Abstract
Post fever retinitis is a heterogenous entity that is seen 2–4 weeks after a systemic febrile illness in an immunocompetent individual. It may occur following bacterial, viruses, or protozoal infection. Optical coherence angiography (OCTA) is a newer non-invasive modality that is an alternative to fundus fluorescein angiography to image the retinal microvasculature. We hereby describe the vascular changes during the acute phase of post fever retinitis on OCTA. Imaging on OCTA was done for all patients with post fever retinitis at presentation with 3 × 3 mm and 8 × 8 mm scans centred on the macula and corresponding enface optical coherence tomography (OCT) scans obtained. A qualitative and quantitative analysis was done for all images. 46 eyes of 33 patients were included in the study. Salient features noted were changes in the superficial (SCP) and deep capillary plexus (DCP) with capillary rarefaction and irregularity of larger vessels in the SCP. The DCP had more capillary rarefaction when compared to the SCP. The foveal avascular zone (FAZ) was altered with an irregular perifoveal network. Our series of post fever retinitis describes the salient vascular features on OCTA. Although the presumed aetiology was different in all our patients, they developed similar changes on OCTA. While OCTA is not useful if there is gross macular oedema, the altered FAZ can be indicative of macular ischemia.
Similar content being viewed by others
Introduction
Post fever retinitis is seen 2–4 weeks after a systemic febrile illness caused by either bacteria, viruses, or protozoa, in an immunocompetent individual1. Uveo-retinal manifestations include solitary or multifocal patches of retinitis, localised or generalised involvement of the retinal vessels in the form of beading of the vessel wall, tortuosity, and perivascular sheathing, and macular serous detachment or oedema, and optic nerve involvement1,2. Optical coherence tomography angiography (OCTA) is a recent advancement which is a non-invasive alternative to fundus fluorescein angiography (FFA) and indocyanine green angiography (ICGA) to assess the retinal and choroidal microvasculature3,4. Dye-based angiography has been found to be useful in assessing retinal vascular involvement and in detecting occlusive complications in retinitis5. Extensive leakage of the dye may obscure adequate visualisation of microvasculature in eyes with retinitis. Compared with FFA and Indocyanine green angiography (ICGA), which are the current retinal/choroidal angiographic gold standards, OCTA acquires volumetric scans that can be segmented to specific depths, uses motion contrast instead of intravenous dye, can be obtained within seconds, provides accurate size and localization information and delineates both the retinal and choroidal vasculature. Disadvantages are its limited field of view, inability to demonstrate leakage, increased potential for artifacts (blinks, movement, vessel ghosting), and inability to detect blood flow below the slowest detectable flow6,7,8,9,10,11.
Standard enhanced depth imaging (EDI) optical coherence tomography (OCT) is only capable of showing the structure of choroid and choriocapillaris. However, the OCTA, being rapid, non-invasive and repeatable, is useful for the assessment of the foveal avascular zone (FAZ) and microvascular changes along with segmental imaging and evaluation of the superficial capillary plexus (SCP) and deep capillary plexus (DCP) in several retinal vascular diseases6,7,8,9,10,11. FAZ and capillary density can be measured at both the SCP and DCP12. Despite the lack of standardised protocols for image acquisition and interpretation of image scans, OCTA is widely used for the detection of pathophysiology, early diagnosis, treatment and determination of the progression in patients, especially with vascular pathology4. It provides good delineation of the pathology along with volumetric data with the ability to show both structural and blood flow information5. It can therefore be vital in understanding the vascular changes in eyes with post fever retinitis.
Methods
This prospective, observational, cross-sectional study with protocol title “FAVOUR”: “Fever Associated Visual Outcome in Uvea and Retina” was approved by the Narayana Nethralaya Hospital Ethics Committee (EC Ref No: C/2018/08/05).
The research followed the tenets of the declaration of Helsinki and an informed written consent was obtained from all study subjects.
The study included 46 eyes of 33 patients who presented with post fever retinitis between August 2018 and July 2020. All patients underwent imaging at presentation to our tertiary eye center on a spectral domain (SD) OCTA system (ANGIOVUE, OPTOVUE, Inc., Fremont, CA, USA) using the Split Spectrum Amplitude Decorrelation Angiography (SSADA) algorithm to quantify vasculature structure, the FAZ, and the superficial and deep retinal vascular plexus densities, by a single trained operator. Scan areas of 3 × 3 mm and 8 × 8 mm centred on the fovea for imaging both superficial and deep retinal plexus were obtained separately for each patient similar to what we have described earlier13. The OCT scanner has a scan speed of 70,000 A-scans per second with 304 A scans per B-scan and 304 B-scans per volume. The axial and transverse resolution of the device is 5 µm and 15 µm, respectively. If the signal strength index was less than 40, the scans were repeated and those with poor signal strength were not included.
Tropicamide 1% eye drops was used for dilatation of pupil in all patients. A total of 5 scans were acquired for every patient using an internal fixation target. Only the best quality scans were chosen for analyses. Exclusion criteria for OCTA images were those with motion artefacts, double vessels or undue stretching of vessels. Foveal centre for OCTA images was correlated with OCT scans at the same levels. A parafoveal ring of 1–2.5 mm diameter, proportional to the total area was used for analysis relative to the density of vascular flow.
Non flow mode in SCP and DCP was used to measure the FAZ. ANGIOANALYTICS (OPTOVUE, Inc., Fremont, CA, USA) blood vessel measurement was used to measure automated vessel flow density. Segmentation was performed both by automated and manual techniques, especially in case of gross oedema or poor scan features.
Local fractal dimension was used to represent the presence of vessels in OCTA scans13. Calculation of the ratio of local fractal dimension of each pixel in an OCTA image to the maximum fractal dimension was done as described in earlier13. Coloured contour, normalised ratio to provide a pictorial representation of an apparent probability index of the presence of vessel was done. Visual comparison of the normalized ratio map with the OCTA image was used to develop a scoring system. The vessel density was computed as a percentage, by counting all the pixels with a normalized ratio between 0.7 and 1.0 and then dividing by the total number of pixels in the OCTA image13. Capillary dropouts is a significant parameter to distinguish between normal and diseased eyes. In this study, capillary dropouts were labeled as "spacing between large vessels" and "spacing between small vessels". Spacing between or around the large vessels with a normalized ratio between 0.0 and 0.3 were considered. Pixels in regions around closely packed small vessels, which may be branching out from a large vessel or surrounding small vessels, with a normalized ratio between 0.3 and 0.7 were termed as “spacing between small vessels”13.
Gadde et al. have described local fractal dimension to calculate vessel density and FAZ area in a normal healthy Asian Indian population13. Quantification of vascular parameters can be affected by projection artefacts (PAs) in the DCP. Govindaswamy et al.14 have described the methodology to reduce the PAs.
The inbuilt software from the instrument allows the users to choose flow and non-flow area on a selected layer. OCTA indices from local fractal analysis differentiate the large and small vessel regions of the non-flow area13. Thus we used custom OCTA metrics rather than using inbuilt software of the machine for the quantitative analysis.
Deep capillary plexus was found to be the affected initially in most of the retinal vascular disorders. We have previously reported that a significant vascular loss in different grades of diabetic retinopathy at the level of deep vascular plexus after removal of projection artifacts. Before the removal of projection artefacts, this was not apparent with the presence of projection artefacts2. Our approach is software-based where a normalized cross-correlation between superficial and deep layer was estimated as a scaling factor to subtract the projection artifact. Hence, it can be presumed that irrespective of the instrument used to obtain and the algorithm used to re-construct angio images, the software-based approach would provide comparable results.
Conference presentation
Oral presentation at a meeting: Preliminary data at 35th Singapore-Malaysia Joint Meeting in Ophthalmology in conjunction with the 1st Asia–Pacific Ocular Imaging Society Meeting, held from 17 to 19 January 2020 at the Academia, Singapore General Hospital Campus.
Informed consent
Written Informed consent was obtained from all study subjects.
Results
Thirty-three consecutive patients with post fever retinitis (46 eyes, 13 bilateral) in the age 18–73 years (median age 40 years) who underwent OCTA between August 2018 and July 2020 were included in the study (Male:Female—17:16). The presumed etiologies for the post fever retinitis were dengue, rickettsia and typhoid fever based on the serology as illustrated in Table 1. The predominant clinical picture was of multifocal retinitis with macular oedema.
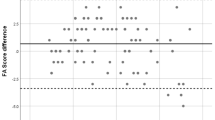
Quantitative analysis
Figure 1 shows the pre and post removal of projection artefact (PAs). In the SCP, the large vessel spacing was increased with small vessel spacing similar to a normative data. The DCP was more affected in terms of small and large vessel spacing and the vessel density was also significantly lower.
The FAZ was not affected during the acute stage in both the SCP and DCP. Figure 2 shows the fractal analysis after removal of the artefacts. The vascular parameters of small and large vessels in the superficial capillary and deep capillary layers are shown in Table 2.
Optical coherence tomography angiography (OCTA) image of superficial (a) and deep layer after removal of projection artifacts (b). (c, d) are the respective images after fractal analysis. Regions in red pixels correspond to vessels, blue corresponds to large vessel spacing, and yellow corresponds to small vessel spacing.
Qualitative analysis
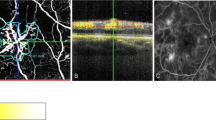
Salient features of active retinitis on OCTA included changes in both SCP and DCP with capillary rarefaction and irregularity of larger vessels in SCP. Pruning of the vessels was noted in SCP and DCP. The FAZ was altered with a broken perifoveal network suggestive of macular ischaemia on 3 × 3 mm scans in patients with active retinitis and areas of retinal thinning on OCT. Capillary rarefaction was better appreciated in the DCP than SCP. Bright hyper-reflective material on OCT was seen corresponding to the areas of capillary rarefaction and artefacts at DCP. The choriocapillaris (CC) layer had a loss of the normal coarse architecture corresponding to areas of retinal oedema on OCT and on the enface image. Both intra retinal and sub retinal oedema had a shadowing effect on the DCP, outer retina (OR) and CC layer causing artefacts thus impeding an accurate measurement of the vascular density and confirmation of the dropout areas. Middle retinal thickening, highly reflective spots (HRS) and hard exudates were seen as bright areas in the DCP and CC and in the OR in some scans. These areas of HRS with middle retinal oedema causing radial striations in the Henle’s layer were more apparent in the CC layer, which may reverse with disease resolution. Inner retinal thickening and middle retinal thickening corresponded with capillary rarefaction in the SCP and DCP, respectively. FAZ enlargement could not be accurately documented in all patients as many presented with macular edema during the acute phase. Figures 3 and 4 shows an OCTA 3X3mm scan in mild and severe intra retinal edema, respectively. Figure 5 shows CC layer with enface projection of active retinitis. Figure 6 shows an 8X8 mm scan which is useful to detect the extent of retinitis, but has poorer vascular resolution compared to 3X3 scans.
(Patient 24) OCTA: 3 mm × 3 mm section. SCP—Capillary rarefaction seen between larger vessels. FAZ maintained. Beading and aneurysmal dilatation of perifoveal vasculature (yellow arrow). DCP—Diffuse capillary rarefaction seen as radial darker stripes (green arrow) corresponding to retinal oedema in Henle’s layer. Areas of pruning noted in the smaller network of vessels. OR—Projection artifacts with darker radial lines continuing in the avascular layer. CC—Loss of the regular coarse architecture. A better appreciation of the darker radial striations corresponding to oedema in the Henle’s layer (green arrow). OCT showing mild intraretinal oedema and HRS and SRF with subretinal hyperreflectivity. OCTA Optical coherence tomography angiography. SCP Superficial capillary plexus, DCP Deep capillary plexus, OR Outer retina, CC Choriocapillaries, OCT Optical coherence tomography, FAZ Foveal avascular zone, HRS Hyperreflective spots.
(Patient 33) OCTA: 3 mm × 3 mm scans of SCP, DCP, OR and CC layers. SCP: Extensive capillary rarefaction in between larger vessels and gross distortion of the FAZ landmarks owing to the significant oedema. (yellow circle). DCP: Projection artefacts with poor demarcation of finer vascular network and a totally lost FAZ due to intraretinal oedema (green arrow). Avascular areas of FAZ showing HR brighter areas due to suspending particle artifacts. OR: Few areas of brighter areas due to the overlying projection artifacts. (red D). CC: Changes in the coarse architecture. Radial striations well delineated due to the oedema in Henle’s layer. OCT: Active retinitis with extensive intra retinal oedema, HRS in all the retinal layers and subretinal hyper reflective material. OCTA Optical coherence tomography angiography, SCP Superficial capillary plexus, DCP Deep capillary plexus, OR Outer retina, CC Choriocapillaries, OCT Optical coherence tomography, FAZ Foveal avascular zone, HRS Hyperreflective spots.
(Patient 24) OCTA 8 mm × 8 mm scan: Larger scan sections show the extent of retinal involvement in active retinitis. Larger vessels in SCP can be seen. Finer vasculature in SCP and DCP are poorly appreciated due to lesser resolution in larger scans. The macular involvement can be estimated from DCP onwards. A CC section shows the radial striations with brighter signals corresponding to the intraretinal HRS. A corresponding OCT B scan shows the severity and retinal involvement. OCTA Optical coherence tomography angiography, SCP Superficial capillary plexus, DCP Deep capillary plexus, OR Outer retina, CC Choriocapillaries, OCT Optical coherence tomography, FAZ Foveal avascular zone, HRS Hyperreflective spots.
Discussion
OCTA has the ability to non-invasively provide details of retinal and choroidal vasculature, which helps us better understand the microvascular changes in eyes with retinitis, which cannot be delineated well on FFA due to the vascular leakage in inflammatory conditions.11 Few studies in post fever retinitis have described changes in the SCP/DCP following dengue and chikungunya retinitis15,16,17. Agarwal et al. reported that there were flow void areas in the SCP, DCP and choriocapillaris slabs in chikungunya retinitis14. Aggarwal et al. have also described the OCTA features in acute macular neuro-retinopathy post dengue fever showing disruption of both the SCP and DCP, flow deficit in the foveal region and an increase in the FAZ. They propose that the presence of hairpin loop configuration of the adjacent retinal capillaries is suggestive of retinal capillary ischaemia, which persisted even at their last follow up16. Bajgai et al.17 noted a broken FAZ in only the SCP of OCTA in a case of dengue maculopathy and these changes persisted at follow‑up visits. Kahloun et al.18 described hypointense areas in the SCP/DCP but larger hypointense areas in the DCP/OR/CC on their swept source (SS) OCTA in a patient with rickettsial retinitis. On follow up six weeks later the hypointense greyish areas of retinal capillary nonperfusion persisted in both SCP/DCP18.
Khatri et al.19,20 have described microaneurysms (MA) on OCTA based on their signals. MAs were classified as high flow MA s and low flow MAs. High Flow MAs show a signal on OCTA. Due to pericyte loss however these high flow MAs are prone to thickening of macula due to leakage and are often are located in the DCP. Nearly three quarters of them were located adjoining cystoid spaces.
Low Flow MAs do not appear on OCTA, they may however be visible on fundus photo or other enhanced techniques.
Schreur et al.21 in their study of retinal MA in patients with diabetic macular edema (DME) by OCTA found that MA with focal leakage and located in a thickened retinal area were more likely to be detected on OCTA. In their study MAs were located in intermediate and deep plexus.
In our series of post fever retinitis, microvascular abnormalities were noted in the SCP and DCP with quantifiable changes in both the smaller and larger vessels. Capillary rarefaction areas corresponding to retinitis patches and pruning of vessels was seen in the active phase. The DCP showed profound capillary rarefaction when compared to the SCP due to the involvement of the middle retinal layers. Our series did not show any individual MAs on OCTA. The CC slabs showed signal void areas which can be attributed to shadowing caused by the overlying retinitis patch similar that reported by Shanmugam et al.22 The regular vascular pattern or the “angio-architecture” in SCP and DCP was lost in active retinitis, the intraretinal edema and exudation causing an impression of vessel drop out. The flow void areas in the choriocapillaris layer are due to the shadow effect of the superficial edema on to the choroid resulting in loss of the regular coarse architecture. These changes are reversible in non-ischemic retinas once the active inflammation subsides.
In a patient with post typhoid fever neuroretinitis, OCTA showed macular thickening and neuro sensory detachment. Choroidal imaging showed abnormal “patchy” flow voids in the choriocapillaris-likely suggestive of a sluggish blood flow or ischemia. Deep range imaging (DRI) of the choroid revealed increased choroidal thickness and dilated choroidal vasculature, indicating a concurrent choroidal inflammation23.
In our series choroidal imaging had artifacts in acute stages due to intraretinal fluid. In cases where choroidal imaging was possible, we noted altered choroidal architecture with darker areas. We will be, in a future study of these patients analyse the choroidal architecture during the follow up of our patients.
A study of OCTA in a patient with varicella retinal vasculopathy showed loss of capillary plexus in both SCP and DCP24.
OCTA has also been useful in choroidal imaging as described in a case of sympathetic ophthalmia.OCTA of the choroidal vascular revealed flow void pockets initially at inflammatory stage, and this normalized over time into typical granular pattern after initiation of the treatment25.
Despite the advantages of being non-invasive and repeatable, OCTA has certain limitations in active retinitis. Its interpretation can be challenging due to projection and motion artifacts and retinal edema due to active retinitis causing an impression of vessel drop out and a loss of the regular “angio-architecture” due to vessel displacements, pruning effects and non-flow areas in edematous areas. The interpretation of OCTA and particularly the FAZ is difficult in patients with gross macular edema and will need longitudinal follow up to assess for enlargement, distortion and possible ischemia.
Other limitations include a relatively small field of view, inability to show leakage, and proclivity for image artifact due to patient eye movement/blinking. Manual segmentation can be tedious and time consuming. The variations in capillary density or vascular thickness are influenced by the type of segmentation. We overcame this limitation by having two observers performing the manual segmentation, comparing the findings and taking the average of the two readings.
Conclusion
Ours is the largest series of OCTA of retinal vasculature findings in post fever retinitis. Although the presumed etiology was different in our patients, they developed similar changes on OCTA. Quantitative analysis confirmed that the insult was more in the DCP. Serial follow up of these patients will help unravel the vascular changes on the road to recovery.
References
Sanjay, S. et al. Post fever uveoretinal manifestations in an immunocompetent individual. EMJ Allergy Immunol. 5, 91–105 (2020).
Kawali, A., Mahendradas, P., Mohan, A., Mallavarapu, M. & Shetty, B. Epidemic retinitis. Ocul. Immunol. Inflamm. 1, 1–7 (2018).
Gorczynska, I., Migacz, J., Zawadzki, R., Capps, A. & Werner, J. Comparison of amplitude-decorrelation, speckle-variance and phase-variance OCT angiography methods for imaging the human retina and choroid. Biomed. Opt. Express. 7, 911–942 (2016).
de Carlo, T., Romano, A. & Waheed, N. A review of optical coherence tomography angiography (OCTA). Int. J. Retina Vitreous 1, 5 (2015).
Spaide, R., Klancnik, J. & Cooney, M. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 133, 45–50 (2015).
Khairallah, M. et al. Optical coherence tomography angiography in patients with Behçet uveitis. Retina 37, 1678–1691 (2017).
Couturier, A. et al. Capillary plexus anomalies in diabetic retinopathy on optical coherence tomography angiography. Retina 35, 2384–2391 (2015).
Coscas, F., Glacet-Bernard, A. & Miere, A. Optical coherence tomography angiography in retinal vein occlusion: Evaluation of superficial and deep capillary plexa. Am. J. Ophthalmol. 161, 160–171 (2016).
Sanfilippo, C. J., Klufas, M. A., Sarraf, D. & Tsui, I. Optical coherence tomography angiography of sickle cell maculopathy. Retin. Cases Brief Rep. 9, 360–362 (2015).
Minvielle, W. et al. Macular microangiopathy in sickle cell disease using optical coherence tomography angiography. Am. J. Ophthalmol. 164, 137–144 (2016).
Chalam, K. V. & Sambhav, K. Optical coherence tomography angiography in retinal diseases. J. Ophthal. Vis. Res. 11, 84–92 (2016).
Sioufi, K., Say, E. A. T., Ferenczy, S. C., Leahey, A. M. & Shields, C. L. Optical coherence tomography angiography findings of deep capillary plexus microischemia after intravenous chemotherapy for retinoblastoma. Retina 39, 371–378 (2019).
Gadde, S. G. et al. Quantification of vessel density in retinal optical coherence tomography angiography images using local fractal dimension. Invest. Ophthalmol. Vis. Sci. 57, 246–252 (2016).
Govindaswamy, N. et al. Quantitative evaluation of optical coherence tomography angiography images of diabetic retinopathy eyes before and after removal of projection artifacts. J. Biophoton. 11, e201800003 (2018).
Agarwal, A., Choudhary, T. & Gupta, V. Optical coherence tomography angiography features of bilateral retinopathy associated with Chikungunya fever. Indian J. Ophthalmol. 66, 142–145 (2018).
Aggarwal, K., Agarwal, A., Katoch, D., Sharma, M. & Gupta, V. Optical coherence tomography angiography features of acute macular neuroretinopathy in dengue fever. Indian J. Ophthalmol. 65, 1235–1238 (2017).
Bajgai, P., Singh, R. & Kapil, A. Progression of dengue maculopathy on OCT-angiography and fundus photography. Ophthalmology 124, 1816 (2017).
Kahloun, R. et al. Swept-source optical coherence tomography angiography in Rickettsial retinitis. Retin. Cases Brief Rep. 13, 348–351 (2019).
Khatri, A. et al. Detection, localization, and characterization of vision-threatening features of microaneurysms using optical coherence tomography angiography in diabetic maculopathy. Eur. J. Ophthalmol. https://doi.org/10.1177/1120672120924609 (2020).
Khatri, A., Bal Kumar, C., Kharel, M., Ashma, K. C. & Pradhan, E. Analysis of microaneurysms and capillary density quantified by OCT-angiography and its relation to macular edema and macular ischemia in diabetic maculopathy. Eye 35(6), 1777–1779. https://doi.org/10.1038/s41433-020-1060-4 (2021).
Schreur, V. et al. Morphological and topographical appearance of microaneurysms on optical coherence tomography angiography. Br. J. Ophthalmol. https://doi.org/10.1136/bjophthalmol-2018-312258 (2018).
Shanmugam, M. et al. Optical coherence tomography angiography features of retinitis post-rickettsial fever. Indian J. Ophthalmol. 67, 297–300 (2019).
Khatri, A. et al. Post typhoid fever neuroretinitis with serous retinal detachment and choroidal involvement: A case report. Am. J. Ophthalmol. Case Rep. 21, 101025. https://doi.org/10.1016/j.ajoc.2021.101025 (2021).
Khatri, A., Timalsena, S., Gautam, S. & Kharel, M. Varicella retinal vasculopathy: Unilateral cilioretinal artery occlusion despite acyclovir therapy caught using optical coherence tomography-angiography (OCTA). Case Rep. Ophthalmol. Med. 2019, 5752180. https://doi.org/10.1155/2019/5752180 (2019).
Khatri, A. et al. A rare entity: Sympathetic ophthalmia presumably after blunt trauma to the phthisical eye and optical coherence tomography angiography metrics to monitor response to treatment. Clin. Case Rep. 8, 149–154. https://doi.org/10.1002/ccr3.2597 (2019).
Author information
Authors and Affiliations
Contributions
S.S.: Design, Acquisition of data, Analysis and interpretation, Manuscript writing, Manuscript editing, Intellectual content. S.G.K.G.: Design, Acquisition of data, Analysis and interpretation, Manuscript editing, Intellectual content. S.A.: Acquisition of data, Manuscript writing, Manuscript editing. P.M.: Design, Analysis and interpretation, Manuscript writing, Manuscript editing, Intellectual content. N.G.: Acquisition of data, Analysis and interpretation, Intellectual content. A.K.: Analysis and interpretation, Manuscript writing, Manuscript editing. C.J.: Analysis and interpretation, Manuscript writing, Manuscript editing. S.S.: Acquisition of data, Analysis and interpretation, Manuscript writing. A.S.R.: Acquisition of data, Analysis and interpretation, Manuscript writing. R.S.: Design, Manuscript editing, Intellectual content. Figures: S.G.K.G., S.A. and S.S. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sanjay, S., Gadde, S.G.K., Agrawal, S. et al. Optical coherence tomography angiography (OCTA) of retinal vasculature in patients with post fever retinitis: a qualitative and quantitative analysis. Sci Rep 11, 17647 (2021). https://doi.org/10.1038/s41598-021-96715-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96715-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.