Abstract
Hypertension (HTN) and osteoarthritis (OA) are frequent in middle-aged and elderly people, and the co-occurrence of these two diseases is common. However, the pathogenesis of the multimorbidity of both diseases and the relation with sleep quality, hyperlipemia, and hyperglycemia is unclear. We conducted a cross-sectional study to make sense of the multimorbidity of HTN and OA and the relation with sleep quality, hyperlipemia, and hyperglycemia. The relation between sleep quality and OA and its joint effect with hyperlipemia or hyperglycemia was evaluated with logistic regression models. The additive interaction was assessed with the relative excess risk due to interaction (REEI), the attributable proportion (AP), and the synergy index (S). According to this research in a remote rural area, approximately 34.2% of HTN patients are accompanied with OA and 49.1% are suffering poor sleep. Both hyperlipemia/hyperglycemia and sleep quality were related to OA prevalence with crude ORs of 1.43 (95% CI 1.014–2.029) and 1.89 (95% CI 1.411–2.519, P < 0.001) respectively. An observed additive effect was found greater than the sum of the effects of sleep quality and hyperlipemia/hyperglycemia posed on OA prevalence alone. This additive interaction was observed in females (OR = 3.19, 95% CI 1.945–5.237) as well as males ≥ 65 years old (OR = 2.78, 95% CI 1.693–4.557), with RERI, AP, and S significant. Therefore, poor sleep and hyperlipemia/hyperglycemia are associated with OA, and further studies on the additive interaction among females and males ≥ 65 are warranted.
Similar content being viewed by others
Introduction
Age-associated multimorbidity has been a common but complex issue over the world, which means the coexistence of several chronic diseases in a person for a long period1,2. Due to the high prevalence, every year multimorbidity caused a major burden on personal health and for social cost in regions including Asia3,4.
Based on the researches to date, about half of chronic disease patients had comorbidities, and multimorbidity was common to see in patients with hypertension (HTN) and osteoarthritis (OA). According to a South African primary healthcare study, 23.70% of OA patients and 12.00% of HTN patients have comorbidities5. As a developing country with a huge population, China shows a similar situation in co-existing diseases in 28.78% and 21.29% of patients respectively with OA and HTN3.
Among the many comorbidities, the multimorbidity of HTN and OA occurred frequently6,7. Epidemiological studies have found that HTN patients significantly have a 1.394 times higher risk of OA, with the comorbidity rate ranged from 20 to 80% in both developed and developing countries8. Although OA was not the most common comorbid disease in HTN, the risk—a prevalent pathology of cartilage in joints, a leading cause of disability, a primary factor of decreased life quality, as well as a high rate of hospitalization—makes it an important topic and worthy to study especially since corresponding research among the Chinese population is limited4,9,10. Further, learning more about OA does help in minimizing the adverse impact on blood pressure control in hypertensive patients.
Following more reports on OA and cardiovascular risk factors, interest in relevant mechanisms and factors between OA and HTN is increasing. Factors associated with this multimorbidity were complex and various, mainly including age, sex, and quality of life11,12, and related population-based studies seem to favor the etiology of ischemia and lipid metabolism with HTN. They thought HTN might decrease peripheral blood flow, resulting in subchondral ischemia and osteocyte cell death13; deregulated lipid metabolism, a possible strong OA determinant, might induce ectopic lipid deposition, initiating OA development14. However, it has not been adequately addressed and no unified conclusion has been drawn.
Adding to the confusion, more sleep disorders, shorter sleep duration, and poorer sleep quality are likely to the complaint of OA, and have been demonstrated to be a risk of HTN. For example, hypertension risk might be increased by sleep disorders, especially sleep deprivation15 and inappropriate sleep duration16, while some studies suggested that sleep disturbance might increase the occurrence of OA17,18, as does the finding might be associated with HTN19. On the contrary, another study pointed that the presence of chronic OA has the potential to increase the risk for incurring sleep disturbances20. It is easy to see there is a limited understanding of the link between sleep quality and OA up to now.
As possible factors associated with OA, the interaction effect between metabolic syndrome (including hyperglycemia and hyperlipidemia) and sleep has not been specifically studied with OA prevalence as an endpoint, much fewer patients with HTN out of that. Therefore, if there is an interaction between sleep and hyperglycemia/hyperlipidemia to the prevalence of OA, then it brings a sense of enlightenment to implement preventive behaviors for protection and control. Besides, it may provide a possible recommendation for combinational therapy and nursing for OA and HTN in clinical practices. Consequently, it is necessary to conduct this study to make up the gap.
In summary, sleep quality, lipid metabolism, OA, and HTN are intertwined, very complex, and not fully elucidated. We included hypertensive patients in a poverty-stricken rural area to make clear the OA prevalence and to ascertain the relation of sleep quality and hyperlipidemia/hyperglycemia with the prevalence of OA, and further to confirm the interaction effect between them.
Materials and methods
Study population
This cross-sectional study included HTN patients from Xuan’en county in a remote mountainous area of central China. All participants are local inhabitants over 18 years old and volunteered to participate, and they have no obstacle in communication. HTN was defined as systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg, or current use of antihypertensive medication. The sample size was estimated with the average prevalence of hypertension in China with the equation: \(n={{Z}_{(\alpha /2)}}^{2}\times p\times (1-p)/{\delta }^{2}\), where \(\alpha\) is 0.05, \(\delta\) is 0.15p, and p is 30%. To compensate for the non-response rate, the sample was increased by 10% with a final sample size of 685. The study followed the guidelines of the Declaration of Helsinki, and ethical approval and informed consent were obtained.
Data collection
The current cross-sectional data were collected from April to July 2018. Data collection took place in two stages: in the first stage, the study collected a broad range of information on sociodemographic characteristics (e.g. sex, age, marital status, monthly income, education level, place of residency), health-related conditions (e.g. BP value, height, weight, waist, hist), and doctor-diagnosed or self-reported OA (yes or no), hyperlipemia, and hyperglycemia. The second stage comprised face-to-face interviews with structured questionnaires to make sense of their sleep quality and compliance with hypertension.
BP values were taken three times using a mercury gauge sphygmomanometer. Consecutive BP measurements were taken at 5-min intervals from the right arm by our investigators, and the average was used for analysis. The information on participants’ sleep quality was gathered with the standard Pittsburgh Sleep Quality Index (PSQI). Seven dimensions were used to describe participants’ sleep quality, including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, sleep medication, and daytime dysfunction. The total score of the PSQI scale ranges from 0 to 21, with lower scores indicating better sleep quality. Compliance of hypertension was measured using the Compliance of Hypertensive Patients’ scale (CHPS), which contained 14 items. Items were evaluated with a 4-point Likert scale, where a higher score indicated a higher level of compliance.
Statistical analysis
Continuous variables are described as means ± standard deviations (M ± SD) and median (interquartile range [IQR]), while frequency and percentages are presented for categorical variables. Differences in sample characteristics were assessed with a chi-squared test for categorical variables. Independent-sample t-test and Mann–Whitney U-test were used for normally distributed and skewed continuous variables.
The independent association between sleep quality and OA, as well as its joint effect (additive interaction) with hyperlipemia or hyperglycemia, were evaluated with logistic regression models after adjusting covariates. Sleep quality was divided into high group (or reference group) if the PQSI score ≤ 6 and low group > 6 scores. Results were illustrated as unadjusted and adjusted odds ratio (OR) and its 95% confidence interval (95% CI). According to Hosmer and Lemeshow21, additive interaction was assessed with the relative excess risk due to interaction (REEI), the attributable proportion (AP), and the synergy index (S); the 95% CIs for the former two indexes should not include 0 and the latter one should not include 1. We calculated RERI by using the formula:
All statistical analyses were performed using STATA version 14.0 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.), and comparisons with P-values < 0.05 were considered statistically significant.
Ethical statement
Ethics approval for this study was granted by the Research Ethics Boards of Wuhan University (project approval code: 2018-1602000-03-02). Informed consent was obtained from all survey participants.
Results
Characteristics of study participants
A total of 837 HTN individuals were comprised of 379 (45.3%) males and 458 (54.7%) females, aged from 30 to 96 years with a median of 69. About half (49.5%) participants were of Tujia nationality in this study area. Most participants were characterized with low education level (primary school and illiteracy accounted for 79.7%) and family monthly income (< ¥3000 accounted for 84.2%).
According to OA dichotomy
The total sample numbered 286 suffered from OA, accounting for 34.2% of the whole participants. Of which, 11 individuals were self-reported OA with typical symptoms like stiffness, swelling, and deformity, and their sleep quality (the P-values for total score and 7 dimensions in PSQI were above 0.10) and all demographic and clinical characteristics (Ps > 0.10) has good homogeneity with the doctor-diagnosed ones. So, they were involved in the analysis. Table 1 shows the distribution differences in the prevalence of OA by participants’ demographic, clinical, sleep, and compliance characteristics. OA prevalence varies in different ages (P = 0.001), sexes (P < 0.001), occupations (P = 0.023), educations (P < 0.001), monthly incomes (P = 0.013), sleep quality scores (P < 0.001), and several dimensions of PSQI except for sleep duration and sleep medicine.
According to hyperlipemia/hyperglycemia and sleep quality
Among the HTN individuals recruited in this study, 169 (20.2%) displayed symptoms of hyperlipemia or hyperglycemia while 411 (49.1%) manifested with low sleep quality. As seen in Table 2, hyperlipemia or hyperglycemia status were found different in HTN duration (P < 0.001), smoking (P = 0.002), alcohol (P = 0.001), all items in CHPS (Ps < 0.05), and several dimensions in PSQI (except for sleep latency, sleep duration, and sleep medicine). When categorizing the total participants according to their sleep quality, significant differences were in sex (P = 0.002), marriage (P = 0.027), occupation (P = 0.007), education (P = 0.001), HTN duration (P = 0.002), tea-drinking (P = 0.012), SBP (P = 0.034), and all dimensions in PSQI (Ps < 0.01) and CHPS (Ps < 0.05).
Association between PSQI and osteoarthritis
The association between PSQI and OA is shown in Table 3. Exposure to hyperlipemia/hyperglycemia and poor sleep quality were both associated with the prevalence of OA in unadjusted and adjusted models. For the participants who suffered hyperlipemia or hyperglycemia, the crude OR was 1.43 (95% CI 1.014–2.029, P = 0.042). Results were also significant in adjusted models (for model 1: 1.83, 95% CI 1.355–2.477, P < 0.001; for model 2: 1.52, 95% CI 1.049–2.214, P = 0.027).
Similar in HTN patients with poor sleep quality, the crude OR was 1.89 (95% CI 1.411–2.519, P < 0.001). The OR was 1.79 (95% CI 1.333–2.415, P < 0.001) after adjusting for sex, age, and occupation; the OR was 1.83 (95% CI 1.352–2.476, P < 0.001) adjusting for additional variables in CHPS.
Joint effects of sleep quality and hyperlipemia/hyperglycemia
Table 4 shows the additive effect of sleep quality with hyperlipemia/hyperglycemia on the prevalence of OA. In all participants, when compared with the reference group, the OR for individuals in low sleep quality and hyperlipemia/hyperglycemia was 2.52 (95% CI 1.377–4.609). The RERI, AP, and S were respectively 1.16 (95% CI − 0.099 to 2.413), 0.43 (95% CI 0.095–0.771), and 3.24 (95% CI 0.681–15.446) with no significance. Similar insignificant results approached in males, and people ≥ 65 or < 65.
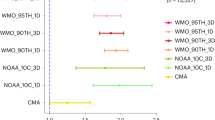
For females, the observed additive effect was greater than the sum of the effects of sleep quality and hyperlipemia/hyperglycemia alone: the OR of poor sleep quality was 1.68 (95% CI 1.200–2.340), hyperlipemia or hyperglycemia was 1.12 (95% CI 1.057–1.180), and poor sleep quality and hyperlipemia/hyperglycemia was 3.19 (95% CI 1.945–5.237). RERI (1.40, 95% CI 0.001–2.798), AP (0.44, 95% CI 0.173–0.704), and S (2.77, 95% CI 1.164–6.574) were statistically significant. (See details in Table 4 and Fig. 1).
We further conducted a sex-stratification analysis on top of age-stratification, and a positive interaction was noted both in males aged ≥ 65 and females aged ≥ 65. The degree of synergy for males ≥ 65 can be seen in Table 4 and Fig. 2: the OR of poor sleep quality, hyperlipemia or hyperglycemia, and poor sleep quality with hyperlipemia/hyperglycemia was respectively 1.53 (95% CI 1.135–2.074), 1.11 (95% CI 1.046–1.167), and 2.78 (95% CI 1.693–4.557). For females aged ≥ 65 years, the OR of poor sleep quality, hyperlipemia or hyperglycemia, and poor sleep quality and hyperlipemia/hyperglycemia was 1.63 (95% CI 1.389–1.904), 1.18 (95% CI 1.083–1.291), and 3.62 (95% CI 2.859–4.575). RERI, AP, and S were statistically significant. (See details in Table 4 and Fig. 3).
Discussion
Analysis of the data from Xuan’en area shows a 34.2% prevalence of OA in hypertensive individuals, indicating a not optimistic situation. Approximately 20.2% of HTN patients have hyperlipemia or hyperglycemia, and 49.1% are suffering poor sleep. In addition, poor sleep quality demonstrates a positive correlation with OA, and it also shows an additive effect with hyperlipemia or hyperglycemia among the males ≥ 65 years and females, especially those ≥ 65.
This investigation is a preliminary attempt to explore sleep quality and its additive relation with the multimorbidity of HTN and OA in a resource-limited mountainous area, central China. Epidemiological researches reveal that sleep problems are frequent in all populations and more than half of the elderly older than 65 suffer from it due to chronic diseases or external environments22. Notably, in this study, poor sleep showed a more pronounced tendency in HTN patients with OA, including subjective sleep, sleep latency, habitual sleep efficiency, sleep disturbances, daytime dysfunction, and total score, even after adjusting for covariates. This was similar to the findings from Regina et al.23,24. Besides, the multimorbidity of OA and HTN found here is much higher than China's overall level of 14.00%, according to China Health and Retirement Longitudinal Study3. Because Xuan’en is a poverty-stricken area with a large number of young people leaving for urban, complicated and diverse chronic diseases of the elderly as well as low-income level, inadequate health literacy, and the absence of adequate medical services undoubtedly constitute a huge threat to life health and quality. Given that rural elderly is still inferior in physical health to their counterparts in urban areas25, more medical resources and fundamental changes are advocated preferential to these regions. Therefore, more economical and convenient screening and referral to primary care is our most urgent concern.
Up to now, the bi-directional relation between sleep and OA has been a major point of discussion in publications concerning this domain, but the possible mechanism is not completely clear yet. A previous national study found a U-shape curve between the prevalence of OA and sleep duration with a nadir in the 7–8 h sleep category26. A case–control study additionally proved that sleep disorder was associated to a significant extent with higher odds of developing OA27. Based on the above ideas, we hypothesized that there would be direct or indirect associations between OA and sleep quality, and verified it in this study. Although accurate causal relation cannot be inferred due to the limitation of a cross-sectional study, it’s suggested that HTN patients with OA could be regularly screened for sleep disturbance with PSQI as a way to relieve the shortage of medical services and medicine. PSQI is a generic scale for measuring the quality and patterns of sleep in adults, and it could be of use for the management of OA and HTN patients28. It was shown to have strong reliability and validity with a sensitivity of 98.7 and specificity of 84.4 to differentiate sleep disturbances29. For the result in our additive interaction analysis, HTN patients aged ≥ 65 years, especially with hyperlipemia or hyperglycemia, are appropriate to use this self-reported instrument to warn of OA development or exacerbation in remote areas. However, to ensure the stability and feasibility of the results, it awaits to be confirmed by further researches.
Currently, the interactions between HTN, metabolism, sleep disorders, and OA are intertwined and complicated. The links between them are not fully elucidated, but a longitudinal study illustrated that poor sleep quality is associated with cardiovascular diseases (CVDs), in particular HTN, starting with microvascular dysfunction30. Other studies confirmed that increased BP is attributed to the metabolic syndrome-related mechanism due to poor sleep31,32. Metabolic syndrome, especially abnormal lipid metabolism, also contributed to the formation and development of OA14. All these might provide an idea for explaining a higher prevalence of OA among HTN accompanied by poor sleep quality and hyperlipemia/hyperglycemia in this research. The link between lipid metabolism, sleep quality, and HTN further strengthens the importance of fostering optimal sleep in preventing or ameliorating the development of OA.
Furthermore, it is novel and attractive in finding a significant additive effect among females after adjusting for age. So far, the only evidence for a gender-age difference has been through several works of literature, the overall prevalence of OA and CVDs (including hypertension, hyperlipemia et al.) was separately higher in females compared to males over the age of 5033,34. The explanation for the higher multimorbidity of HTN and OA in females is associated with the estrogen level, as it correspondingly decreased after peak menopausal age35. That, plus the fact that females are more vulnerable to poor sleep than males, may explain why the joint effect of HTN, sleep quality, and hyperlipemia/hyperglycemia is more notable in females.
To our knowledge, this is the first study to report the additive interaction between sleep and hyperlipemia/hyperglycemia linked with OA prevalence. Nonetheless, several limitations should be addressed. Due to the study design of a cross-sectional study, no causal relationship between sleep quality and the prevalence of OA can be inferred. Therefore, it calls for more rigorous designs to identify predictive factors of sleep impairment in OA. Also, the absence of evaluation indexes that include the intensity of pain, quality of life, and condition of medication makes it difficult to clarify disease outcomes and turnover for HTN patients with OA. Because of a few studies and small samples, we are inspired to go into much depth on this topic in the future with more large-scale studies and multi-regional cooperations.
Conclusion
Poor sleep quality is common and troublesome among people with HTN complicated with OA, and it shows a positive correlation with the prevalence of OA. The additive interaction between HTN, hyperlipemia or hyperglycemia, and sleep quality was observed in females and males ≥ 65, but it was complex and not fully elucidated. Further studies on the links are warranted.
Data availability
The datasets generated for this research are available on request to the corresponding author.
Abbreviations
- HTN:
-
Hypertension
- OA:
-
Osteoarthritis
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- CHPS:
-
Compliance of Hypertensive Patients’ scale
- PSQI:
-
Pittsburgh Sleep Quality Index
- OR:
-
Odds ratio
- REEI:
-
Relative excess risk due to interaction
- AP:
-
Attributable proportion
- S:
-
Synergy index
- CVD:
-
Cardiovascular disease
References
Ingmar, S. & William, D. W. Does multimorbidity influence the occurrence rates of chronic conditions? A claims data based comparison of expected and observed prevalence rates. PLoS ONE 7(9), e45390 (2012).
Marengoni, A. et al. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am. J. Public Health 98(7), 1198–1200 (2008).
Yan, W. et al. Multimorbidity status of the elderly in China-research based on CHARLS data. Chin. J. Disease Control Prevent. 23(4), 426–430 (2019).
Pefoyo, A.-J.-K. et al. The increasing burden and complexity of multimorbidity. BMC Public Health 15(1), 415 (2015).
Lalkhen, H. & Robert, M. Multimorbidity in non-communicable diseases in South African primary healthcare. S. Afr. Med. J. 105(2), 134–138 (2015).
Sinnige, J. et al. Multimorbidity patterns in a primary care population aged 55 years and over. Fam. Pract. 32(5), 505–513 (2015).
Kim, H.-S. et al. Association between knee osteoarthritis, cardiovascular risk factors, and the Framingham Risk Score in South Koreans: A cross-sectional study. PLoS ONE 11(10), e165325 (2016).
Lee, S. et al. The prevalence of osteoarthritis and risk factors in the Korean population: The Sixth Korea National Health and Nutrition Examination Survey (VI-1, 2013). Korean J. Fam. Med. 40(3), 171–175 (2019).
Rocca, W.-A. et al. Prevalence of multimorbidity in a geographically defined American population: Patterns by age, sex, and race/ethnicity. Mayo Clin. Proc. 89(10), 1336–1349 (2014).
Barnett, K. et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 380(9836), 37–43 (2012).
Mini, G.-K. & Thankappan, K.-R. Pattern, correlates and implications of non-communicable disease multimorbidity among older adults in selected Indian states: A cross-sectional study. BMJ Open 7(3), e13529 (2017).
Pengpid, S. & Karl, P. Multimorbidity in chronic conditions: Public primary care patients in four greater Mekong countries. Int. J. Environ. Res. Public Health 14(9), 1019 (2017).
Findlay, D.-M. Vascular pathology and osteoarthritis. Rheumatology 46(12), 1763–1768 (2007).
Zhuo, Qi. et al. Metabolic syndrome meets osteoarthritis. Nat. Rev. Rheumatol. 8(12), 729–737 (2012).
Mirjat, A. A. et al. Factors influencing sleep quality and effects of sleep on hypertension. Sleep Vigilance. 4, 125–136 (2020).
Han, B. et al. Sleep and hypertension. Sleep Breathing. 24, 351–356 (2020).
Cho, Y. et al. Association between sleep duration and osteoarthritis and their prevalence in Koreans: A cross-sectional study. PLoS ONE 15(4), e230481 (2020).
Jung, J. H. et al. The association between osteoarthritis and sleep duration in Koreans: A nationwide cross-sectional observational study. Clin. Rheumatol. 37, 1653–1659 (2018).
Zhang, Y.-M., Wang, J. & Liu, X.-G. Association between hypertension and risk of knee osteoarthritis: A meta-analysis of observational studies. Medicine 96(32), e7584 (2017).
Parmelee, P., Tighe, C. & Dautovich, N. Sleep disturbance in osteoarthritis: Linkages with pain, disability, and depressive symptoms. Arthritis Care Res. 67, 358–365 (2015).
Hosmer, D., Lemeshow, S. Confidence interval estimation of interaction. Epidemiology. 3(5), 452–456 (1992).
Wolkove, N. et al. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ 176(9), 1299–1304 (2007).
Taylor-Gjevre, R. et al. Components of sleep quality and sleep fragmentation in rheumatoid arthritis and osteoarthritis. Musculoskeletal Care 9(3), 152–159 (2011).
Gjevre, J.-A. et al. Assessment of sleep quality in rheumatoid arthritis and osteoarthritis patients. Chest 138(4 Supplement), 631A (2010).
Weidong, Z. A Research on the Difference of Health of Elderly Between Urban and Rural and Its Influencing Factors (Hebei University, 2018).
Park, H.-M. et al. Relationship between sleep duration and osteoarthritis in middle-aged and older women: A nationwide population-based study. J. Clin. Med. 8(3), 356 (2019).
Jacob, L. et al. Association between sleep disorders and osteoarthritis: A case–control study of 351,932 adults in the UK. J. Sleep Res. e13367. https://doi.org/10.1111/jsr.13367 (2021).
Pickering, M.-E. et al. Sleep disturbances and osteoarthritis. Pain Pract. 16(2), 237–244 (2016).
Fu, K. et al. Sleep quality and fatigue are associated with hip osteoarthritis pain exacerbations: An internet-based case-crossover study. J. Rheumatol. 46(11), 1524–1530 (2019).
Bonsen, T. et al. Sleep quality and duration are related to microvascular function: The Amsterdam Growth and Health Longitudinal Study. J. Sleep Res. 24(2), 140–147 (2015).
Bansil, P. et al. Associations between sleep disorders, sleep duration, quality of sleep, and hypertension: Results from the National Health and Nutrition Examination Survey, 2005 to 2008. J. Clin. Hypertension. 13(10), 739–743 (2011).
Penev, P. Short sleep and circulating adipokine concentrations: Does the fat hit the fire? Sleep. 34(2), 131–132 (2011).
Roman-Blas, J. et al. Osteoarthritis associated with estrogen deficiency. Arthritis Res. Ther. 11, 241 (2009).
Mosca, L. et al. Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women--2011 Update: A Guideline From the American Heart Association. Circulation. 123(11), 1243–1262 (2011).
Fernandes, G.-S. & Ana-M, V. Cardiovascular disease and osteoarthritis: Common pathways and patient outcomes. Eur. J. Clin. Invest. 45(4), 405–414 (2015).
Acknowledgements
Here we are thankful to all the participants in this study. We are also grateful to all the investigators for collecting and calculating data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceived and designed this study: L.R. Wrote original draft: L.R. Review and editing: L.R., X.T., and X.T.; Calculated data: L.R., Y.Z., Q.C., J.Z., and X.T. Performed the study and collected data: Y.Z., J.Z., Q.C., and L.R. Provided with analysis tools: X.T. All authors have read and approved the manuscript in its final form.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ran, L., Chen, Q., Zhang, J. et al. The multimorbidity of hypertension and osteoarthritis and relation with sleep quality and hyperlipemia/hyperglycemia in China’s rural population. Sci Rep 11, 17046 (2021). https://doi.org/10.1038/s41598-021-96523-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96523-0
This article is cited by
-
Interaction between rheumatoid arthritis and mediterranean diet on the risk of cardiovascular disease for the middle aged and elderly from National Health and Nutrition Examination Survey (NHANES)
BMC Public Health (2023)
-
Osteoarthritis is positively associated with self-reported sleep trouble in older adults
Aging Clinical and Experimental Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.