonia patients in the ICU. J. Cardiovasc. Imaging 29, 60–68 (2021).
Bleakley, C. et al. Right ventricular dysfunction in critically ill COVID-19 ARDS. Int. J. Cardiol. https://doi.org/10.1016/j.ijcard.2020.11.043 (2020).
Calderón-Esquivel, N. et al. Correlación de variables ecocardiográficas y biomarcadores en pacientes graves con COVID-19. Cir. Cir. 89, 1–6 (2020).
Ceriani, E. et al. Early echocardiographic findings in patients hospitalized for COVID-19 pneumonia: A prospective, single center study. Intern. Emerg. Med. https://doi.org/10.1007/s11739-021-02733-9 (2021).
Chotalia, M. et al. Right ventricular dysfunction and its association with mortality in coronavirus disease 2019 acute respiratory distress syndrome. Crit. Care Med. https://doi.org/10.1097/ccm.0000000000005167 (2021).
D’Alto, M. et al. Right ventricular-arterial uncoupling independently predicts survival in COVID-19 ARDS. Crit. Care 24, 1–10 (2020).
Doyen, D. et al. Characteristics of cardiac injury in critically ill patients with coronavirus disease 2019. Chest. https://doi.org/10.1016/j.chest.2020.10.056 (2020).
García-Cruz, E. et al. Critical care ultrasonography during COVID-19 pandemic: The ORACLE protocol. Echocardiography 37, 1353–1361 (2020).
Gibson, L. E. et al. Right ventricular strain is common in intubated COVID-19 patients and does not reflect severity of respiratory illness. J. Intens. Care Med. https://doi.org/10.1177/08850666211006335 (2021).
Giustino, G. et al. Characterization of myocardial injury in patients with COVID-19. J. Am. Coll. Cardiol. 76, 2043–2055 (2020).
Iyengar-Kapuganti, R. L. et al. Point-of-care ultrasound findings and clinical outcomes in patients with COVID-19. J. Am. Soc. Echocardiogr. 33, 1416–1417 (2020).
Jain, R. et al. Comprehensive echocardiographic findings in critically ill COVID-19 patients with or without prior cardiac disease. J. Patient Cent. Res. Rev. 8, 68–76 (2021).
Karagodin, I. et al. Echocardiographic correlates of in-hospital death in patients with acute COVID-19 infection: The world alliance societies of echocardiography (WASE-COVID) STUDY. J. Am. Soc. Echocardiogr. https://doi.org/10.1016/j.echo.2021.05.010 (2021).
Kim, J. et al. Prognostic utility of right ventricular remodeling over conventional risk stratification in patients with COVID-19. J. Am. Coll. Cardiol. 76, 1965–1977 (2020).
Krishna, H. et al. Cardiac abnormalities in COVID-19 and relationship to outcome. Mayo Clin. Proc. 96, 932–942 (2021).
Li, Y. et al. Echocardiographic characteristics and outcome in patients with COVID-19 infection and underlying cardiovascular disease. Front. Cardiovasc. Med. https://doi.org/10.3389/fcvm.2021.642973 (2021).
Li, Y. L. et al. Acute right ventricular dysfunction in severe COVID-19 pneumonia. Rev. Cardiovasc. Med. 21, 635–641 (2020).
Liaqat, A., Ali-Khan, R. S., Asad, M. & Rafique, Z. Evaluation of myocardial injury patterns and ST changes among critical and non-critical patients with coronavirus-19 disease. Sci. Rep. 11, 4828 (2021).
Moody, W. E. et al. Impact of right ventricular dysfunction on mortality in patients hospitalized with COVID-19, according to race. CJC Open. https://doi.org/10.1016/j.cjco.2020.09.016 (2020).
Norden, N. et al. Cardiac involvement in critically ill and mechanically ventilated patients with COVID-19-a prospective, observational echocardiographic study. Am. J. Cardiovasc. Dis. 11, 253–261 (2021).
Pagnesi, M. et al. Pulmonary hypertension and right ventricular involvement in hospitalised patients with COVID-19. Heart 106, 1324–1331 (2020).
Rath, D. et al. Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection. Clin. Res. Cardiol. 109, 1491–1499 (2020).
Schott, J. P. et al. Transthoracic echocardiographic findings in patients admitted with SARS-CoV-2 infection. Echocardiography 37, 1551–1556 (2020).
Soulat-Dufour, L. et al. Prognostic value of right ventricular dilatation in patients with COVID-19: A multicentre study. Eur. Heart J. Cardiovasc. Imaging. https://doi.org/10.1093/ehjci/jeab067 (2021).
Szekely, Y. et al. Spectrum of cardiac manifestations in COVID-19: A systematic echocardiographic study. Circulation 142, 342–353 (2020).
van den Heuvel, F. M. A. et al. Cardiac function in relation to myocardial injury in hospitalised patients with COVID-19. Neth. Heart J. 28, 410–417 (2020).
Vasudev, R. et al. The utility of bedside echocardiography in critically ill COVID-19 patients: Early observational findings from three Northern New Jersey hospitals. Echocardiography 37, 1362–1365 (2020).
Wats, K. et al. Association of right ventricular dysfunction and pulmonary hypertension with adverse 30-day outcomes in COVID-19 patients. Pulm. Circ. 11, 204589402110070 (2021).
Woolf, S. H., Chapman, D. A. & Lee, J. H. COVID-19 as the leading cause of death in the United States. JAMA. https://doi.org/10.1001/jama.2020.24865 (2020).
Lang, J. P. et al. A current review of COVID-19 for the cardiovascular specialist. Am. Heart J. 226, 29–44 (2020).
Vieillard-Baron, A., Price, L. C. & Matthay, M. A. Acute cor pulmonale in ARDS. Intens. Care Med. 39, 1836–1838 (2013).
Libby, P. & Lüscher, T. COVID-19 is, in the end, an endothelial disease. Eur. Heart J. 41, 3038–3044 (2020).
Park, J. F., Banerjee, S. & Umar, S. In the eye of the storm: The right ventricle in COVID-19. Pulm. Circ. 10, 204589402093666 (2020).
Cao, Y., Zhang, M., Guo, Y. & Zhang, Y. The overlooked chamber in coronavirus disease 2019. ESC Heart Fail. 7, 3483–3486 (2020).
Bompard, F. et al. Pulmonary embolism in patients with COVID-19 pneumonia. Eur. Respir. J. 56, 2001365 (2020).
Middeldorp, S. et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J. Thromb. Haemost. 18, 1995–2002 (2020).
Pirzada, A., Mokhtar, A. T. & Moeller, A. D. COVID-19 and myocarditis: What do we know so far? CJC Open 2, 278–285 (2020).
Biteker, F. S. et al. Prognostic value of transthoracic echocardiography and biomarkers of cardiac dysfunction in community-acquired pneumonia. Clin. Microbiol. Infect. 22, e1–e6 (2016).
Lazzeri, C., Bonizzoli, M., Batacchi, S. & Peris, A. Echocardiographic assessment of the right ventricle in COVID-related acute respiratory syndrome. Intern. Emerg. Med. https://doi.org/10.1007/s11739-020-02494-x (2020).
Author information
Authors and Affiliations
Contributions
B.C., A.M.M., M.P. and G.F.R. conceived and designed the study, and drafted the first version of the manuscript; B.C. and G.F.R. acquired and analyzed the data; B.C., A.M.M., S.B., R.C., A.C., M.P. and G.F.R. revised the manuscript critically and gave final approval of the version to be submitted.
Corresponding author
Ethics declarations
Competing interests
AC: unrestricted grants from Merck-Serono; AMM: advisory board and lecture fees from MSD. SB received research grants from MSD, outside the scope of this study. The other authors have nothing to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Corica, B., Marra, A.M., Basili, S. et al. Prevalence of right ventricular dysfunction and impact on all-cause death in hospitalized patients with COVID-19: a systematic review and meta-analysis. Sci Rep 11, 17774 (2021). https://doi.org/10.1038/s41598-021-96955-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96955-8
This article is cited by
-
Acute and Post-Acute COVID-19 Cardiovascular Complications: A Comprehensive Review
Cardiovascular Drugs and Therapy (2023)
-
Diagnosis and treatment of right ventricular dysfunction in patients with COVID-19 on veno-venous extra-corporeal membrane oxygenation
Journal of Cardiothoracic Surgery (2022)
-
Echocardiographic estimation of pulmonary hypertension in COVID-19 patients
Netherlands Heart Journal (2022)
-
Role of prognostic scores in predicting in-hospital mortality and failure of non-invasive ventilation in adults with COVID-19
Internal and Emergency Medicine (2022)
-
Characterising right ventricular dysfunction in acute respiratory distress syndrome due to COVID-19: which measurements are best?
Intensive Care Medicine (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.